Abstract
Background
One of the modifiable risk factors for ST elevation myocardial infarction is prehospital delay. The purpose of our study was to look at the effect of contamination contamination obsession on prehospital delay compared with other measurements during the Covid-19 pandemic.
Method
A total of 139 patients with acute STEMI admitted to our heart center from 20 March 2020 to 20 June 2020 were included in this study. If the time interval between the estimated onset of symptoms and admission to the emergency room was >120 min, it was considered as a prehospital delay. The Beck Depression Inventory (BDI), the Beck Anxiety Inventory (BAI), and Padua Inventory-Washington State University Revision (PI-WSUR) test were used to assess Contamination-Obbsessive compulsive disorder (C-OCD).
Result
The same period STEMI count compared to the previous year decreased 25%. The duration of symptoms onset to hospital admission was longer in the first month compared to second and third months (180 (120–360), 120 (60–180), and 105 (60–180), respectively; P = 0.012). Multivariable logistic regression (model-2) was used to examine the association between 7 candidate predictors (age, gender, diabetes mellitus (DM), hypertension, smoking, pain-onset time, and coronary artery disease (CAD) history), PI-WSUR C-OCD, and admission month with prehospital delay. Among variables, PI-WSUR C-OCD and admission month were independently associated with prehospital delay (OR 5.36 (2.11–13.61) (P = 0.01); 0.26 (0.09–0.87) p < 0.001] respectively].
Conclusion
Our study confirmed that contamination obsession was associated with prehospital delay of STEMI patients, however anxiety and depression level was not associated during the pandemic.
Keywords: STEMI, Contamination obsession, Prehospital delay
1. Background
In recent years, a dramatic increase in coronary artery disease prevalence has become a significant health problem [1,2]. The adoption of new medical and pharmaco-invasive treatments has decreased in-hospital mortality in acute coronary syndrome (ACS) from 30% to 3%–8% today. Many clinical, demographic and laboratory parameters and risk scores have been demonstrated to predict hospitalization, adverse effects, and mortality of ACS [3,4]. Prehospital delay is one of the modifiable prognostic risk factors for STEMI patients.
The potential for divergence of medical attention and resources from ACS and other acute diseases is one of the significant potential consequences of coronavirus disease 2019 (COVID-19), alongside the morbidity and mortality associated with the viral infection. During the pandemic, delays in hospital admissions were expected, confirmed by several studies [[5], [6], [7], [8]]. However, efforts to overcome this problem during the early period of the pandemic has been made in the UK. Mafham et al. pointed out that the drop in hospital admission for ACS was reduced following a publicity campaign by a scientific community in England [9].
Anti-contamination practices such as hand washing have reduced the spread of COVID-19, However, they have led to a surge in some mental health problems like Obsessive-Compulsive Disorder (OCD), which is recognized as a severe anxiety disorder [10,11]. Contamination OCD (C-OCD) is the most prevalent type of OCD characterized by washing behaviours or avoiding contaminated objects. In vulnerable people who have different types of obsessions and compulsions, the sanitation habits started as a normal shielding behavior, unfortunately, might lead to C-OCD. However, COVID-19 anxiety cannot be predicted according to the pre-pandemic contamination and obsessive-compulsive washing symptoms [12].
We investigated the variations in OCD symptoms at different months and their relationship with monthly varying prehospital delay in STEMI patients. As far as the researchers investigated, to our knowledge no studies have evaluated the effect of OCD, depression, and anxiety altogether on prehospital delay in STEMI patients so far. A better understanding of this impact may play an essential role in increasing access to revascularization in patients with STEMI and improving prognosis. As a result, we aimed to investigate the effect of C-OCD on prehospital delay compared with other measurements during the COVID-19 pandemic.
2. Method
2.1. Study population
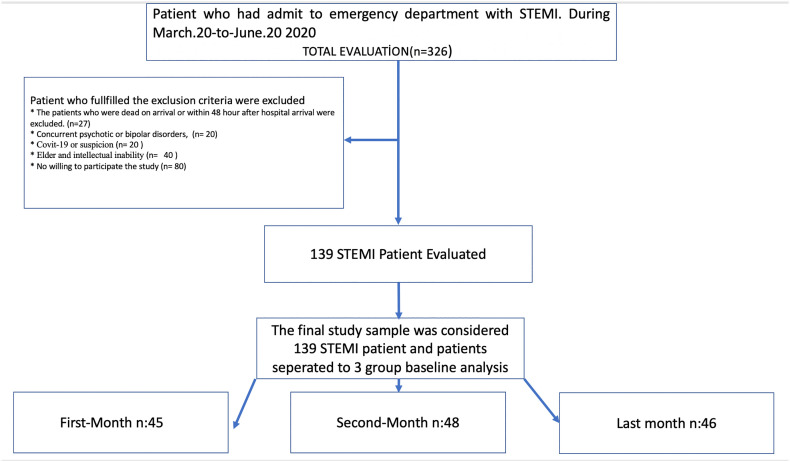
This cross-sectional study included 139 patients with STEMI. The inclusion criteria were age ≥ 18 years, a final discharge diagnosis of acute STEMI, with elevated troponin levels; the detailed inclusion and exclusion criteria were displayed in the consort flow diagram of the study (Fig. 1 ). Accordingly, patients with acute STEMI admitted to our macro-hub heart center from 20 March 2020 to 20 June 2020, who survived for more than 48 h, and agreed to participate in our research were included in this study.
Fig. 1.
Consort flow diagram (inclusion-exclusion criteria).
