Abstract
Best-published evidence supports the combined use of vaccines with non-pharmaceutical interventions (NPIs), to reduce the relative risk of contracting severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that causes COVID-19; this will enable a safe transition to achieving herd immunity. Albeit complex, the strategic public health goal is to bundle NPIs to keep the basic reproduction number R0 below one. However, validation of these NPIs is conducted using random clinical trials, which is challenging in a swiftly moving pandemic given the need for recruiting large participant cohort over a longitudinal analysis period. This review highlights emerging innovations for potentially improving the design, functionality and improved waste management of disposable face masks such as filtering facepiece (FFPs) respirators, medical masks, and reusable face coverings to help prevent COVID-19. It describes use of different mathematical models under varying scenarios to inform efficacy of single and combined use of NPIs as important counter-measures to break the cycle of COVID-19 infection including new SARS-CoV-2 variants. Demand for face masks during COVID-19 pandemic keeps increasing, especially for FFPs worn by medical workers. Collaborative and well-conducted randomised controlled trials across borders are required to generate robust data to inform common and consistent policies for COVID-19 and future pandemic planning and management; however, current use of systematic reviews of best available evidence can be considered to guide interim policies.
Keywords: COVID-19, Face masks, Face coverings, Non-pharmaceutical interventions, Relative risk modelling, Sustainability
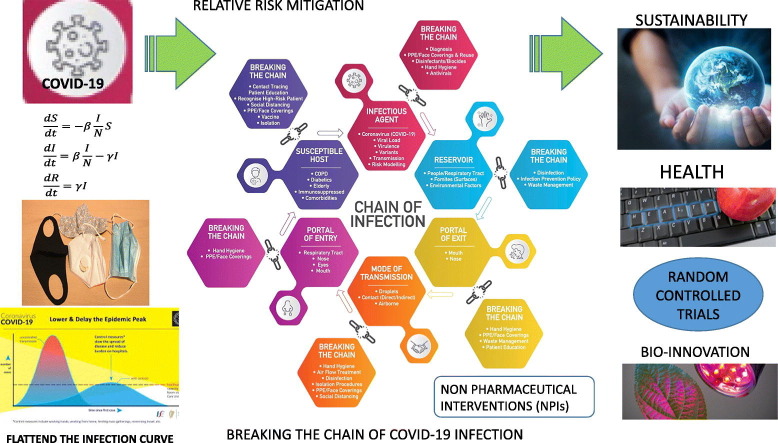
Graphical abstract
1. Introduction
At the time of writing (8th December 2020), there has been, 68,225,313, cases of coronavirus disease (COVID-19) reported worldwide, including 1,556,877 deaths (European Centre for Disease Prevention and Control, 2020). COVID-19 pandemic has imposed unprecedented challenges to healthcare systems (Chowdhury et al., 2020), where this respiratory-virus has spread to local communities globally. COVID-19 is primarily a respiratory disease and the spectrum of infection with this virus can range from very mild, non-respiratory symptoms to severe acute respiratory illness, sepsis with organ dysfunction and death (WHO, 2020a). Some people infected have reported no symptoms (WHO, 2020a). There is currently a 7-day average of 204,574 new cases of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the United States (Johns Hopkins University, 2020), which is the highest affected country for COVID-19. Several of these affected countries are experiencing peak infections rates, such as the United States, Russia and Turkey (Table 1 ). The occurrence of third waves of COVID-19 infection that affects greater numbers of people is common for many countries globally, which puts added pressure on deploying appropriate disease-prevention counter-measures.
Table 1.
Daily confirmed new cases of COVID-19 (7-day moving average) — outbreak evolution for the current 10 most affected countries (08/12/2020).
| Country | Population | 7-day mean average (K−1) for COVID-19 | Highest 7-day mean average (K−1) for COVID-19 | Total number of COVID-19 cases | Total number of COVID-19 deaths | Trend direction of COVID-19 cases in country | Days since first case of COVID-19 reported |
|---|---|---|---|---|---|---|---|
| United States⁎ | 331,002,651 | 204.574 | 204.574 | 14,949,299 | 283,703 | ⇑ Up | 320 |
| Brazil | 212,559,417 | 39.521 | 55.891 | 6,623,911 | 177,317 | ⇓ Down | 285 |
| India | 1,380,004,385 | 36.001 | 96,735 | 9,703,770 | 140,958 | ⇓ Down | 312 |
| Turkey⁎ | 84,339,067 | 32.736 | 32.736 | 860,432 | 15,103 | ⇑ Up | 271 |
| Russia⁎ | 145,934,462 | 28.701 | 27.701 | 2,466,961 | 43,122 | ⇑ Up | 311 |
| Italy | 60,461,826 | 20.709 | 37.977 | 1,742,557 | 60,606 | ⇓ Down | 311 |
| United Kingdom | 67,886,011 | 17.370 | 26.870 | 1,754,911 | 62,130 | ⇓ Down | 311 |
| Germany | 83,783,942 | 15.971 | 22.820 | 1,229,269 | 20,002 | ⇓ Down | 315 |
| Ukraine | 43,732,762 | 11.928 | 14.167 | 843,898 | 14,208 | ⇓ Down | 279 |
| Iran | 83,992,949 | 11.56 | 13.961 | 1,051,374 | 50,594 | ⇓ Down | 292 |
Data accessed from Johns Hopkins University on 8th December, 2020 (https://www.coronavirus.jhu.edu/data/new-cases).
Countries currently experiences peak number of cases of COVID-19.
Many countries are appealing for greater compliance with increased and correct wearing of face masks, maintaining social distancing, adopting hand hygiene, use of personal and protective equipment (PPE), along with detection testing and contact tracing that are also referred to as ‘non-pharmaceutical interventions’ (NPIs) (Rowan and Laffey, 2020a). The combined use of complementary NPIs are deployed to help flatten the curve of COVID-19 infections so as to particularly protect to our frontline healthcare workers (HCWs) and the most vulnerable in society (Rowan and Laffey, 2020a). For example, the WHO (2020a) stated “use of a mask alone is insufficient to provide an adequate level of protection, and other measures should be adopted”. The WHO (2020a) advises that each country apply their own risk based-approach when recommending different increasing tiers of NPIs including restrictive lockdowns, which also inflicts significant economic hardship on societies (Rowan and Galanakis, 2020). The emergence of COVID-19-related “behavioural fatigue” or “adherence fatigue” associated with sustained societal compliance with NPIs brings added public health pressures. Michie et al. (2020) described a Google search for “pandemic fatigue” that resulted in approximately 200 million hits, with articles on the first page with titles such as “10 reasons why pandemic fatigue could threaten global health”, and “Europe experiencing pandemic fatigue”.
Precisely how coronavirus spreads between susceptible individuals remains a matter of debate, but transmission of this respiratory virus may be through contact, droplet, or airborne spread (Asadi et al. 2020). “Direct” modes indicate person-to-person transmission such as via contaminated hands, or indirectly via fomites, which are inanimate or non-living objects or materials (i.e. transfer via a contaminated door handle through touch). If we touch a contaminated surface, we may then potentially transfer the virus onto the face mask if adjusting it, and may then directly inoculate the virus onto mucosal surfaces such as through the touching of the nose or eyes (Wibisono et al., 2020). Droplet and airborne spread occur through the air through sneezing, coughing, singing, talking and exhaling (Chua et al., 2020). It is appreciated that particles larger than 5 μm may fall to the ground within 1 m. However, a “gas cloud” theory has been proposed where aggregated mucosalivary droplets from these different exhalation activities can form a cloud, and potentially be expelled up to 7 to 8 m in combination with environmental factors (Bourouiba, 2020: Dbouk and Drikakis, 2020a, Dbouk and Drikakis, 2020b). Uncertainty surrounding the modes by which these respiratory viruses transmit among humans under varying conditions hinders evaluation of the efficacy of NPIs designed to prevent their spread (Milton et al., 2013; Perencevich et al., 2020).
The first COVID-19 vaccine, manufactured by Pfizer-BioNTech, was administered in the UK today (Diaz, 2020). Priority emphasis has been placed on protecting the most vulnerable to reduce illness and death. While Phase 3 clinical trial data highlights both safety and 95% efficacy for this vaccine, it will take time to observe if it prevents COVID-19 transmission and creates broad herd immunity in communities. Thus, despite this positive news, there will remain a strong reliance on the combined use of NPIs to prevent COVID-19 transmission. The Republic of Ireland has managed to curtail two waves of COVID-19 through effective implementation of these NPIs, along with enforcing two lockdowns (Government of Ireland, 2020); however, key challenges remain including greater mingling of people due to the opening up of hospitality that coincides with the festive Christmas holiday period. There is sustained pressure on maintaining supply chains of vital personal and protective equipment (PPE) to ensure that frontline healthcare workers, and the most at risk populations are protected (Rowan and Laffey, 2020b; Cook, 2020; Flaxman et al. 2020; Perencevich et al., 2020).
While there is priority emphasis on flattening COVID-19 infections to enable effective roll out of vaccines, there is a commensurate urgency to avoid economic chaos (Guan et al., 2020; Rowan and Laffey, 2020b). Many countries have tried to lift NPIs that has increased the occurrences and likelihood of disease resurgence (Chowdhury et al., 2020). Ensuring continuity in the supply chain for vital personal and protective equipment (PPE) has been a significant challenge that has been met, where possible, by increased production of single-use plastic PPE along with initiatives to safely address their reuse under emergency use authorization (Rowan and Laffey, 2020b). Given the initial gap in knowledge on specific efficacy of existing and emerging counter-measures to combat COVID-19, there has been a commensurate surge of new publications on PPE and other NPIs to meet these public health needs that also has implications for sustainable waste management (Silva et al., 2020). For example, recently research and systematic reviews on these topics approximate 20,000 publications since the first reporting of COVID-19 (such as Silva et al., 2020; Derraik et al., 2020; Rowan and Laffey, 2020a; Rubio-Romero et al., 2020; Chu et al., 2020; Barceló, 2020).
