Abstract
Objectives:
Pressure ulcers are a common healthcare problem, particularly among hospitalized patients who need long-term treatment; however, preventive medicine can reduce the prevalence. A multidisciplinary approach is fundamental to providing proper care, and the general health status and cooperation of the patient determine treatment modalities. Simple methods can prevent pressure ulcers and their recurrence. The aim of this study was to share clinical experience and evaluate the approach and treatment modalities used for pressure ulcers.
Methods:
Fifty-two patients hospitalized with the indication of pressure ulcers were evaluated retrospectively. Age, sex, localization of the decubitus ulcer, treatment method, comorbid diseases, and any postoperative complications were analyzed.
Results:
Thirty-five patients were male and 17 were female. The mean age was 50.3 years. The most common accompanying disease was diabetes mellitus and the most common etiology was paraplegia. Pressure ulcers were localized on the sacral area in 45 patients, the ischial area in 23, the trochanteric area in 11 patients, and other parts of the body (scapular, lumbar) in 3 patients. Fasciocutaneous rotation flaps, myocutaneous flaps, and perforator flaps were the most used reconstruction techniques. No major complication was observed.
Conclusion:
The most important point with regard to pressure ulcers is prevention. Healthcare system expenses can be significantly reduced by preventing the formation of decubitus ulcers. The progression of pressure ulcers can be easily controlled if the necessary care and treatment are provided in the early period. The role of the plastic surgeon in advanced stages is to perform reconstruction in appropriate cases and to educate patients and their caregivers with the aim of preventing recurrence.
Keywords: Pressure ulcer, public health, reconstructive surgery
Pressure ulcers are frequently observed in bedridden patients and can lead to major problems when left untreated. There is a high prevalence in hospitalized patients requiring long-term treatment.[1] They are a major reason for hospitalization in immobile patients, and are often seen in elderly patients with impaired sensory function. This represents a significant cost to the healthcare system, and the mortality rate in this patient group is unnecessarily high. Risk factors for pressure ulcers other than advanced age include neurological defects, malnutrition, chronic disease, and immobility. In spite of the development of preventive health services, more than 90% of patients with a spinal cord injury have been reported to develop pressure ulcers, especially in developing countries.[2] The prevalence among hospitalized patients has been as much as 18.1% in Europe,[3] and in studies performed in our country, the incidence has been reported to range between 7.2% and 11.6%;[4] however, it varies between 1% and 50% in intensive care units.[5]
The most successful treatment of pressure ulcers is achieved with multidisciplinary participation from the departments of plastic surgery, physical therapy and rehabilitation, infectious diseases, orthopedics, general surgery, neurology, and internal medicine. Surgical treatment now consists primarily of radical debridement, followed by closure of the defect with flaps with a good blood supply and adequate volume.[6] Ulcer recurrence is more frequent after skin grafting, and this method is no longer used as often. In spite of advances in surgical treatments, recurrence rates sometimes exceed 80%, indicating that this major problem has not been fully resolved.[7] This study was an evaluation of 52 patients with pressure ulcers who were treated in one clinic between 2013 and 2018.
Methods
The data of 52 patients with stage 3 and 4 pressure ulcers who were treated at a single clinic between September 2013 and September 2018 were evaluated retrospectively. The study was conducted in accordance with the Helsinki Declaration and the necessary patient approvals were obtained. Patients details of age, sex, etiology, comorbid factors, location of pressure sores, reconstruction methods, and complications were evaluated.
Conservative treatment was initiated immediately after the patients were admitted to the clinic. Pressure ulcers were managed with position change in the bed every 2 hours, rest on an air-filled or other soft cushion, and preventing both drying of the skin and contamination of the ulcerated area with stool and urine. Since infection complicates the management of pressure sores, the antibiotherapy in use was carefully monitored and adjusted as needed according to the results of the histopathological examination of the biopsy sample and the antibiogram in patients who demonstrated any signs of infection.