2.2. Data collection and verification
The duration of symptoms onset to hospital admission was determined as the prehospital delay.
time. The symptoms onset was defined as the time reported by patients when they were aware.
of their acute or severe illness, and this condition prompted them to seek medical attention. Only patients admitted to the hospital within 24 h of the onset of symptoms were included.
2.3. Definitions and outcomes
Admissions to the emergency department are more likely to be associated with heart disease at our center because it is a major center for cardiovascular diseases. Since non-cardiac reasons like COVID-19 may increase the troponin and result in misdiagnosis, non-STEMI patients were not included in the study.
Demographic characteristics of the patients were recorded. A 12‑lead electrocardiogram (ECG) along with emergency bedside transthoracic echocardiography (TTE) were performed on all patients. STEMI diagnosis was defined based on confirmed ECG, troponin positivity, and the guidelines by the European Society of Cardiology (ESC). All cases were also confirmed angiographically [13]. TTE was performed in the emergency unit to classify as ejection fraction ≤35, between 35 and 50, or 50 ≥ using the Philips iE33 Doppler Ultrasound System.
2.4. Prehospital time definition
Patients admitted to the emergency department without an ambulance were categorized as self-transported and those arriving by ambulance were categorized as ambulance transported. If the time interval between the estimated onset of symptoms and admission to the emergency room was >120 min, it was described (categorized) as a prehospital delay [14,15].
The application of primary percutaneous intervention during the pandemic period was not changed. Patients under investigation (PUI) for Covid-19 had procedures performed in isolated rooms with adequate personal protective equipment.
2.5. Data collection
The patients were asked to complete a standard questionnaire after being transferred from the intensive care unit to the inpatient unit during the hospitalization. The interviews were conducted by cardiology resident [BK, DC], and all demographic data, cardiovascular risk factors, medical history, comorbidities, and symptoms associated with the acute myocardial infarction (MI) were recorded. Pain onset time was categorized as day time [after 8 a.m. to 6 p.m.] or night-time [after 6 p.m. to 8 a.m.] according to onset of symptoms. The level of literacy and education was assessed using three different answer options reflecting the national education system. Besides, fear of contracting COVID-19 before admission to hospital was also questioned, and patients' responses were recorded as mild, moderate, or high.
The Beck Depression Inventory (BDI) and the Beck Anxiety Inventory (BAI) were applied to.
measure the frequency and severity of patient depression and anxiety. Padua Inventory-Washington State University Revision (PI-WSUR) was used to assess obsession severity. BDI.
and BAI are Likert-type scales that involve 21 symptoms and attitudes, behavioral changes, and.
somatic symptoms [16,17]. We used PI-WSUR as it has been validated for screening purposes and matched better with our study. The PI-WSUR scale consists of 39 items and five subscales. We used PI-WSUR-total and PI-WSUR C-OCD subscales for analysis [18]. Patients with difficulties in reading or writing were supported while filling out the questionnaires. In addition, ambiguous questions and answers were explained without any guidance for their decision. Each question was scored with a 5-point Likert from 0 (not at all) to 4 (very much). Laboratory analysis results were obtained from the hospital information system, and only admission laboratory values were used for analyses. The study was performed according to the principles stated in the Declaration of Helsinki, and it was approved by the local Ethics Committee. Informed consent was obtained from all participants included in the study.
2.6. Statistical analysis
Kolmogorov-Smirnov test and/or a visual histogram were used to assess normality. Non-normally distributed continuous variables were expressed as the median and interquartile range [IQR] [quartile 1 to quartile 3]; and normally distributed variables were expressed as mean ± standard deviation [SD]. Then, an independent t-test or Mann–Whitney U test was used to compare the two groups according to distribution. Categorical variables were compared by Chi-Square or Fisher exact test and presented as a count and percentage. Moreover, for [For] comparing continuous variables in the three groups according to their admission months, we used ANOVA and Kruskal-Wallis tests according to the distribution of variables; in addition, we used the Chisquare test for categorical data comparison among the three groups
2.6.1. Primary outcome
The primary outcome is a prehospital delay, the delayed arrival to the hospital, and we defined as the time from symptom onset to arriving at the emergency department. Prehospital delay was defined as the time from symptoms onset to arriving at the emergency department. We defined admission time > 120 min as prehospital delay since it was established in previous studies [14,15].
2.6.2. Candidate predictors
We applied logistic regression method to investigate the relationship between the primary outcome (prehospital delay) and candidate predictors. Effects of individual predictors were reported using Odds-ratio (OR) and 95% confidence interval (CI). All continuous variables were incorporated into the model as flexible smooth parameters using restricted cubic spline, then the effects of continuous predictors were summarized using their interquartile range. Due to the expectation of interaction between “admission-month* variables [PI-WSUR, PI-WSUR C-OCD], the interaction term was appended to the regression models. Variables with low <5% or high frequency > 95% were excluded from the model. As a result, we included Age, Gender, diabetes mellitus (DM), hypertension (HT), Smoking history, Pain time [day or night], and CAD history as seven-candidate predictors for all models.
The association of prehospital-delay with seven candidate predictors, admission-month, and “PI-WSUR” was evaluated using logistic regression (Model-1).
In model 2, we used “PI-WSUR C-OCD”, instead of PI-WSUR, but other predictor variables were the same. In model 3, we used PI-WSUR C-OCD, BDI, and BAI instead of PI-WSUR, but other predictor variables were the same as model-1.