“Face masks are physical barriers to respiratory droplets that may enter the mouth and nose and to the expulsion of mucosalivary droplets from infections individuals” (Chua et al., 2020). The classification of, and technical standards for, different type of disposable masks available according to their intended use, as defined by the European Centre for Disease Prevention and Control (2020), has been comprehensively described by Rubio-Romero et al. (2020). In brief, (a) filtering facepiece (FFP) respirators are classified as PPE and are designed to protect the wearer from exposure to airborne contaminants, such as N95-type respirators; (b) medical face masks (also known as surgical or procedural masks), are classified as a medical device that covers the mouth, nose and chin ensuring a barrier that limits the transition of infective agent between hospital staff and patients; and (c) other face masks (also commonly known as non-medical, home-made cloth or barrier masks) includes various forms of self-made or commercial masks, or face coverings, made of cloth or textiles that are not standardized and not intended for use in healthcare settings (Rubio-Romero et al., 2020) (Fig. 1 ). The effectiveness of these disposable FFP masks is different depending on type and certification, which is established across 3 levels of protection depending on leakage of all particles into the interior, either through the adjustment of the mask to the face, by the exhalation valve, if any, or penetration through the filter that are 22%, 8% and 2% for FFP1, FFP2 and FFP3 respectively. The effectiveness of two types of medical masks, namely surgical or procedural masks, is defined by bacterial filtration efficiency, differential pressure (Pa/cm2), splash resistant pressure (kPa) and microbial cleaning. Improvised non-medical face coverings are intended for low-risk cases where the risk of infection can be potentially increased due to humidity, liquid diffusion and virus retention (European Centre for Disease Prevention and Control, 2020b).
Fig. 1.
Examples of disposal face masks and reusable cloth face covering: (a) KN95-type filtering face piece mask, (b) medical or procedural mask, and (c) non-medical reusable cloth face covering.
Given the aforementioned, the purpose of this review is (1) to highlight key developments surrounding sustainable use of disposable face masks such as PPE, medical masks, and reusable face coverings; (2) to review the role of face masks in the context of other NPIs in breaking the cycle of COVID-19 infection, and; (3) to use relative risk assessment and statistical modelling to inform efficacy of single, and combined NPIs to prevent COVID-19 transmission with particular emphasis on different face mask designs and functionality features. This review does not address non-disposable filtering facepiece (FFP3) respirators.
2. Transmission and survival of SARS-CoV — breaking the chain of infection
2.1. Characteristics of SARS-CoV-2 and survival of contact surfaces
SARS-CoV-2 is a Coronavirus, which is characterised as a positive stranded RNA virus with an envelope containing glycoprotein spikes. Coronaviruses are among the largest RNA viruses comprising a genome of between 26 and 32 kb in size (Jin et al., 2020), and ranges from 60 to 140 nm in size (Chua et al., 2020). Therefore, “face masks and respirators made of materials with larger pore sizes, such as cotton and synthetic material, will not be able to effectively filter these viruses or virus-laden droplets, as compared with those materials with much smaller pore smaller pore sizes”. Additionally, face masks and respirators made of, or coated with, water-resistant materials are more effective against large virus-laden respiratory droplets” (Chua et al., 2020). Coronaviruses, such as SARS-CoV-2 comprise complex structural enveloped viruses and it is this complexity that attributes to its sensitivity to popular disinfectants and biocides (Rowan and Laffey, 2020b; Kampf et al., 2020; Van Doremalen et al., 2020). Researchers have reported that the use of conventional disinfectants and biocides inactivate SARS-CoV-2 by disrupting the lipid-containing viral envelope, the capsid, and the genome (Dev Kumar et al., 2020). Indeed, compared to that of naked viruses, enveloped viruses, such as SARS-CoV-2, are generally more sensitive to conventional disinfection strategies and at similar dosages. Thus, in this case, the evolution of greater complexity at the cost of vulnerability can be readily exploited in mitigation approaches (Pinon and Vialette, 2018).
The emergence of SARS-CoV-2 variants in the UK (Volz et al., 2021) and South Africa (WHO, 2020b) may influence viral transmissibility, and possibility pathogenicity. However, it is unlikely that the multiple mutations observed in SARS-CoV-2 variants alternating outer surface spike proteins will impact on efficacy of commonly-used disinfection, or penetrating face masks, given that these mutations lead to minor morphological changes to what is still a large enveloped coronavirus from a destructive or preventative perspective. However, an evaluation of variant analysis of SARS-CoV-2 to ensure efficacy of NPIs are merited in order to comprehensively establish same (Koyama et al., 2020). Previous studies have highlighted the importance of the outer lipid membrane in rendering enveloped viruses more susceptible to naked viruses when using disinfectants (Rotter, 2001; Figueroa et al., 2017; Kampf, 2018; Blázquez et al., 2019). WHO (2020b) noted that previous reports of the D614G mutation, and the recent reports of virus variants from the Kingdom of Denmark, the United Kingdom of Great Britain and Northern Ireland, and the Republic of South Africa have raised interest and concern in the impact of viral changes. Moreover, the WHO (2020b) stated “Over a period of several months, the D614G mutation replaced the initial SARS-CoV-2 strain identified in China and by June 2020 became the dominant form of the virus circulating globally. Studies in human respiratory cells and in animal models demonstrated that compared to the initial virus strain, the strain with the D614G substitution has increased infectivity and transmission. The SARS-CoV-2 virus with the D614G substitution does not cause more severe illness or alter the effectiveness of existing laboratory diagnostics, therapeutics, vaccines, or public health preventive measures”. Given greater transmissibility of SARS-CoV-2 variants, there is likely to be enhanced pressure on supply chain for personal and protective equipment such as filtering face-piece respiratory (FFR) masks, and stricter adherence to NPIs.
Current evidence shows that disinfectants, such as use of 70% (v/v) alcohol, are effective for hand sanitation and for fomite disinfection (Dev Kumar et al., 2020; Van Doremalen et al., 2020; Kampf et al., 2020). Moreover, several authors are reported on the viability of SARS-CoV-1 and SARS-CoV-2 on different surfaces, such as printed paper, tissue, wood, glass, banknotes, plastic, stainless steel, surgical masks layers under a variety of temperature and relative humidity (RH) conditions (Pagat et al., 2007; Behzadinasab et al., 2020; Chan et al., 2020; Derraik et al., 2020).
In general, SARS-CoV-2 is inactivated on surfaces within 4 days at ambient room temperatures, depending upon the viral load and presence of organic matter or soiling. For example, Chin et al. (2020) used medium tissue culture infective dose (TCID50) to report reductions of ≥4.5 log10 for SARS-CoV-2 at room temperature (22 °C, 65% RH) and 37 °C after 14 and 3 days respectively. However, Riddell et al. (2020) measured the survival rates of SARS-CoV-2, suspended in a standard ASTM E2197 matrix, and reported that using initial viral loads broadly equivalent to the highest infectious patients, viable virus was isolated for up to 28 days at 20 °C from common surfaces, such as glass, stainless steel, and both paper and polymer banknotes. This highlights the importance of using hand hygiene and surface disinfection and to avoid touching the outer layer of face masks during the COVID-19 pandemic.
Chin et al. (2020), and other (Chan et al., 2020) highlighted much longer persistence of SARS-CoV-2 on surfaces under colder or refrigeration temperatures (4 °C), where the virus was only reduced by 0.7 to 2 log10 after 14 days. The soiling of face masks and coverings, such as potentially touching the outer surfaces where fingers are coated with natural oils, and possibly with SARS-CoV-2 if contaminated, may contribute to viral persistence. For example, Kasloff et al. (2020) simulated typical infectious body fluids of infective patients and showed that to achieve a 5 log10 reduction of SARS-CoV-2 at room temperature (20 °C), it took 14 days on nitrile gloves, and survival up to 21 days on plastic face shields, N100 filtering facepiece respirators (FFRs) and polyethylene overalls. Some residual SARS-CoV-2 infectivity was evident from the artificially-inoculated FFRs after 3 weeks. Chin et al. (2020), using non-soiling studies, reported that SARS-CoV-2 exhibited residual infectivity on the inner and outer layers of surgical masks after 7 days where there were ≥4.8 log10 and 3 log10 reductions in viral load respectively. Fischer et al. (2020) noted ≥4 log10 reduction (TCID50/mL) on SARS-CoV-2 inoculated N95 respirator and stainless steel respirator disks after 24 h and 48 h respectively when held at 21–23 °C, 40% RH. These observations may have implications for longer survival of SARS-CoV-2 when suspended in aerosols or on contact fomite surfaces (such as face coverings), given the transition to the colder winter season in the Northern hemisphere.