The hemodynamic status (hemoglobin, albumin, kidney and liver function tests) of the patient was reviewed before the permanent closure of the wound was performed. In particular, medical therapies recommended by the neurology clinic for the treatment of muscle spasms observed in patients with spinal cord injury and appropriate exercise recommendations by the physical therapy and rehabilitation clinics were arranged. Patients with a stable general condition and hemodynamic state were considered to be ready for reconstructive surgery when their infection was cured, muscle spasms had resolved, and their wounds were completely free of necrotic tissue.
The surgical treatment began with the removal of the bursa and any heterotopic calcification around the ulcer. Any bone protrusions that might cause pressure ulcers and any infected necrotic bone fragments were also removed. Care was taken to ensure hemostasis. The defect was closed with very well perfused flaps so that all dead spaces were secured.
Results
The study population consisted of 52 patients (35 men and 17 women). The mean age of the patients was 50.3 years (range: 2-91 years). The most common comorbidity was diabetes mellitus (12 patients), followed by hypertension and ischemic heart disease (Table 1). The most common factor in the etiology was paraplegia (n=23), followed by a history of recent intensive care treatment (n=18) (Table 2).
Table 1.
Comorbidities
| n | % | |
|---|---|---|
| Diabetes mellitus | 12 | 23 |
| Hypertension | 11 | 21 |
| Ischemic heart disease | 5 | 10 |
| Chronic obstructive pulmonary disease | 3 | 6 |
| Other (malignancy, dementia, Parkinson’s disease, multiple sclerosis, Guillain-Barre syndrome) | 8 | 15 |
Table 2.
Etiological factors
| n | % | |
|---|---|---|
| Paraplegia | 23 | 44 |
| History of stay in intensive care unit | 18 | 35 |
| Other (scoliosis, spina bifida, polio sequelae, postoperative immobility) | 9 | 17 |
There were 84 pressure ulcers observed in the 52 study patients. The ulcers were primarily localized on the sacral region (n=45), followed by the ischial (n=23) and trochanteric (n=11) regions (Table 3). The reconstruction methods used most often were a fasciocutaneous rotation flap, musculocutaneous flap, and a perforator flap. One patient underwent primary suturing (Fig. 1) (Table 4). The mean duration of hospital stay was 14 days (range: 1-47 days). The postoperative complication rate was 17.3%. The most common complication to occur was dehiscence on the suture line, seen in 5 cases. Hematoma and seroma formation were observed in 2 patients, and there was partial necrosis in 2 cases. The patients who had partial necrosis were treated with a post-debridement fascia advancement flap or graft.
Table 3.
Location of pressure ulcers
| n | % | |
|---|---|---|
| Sacral region | 45 | 86 |
| Ischial region | 23 | 44 |
| Trochanteric region | 11 | 21 |
| Other regions (lumbar, vertebral, scapular) | 4 | 8 |
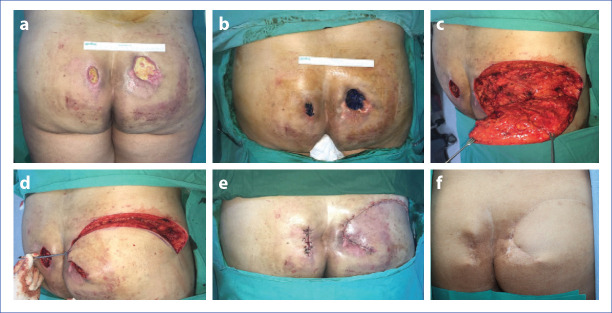
Figure 1.
(a). Parasacral pressure ulcer, preoperative appearance, (b) delineation of the contours of the pressure ulcer with methylene blue dye, (c) designing a fasciocutaneous flap after debridement and el vation over the muscle, (d) advancement of the flap, (e) early postoperative outcome, (f) appearance at postoperative second year.
Table 4.