2.6.3. Model Performance measurement
Performance of the models measured by Likelihood ratio X [2], Bayesian information criteria (BIC), and the Harrel’ C-index. The models were compared according to the assessment of fit (likelihood ratio Chi-square) and quality (BIC); and the partial χ2 value was used to evaluate the relative significance of each predictor in model 1 and model 2.
The calibration was assessed by plotting the observed outcome on the y-axis and the predicted outcome on the x-axis. Deviation from the 45° line indicates bias for the predicted outcome. C-index was used to evaluate the discrimination of the model. Bootstrap resampling, which used 200 random samples drawn with replacement, was performed for internal validation. In each bootstrap sample, predictive models were developed and evaluated in the whole sample to quantify the optimism in the estimated apparent performance.
2.6.4. Nomogram
This diagram provides a graphical depiction of all variables in the model (we use it for model-2) in addition to allowing the user to obtain predicted values manually.
All statistical analyzes were performed using “rms”, “Hmisc”, “gtrendr” and “ggplot2” packages with R version 4.02 (R statistical software, Vienna, Austria).
3. Results
The study comprised 139 patients (45, 48, and 46 in the first, second, and third months.
respectively), and the patients' demographic characteristics are presented in Table 1 . There was.
Table 1.
Baseline characteristics of all group, and also comparison labaratory, clinical, and physcological differance according to admission month.
| Variables | All group 139 | First: n:45 (march20-april20) | Second n:48 (April20–May20) |
Third n:46 (May20–June20) |
P value |
|---|---|---|---|---|---|
| age | 55(48–64) | 55(49–66) | 53(43.5–62.3) | 56(51–64) | 0.512 |
| Gender (male) | 95(68.3%) | 34(75.6%) | 35(72.9%) | 26(56.5%) | 0.104 |
| Diabetes mellitus | 27(19.4%) | 8(17.8%) | 5(10.4%) | 14(30.4%) | 0.053 |
| Hypertension | 37(26.6%) | 15(33.3%) | 10(20.8%) | 12(26.1%) | 0.393 |
| Hystory of CAD | 25(18%) | 7(15.6%) | 9(18.8%) | 9(19.6%) | 0.871 |
| Dyslipidemia | 37(26.6%) | 14(31.1%) | 11(22.9%) | 12(26.1%) | 0.668 |
| Smoking (any-time) | 102(73.4%) | 31(68.9%) | 31(64.6%) | 40(87%) | 0.035 |
| Symptoms onset time, day-time | 70 (50.4%) | 26(57.8) | 22(45.8%) | 22(47.8%) | 0.472 |
| Symptom-to-admit hospital (minutes) | 120(60–180) | 180(120–360) | 120(60–180) | 105(60–180) | 0.012 |
| Door-to-Wiring duration minutes | 35(29–42) | 38(31–50) | 33(28–45) | 33(29–42) | 0.062 |
| St elevation amount (lead) | 3(3–4) | 3(3–5) | 3(3–4.25) | 3(3–4) | 0.117 |
| Hospitalization duration day | 3-(3–5) | 3(3–6) | 3(3–4) | 4(3–5) | 0.112 |
| Symptom-pain severity | 9(8–10) | 9(8–10) | 9(8–10) | 9(7–10) | 0.442 |
| Chest pain | 139 (100%) | 45(100%) | 48(100%) | 46(100%) | 1.00 |
| Back-pain | 35(25.2) | 12(26.7%) | 12(25%) | 11(23.9%) | 0.955 |
| Sweating | 77(55.4%) | 19(42.2%) | 34(70.8) | 24(52.2%) | 0.018 |
| Dyspne | 21(15.1%) | 2(4.4%) | 10(20.8) | 9(19.6%) | 0.052 |
| Gastrointestinal symptom | 51(36.7%) | 13(28.9%) | 15(31.3%) | 23(50%) | 0.071 |
| Afraid of virus low Intermediate high |
76 (54.7%) 37(26.6%) 26(18.7%) |
27(60.0%) 6(13.3%) 12(26.7%) |
24(50%) 19(39.6%) 5(10.4%) |
25(54.3%) 12(26.1%) 9(19.6%) |
0.045 |
| Preceding angina | 53(38.1%) | 16(35.6%) | 19(39.6%) | 18(39.1%) | 0.910 |
| Infarct localisation (anterior) | 68(48.9%) | 22(48.9%) | 23(47.9%) | 26(56.5%) | 0.662 |
| Admission ef <35 35–50 <50 |
10(7.2%) 84(72.3%) 45 (20.2%) |
6(13.3%) 32(71.1%) 7(15.6%) |
4(8.3%) 24(50%) 20(41.7%) |
1(2.1%) 28(60.9%) 18(39.1%) |
0.01 |
| Use of ambulance | 84 (60.9%) | 26(57.8%) | 26(55.3%) | 32(69.6%) | 0.325 |
| Sedantary life | 61 (43.9%) | 12(26.7%) | 22(45.8%) | 27(58.7%) | 0.008 |
| Systolic BP mmhg | 122(110–135) | 122(110–136) | 124(112–140) | 114(100–129) | 0.066 |
| Diastolic BP mmhg | 73(70–84) | 75(70–84) | 80(70–86) | 73(69–75) | 0.053 |
| Hemoglobin g/dl | 14.6(13.1–15.5) | 14.1(12.9–15.5) | 14.9(13.3–15.8) | 14.5(12.7–15.3) | 0.150 |