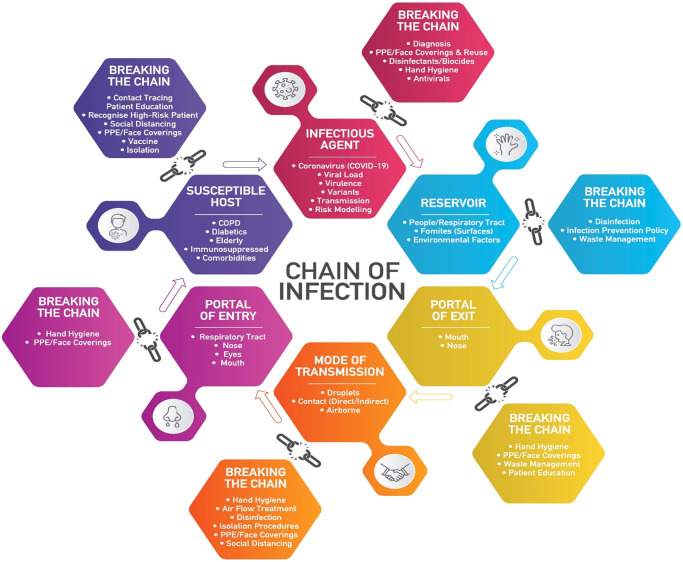
2.2. Breaking the chain of infection in the context of non-pharmaceutical interventions (NPIs) to address COVID-19
Adopting key principles of conventional infection control practices has proven effective against COVID-19, namely, breaking the chains in the infection cycle in at risk settings including use of non-pharmaceutical interventions (NPIs) (Fig. 2 ). In the context of this infection cycle (Fig. 2), the “infectious agent” is the pathogen, such as SARS-CoV-2, which causes diseases that can be influenced by level of virus or load, transmissibility and virulence of viral variants. The “Reservoir” includes places in the environment where the pathogen resides, such as people, contact surfaces (door handles, and medical equipment (stethoscope, thermometer), where persistence can be influenced by presence of organic matter and environmental factors (temperature, relative humidity). For example, Rowan (2019) reviewed the disruptive potential of pulsed light technology to disinfect contaminated surfaces in healthcare to prevent disease transmission. “Portal of exit” is the way the infectious agent leaves the reservoir, such as through open aerosols, and splatter of body fluids including coughing, sneezing, and saliva (WHO, 2020a). “Mode of transmission” is the means by which the infectious agent can be passed on, such as through direct or indirect contact or by inhalation (WHO, 2020a). There is also the possibility of transmission from people who are infected and the shedding virus, but have not yet developed symptoms; this is called pre-symptomatic transmission (Arons et al., 2020). Lee et al. (2020) quantitatively evaluated SARS-CoV-2 molecular shedding among 303 patients in a community treatment centre in Cheonan, Republic of Korea; of those initially considered asymptomatic, 89 (about 30%) remained healthy throughout the study. Twenty-one others went on to develop symptoms of the virus. The incubation period for COVID-19, which is the time between exposure to the virus and symptom onset, is on average 5–6 days, but can be as long as 14 days (WHO, 2020a). “Portal of entry” is the way the infectious agent can enter a new host, such as, the respiratory tract, mucous membranes or contaminated personal and protective equipment (PPE) (WHO, 2020a). “Susceptible host” can be any person, but the most vulnerable are those who are immune-suppressed or have comorbidities or an aging immune system (elderly) (WHO, 2020a; Murphy et al., 2020). Fig. 2 highlights the important role of NPIs, (such as PPE, face coverings), in breaking multiple inter-connected links in the infection cycle that will prevent COVID-19 transmission.
Fig. 2.
Breaking the chain of COVID-19 infection: contributions of different NPIs.
The main modes of SARS-CoV-2 transmission is through suspension in virus-laden aerosols or droplets that are typically liberated through the nose and mouth of infected spreaders. Airborne spread occurs with pathogens found in exhaled droplets <5 μm in diameter (Chua et al., 2020); where it is generally thought that SARS-CoV-2 can be transmitted in exhaled particles smaller or larger than 5 μm (Leung et al., 2020). A greater risk of SARS-CoV-2 transmission is appreciated through talking, singing, coughing and sneezing where the aerosolised virus can remain airborne due to low sedimentation velocity; thus, highlighting the importance of maintaining a 2 m (6.6 ft) social distancing and the wearing of face masks (WHO, 2020a). The further the distance apart from an infected SARS-CoV-2 spreader, the lower the relative risk of acquiring SARS-CoV-2, such as from airborne aerosols and droplets. Using laser light scattering, Anfinrud et al. (2020) found that there were average emissions of about 1000 droplet particles per second speech, with high emission rates of up to 10,100 droplet particles per second. Stadnytsky et al. (2020) estimated that 1 min of loud speaking generates greater than 1000 droplets containing virus; this was calculated by fitting the time-dependent decrease in particle detected to exponential decay. Chu et al. (2020) conducted a systematic review and meta-analysis of 172 observational studies and found that there is a 12.8% chance of contracting COVID-19 with physical distancing measures of less than 1 m, but this falls to just 2.6% with a distance of 1 m or more. The WHO (2020a) stated that “Droplet transmission occurs when a person is in close contact (within 1 m) with an infected person and exposure to potentially infective respiratory droplets occurs, for example, through coughing, sneezing or very close personal contact resulting in the inoculation of entry portals such as the mouth, nose or conjunctivae (eyes)”. This emphasizes the challenges of mitigating transmission of SARS-CoV-2 in the indoor environment as there is a higher risk of viral exposure with the close congregation of potential viral spreaders, and there is limited ability for air treatment or exchange. Thus, improving behavioural change, such as avoiding complacency, when using face masks and face coverings to ensure that both the nose and mouth are kept covered will be beneficial (Rowan and Laffey, 2020b).
SARS-CoV-2 is spread through infectious aerosols (Asadi et al. 2020). Beldomenico (2020) also proposed that superspreaders play an important role in the spread of SARS-CoV-2. The potential variance in individuals to spread SARS-CoV-2 may also explain apparent differences between studies that typically report on low secondary attack rates with homes (11.2% in one Chinese study (Bi et al., 2020) and attack rates in specific clusters of transmission, such as the Skagit County choir where 87% of attendees were affected by one individual (Hamner et al., 2020). Kenyon (2020) highlighted the complexity of quantifying relative risk (RR) for susceptible individuals as there is increasing evidence that a large proportion of SARS-CoV-2 transmissions occur whilst the transmitters have low or no infection (Arons et al., 2020). Thus, it is also increasingly recognised that asymptomatic infected individuals, or symptomless spreaders, may also effectively cross-infect other susceptible people with SARS-CoV-2 (Asadi et al., 2020a, Asadi et al., 2020b; Arons et al., 2020), which supports the need for wearing of face masks and improvised face coverings and to follow additional nonpharmaceutical mitigation strategies. However, Perencevich et al. (2020) highlighted that no studies have evaluated the effects or potential benefits of face shields on point source control (i.e., containing a sneeze or cough), when worn by asymptomatic or symptomatic persons. These authors also noted that major recommendations should be evaluated using clinical studies, but it is unlikely that a randomised trial has been conducted to verify efficacy due to restricted time associated with fast moving pandemic conditions; thus, with the introduction of new vaccines, many future randomised control studies that focus on efficacy of NPIs may be retrospective in nature. The type and degree of non-pharmaceutical strategies applied are influenced by the perceived severity of the relative risk; for example, full PPE should be worn in a high-at-risk healthcare setting, such as ICU (Rowan and Laffey, 2020b). Whereas wearing improvised cloth face coverings, hand-sanitation and social distancing are used for lower relative risk community settings. However, the relative contribution of each of these transmission modes remains uncertain, and variance in viral, host, or environmental factor is likely to influence which modality is favoured in different settings (Tellier et al., 2019; Asadi et al., 2020b).
2.3. Aerosol and non-aerosol generating procedures: the role of face mask and face covering including design, features, characteristics and maintenance
Medical masks should be certified according to international and national standards to ensure they offer predictable product performance when used by HCWs, according to the risk and type of procedure in a healthcare setting (WHO, 2020a; Rubio-Romero et al., 2020). “Defined for single use, a medical masks' initial filtration (at least 95% droplet filtration), breathability, and if required, fluid resistance are attributed to the type (e.g. spunbond or meltblown), and layers of manufactured non-woven materials (e.g. polypropylene, polyethylene or cellulose)” (WHO, 2020a). Recent theories suggest that SARS-CoV-2 can also be transmitted by attachment to particles or dust that have been from contaminated surfaces, which have been recently designated as “aerosolized fomites” (Asadi et al., 2020a, Asadi et al., 2020b). This, if true, further strengthens the importance of wearing face masks and coverings to prevent infection. The scientific community has been discussing whether the COVID-19 virus, might also spread through aerosols in the absence of aerosol generating procedures (AGPs) (WHO, 2020a). This is an area or active research. It is noteworthy, that the presence of viral RNA is not the same as replication- and infection competent (viable) virus that could be transmissible and capable of sufficient inoculum to initiate invasive infection. High quality research, including randomised trials in multiple settings, are required to address many of the acknowledged research gaps related to AGPs and airborne transmission of the COVID-19 virus (WHO, 2020a). The global spread of COVID-19 has substantially increased the demand for face masks worldwide that has accelerated research and innovation surrounding their efficacy (Rowan and Laffey, 2020a). In general, the term “face mask governs a broad range of protective equipment with a primary function of reducing the transmission of particles or droplets” (Fischer et al., 2020). Fischer et al. (2020) tested 14 commonly available masks, or mask alternatives that included improvised face coverings, using a simple yet cost-effective optical measurement method to evaluate the efficacy of masks to reduce the transmission of respiratory droplets during regular speech. Improvements in preventing droplet transmission was evident using increased layers of cotton-polypropylene and pleats compared to fitted N95, while neck gaiters or bandanas offered very little protection. Fischer et al. (2020) also observed a significant increase in relative droplet count when the N95 respirator was fitted with a value.