Materials used in reconstruction
| n | % | |
|---|---|---|
| Fasciocutaneous rotation flap | 41 | 79 |
| Musculocutaneous flap | 21 | 40 |
| Perforator flap | 10 | 19 |
| Tensor fascia lata advancement flap | 8 | 15 |
| Bipediculated flap | 4 | 8 |
| Primary suture | 1 | 2 |
Discussion
Although pressure ulcers are seen in people of all ages, the incidence increases with age. The prevalence varies from study to study and from country to country.[2–5]
Reconstruction of the defect is essential after all dead tissue is removed. This may involve myocutaneous, fasciocutaneous, local skin, advancement, perforator flaps, or other flaps. In our practice, patients were followed up with dressings or vacuum assisted closure after debridement until they were ready for surgery.
Pressure ulcers are most frequently observed on the sacrum, ischial and trochanteric regions, and the heels. In a 2000-case study conducted by Dansereau and Conley,[8] the authors observed that pressure ulcers were seen in the ischial (28%), trochanteric (19%), sacral (17%) and regions, and 36% were localized on the heels, malleoli, and knees. The results of our study indicated the presence of pressure ulcers in the sacral (n=45, 86%), ischial (n=23, 44%), trochanteric (n=11, 21%), and other regions (scapula, lumbar region: n=4, 4%).
Sacral pressure ulcers are frequently seen in patients with spinal cord injuries.[9] In our study, the most common etiological factor in patients with sacral pressure ulcers was a history of intensive care unit treatment (n=17) and paraplegia (n=19).
The most commonly used flaps for cavitary sacral pressure ulcers were fasciocutaneous flaps, musculocutaneous flaps, and perforator flaps. Fasciocutaneous flaps are thinner than musculocutaneous flaps, which might appear to be a disadvantage, however, flap rotation and adaptation are easier with fasciocutaneous flaps. Moreover, the risk of recurrence is less when compared with muscle-skin flaps. [10, 11] In our practice we have preferred to use gluteus maximus muscle-skin flaps for the repair of cavitary sacral pressure ulcers in bedridden patients.
The use of perforator-based V-Y advancement flaps, tensor fascia lata (TFL) flaps, and musculocutaneous flaps has been described for the repair of trochanteric pressure ulcers.[12–14] We most often used TFL V-Y advancement flaps to treat trochanteric pressure ulcers. Techniques defined for the repair of ischial pressure ulcers include using phytocutaneous flaps, perforator flaps, and myocutaneous flaps. [15–17] Fasciocutaneous rotation flaps were employed most frequently in this study to treat ischial pressure ulcers.
Erçöçen et al.[18] reported a complication rate in the postoperative period of 17.3%, and the most commonly seen complications were detachment on the suture line, infection, and flap necrosis. In another study, Bamba et al.[19] found a complication rate of 58.7%, with recurrence and infection on the suture line as the most common long-term complications reported. In our study, the rate of complications was also 17.3%, and the most commonly seen was detachment of the suture line, which was consistent with the literature. Seroma, hematoma, and partial necrosis of the flap were also observed in our study.
Pressure ulcers are common in hospitalized patients who are receiving long-term treatment. Paraplegia is the most common etiological factor described in the literature, and the same was true in our series, followed by patients without paraplegia with a history of intensive care unit treatment.[20, 21] This was a noteworthy finding, demonstrating that preventive medicine can help to avoid the development of pressure ulcers.
Although reconstruction is still a controversial issue in e derly patients with advanced pressure ulcers, it has been established that infection, protein loss, morbidity, and mortality will increase in patients without proper debridement and reconstruction.[21, 22] Appropriate patient selection, debridement, and reconstruction with appropriate postoperative rehabilitation with can be very beneficial in elderly patients. In patients whose general health condition is a contraindication for surgery, at a minimum, progression of pressure ulcers can be prevented with good wound care and conservative treatment.