| White blood cell | 12.6(9.9–14.9) | 13.2(10.0–15.1) | 12.6(9.9–13.9) | 11.4(9.3–15.0) | 0.742 |
| Platelet per-cubic mm3 | 272(222–338) | 258(227–336) | 284(248–360) | 255(195–299) | 0.041 |
| Creatinine (mg/dl) | 0.85(0.75–1.0) | 0.90(0.80–0.98) | 0.90(0.76–1.0) | 0.81(0.70–1.01) | 0.314 |
| SpO2 | 97(96–97) | 96(96–97) | 97(96–97) | 97(96–97.3) | 0.195 |
| Support from relative | 31(22.3%) | 9(20%) | 16(33.3%) | 6(13%) | 0.055 |
| House person-lived | 3(2–4) | 4(3–5) | 3(2–4) | 3(2–4) | 0.665 |
| Education. low Middle high |
69(49.6%) 23(16.5%) 47(33.8%) |
22(48.9%) 13(28.9%) 10(22.2%) |
23(47.9%) 4(8.3%) 21(43.8%) |
24(52.2%) 6(13%) 16(34.8%) |
0.045 |
| PI-WSUR total | 35(20–49) | 37(27–63) | 36(23–49) | 25(15–44) | 0.005 |
| PI-WSUR C-OCD | 16 (8–27) | 21(11–32) | 16.5(9–26) | 11(5–24) | <0.001 |
| Beck anxiety inventory | 4(2–6) | 6(4–12) | 4(1–5) | 3(2–4) | <0.001 |
| Beck depression inventory | 5 (2–6) | 8(3–14) | 5(2−12) | 4(2–6) | <0.001 |
Data are given in mean ± SD or in numbers with percentages. The one-way ANOVA, Kruskal-Wallis rank sum test, Fisher's exact test and χ2 test were performed. Gastrointestinal symptom (indigestion, and/or nausea and/or vomiting), PI-WSUR:Padua inventory Washington university revision. C-OCD:Contamination obsessive compulsive disorder, BP- blood pressure; CAD- coronary artery disease, CV- cardiovascular; IQR- interquartile range day-time: 8 am-18 pm.
no statistically significant difference in terms of age, gender, DM, and HT. However, the duration of prehospital admissions was longer in the first month than the second and third months (180 (120–360), 120 (60–180), and 105 (60–180), respectively; P = 0.012). In case of.
over three months, there was a statistically significant difference for PI-WSUR, PI-WSUR C-OCD, BDI, and BAI (0.005, <0.001, <0.001, <0.001, respectively). However, there was no statistically significant difference in support levels from relatives and housemates for each month across three months (P = 0.055, P = 0.655, respectively). There was a 25% reduction in the.
number of STEMI cases in the “same time-frame” compared with the previous year (438 cases in 2019 and 326 cases in 2020).
A univariable logistic regression demonstrated no association between prehospital-delay and potential predictors, including age, gender, DM and HT (Table 2 ). Conversely, admission month, PI-WSUR, PI-WSUR C-OCD, BDI, and BAI were associated with prehospital delay (from first month to third month OR 0.21(0.08–0.54), OR 3.81(2.02–7.16), OR 5.38(2.54–11.39), OR 2.26(1.24–4.13), OR 1.60(1.03–2.47), respectively).
Table 2.
Univariable logistic regression between prehospital-delay and predictors.
| Variables | Odds-ratio and CI | p value |
|---|---|---|
| Age (from 48 to 64 years) | 1.47 (0.88–2.46) | 0.13 |
| Gender (male referance) | 1.34 (0.63–2.83) | 0.43 |
| Diabetes mellitus | 0.90 (0.38–2.13) | 0.82 |
| Hypertension | 1.72 (0.76–3.86) | 0.18 |
| Smoking | 0.42 (0.18–1.01) | 0.06 |
| Coronary Artery Disease history | 0.42 (0.17–1.02) | 0.06 |
| Pain time (day-time referance) | 0.31(0.15–0.64) | 0.001 |
| PI-WUR total (from 20 to 49) | 3.81 (2.02–7.16) | <0.001 |
| Beck-depression (from 2 to 9) | 2.26(1.24–4.13) | 0.007 |
| Beck-anxiety (from 2 to 6) | 1.60(1.03–2.47) | 0.03 |
| Admission-month (from first month to third month) | 0.21(0.08–0.54) | 0.001 |
| PI-WSUR C-OCD (from 8 to 27.5) | 5.38(2.54–11.39) | <0.001 |
Data are given in OR (95%CI). Univariable Logistic regression analyses was used.
Abbreviation: PI-WSUR; Padua inverntory Washington university revision, C-OCD:Contamination obsessive compulsive disorder.
Multivariable logistic regression was used to examine the association between the mentioned 7 candidate predictors, PI-WSUR, and admission month with the prehospital delay (Table 3 , model 1). Among variables, PI-WSUR and admission month were independently associated with prehospital delay (OR 3.45 (1.62–7.34) (P = 0.04); 0.33 (0.11–0.97) (P < 0.001), respectively).
Table 3.