The WHO (2020a) have provided comprehensive guidance on use of masks and improvised fabric face coverings in the context of the COVID-19 pandemic. New guidance is provided on non-medical (also referred to as “fabric”) mask features and characteristics, including choice of fabric, number and combination of layers, shape, coating and maintenance. “Masks can be used either for protection of healthy persons (worn to protect oneself when in contact with an infected individual) or for source control (worn by an infected individual to prevent onward transmission). However, the use of a mask alone is insufficient to provide an adequate level of protection or source control, and other personal and community level measures should also be adopted to suppress transmission of respiratory viruses. Whether or not masks are used, compliance with hand hygiene, physical distancing and other infection prevention and control (IPC) measures are critical to prevent human-to-human transmission of COVID-19” (WHO, 2020c). While non-medical masks may be made from different combinations of fabrics, layering and are available in diverse shapes; however, few of these combinations of fabrics and materials have been systematically reviewed for filtration and breathability. A non-medical mask standard has been developed by the French Standardization Association (AFNOR, 2020) to define minimum performance in terms of filtration (minimum 70% solid particle filtration or droplet filtration), and breathability (maximum pressure difference of 0.6 mbar/cm2 or maximum inhalation resistance of 2.4 mbar and maximum exhalation resistance of 3 mbar. It is noted that the lower filtration and breathability standardized requirements and overall expected performances, should be considered for source control (used by infected persons) in community settings, and not for prevention. WHO (2020c) recommended that they can be used ad-hoc for specific activities where social distancing cannot be maintained, and their use should be accompanied to hand hygiene and physical distancing. Dbouk and Drikakis, 2020a, Dbouk and Drikakis, 2020b described a computational fluid dynamic model that takes into account turbulent dispersion forces, droplet phase-change, evaporation, and breaking up in addition to droplet-droplet and droplet-air interactions, mimicking reave events by using data that closely resemble coughing (Table 2 ). The study showed that criteria employed for assessing face mask performance requires modification to take into account the penetration dynamics and airborne droplet transmission, the fluid dynamics leakage around the filter, and reduction of efficiency during cough cycles. The study proves that use of masks reduce airborne droplet transmission, and will protect the wearer from contaminated droplets; however, many droplets still spread around and away from the mask cover (Table 2). Therefore, use of a mask does not provide full protection and social distancing remains important during the pandemic.
Table 2.
Published studies on new face mask design, functionality and sustainability factors to help address supply chain shortage and improvements in waste managements presented by ongoing COVID-19 pandemic.
| Innovations | Main development(s) | Citing reference(s) |
|---|---|---|
| Computational fluid dynamics for face mask filter efficacy | Face mask filters – textile, surgical or respiratory – understanding of droplet dynamics through and around a face mask filters resembling cough many – new criterion for calculating mask efficiency to consider penetration dynamics proposed – masks do not provide complete protection | Dbouk and Drikakis, 2020a, Dbouk and Drikakis, 2020b |
| Air dispersion distances through patient simulator | Normal cough induces turbulent flow that spreads about 70 cm from the subject – N95 mask prevented air leakage than surgical mask during coughing. But there remains sideway leakage. | Hui et al., 2012 |
| Forward jet of droplets and leakage around mask – droplet transmission | Using the Schlieren optical method, it was shown that wearing a standard surgical mask blocks the forward jet of droplets, but allows leakage around the top, bottom and sides. N95 reduces the droplet leakage around mask edges during coughing – none of the masks entirely prevented penetrating or escaping the mask – i.e., droplet transmission. | Tang et al., 2009 |
| Self-designed triple-layer cotton masks to suppress respiratory droplet levels | Self-designed triple-layer cotton masks worn by respiratory infected person (influenza and COVID-19 participants) were shown to be similar to medical masks for suppressing droplet levels in regular bedroom and a car with air conditioning where cough/sneeze counts were measured | Ho et al. (2020) |
| Face masks with respiratory valve had lower exchange rate of breathing assistance | Studies to evaluate and characterize the comfort sensation and performance of 12 types of face masks (related to shape, respiratory valve, brand, main materials and protection level) related to breathing assistance for healthcare in fog and haze weather [non-COVID-19] – dynamic changes in airflow rate and breathing resistance were acquired by virtual instrument system- cotton mask had lower rate of breathing assistance than nonwoven fabric masks. | Yao et al., 2019 |
| Mask face detection based on a hybrid AI, deep transfer learning and classic machine learning model | Use of Artificial Intelligence (AI), deep transfer learning and classic machine learning to evaluate mass usage of face masks to potentially inform protection and compliance during COVID-19. Researchers used three data sets: Real-World Masked Face (RMFD) consisting of images of 5000 masked faces and 90,000 unmasked faces; Simulated Masked Face Dataset (SMFD) with 785 for simulated masked faces and 785 for unmasked faces; Labelled Faces in the Wild (LFW) containing 13,000 masked faces of celebrities. Focus was in training for accuracy of face mask detection. | Loey et al., 2021 |
| Use of spray-simulation method (mimicking a sneeze) along with germ-free mice | Development and validation of spray-simulation method (mimicking a sneeze) for determining efficacy of combed-cotton textiles used as two-layer barriers for protecting germ-free mice from bacteria carrying droplets. Authors used aqueous suspension of 12 probiotic-cultured dairy bacteria – authors advocated use of bacteria as they exist in association with respiratory viruses in respiratory fluids – they also used bacteria to quantify number of droplets that escape textile barrier | Rodriguez-Palacios et al., 2020 |
| Surgical and homemade masks, even without fitting, reduces particles emitted via breathing, talking, and coughing | Wearing of surgical masks, or N95 respirators, even without fit-testing, reduces number of emitted expiratory particles from breathing, talking, and coughing from experimental studies. But, efficacy of wearing homemade cloth or paper masks is less clear, and confounded by shedding of masks fibres, with some reductions observed, particularly for larger particles (>0.5 μm). Authors did not measure virus-laden aerosols and droplets, but observations consistent that wearing mask can help with mitigating pandemic-associated with respiratory disease. | Asadi et al., 2020a |
| Bio-based facemasks – use of electrospinning gluten and carbonization | Suggested sustainable future-use of wheat gluten biopolymer, a by-product of cereal industries, as alternative to using petrochemicals for reusable facemask. Fine mesh nanofilter membrane structure to be achieved via electrospinning and subsequent carbonization at over 700 °C. | Das et al., 2020 |
| Design, velocity and fitness innovation for sustainable face masks including home made | Understanding performance of commercial masks and Advantages of wearing commercial and home-made face coverings during pandemic. Review of masks made from household materials. Limited studies that used randomised control trials for investigating efficacy of cloth masks showing that they are not suitable for HCWs. | Davies et al., 2013; Chughtai et al. (2013); Chua et al., 2020 |
| Cloth masks loose filtration efficacy after frequent washing and drying cycles. | Studies on the effect of washing and drying on cloth mask highlighted a drop in filtration performance that was correlated to pore size and shape of the masks. It was found that the PM10 filtration efficiency dropped by 20% after 4th washing and drying cycle, that was attributed to continuous stretching of the masks, enlarging the pore size, thus impairing mask performance. | Neupane et al., 2019 |
| Engineering multifunctional face masks | Increasing trend for published information that highlights innovation to improve filtering capacity (such as pore size) of mask materials and improving additional functions in terms of design (such as antimicrobial properties, coatings) to enhance user comfort, and convenience (such as introduction of self-cleansing and sensing properties. However, these are laboratory studies. | Chua et al., 2020 |
| Increased super hydrophobicity and transparent qualities of masks materials | Graphene-coated masks shown to exhibit significant superhydrophobic and photothermal performance that can repel incoming aqueous droplets masks exposed up to 80 °C under sunlight illumination can achieve self-sterilisation. Transparent properties included on face masks to improve quality for the hearing impaired such as digital face recognition, human-facing industry. | Son et al., 2020; Zhong et al., 2020; Chua et al., 2020 |
| Differences in FFE for head tie, ear-loop face masks | 29 different face masks alternative including expired N95 respirators with intact elastic straps and respirators subjected to ethylene oxide or VH2O22 sterilisation – procedural face masks with elastic ear loops showed lowest fitted filtration efficacy at 38.1%. Thus, highlighting increased risk. | Sickbert-Bennett et al., 2020 |
The WHO (2020c) recognises that many countries have recommended the use of fabric masks/face coverings for the general public, but also recognises that the widespread use of masks by healthy people in the community is not yet supported by high quality or direct evidence where there are potential benefits and harms to consider. The WHO advises decision-makers to apply risk-based approaches when encouraging the use of for the general public to include, (1) purpose of mask use, (2) risk of exposure to the COVID-19 virus, (3) vulnerability of the mask wearer/population, (4) setting in which the population lives, (5) feasibility, such as availability and cost of masks, and ability of mask wearer to tolerate adverse effects of wearing a mask, and (6) type of mask, such as medical versus-non-medical mask. Examples of where the general public should be encouraged to use medical and non-medical mask in areas with known or suspected community transmission.
2.4. Reprocessing and extended use of PPE and face coverings to meet supply chain shortfall in the context of COVID-19 pandemic
There has been a commensurate interest in reuse of PPE in healthcare, particularly important filtering facepiece respirators (FFRs), such as N95 respirators, to meet supply chain shortages during COVID-19 pandemic (Rowan and Laffey, 2020a; Rubio-Romero et al., 2020). This need for potential extended or reuse of FFRs is likely to be remain beyond COVID-19 given sustained concerns by clinicians and healthcare workers, along with meeting the surge in patients attending health screening (non-COVID-19 related) and requiring medical procedures. Several countries have adopted PPE reuse through reprocessing technologies that address fit testing post treatments along with disinfection and filtration efficacy (Rubio-Romero et al., 2020). A comprehensive review of efficacy and usage of face masks has been conducted by Rubio-Romero et al. (2020). Given the heat sensitivity and complexity of materials used in single-use PPE, only a limited number of reprocessing technologies have been authorized for their emergency reuse by the FDA, such as using hydrogen peroxide in vapor form (30–35% VH2O2) used alone or combined with ozone (FDA, 2020; Rowan and Laffey, 2020a). McEvoy and Rowan (2019) provided an informative and comprehensive review on the use of VH2O2 in the adjacent area of terminal sterilisation of medical devices. Countries are also pursing use of ultra-violet germicidal irradiation technologies (UV dose 2000 μJ/cm2) (Derraik et al., 2020), but there remains uncertainty surrounding the efficacy of this 2-dimensional irradiation to penetrate complex filtration system associated with FFRs (Rowan and Laffey, 2020b). Use of conventional moist heat at 60 °C (60 min, at high humidity), is also potentially efficacious for safe PPE reprocessing (Derraik et al., 2020; Rowan and Laffey, 2020b).