Conclusion
Pressure ulcer management is not a simple process and it can be particularly complicated in patients with comorbidities. Many patients in the risk group for the pressure ulcers are also at risk in terms of cardiovascular, pulmonary, and urological problems, as well as coagulopathy.[22] The presence of additional issues, such as infection and systemic problems, further increase mortality and morbidity.
Preventive medicine is very important in the prevention of pressure ulcers. In particular, the elderly as well as hospitalized and immobile patients and their relatives should be given training on how to prevent pressure ulcers and the greatest care should be provided to these patients. Once a pressure ulcer has occurred, the most effective way to prevent the progression of disease is to start the treatment process with a multidisciplinary approach as quickly as possible.
Disclosures
Peer-review: Externally peer-reviewed.
Conflict of Interest: None declared.
Authorship Contributions: Concept – F.I., S.H.K.; Design – F.I., S.H.K., S.B.; Supervision – S.H.K., F.I.; Materials – M.S., H.A.A.; Data collection &/or processing – M.S., H.A.A.; Analysis and/or interpretation – F.I., S.B.; Literature search – F.I., S.B., H.A.A.; Writing – F.I., S.B.; Critical review – F.I., M.S., H.A.A.
References
- 1.Meehan M. Multisite pressure ulcer prevalence survey. Decubitus. 1990;3:14–7. doi: 10.1097/00129334-199011000-00006. [CrossRef ] [DOI] [PubMed] [Google Scholar]
- 2.Burns AS, O'Connell C. The challenge of spinal cord injury care in the developing world. J Spinal Cord Med. 2012;35:3–8. doi: 10.1179/2045772311Y.0000000043. [CrossRef ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vanderwee K, Clark M, Dealey C, Gunningberg L, Defloor T. Pressure ulcer prevalence in Europe:a pilot study. J Eval Clin Pract. 2007;13:227–35. doi: 10.1111/j.1365-2753.2006.00684.x. [CrossRef ] [DOI] [PubMed] [Google Scholar]
- 4.Baydar M, Peker Ö. Epidemiology of Pressure Ulcer. Turkiye Klinikleri J Int Med Sci. 2007;3:1–5. [Google Scholar]
- 5.Manzano F, Navarro MJ, Roldán D, Moral MA, Leyva I, Guerrero C, et al. Granada UPP Group. Pressure ulcer incidence and risk factors in ventilated intensive care patients. J Crit Care. 2010;25:469–76. doi: 10.1016/j.jcrc.2009.09.002. [CrossRef ] [DOI] [PubMed] [Google Scholar]
- 6.Bamba R, Madden JJ, Hoffman AN, Kim JS, Thayer WP, Nanney LB, et al. Flap Reconstruction for Pressure Ulcers: An Outcomes Analysis. Plast Reconstr Surg Glob Open. 2017;5:e1187. doi: 10.1097/GOX.0000000000001187. [CrossRef ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Evans GR, Dufresne CR, Manson PN. Surgical correction of pressure ulcers in an urban center: is it efficacious? Adv Wound Care. 1994;7:40–6. [PubMed] [Google Scholar]
- 8.Dansereau JG, Conway H. Closure of Decubiti in Paraplegics. Report of 2000 Cases. Plast Reconstr Surg. 1964;33:474–80. [CrossRef] [PubMed] [Google Scholar]
- 9.Gusenoff JA, Redett RJ, Nahabedian MY. Outcomes for surgical coverage of pressure sores in nonambulatory, nonparaplegic, elderly patients. Ann Plast Surg. 2002;48:633–40. doi: 10.1097/00000637-200206000-00012. [CrossRef ] [DOI] [PubMed] [Google Scholar]