Multivariable logistic regression, model-1, model-2 and model-3. Model performance measurements.
| Variables | Odds-ratio and CI | P value | C-index | Likelihood ratio | BIC | p interaction |
|---|---|---|---|---|---|---|
| Model-1 |
0.830 |
51.73 |
188.2 |
0.002 |
||
| PI-WSUR total (from 20 to 49) | 3.45 (1.62–7.34) | 0.04 | ||||
| Admission-month (from first month to third month) | 0.33 (0.11–0.97) | 0.01 | ||||
| Model-2 |
0.855 |
58.31 |
181.6 |
<0.001 |
||
| PI-WSUR-C-OCD (from 8 to 27.5) | 5.36 (2.11–13.61) | 0.01 | ||||
| Admission-month (from first month to third month) | 0.26 (0.09–0.87) | <0.001 | ||||
| Model-3 |
0.856 |
59.30 |
190.6 |
<0.001 |
||
| PI-WSUR C-OCD (from 8 to 27.5) | 4.87 (1.74–13.61) | 0.02 | ||||
| Beck-depression inventory (from 2 to 9) | 1.13 (0.46–2.79) | 0.77 | ||||
| Beck-anxiety inventory (from 2 to 6) | 1.28 (0.74–2.20) | 0.36 | ||||
| Admission-month (from first month to third month) | 0.32 (0.10–0.98) | <0.001 | ||||
Data are given in Odds-Ratio (95%CI). Multivariable Logistic regression analyses was used All 3 models adjusted Age, Gender, Diabetes Mellitus, Hypertension, Smoking hystory, Pain time (daytime (from 8 a.m. to 6 p.m.) or at night (from 6 p.m. to 8 a.m.) and Coronary artery disease history. p value for odds-ratio; p interaction for model1- PI-WUR-total scores and admission month interaction p-value, for model 2–3 interaction between month and PI-WUR-contamination scores and admission-month interaction p-value. Abrevations: BIC: Bayesian information criteria (lower value depict better model), Harrel c-index statistics measures the discriminative ability of the model, and values closer to 1.0 are better. Likelihood Ratio X2 higher value represent better model performance. PI-WSUR:Padua inventory-Washington university revision, C-OCD:Contamination obsessive compulsive disorder.
Furthermore, the relationship between 7 predictors, PI-WSUR C-OCD, and admission month with prehospital delay was examined in model 2. PI-WSUR C-OCD and admission month were independently associated with the prehospital delay in model 2 (OR 5.36 (2.11–13.61) (P = 0.01); 0.26 (0.09–0.87) (P < 0.001), respectively). The interactions between admission month and PI-WSUR C-OCD were assessed (P < 0.001 for interaction) (Table 3, model 2). Additionally, the relationships of the 7 predictors, PI-WSUR C-OCD, BDI, BAI, and admission month with prehospital delay were examined in model 3. PI-WSUR C-OCD and admission month were independently associated with the prehospital delay (OR 4.87 (1.74–13.61) (P = 0.02); 0.32 (0.10–0.98) (P < 0.001), respectively). However, BDI and BAI were not associated with prehospital delay. The interactions between admission month and PI-WSUR C-OCD were assessed (P < 0.001 for interaction).
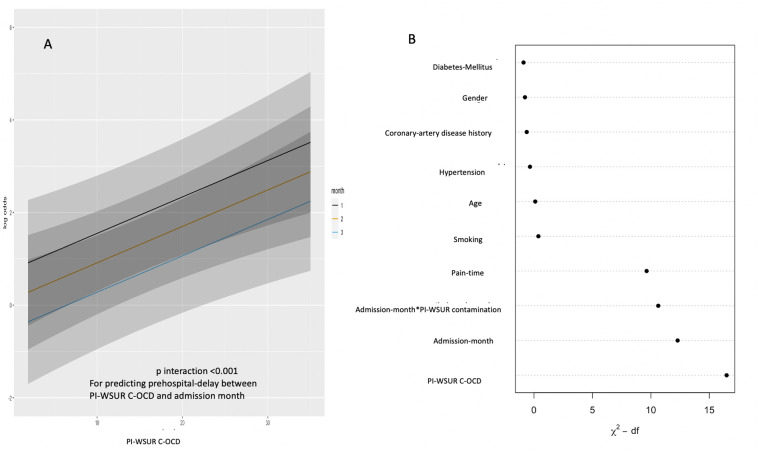
The performance of model 1, model 2, and model 3 is demonstrated in Table 3. Model 2 possessed the lowest BIC value, the highest likelihood X2 and Harrel C-index when compared with model 1 and model 3, indicating that it is the most accurate and straightforward model for predicting prehospital delay (lower BIC value, higher likelihood X2, and better Harrel C-index). In Fig. 2a, we manifested monthly changing PI-WSUR C-OCD score for predicting log-odds.
Fig. 2.
(A) interaction between month and PI-WSUR C-OCD:Padua inventory-Washington university revision Contamination obsessive compulsive disorder (B) Relative importance of each predictor in the model-2.
of prehospital delay. In Fig. 2b, we summarized the relative importance of each predictor in model 2. In Fig. 2a, we manifested monthly changing PI-WSUR C-OCD score for predicting log-odds of prehospital-delay. In Fig. 2b, we summarized the relative importance of each predictor in the Model-2.
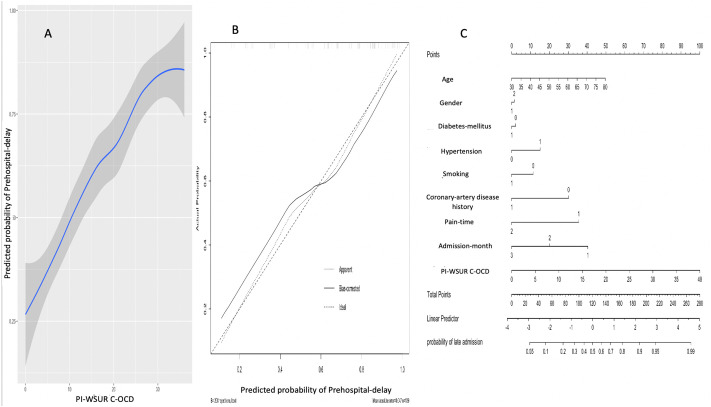
PI-WSUR-contamination was ranked as the most contributing predictor for the prehospital delay, and admission-month was the second contributing predictor. In Fig. 3a, the prehospital delay probability was plotted according to PI-WSUR C-OCD, which was adjusted with all parameters in the model 2 for the probability of prehospital delay.