A limiting factor in harmonized reprocessing of PPE will be the availability of sophisticated technologies, such as VH2O2, to meet unprecedented high demand during COVID-19 pandemic (Rowan and Laffey, 2020a; Ilyas et al., 2020). Decisions underpinning PPE reuse are likely to be governed by infection prevention groups in healthcare, in consultation with competent regulatory authority for each country, where critical shortages in supply chain will inform deployment in order to protect frontline healthcare workers (HCWs). However, lack of acceptance by HCWs for the use of reprocessed PPE might be a barrier to general deployment, which can be potentially addressed through education, training and social marketing to highlight efficacy and safety. PPE supply chain shortfalls have been primarily met by enhanced production by original equipment manufacturers (Rowan and Laffey, 2020b). In addition, initiatives and collaborations performed by companies, hospitals, and researchers in utilising 3D printing during the COVID-19 pandemic has contributed to this effort to address supply chain shortfalls in face shields (Tino et al., 2020). Homemade and commercial cloth or fabric face coverings are less complicated, and can be effectively reprocessed by moist heat combined with using a detergent (60 °C for 30 min), such as using a domestic laundry machine combined with spin drying (Rowan and Laffey, 2020a). Face shields are used without a mask, they should wrap around the sides of the wearer's face and extend below the chin. It was recently reported that only those wearing face shields at a Swiss hotel succumbed to COVID-19, where no reported cases occurred for staff and guests who wore face masks in the same hotel. The WHO (2020c), and other authorities, have advised that face shields can offer an added layer of protection, but in addition to a face mask, social distancing, and handwashing, not as a substitute.
2.5. Innovation surrounding face mask design and functionality for future sustainability
Best available evidence supports the effective use of face masks as nonpharmaceutical counter-measures for addressing COVID-19 (Wang et al., 2020a); where there has been advancements on the reprocessing of single-use face masks under Emergency Use Authorisation (Rowan and Laffey, 2020a). However, published evidence shows that masks do no provide 100% protection (Wang et al., 2020b), with significant variance depending on the filtration efficiency and design. There has been a surge in innovation to improve face mask design, comfort, functionality and sustainability, such as improvements in recycling and medical waste management (Table 2). Despite well-conducted studies, there is a pressing need to extensively test and validate these new innovations through regulated multi-actor, collaborating, randomised controlled trials.
Mask efficiency is defined as percentage of a contaminant removed by a mask filter, where mass, weight, number of particles, or volume can quantify this performance (Hutten, 2016) (Table 2). Typically, certification standards (ASTM F1862M-17, 2017; ASTM F201-19, 2019) usually define a surgical mask efficiency as a standard value independent of coughing incidents or cycle. However, Dbouk and Drikakis, 2020a, Dbouk and Drikakis, 2020b noted that these standards neglect fluid flow dynamics effects and droplet leakage through mask openings. Additionally, there is no consideration that mask efficiency can deteriorate considerably over time due to saturation effects; thus, coughing and fluid dynamics need to be considered in calculating fluid efficiency. The main mechanisms of filtering through masks are droplet diffusion, interception and impaction. Also, the frequency of coughs may further challenge efficiency. Continued, or cyclic coughing, increases dynamic flow that can negatively affect efficacy of mask filter performance where a wide range of filter efficiencies have been described (Rengasamy et al., 2010). Previous studies reported that use of surgical masks effectively reduce emission of large droplets and minimize lateral dispersion of droplets (Driessche et al., 2015; Stockwell et al., 2018).
Ho et al. (2020) reported that self-designed triple-layered cotton masks worn by respiratory infected volunteers were similar to participants wearing medical masks (Earloop Procedure Face Mask 1820: 3M, MN, USA) for suppressing respiratory droplet levels in a regular bedroom, and a car with air conditioning. (Table 2). Specifically, 211 adult volunteers with 208 confirmed cases of influenza (influenza A = 188; influenza B = 17) and 6 suspected cases of COVID-19 from Taipei-Keelung metropolitan area were recruited. Four 1-hour repeated measurements of particles with size range 20–1000 nm measured by number concentrations (NC0.002-1), temperature and relative humidity, and cough/sneeze per hour for each volunteer. Authors concluded that cotton masks could potentially substitute for medical masks for respiratory infected person in a microenvironment with air conditioning. Also, healthy individuals may use cotton masks in the community setting as cotton masks are washable and reusable. However, wearing of medical masks is still popular in community settings, globally (Secon, 2020). Previous studies have reported that the oral cavity is the main source of expiratory droplets in the 5 to 100 μm range during speech and cough (Johnson and Morawska, 2009).
Previous studies have shown that towel (100% cotton) and common cloth (70% cotton and 30% polyester) masks showed 40–60% filtration efficiency for polydisperse sodium chloride (NaCl) aerosol particles (75% ± 20 nm count median diameter (CMD) and a geometric standard deviation (GSD) not exceeding 1.86) at 5.5 cm/s face velocity (Rengasamy et al., 2010) (Table 2). Yao et al. (2019) investigated comfort sensation and performance of face mask related to breathing resistance for healthcare in fog or haze weather (non-COVID-19) (Table 2). The dynamic changes in airflow rate, and the breathing resistance were acquired by a virtual instrument system and a microelectronic system. The researchers used six evaluation indices for defining dynamic performance and comfort sensation of face mask where 12 different types of face masks from four brands with different features were tested, namely shape, respiratory valve, brand, main materials, and protection level. The average breathing frequency was set at 20 times per minute, and the peak flow rate of both exhalation and inhalation was 85 L/min in dynamic measurement. Findings showed that face masks with a respiratory valve had a lower change rate of breathing resistance. Moreover, cotton masks had lower change rate of breathing resistance than the non-woven fabric masks. The cup-type mask had lower change rate of breathing than the folding mask.
A review of best-published information on face masks design and efficacy reveals that face masks prevent, or reduce transmission and contraction of COVID-19, but they should not be considered as a single preventative or counter-disease measure, as they do not guarantee 100% protection. There is considerable surge in published papers on sustainability in face mask design (such as materials, layering), comfort (style), and efficacy of respiratory level of protection, but these studies, for the most part, are based on observational or laboratory studies, and not longitudinal clinical trials (Peebles, 2020). It is envisaged that future robust clinical trials will contribute significantly to this gap in knowledge.
Loey et al. (2021) reported on using artificial intelligence for detecting face mask wearing, which would support studies such as compliance and efficacy in the era of the COVID-19 pandemic (Table 2). Specifically, these authors reported on the development of a hybrid deep transfer learning model with machine learning methods for face mask detection where several thousand images of masked and non-masked individuals were analysed, which were contained in three datasets, namely, Real-World Masked Face Dataset, the Simulated Masked Face Dataset, and the labelled Faces in the Wild. The authors reported on testing and training accuracy for face mask detection at 99.64%, 99.49% and 100% respectively for these datasets.
Rodriguez-Palacios et al. (2020) reported on the use of a functional in vivo test method for assessing facemask/filtration materials using germ free (GF) mice where probiotic bacteria suspended in microdroplets were used, instead of respiratory viruses (Table 2). Use of bacteria, in this instance, was deemed appropriate as bacteria accompany respiratory viruses in respiratory droplets. This study reports on use of an in vivo spray-simulation method (mimicking a sneeze), where combed-cotton textiles used as two-layer barriers covering mice cages prevented the contamination of all GF animals when sprayed with 10–20 bacterial droplet units/cm2.
Asadi et al. (2020) conducted experimental studies using homemade cotton cloth and paper face masks that showed reductions in number of emitted expiratory particles from breathing, talking, and coughing. However, these observations are not as clear, and confounded by shedding of masks fibres, as compared significant outward particle emission reductions from wearing surgical masks and N95 respirators, even without fit-testing. The authors attest that these observations are consistent with suggestions that mask wearing can help in mitigating pandemic associated respiratory diseases. Also, their results suggest that importance of regular change of disposable masks and washing of homemade masks, and suggest that special care must be taken in removing and changing of masks.
Das et al. (2020) described electrospinning and subsequent carbonization of wheat gluten biopolymer to form nanofiber membranes for bio, or gluten-based facemasks (Table 2). These same gluten materials can be processed into cohesive thin films using plasticiser and hot press. Additionally, lanosol, a naturally-occurring substance, can be added that imparts fire (V−) rating in vertical burn test), and microbial resistance in gluten plastics. Thus, the authors advocate that thin films of flexible gluten with very low amounts of lanosol (<10%) can be bonded together with the carbonised mat and shaped by thermoforming to create the facemasks. Most medical or surgical face masks are made of non-renewable petroleum-based polymers such as polypropylene, polystyrene, polycarbonate, polyethylene, and polyester (Das et al., 2020), which are non-biodegradable and contribute towards environmental pollution. Thus, there is pressing need to rapidly develop facemasks that are fully bio-based and effective along with being low cost, lightweight and comfortable.
For facemasks, filter media is an important component (Table 2). In general, fibrous material are used to create particulate matter (PM) filters, which can be designed according to a particular size of a PM that can be ultrafine (<0.1 μm), fine (0.1–2.5 μm), and course (2.5–10 μm); denoted as PM0.1, PM2.5 and PM10 respectively. Filtration occurs through interception, inertial impaction, diffusion, and inter-molecular/electrostatic/gravitational interactions of the target particles on the surface of the filter medium. However, for virion particles, whose diameter is very small (ca. 20–400 nm), Brownian diffusion is the main filtration mechanism (Mao, 2017). Face masks provide respiratory protection from infected individual by filtration capacity of the media against the aerosol particles. Since the size of coronaviruses are typically in the range 160–200 nm (Pellett et al., 2014), non-woven filter media would be more effective that woven alternatives (Chellamani et al., 2013). Non-woven filters exhibit higher barrier properties compared to cotton and petroleum-based polyesters. Das et al. (2020) noted that these non-woven filter media can be manufactured by the process of electrospinning, which is the most cost-effective and facile methods to create fibrous membranes with a myriad of fibre diameters and porosity. Previous researchers have also used gluten with polyvinyl alcohol (PVA) through electrospinning into nanofibers (Dhandayuthapani et al., 2014; Aziz et al., 2019). Strain et al. (2015) also previously described the use of electrospun recycled polyethylene terephthalate (rPET) to develop fibrous membranes for cigarette smoke filtration. However, for the development of face masks, interdisciplinary research encompassing electrospinning, thermos-chemical conversion, gluten bio-polymer processing, and mask testing would need to addressed (Das et al., 2020). These authors also note the addition of fire retardant and moisture resistance of gluten could be enhanced by adding lanosol, and polyaminoamide epichlorohydrin (PAE), respectively, which are important for face mask using future carbonised gluten fibres.