- 10.Yamamoto Y, Ohura T, Shintomi Y, Sugihara T, Nohira K, Igawa H. Superiority of the fasciocutaneous flap in reconstruction of sacral pressure sores. Ann Plast Surg. 1993;30:116–21. doi: 10.1097/00000637-199302000-00004. [CrossRef ] [DOI] [PubMed] [Google Scholar]
- 11.Aggarwal A, Sangwan SS, Siwach RC, Batra KM. Gluteus maximus island flap for the repair of sacral pressure sores. Spinal Cord. 1996;34:346–50. doi: 10.1038/sc.1996.63. [CrossRef ] [DOI] [PubMed] [Google Scholar]
- 12.Yildirim S, Taylan G, Aköz T. Freestyle perforator-based V-Y advancement flap for reconstruction of soft tissue defects at various anatomic regions. Ann Plast Surg. 2007;58:501–6. doi: 10.1097/01.sap.0000247953.36082.f4. [CrossRef ] [DOI] [PubMed] [Google Scholar]
- 13.Borman H, Maral T. The gluteal fasciocutaneous rotation-advancement flap with V-Y closure in the management of sacral pressure sores. Plast Reconstr Surg. 2002;109:2325–9. doi: 10.1097/00006534-200206000-00025. [CrossRef ] [DOI] [PubMed] [Google Scholar]
- 14.Nisanci M, Sahin I, Eski M, Alhan D. A new flap alternative for trochanteric pressure sore coverage:distal gluteus maximus musculocutaneous advancement flap. Ann Plast Surg. 2015;74:214–9. doi: 10.1097/SAP.0b013e3182920c7c. [DOI] [PubMed] [Google Scholar]
- 15.Kumar U, Jain P. Infragluteal fasciocutaneous flap for management of recurrent ischial pressure sore. Indian J Plast Surg. 2018;51:70–76. doi: 10.4103/ijps.IJPS_15_18. [CrossRef ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Legemate CM, van der Kwaak M, Gobets D, Huikeshoven M, van Zuijlen PPM. The pedicled internal pudendal artery perforator (PIPAP) flap for ischial pressure sore reconstruction: Technique and long-term outcome of a cohort study. J Plast Reconstr Aesthet Surg. 2018;71:889–94. doi: 10.1016/j.bjps.2018.01.032. [CrossRef ] [DOI] [PubMed] [Google Scholar]
- 17.Lefèvre C, Bellier-Waast F, Lejeune F, Duteille F, Kieny P, Le Fort M, et al. Ten years of myocutaneous flaps for pressure ulcers in patients with spinal lesions:Analysis of complications in the framework of a specialised medical-surgical pathway. J Plast Reconstr Aesthet Surg. 2018;71:1652–63. doi: 10.1016/j.bjps.2018.07.007. [CrossRef ] [DOI] [PubMed] [Google Scholar]
- 18.Erçöçen AR, Yılmaz S, Can Z, Emiroğlu M, Yormuk E. Basıyaralarının cerrahi tedavisi: 108 Olgunun değerlendirilmesi. Turk J Plast Surg. 2000;8:82–89. [Google Scholar]
- 19.Bamba R, Madden JJ, Hoffman AN, Kim JS, Thayer WP, Nanney LB, et al. Flap Reconstruction for Pressure Ulcers: An Outcomes Analysis. Plast Reconstr Surg Glob Open. 2017;5:e1187. doi: 10.1097/GOX.0000000000001187. [CrossRef ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leigh IH, Bennett G. Pressure ulcers:prevalence, etiology, and treatment modalities. A review. Am J Surg. 1994;167:25S–30S. doi: 10.1016/0002-9610(94)90007-8. [DOI] [PubMed] [Google Scholar]
- 21.Cushing CA, Phillips LG. Evidence-based medicine:pressure sores. Plast Reconstr Surg. 2013;132:1720–32. doi: 10.1097/PRS.0b013e3182a808ba. [CrossRef ] [DOI] [PubMed] [Google Scholar]
- 22.Kwok AC, Simpson AM, Willcockson J, Donato DP, Goodwin IA, Agarwal JP. Complications and their associations following the surgical repair of pressure ulcers. Am J Surg. 2018;216:1177–81. doi: 10.1016/j.amjsurg.2018.01.012. [DOI] [PubMed] [Google Scholar]