Fig. 3.
(A) Probability of Prehospital delay was plotted according to PI-WSUR C-OCD: Padua inventory-Washington university revision Contamination obsessive compulsive disorder, (B) The corrected calibration (internal validation), (C) Nomogram for probability of prehospital delay.
The corrected calibration depicted a fair agreement with the apparent calibration; in our calibration plot, the mean absolute error was 0.047 and the quantile of error was 0.115 (Fig. 3b). This means that prehospital delay is underestimated if the probability is lower than 60% and overestimated if the probability is over 60% according to model 2. We generated a nomogram using variables in model-2 and variable coefficient in predicting the probability of prehospital-delay (Fig. 3c). As an example, 70 years-old, male, DM present, no HT, smoker, no CAD history, day-time applied patient involved in the first month and PI-WSUR C-OCD score 15, the result is 140 point, which means 65% probability to prehospital delay.
4. Discussion
We found a significant relationship between prehospital delay with PI-WSUR total and PI-WSUR C-OCD. Moreover, the results of this study showed that admission in the early period.
of the pandemic and higher PI-WSUR C-OCD score increased prehospital delay in patients with STEMI [(PI-WSUR OR 5.36 (2.11–13.61) (when PI-WSUR score increased from 8 to 27.5), (p interaction between admission month and PI-WSUR <0.001)] model 2. Prehospital delay duration was significantly longer in patients admitted in the first month than the third month (180 (120–360) IQR, 105 (60–180) IQR, respectively; P = 0.012) (Table1). OCD (with 3% prevalence in general population) may present with different clinical situations, often manifesting with the fear of being infected and cleaning habits [13]. During the COVID-19 pandemic, washing hands continuously to prevent the spread of infection along with staying away from public areas to avoid infection have made the OCD-like lifestyle a new normal lifestyle [19]. During the COVID-19 pandemic, with the change of hygiene recommendations and.
classical lifestyle according to these recommendations, an infrastructure has been prepared for the formation of C-OCD in the general society [20]. Parallel to this, in our study, PI-WSUR total score and PI-WSUR C-OCD were higher in the period of 20 March to 20 April compared to the period of 20 May to 20 June (37 (27–63) IQR, 25 (15–44) IQR, P = 0.045; 21 (11−32) IQR, 11 (5–24) IQR, P < 0.001, respectively) (Table-1). The effect of contamination fear on hospital admission time has been speculated in many studies, but it has not been studied comprehensively so far [[21], [22], [23], [24], [25], [26]]. As far as the researchers investigated, this is the first study which evaluates the association between contamination fear and prehospital delay during the COVID-.
19 pandemic.
Kadahat et al. demonstrated that the number of cardiac procedures decreased by 48% during the COVID-19 pandemic [21]. According to data from 73 centers in Spain, admissions with STEMI rates decreased by 40% compared to the period before COVID-19 pandemic [22]. In another study from the US, the number of STEMI patients decreased by 38% compared to former periods [23]. Furthermore, De Rossa et al. demonstrated that STEMI rates decreased by 26.5% compared to the previous year and STEMI mortality increased as well, the risk ratio (RR) was 3.3, 95% CI 1.7–6.6 compared to 2019 (P < 0.001) [27]. A recent study showed that out- of hospital cardiac arrest incidence significantly increased compared to the previous year [26]. Several studies have attempted to determine whether prehospital delays might be shortened by public education concerning ACS symptoms. A systematic review of 10 studies proposing to decrease prehospital delay times concluded that there was a little evidence that public education interventions reduced prehospital delay [28].
In a recent Twitter study by Kumar et al. in the period of March 17–30, 2020, the most perceived negative-opinion in social-media was “fear” when examining the perception of COVID-19 related content [5]. Also, we found a similar tendency in our study using the “gtrendr” package,
and “death” was the most searched word on the internet related to COVID-19 during the timeframe between 20 March-20 June 2020 [29]. STEMI patients may have avoided admission to the hospital due to the fear of COVID-19. Besides, Stella et al. found that STEMI decreased by 21%, and chest pain admission decreased up to 54% compared with the previous period [6]. This discrepancy is supported in another study in which they found significant increases in mortality from cardiovascular disease and other diseases during COVID-19 [7]. A nationwide registry in Turkey revealed an overall 47.1% decrease in the rate of acute MI admissions during the COVID-19 pandemic. Furthermore, this registry showed that admission time of the patients, who were directly admitted to the hospital, was 100 (90–550, IQR) minutes during the pre-pandemic period. However, it increased to 145 (70–303, IQR) minutes during the pandemic [8]. As the nationwide registry showed “door-to-balloon time” was not affected; similar to this finding, in our study, the “door to wire” duration did not change during different months. Our study showed that the most possible and strongest factor for explaining prehospital delay was C-OCD, and as Fig. 2 shows, this could be explained by the shift in the community behavior due to COVID-19 pandemic. The idea behind reduction in STEMI mortality is dependant on early reperfusion which is time dependant, risk modification, and strong antiplatelet therapy. However, during a pandemic, this idea was broken [13]. Using most of the available healthcare resources including human force to deal with the pandemic made it difficult to achieve early reperfusion goal [7,9].