Gandhi and Rutherford (2020) theorized that face masks could provide some degree of immunity ‘variolation’, where small doses of the virus potentially penetrate the covering and stimulate the immune response that may help with herd immunity. While this remains to be proven, it is recognised that immune-priming can potentially improve subsequent exposure to larger viral or bacterial loads. This immune-priming concept is also been exploited by researchers as a means of reducing inflammatory responses, such as use of purified β-glucans from medicinal fungi for addressing acute respiratory distress syndrome (ARDS) and sepsis that contributes significantly to severe respiratory systems experienced by critically ill COVID-19 patients (Murphy et al., 2020a; Murphy et al., 2020b; Masterson et al., 2020). Future design innovations may support greater aerosol filtration efficacy for face masks and coverings to help reduce transmission, such as potentially using head ties, instead of ear loops. For example, Sickbert-Bennett et al. (2020) reported that surgical masks with ties had filtration efficiency (FFE) of 71.5% (±5.5), while procedural mask with ear loops had lower FFE at only 38.1% (±1.1) (Table 2). There is a growing interest in evolving face masks and coverings for efficacy and wearer comfort ranging from anti-fogging capacity for those wearing spectacles to evaluating alternative biomaterials to potentially replace plastics in one-time-use PPE. The latter enable improved recycling and waste management (Silva et al., 2020; Wang et al. 2020; Ilyas et al., 2020).
Davies et al. (2013) tested filtration efficacy of house-hold masks made using different materials (including 100% cotton T-shirt, scarf, tea towel, pillowcase, antimicrobial pillowcase, vacuum cleaner bag, cotton mix, linen and silk) against bacterial (Bacillus atrophaeus, 0.95–1.25 μm) and viral (Bacteriophage MS2, 0.023 μm) aerosols (Table 2). All materials were capable of blocking test microorganisms to different extents, and they all worked better in the case of using the larger B. atrophaeus endospores. Although surgical mask, as a control sample, exhibited the highest efficacy, cleaner bag, tea towel, and cotton mix also showed filtration efficacy. However, the authors also simultaneously reported on the ease of breathing, which is indicated by pressure drop. The higher the pressure drop, the higher the difficulty for the wearer to breathe. It is observed that despite high filtration efficacy of a vacuum cleaner bag, and tea towel, their high-pressure drop values make them unsuitable for masks. Doubling the layers did not improve filtration efficacy; yet, doubling increased pressure drop, indicating more difficulty for breathing. Wearing a mask can reduce the infection probability yet cannot eliminate the risk of contracting the disease, when used alone as a non-pharmaceutical preventive measures, such as hand hygiene, social distancing, quarantine, and immunization. Chughtai et al. (2013) reviewed cloth masks using randomised clinical trial to evaluate how efficient cloth masks are for protecting HCWs. Findings revealed that respiratory infection was highest in the cloth mask group and that the particle penetration of cloth masks was 97% (versus 44% for medical masks), the authors concluded that cloth masks should not be used for HCWs, especially in highly infectious situations. Neupane et al. (2019) studied the effect of washing and drying of cloth masks on the filtration performance and correlated the performance of the pore size and shape of the masks. These authors concluded that the PM10 filtration efficiency dropped by 20% after the 4th washing and drying cycle, which was attributed to the increase in pore size and the lack of microfibers with the pore region. The authors noted that long-term usage of the cloth mask entails continuous stretching of the mask, enlarging the pore size, thus, impairing mask performance. Studies are lacking as to the specific number of times cloth mask can be washed to retain efficacy, but the risk also depends upon the degree of other mitigating non-pharmaceutical counter-measures present. Sickbert-Bennett et al. (2020) evaluated 29 different fitted face mask alternatives showed that surgical and procedural masks had lower fitted filtering performance (FFE) to that of N95 respirators (98.5% FFE), while procedural face masks secured with elastic ear loops showed lowest FFE at 38.1%. Thus, highlighting variance in FFE depending upon head tie and ear loop, which may be considered under risk mitigation for wearer in the context of overall non-pharmaceutical counter-measures and degree of potential exposure to infectious respiratory droplets.
Chua et al. (2020) reviewed innovations in face masks that may improve filtering capacity of mask materials and the addition of functions and properties into the design of masks, including super hydrophobicity (Table 2). These authors expanded upon use of polymer nanofibrous membranes, electret membranes and porous-metal organic framework (MOF)-based filters for masks, compared with existing commercial filters made of thick layers of micron-sized fibres that balance air resistance and filtering performance. Natural-based extracts, such as tea tree oils, extract of olive and Euscaphis japonica and Sophora flavescent have been sprayed on surfaces of polymeric air filters for antimicrobial properties; however, high loading of antimicrobial herbal extracts may lead to increased pressure drops (Son et al., 2020). Other experimental device-coating studies focus on combinational metal-based nanoparticles for broad spectrum activities, such as incorporation of silver-nanoparticle (AgNP)-impregnated activated carbon cloth (ACC) into a mask resulting in >99.88% virus filtration while having increased air permeability compared to FFP3 mask (US Patent Application US2011011095A1). Currently, many masks, some including a number of types of antimicrobial agents, are commercially available (Chua et al., 2020): however, mask antimicrobial activities have only been studied under strict laboratory conditions. An understanding of day-to-day performance under the actual lived-experience or clinical trial settings is lacking, as are our understanding of potential influence of actors affecting mask reusability including washing, drying or non-thermal processing. Notwithstanding the latter, Chua et al. (2020) recognised that existing models of masks and respirators serve users well in terms of appropriate level of protection against airborne pathogen.
2.6. Mathematical and statistical modelling applied to decision-making with respect to the ongoing COVID-19 pandemic
There is a gap in knowledge on the efficacy of NPIs, in terms of relative risk (RR), in preventing COVID-19 infection. R 0, the reproduction number, has been used as a measure to monitor efficacy of NPIs as it indicates the relative contagiousness of an infectious disease; R 0 denotes the average number of people who will potentially contract a contagious disease from one person with a disease, such as COVID-19 (Perencevich et al., 2020). R 0 specifically applies to a population who previously were free of infection, and were not vaccinated. For example, an R 0 of 7 infers that one infected person may potentially transmit COVID-19 to an average of 7 other susceptible people. Thus, national emergency public health teams carefully track R 0 values daily as a means of assessing how effective the implementation of strategic disease counter-measures have been (example, Government of Ireland, 2020b). This also informs ongoing public health policy decision(s), such as bans on large-in-person gatherings, closure of restaurants and retail stores, and if to implement lockdowns, such as in the Republic of Ireland where citizens have just re-emerged from its second level 5 lockdown period (Government of Ireland, 2020c). Perencevich et al. (2020) also supports that taken as a bundle, the effectiveness of adding face coverings and face shields as a community setting to other NPI containment strategies merits evaluation. The authors noted that his situation is challenging as there is no prior robust template or ‘dress rehearsal’ to follow, and public health managers and politicians need to make full decisions (100%) on the basis of a diversity of epidemiological data that is probability based; thus, tracking R 0 values provides tangible indicators of efficacy. The implicit goal of NPIs, alone or in combination with other NPIs, should be to interrupt transmission by reducing R 0 to less than 1.
In the context of predicting the variables related to an epidemic (e.g. mortality rate, disease spread, number of infected people, time until herd immunity is reached, etc.), the SIR model of Kermack and McKendrick (1927) and extensions have been used since the 1920s. SIR stands for Susceptible – Infected – Recovered, which are the main compartments individuals may belong to during an epidemic. The general formulation of a SIR model is given by a system of ordinary differential equations (ODEs) describing the instant variation in the populations of each compartment over time (t). The SIR system of ODEs may be written as
where S, I and R represent the number of susceptible, infected and recovered individuals, N is the total population, i.e. N = S + I + R, β is the infection rate and γ is the recovery and/or mortality rate. In practice, the expression βI/N is known as the “force of infection”, and the system requires the specification of the initial conditions for each compartment, as well as the values for the parameters β and γ, which are estimated from data. Each equation may be seen as the instantaneous rate of change in population size for each compartment. Typically, numerical methods are used to solve the system of ODEs and produce simulated results based on the estimates for β and γ, which are then compared to the observed data as means of validation. It can then be used to predict future number of cases and deaths, as well as the length of time a particular epidemic is likely to last.
It is often of interest to study the properties of this system and determine conditions for the persistence of the epidemic in the population. By making simple assumptions, it is possible to derive analytical expressions for what is called the “basic reproduction number”, better known as R0. Assuming that the time an infected individual remains in this infected state is exponentially distributed with parameter γ, it is straightforward to show algebraically that the average number of new infections caused by a single infected individual is R 0 = β/γ. When this ratio is greater than 1, the instantaneous change in the number of infected individuals is positive, and therefore an epidemic occurs. Conversely, when it is less than 1, the disease is contained.
More specifically in the context of the COVID-19 pandemic, there have been many attempts to model data from several countries and regions of the world using these epidemiological modelling tools. For example, Katul et al., 2020a, Katul et al., 2020b used a slightly extended SIR model to calculate an asymptotic global R 0 of 4.5, which shows how important mitigation strategies are for this rapidly growing pandemic. Toda (2020) also used a SIR model and studied the economic impact of the pandemic. He found that under optimal mitigation policies controlling timing and intensity of social distancing, simultaneous infection may be reduced from 28% to 6.2%, thus reducing the risk of overwhelming healthcare systems, but at the same time yielding a longer period of economic burden.
Extensions of the SIR model have also been proposed. For instance, Calafiore et al. (2020) proposed a modified model which added a new compartment “D”, for deceased individuals, therefore separating those who recovered from the disease versus those who did not. He et al., 2020a, He et al., 2020b, on the other hand, utilised a SEIR system (where “E” is the compartment corresponding to exposed individuals, those who have been infected but are still asymptomatic and uncapable of spreading the virus) and added two extra compartments representing quarantined and hospitalised individuals, as well as split the infected compartment into two, to separate the individuals who became infected during a quarantine phase. They fitted the model to data from the Hubei province in China and found from their parameter estimates that efficiently carried out quarantine measures are helpful to control the spread of the disease. López and Rodó (2020) also included a quarantined compartment in a SEIR-type model, and applied it to data from Spain and Italy. Giordano et al. (2020) proposed a multi-compartment extension called SIDARTHE, which included susceptible, infected, diagnosed, ailing, recognised, threatened, healed and extinct individuals. An important distinction made is between diagnosed versus non-diagnosed individuals, since asymptomatic and/or non-diagnosed people are more likely to spread the disease faster than those who have been diagnosed and are in isolation. Their findings support the combination of NPIs and contact tracing to combat the pandemic.
It is clear that one of the many challenges when modelling the COVID-19 pandemic are the effects of many different confounders acting in concert to result in higher or lower basic reproduction numbers. Of course, it would be ideal to obtain stratified R0 estimates for different groups, however there is a lack of resolution in most datasets thus not allowing for such approach. We may question how accurate these mechanistic models actually are, and how reliable the long-term projections are. For reasons of parsimony and to avoid parameter estimation problems, only the most important mechanisms and compartments are included in SIR-type models. However, this leaves out potentially important variables that could play an important role. Also, the long-term projections rely upon the current assumptions to remain the same, and it is almost never the case where circumstances do not vary over time. Therefore, the main contribution is not focussed on the reliability of these projections per se, but in understanding what the likely future outcome is so as to avoid it if necessary.
Regarding short-term prediction, different time series models have been proposed to obtain forecasts of number of cases and number of deaths. This can be especially useful to determine possible growth trends in the number of patients requiring healthcare, which in turn can help to avoid the collapse of healthcare systems. Oliveira and Moral (2020) proposed a state-space hierarchical model based on a time-varying autoregressive process and an outlier detection process to forecast the number of daily COVID-19 cases worldwide. Let Y it be the number of reported cases for country i at time t. They assume the distribution of Y it, conditional on the number of reported cases at the previous day Y i, t−1, to be negative binomial with mean μ it = exp {γ it + Ωit} and dispersion ψ. The serial autocorrelation is modelled through the parameter γ it = ϕ it γ i, t−1 + η it, where η it is a Gaussian white noise process and ϕ it is allowed to vary over time, which introduces novelty to this type of modelling framework. The parameter Ωit = λ it ω it is an observational-level random effect accounting for extra variability induced by outliers in the time series data, where λit is a Bernoulli process and assumes value 1 when observation yit is an outlier and 0 otherwise, and ωit is a normal random effect representing the extra variability attributed to outliers. Oliveira and Moral (2020) found that this particular model generates highly accurate and precise forecasts for up to seven days ahead, for most countries of the world. This modelling framework does not incorporate any biological mechanisms and population states, such as the compartment models previously discussed. However, the highly accurate short-term forecasts can be complemented by the long-term projections from SIR-type models to aid decision-making and policy implementation.
Other methods can be used for short-term forecasting. Zeroual et al. (2020) carried out a study comparing six deep learning methods to forecast the daily number of confirmed and recovered cases, using data from Italy, Spain, France, China, the USA and Australia. They found that the variational autoencoder method was superior when compared to simple recurrent neural networks, long and bidirectional short-term memory, and gated recurrent units. These are what we may refer as “black-box” methods. In essence, current data is used to train (or calibrate/estimate) the algorithm, which will be used to produce future forecasts. There is a validation step used to fine tune the algorithm, and this consists of using only part of the data to train the method, and comparing the forecasts with the actual observed data. By providing multiple and extensive validation studies, Oliveira and Moral (2020) highlight their importance for two primary reasons: (1) to ensure the method is fine-tuned to deliver the best possible performance and (2) so that the uncertainty around forecasts is properly described and over-reliance on point estimates is avoided.
An alternative to describe temporal trends and patterns is the use of generalized additive models, a very flexible modelling framework. Let Y t be the response variable of interest (e.g. number of COVID-19 cases or deaths, viral load, particle concentration etc). We may assume that Y t follows a particular probability distribution with probability mass function or probability density function p(μ t, θ), where μ t represents the mean response at time t and θ is a vector of parameters (that may be known or estimated from the data). The mean is modelled as a function of time, such that g(μ t) = f(t; β), where g(·) is a monotonic and differentiable link function, f(·) represents a sum of basis functions, often represented by splines, and β a vector of parameters to be estimated (other covariates may also be included if available). The aim is to describe the temporal process with a smooth function, and the degree of smoothness is typically determined via cross-validation or by adding specific penalties to the loss function being optimized (e.g. the log-likelihood or residual sums of squares). For instance, He et al., 2020a, He et al., 2020b fitted a Gaussian generalized additive model to viral load time series data, using cubic splines as the smooth function in the linear predictor, to examine viral shedding temporal trends. They found no significant difference across sex, age groups (over and under 65 years old) or disease severity, however.
Flaxman et al. (2020) implemented a semi-mechanistic hierarchical model to forecast the number of cases and number of deaths for several different countries, and estimated a time-varying basic reproduction number. Here, time series modelling is combined with biological information regarding infectious windows, in what is called a “semi-mechanistic” approach. This results in smooth forecast curves that can accurately depict future trends in the short-term for most countries for up to two weeks ahead. They also included the effects of NPIs in their model and found that lockdowns in particular have had a significant effect driving R0 below one. In a different approach, Ferguson et al. (2020) adapted individual-based models developed to aid in pandemic influenza planning to COVID-19 and found that R0 is likely to quickly rebound to being greater than one when NPIs are relaxed.
The hierarchical models discussed above have the inclusion of random effects as a common feature. These are important to accommodate the correlation between observations taken in same experimental or observational units (often referred to as a “grouping factor”), such as patients or geographical regions. The random effects are assumed to be have arisen from a probability distribution with a particular mean and variance (which are often the parameters of interest in the estimation process when assuming Gaussian random effects). This latent distribution is assumed to represent the entire population of interest, of which we have a representative sample in the available data. In the case of meta-analyses, parameter estimates obtained by different studies referring to the description of an effect of interest (e.g. use of face masks, social distancing of at least 1 m, etc.) are combined. Their total variability can be decomposed as between- and within-study variance, with the aid of random effects, and the effects of different characteristics of the studies on the parameter estimates can also be investigated. For instance, Chu et al. (2020) carried out random effects meta-analyses using data from 44 comparative studies worldwide (which included a total of 25,697 patients with COVID-19, SARS or MERS) to assess the effect of different NPIs. They found distancing, use of face masks and eye protection to be favoured in terms of reducing transmission. They highlight, however, the need for robust randomised trials to fill the knowledge gap with respect to effectiveness of different types of NPIs.
It is clear that the combination of different modelling methods is beneficial to understanding the problem as a whole and estimating effects with higher precision (Baker et al., 2018). Therefore, we may look at the short- and long-term projections at the same time using a combination of time series models, deep learning methods and mechanistic compartmental models. There is a problem, however, pertaining to data quality (Vespignani et al., 2020). Precise estimates can only be obtained from good-quality, large datasets. This is especially true when using machine learning black-box methods. These algorithms will reproduce patterns identified in the data, therefore if there is a lack of precision when collecting and/or reporting the data, the algorithms will reproduce the atypical and even non-sensical behaviours found in the data. For instance, Oliveira and Moral (2020) estimate that approximately 12.6% of the daily COVID-19 cases reported worldwide by the European Centre for Disease Control and Prevention (ECDC) represent outliers or points that contribute to extra variability. This reflects poor data collection practices by many countries, and therefore contribute to less accurate future forecasts. Extending the modelling methods discussed above to incorporate different mechanistic processes and NPI effects, therefore, requires good data quality to provide estimates that will be useful when elaborating public policies to prevent the spread of the virus.
Observational public health studies have revealed a number of potentially increasingly problematic factors, or multipliers that merit statistical modelling match with appropriate use of NPIs to break cycle of infections and to reduce R0, these include inter alia high COVID-19 positivity in community; close proximity and increased numbers of citizens from different households; greater transmissibility of variants; increased pathogenicity of virus across different age groups; presence of co-morbidities; gathering of vulnerable, such as in residential homes; lack or absence of vaccination; reduced testing and contract tracing; non-use of face masks or coverings; absence of hand-hygiene or disinfection; occurrence of superspreaders; COVID-19 public health compliance fatigue; environmental persistence such as prolonged survival at colder temperatures; PPE supply chain shortage; affordability; increasing presence of asymptomatic or pre-symptomatic spreaders (Fig. 2). Statistical modelling that addresses improvements in design and functionality of face coverings and future eco-sustainable, non-plastic, medical or surgical masks will inform efficacy of these counter-measures for a spectrum of increasing risk situations (Table 2). Controlled random studies should also consider extended use, re-use or reprocessing situations along with promoting user behavioural change to any perceived barriers and to improve awareness would also be relevant (Fig. 2). Several other studies have also examined the relationship between COVID-19 and meteorological factors, such as temperature (Ma et al., 2020), humidity (Liu et al., 2020) and air pollution (Zhu et al., 2020). Gupta et al. (2020) also reported on the relationship between weather parameters and COVID-19 spread using daily data of new cases in 50 US states between Jan 1 and April 9, 2020 and found that spread in the US was significant for states with 4 < absolute humidity < 6 g/m3 and number of new cases >10,000.