Therefore, specific measures, such as increasing public awareness may reduce the fear of acquiring infection and mitigate the potential complications of STEMI during the COVID-19 pandemic. In the UK, the partial improvement in hospital admission rates by the end of May 2020 demonstrated that the British Heart Foundation publicity campaign in early April 2020, in which people with heart attack symptoms were encouraged to go to the hospital, could have helped to decrease such fears [9].
The similarity of decreases in STEMI admission rates, irrespective of age, sex, and comorbidities, depicts that our findings might be generalizable to all patients who are having an acute MI during a pandemic. Exploring potential predictive factors of prehospital delay for.
STEMI is important. As a result, our study recommends prehospital delay of STEMI should be closely monitored in order to prevent decline in admission trends and prehospital delay during any subsequent pandemic.
4.1. Strengths and limitations
One of the main strengths of this study is that it had a relatively long time and sample during the pandemic, and it was conducted in a percutaneous coronary intervention (PCI)-capable hospital. Hence, the results could be extended to other places with similar settings. Moreover we confirmed the accuracy of STEMI diagnosis by ECG, troponin, and angiography. Our study had also several limitations. First, we could not exclude the influence of patients recall bias for symptoms onset time. However, data were collected during the patient's admission within 48–72 h after symptoms onset. Another limitation is that survivor bias might exist as patients who were dead on arrival, or within 24 h of hospital arrival, were excluded. Another limitation is the single-center cross-sectional design of our study. The participants' low educational level may have influenced the measurement reliability due to the challenge in answering of the PI, BDI, and BAI questionnaire. Our results were affected homogeneously as no difference between our groups according to education level was observed. In addition, some factors in the BDI and BAI (dyspnea, fatigue, and insomnia) can be common in symptomatic applicants; therefore, the scores may not represent real depression or anxiety severity in patients with severe symptoms.
5. Conclusion
Our study confirmed that C-OCD was associated with prehospital delay of STEMI patients, but.
anxiety and depression level were not associated with prehospital delay during the pandemic. Efforts should be made in future to reduce prehospital delay during pandemics.
5.1. Main messages
The greater alteration in contamination obsession during Pandemic was associated with increased prehospital delay. The upward trend of contamination obsession change was significantly associated with increased prehospital delay. However, no significant association was seen between prehospital delay with anxiety and depression level among people with STEMI.
5.2. Current research questions
The value of contamination obsession on prehospital delay compared with other measurements.
during the COVİD-19 pandemic. Is there a difference in the relationship between admission month and prehospital delay?
5.3. What is already known on the subject
Prehospital delay is one of the modifiable prognostic risk factors for STEMI patients. Although it has been speculated in many studies, the effect of contamination obsession on hospital admission time has not been studied comprehensively so far.
Contributors
Conceptualization; A.K., B.Ke.,C.K., Data curation; A.K., H.C.T., Z.B., N.O., Formal analysis; A.K., C.D. S.C.E., N.O., C.K. Funding acquisition; NON-APPLICABLE Investigation; A.K., B.Ke., D.C., O.Y.A., N.O., C.K., Methodology; A.K., B.Ke., H.C.T, D.C., C.K., Project administration; A.K., B.Ke., C.K., Resources; NON-APPLICABLE., Software; A.K., H.C.T., Z.B., C.K., Supervision; A.K., B.Ke., C.D., D.C., O.Y.A., C.K., Validation; A.K., B.Ke., O.Y.A., C.K., Visualization; A.K., S.C.E., H.C.T., C.K., Writing - original draft; A.K., B.Ke.,Z.B., C.K., Writing - review & editing. ALL AUTHORS
Funding
The authors have not declared a specific grant for this research from any funding.
agency in the public, commercial or not-for-profit sectors.
Declaration of Competing Interest
None.
References
- 1.Szummer K., Jernberg T., Wallentin L. From early pharmacology to recent pharmacology interventions in acute coronary syndromes: JACC state-of-the-art review. J Am Coll Cardiol. 2019;74:1618–1636. doi: 10.1016/j.jacc.2019.03.531. [DOI] [PubMed] [Google Scholar]
- 2.Bueno H., Rossello X., Pocock S.J., et al. In-Hospital Coronary Revascularization Rates and Post-Discharge Mortality Risk in Non-ST-Segment Elevation Acute Coronary Syndrome. J Am Coll Cardiol. 2019;74(11):1454–1461. doi: 10.1016/j.jacc.2019.06.068. [DOI] [PubMed] [Google Scholar]
- 3.Szummer K., Jernberg T., Wallentin L. From Early Pharmacology to Recent Pharmacology Interventions in Acute Coronary Syndromes: JACC State-of-the-Art Review. J Am Coll Cardiol. 2019;74(12):1618–1636. doi: 10.1016/j.jacc.2019.03.531. [DOI] [PubMed] [Google Scholar]
- 4.Gruppo Italiano per lo Studio della Streptochinasi nell'Infarto Miocardico [GISSI] Effectiveness of intravenous thrombolytic treatment in acute myocardial infarction. Lancet. 1986;1:397–402. [PubMed] [Google Scholar]
- 5.Kumar A., Khan S.U., Kalra A. COVID-19 pandemic: a sentiment analysis [published online ahead of print, 2020 Jul 17] Eur Heart J. 2020:ehaa597. doi: 10.1093/eurheartj/ehaa597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stella F., Alexopoulos C., Scquizzato T., Zorzi A. Impact of the COVID-19 outbreak on emergency medical system missions and emergency department visits in the Venice area. Eur J Emerg Med. 2020;27(4):298–300. doi: 10.1097/MEJ.0000000000000724. [DOI] [PubMed] [Google Scholar]
- 7.Woolf S.H., Chapman D.A., Sabo R.T., Weinberger D.M., Hill L. Excess Deaths From COVID-19 and Other Causes, March–April 2020 [published online ahead of print, 2020 Jul 1] JAMA. 2020;324(5):510–513. doi: 10.1001/jama.2020.11787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Erol M.K., Kayıkçıoğlu M., Kılıçkap M., et al. Treatment delays and in-hospital outcomes in acute myocardial infarction during the COVID-19 pandemic: A nationwide study. Anatol J Cardiol. 2020;24(5):334–342. doi: 10.14744/AnatolJCardiol.2020.98607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mafham M.M., Spata E., Goldacre R., et al. COVID- 19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396 doi: 10.1016/S0140-6736(20)31356-8. 381–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ravi P.R. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr. 2020;52 doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ruscio A.M., Stein D.J., Chiu W.T., Kessler R.C. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15:53–63. doi: 10.1038/mp.2008.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Knowles K.A., Olatunji B.O. Anxiety and safety behavior usage during the COVID-19 pandemic: The prospective role of contamination fear [published online ahead of print, 2020 Oct 20] J Anxiety Disord. 2020;77:102323. doi: 10.1016/j.janxdis.2020.102323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ibanez B., James S., Agewall S., et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology [ESC] Eur Heart J. 2018;39(2):119–177. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 14.Goldberg R.J., Steg P.G., Sadiq I., Granger C.B., Jackson E.A., Budaj A., et al. Extent of, and factors associated with, delay to hospital presentation in patients with acute coronary disease [the GRACE registry] Am J Cardiol. 2002 Apr 1;89(7):791–796. doi: 10.1016/s0002-9149(02)02186-0. [DOI] [PubMed] [Google Scholar]
- 15.Kirchberger I., Heier M., Wende R., von Scheidt W., Meisinger C. The patient’s interpretation of myocardial infarction symptoms and its role in the decision process to seek treatment: the MONICA/KORA Myocardial Infarction Registry. Clin Res Cardiol. 2012;101(11):909–916. doi: 10.1007/s00392-012-0475-8. [DOI] [PubMed] [Google Scholar]
- 16.Beck A.T., Ward C.H., Mendelson M., Mock J., Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 17.Beck A.T., Epstein N., Brown G., Steer R.A. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 18.Burns G.L., Koertge S.G., Formea G.M., Sternberger L.G. Revision of the Padua Inventory of obsessive-compulsive disorder symptoms: Distinctions between worry, obsessions, and compulsions. Behav Res Ther. 1996;34:163–173. doi: 10.1016/0005-7967(95)00035-6. [DOI] [PubMed] [Google Scholar]
- 19.[Accessed October 14, 2020] https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cleaning-disinfection.html
- 20.McKay D., Minaya C., Storch E.A. Conducting exposure and response prevention treatment for contamination fears during COVID-19: The behavioral immune system impact on clinician approaches to treatment. J Anxiety Disord. 2020;74:102270. doi: 10.1016/j.janxdis.2020.102270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kadavath S., Mohan J., Ashraf S., et al. Cardiac Catheterization Laboratory Volume Changes During COVID-19 – Findings from a Cardiovascular Fellows Consortium [published online ahead of print, 2020 Jun 11] Am J Cardiol. 2020 doi: 10.1016/j.amjcard.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rodríguez-Leor O., Cid-Álvarez B., Ojeda S., et al. Impacto de la pandemia de COVID-19 sobre la actividad asistencial en cardiología intervencionista en España. REC Interv Cardiol. 2020;2:82–89. [Google Scholar]
- 23.Garcia S., Albaghdadi M.S., Meraj P.M., et al. Reduction in ST-Segment Elevation Cardiac Catheterization Laboratory Activations in the United States During COVID-19 Pandemic. J Am Coll Cardiol. 2020;75(22):2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pessoa-Amorim G., Camm C.F., Gajendragadkar P., et al. Admission of patients with STEMI since the outbreak of the COVID-19 pandemic. A survey by the European Society of Cardiology [published online ahead of print, 2020 May 28] Eur Heart J Qual Care Clin Outcomes. 2020;6(3):210–216. doi: 10.1093/ehjqcco/qcaa046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ferlini M., Andreassi A., Carugo S., et al. Centralization of the ST elevation myocardial infarction care network in the Lombardy region during the COVID-19 outbreak. Int J Cardiol. 2020;312:24–26. doi: 10.1016/j.ijcard.2020.04.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lai P.H., Lancet E.A., Weiden M.D., et al. Characteristics Associated With Out-of-Hospital Cardiac Arrests and Resuscitations During the Novel Coronavirus Disease 2019 Pandemic in New York City [published online ahead of print, 2020 Jun 19] JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.De Rosa S., Spaccarotella C., Basso C., et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;41(22):2083–2088. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kainth A., Hewitt A., Sowden A., et al. Systematic review of interventions to reduce delay in patients with suspected heart attack. Emerg Med J. 2004;21(4):506–508. doi: 10.1136/emj.2003.013276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.https://cran.r-project.org/web/packages/gtrendsR/gtrendsR.pdf