Chowdhury et al. (2020) investigated dynamic interventions to control the COVID-19 pandemic, where these researchers described a multi-variate prediction model, based on up-to-date transmission and clinical parameters, to simulate outbreak trajectories in 16 countries, from diverse regions and economic categories. In each country, these authors modelled the impacts on intensive care unit (ICU) admissions and death over an 18-month period for the following scenarios: (1) no intervention, (2) consecutive cycles of NPI mitigation measures followed by a relaxation period, and (3) consecutive cycles of suppression measures followed by a relaxation period. Chowdhury et al. (2020) noted that such “schedules” of social distancing might be particularly relevant to low-income countries, where a single, prolonged suppression intervention is unsustainable. These researches advocated that efficient implementation of dynamic suppression interventions can be considered pragmatic options to: (1) prevent critical care overload and deaths, (2) gain time to develop preventive and clinical measures, and (3) reduce economic hardship globally.
At this time of writing, less than 50% of the American population wear face masks and coverings (Cullen, 2020; Donmez, 2020). Use of the Institute of Health Metrics and Evaluation (IHME) model predicts that enforcing non-pharmaceutical interventions, such as face masks and social distancing, can potentially save 122,070 U.S. citizens (Donmez, 2020). Eker (2020) reflected on three popular models from a validity and usefulness perspective in terms of providing a structured framework to understand and interpret the epidemical and social mechanisms behind this COVID-19 pandemic. However, such models cannot be considered as accurate predictions tools, not only because no model is capable of doing this, but also because these models are lacking thorough formal validation. Eker (2020) reported that COVID-19 creates a citation where facts are uncertain, stakes are high, and decisions are very urgent, which is challenging for public health decision makers. Nzediaegwu and Chang (2020) reported that the number of PPE used daily in Africa is also estimated to reach seven hundred million, as several African countries have mandated compulsory face mask usage for their citizens to prevent COVID-19 transmission. Improving compliance with face covering wearing in at-risk settings presents a significant opportunity for reducing infection cases; Silva et al. (2020) noted that wearing of face masks is to be enforced in 50 countries to address COVID-19 transmission. The WHO (2020b) projected supplies of PPE must increase 40% to deal effectively with the COVID-19 pandemic; essential PPE supplies include an estimated 89 million medical masks, 76 million pairs of medical gloves, and 1.6 million pairs of goggles.
2.6.1. Mathematical and statistical modelling applied to studies of the effectiveness of face masks to avoid spreading COVID-19 including enhanced design innovation for mitigating against more transmissible SARS-CoV-2 variants
Regarding the inclusion of facemask use-related parameters within different modelling frameworks, different approaches have been used. Haug et al. (2020) combined statistical modelling and machine learning techniques and estimated that wearing a mask yields a reduction of R0 between 1.8% and 12%, while social distancing yields an approximate reduction of 20%. However, this does not take into account scenarios of high public adherence and/or high efficiency of facemasks. According to Howard et al. (2021), a combined high mask efficacy and average public adherence, or average mask efficacy and high public adherence, are likely to lead to disease containment. This was confirmed by different studies that included mask efficiency in their mathematical modelling approach. For instance, Stutt et al. (2020) developed a combined modelling approach, involving a branching process based on the negative binomial distribution and a SEIR-type model (discriminating between symptomatic and asymptomatic individuals, as well as two populations: masked and unmasked individuals), and included two parameters in their models, reflecting mask adherence and efficiency. They assume that efficiency in exhalation is greater than 50% on average, but that it is poorer when inhaling. Their assessment indicates that when R0 is 4, it may only be reduced to below 1 when almost 100% of the population is wearing masks that are more than 50% effective, at all times, even when not displaying symptoms. This is an important distinction, since their findings show that when masks are only used when individuals are symptomatic, even 100% of mask adherence combined with 100% efficiency would not be able to reduce an R0 of 4 to less than 1. In terms of comparing surgical vs. homemade masks, Eikenberry et al. (2020) developed an extended SEIR-type model, that also included symptomatic/asymptomatic compartments, and masked and unmasked populations. While their results are similar when compared to Stutt et al.'s (2020), they found that the adoption of even very weak masks (20% effectiveness) could be useful when R0 is relatively small. The assessment of a similar type of extended model developed by Worby and Chang (2020) corroborates this finding, and highlights the importance of optimized distribution, especially when resources are limited. They show that under these circumstances surgical masks should be prioritized for infected and vulnerable individuals. In the absence of current estimates for the efficacy and public adherence to facemasks, these mathematical modelling techniques illustrate possible outcomes of a range of different scenarios, and this proves to be an invaluable tool when developing public policy to contain the spread of the virus.
The combined modelling approach described by Haug et al. (2020) can inform improved efficacy of mask design and functionality, and to compare these innovations with other NPIs based on estimated effectiveness in reducing R0. For example, disposable surgical mask are commonly produced by using non-woven methods using 20 g−2 polyproplyene with spunbound technology, or 25 g m−2 non-woven sheet polypropylene using melt-blown technology; the filtration efficiency of surgical masks is influenced by fibre selection, fabrication method, the structure of the web, and the cross-sectional shape of the fibre. Each layer has a different specific function: the middle layer works as a filter; the outermost layer imposes hydrophobicity, and the innermost layer absorbs fluids from the wearer; where all three layers work by restricting transmission of small particles or pathogens from both directions (Chua et al., 2020). Disposable surgical masks consists of folded piles of fabrics that are loose fitting on the user's face, whereas N95 respirator consists of three polypropylene filtering layers and tight-edge fitting. The filter layer is generated from nylon, cotton, polyester and polypropylene where the diameter of fibres affects mechanical filtration characteristics; N95 type respirators operates at approximately 85% efficiency as the pore size of 300 nm is greater than the size of SARS-CoV-2, which is 65 to 140 nm (El-Atab et al., 2020).
For example, electrospun air filters can be modelled as offer better properties; such as the composite air filter membranes generated by electrospinning a mixture of polyvinyl chloride and polyurethane polymer demonstrated good mechanical properties with tensile strength up to 9.9 MPa with excellent air permeability (706.84 nm s−1), a high filtration efficiency (99.5%), and a low pressure drop (144 Pa) (Zhu et al., 2017). Moreover, composite membrane fabricated with Nylon 6 and PAN produced higher filtration efficiency (99.99%), where these approaches might offer improved protection against more transmissible SARS-CoV-2 variants. Wang et al. (2020) applied superhydrophobic electrospun approach using PSU with TiO2 nanoparticles in multi-layers that achieved 99.9997% filtration efficiency with a pressure drop of 45.4 Pa. However, these general electrospinning fabrication methods still use non-environmentally friendly polymers. Eco-friendly materials can be substituted with natural polymers such as polysaccharides, glutens, proteinaceous materials, biosynthetic polymer materials, and chemical synthesis of polymers (Wibisono et al., 2020). Lv et al. (2019) produced an eco-friendly electrospun membrane using polyvinyl alcohol (PVA), konjac glucomannan (KGM), and ZnO nanoparticles that increased filtration efficiency to 99.9% and increased pressure drop by 130 Pa (300 nm particles). The additions for anti-viral functional materials to layers (Table 2) can also be evaluated for improved protection. Haug et al. (2020) modelling approach can also inform development of cloth masks including number of layers, layer density, and facial fitness, and yet at the same time still considering breathability, washability and reusability. Advancement of non-medical cloth masks by combining fabric materials, such as cotton-silk, cotton-chiffon, and cotton-flannel, can potentially increase filtration efficiency to 80% (<300 nm particles (Feng et al., 2020). Currently, the most efficient face coverings are 100% cotton masks, which is based on filtration efficiency and pressure drop (Wibisono et al., 2020).
2.7. Random controlled trials and risk mitigation
Wang et al. (2020b) was one of the earliest retrospective cohort studies (28 February to 27 March 2020 in Beijing, China) of 335 people in 124 to investigate community mask wearing, hand washing, and social distancing on COVID-19 risk reduction within families. This study confirmed that the highest risk of transmission prior to symptom onset, and provided first evidence of the effectiveness of mask use, disinfection and social distancing in preventing COVID-19. The overall secondary attack rate was 23.0% (77/335). Face masks were 79% effective and disinfection was 77% effective in preventing transmission, while calculated R0 showed that close frequent contact increased the risk of transmission 18.26 times. Household crowding was also significant; results demonstrated the involvement of pre-systematic infectiousness of COVID-19 patients (Wang et al., 2020b).
Chu et al. (2020) conducted a systematic review and meta-analysis to investigate the optimum distance for avoiding person-to-person SARS-CoV-2, SARS-CoV, and MERS-CoV transmission, and to assess the use of face masks and eye protection to prevent transmission of these viruses. These authors used meta-analysis of associations of by pooling risk ratios, or adjusted odds ratios, depending on the availability from 172 observational studies across 16 countries and six continents (n = 25,697 participants), using DerSimonian and Laird random-effects models. Chu et al. (2020) also used the Newcastle-Ottawa scale to rate risk of bias for comparative non-random studies. Risk of transmission of these viruses was lower with physical distancing of 1 m or more, compared with a distance of less than 1 m; protection was increased as distance was lengthened; face mask use could result in a large reduction in risk of infection, with stronger associations with N9 or similar respirators compared with disposable surgical masks or similar (e.g., reusable 12–16 layer cotton masks; and eye protection was associated with less infection. The primary limitation of this Chu et al. (2020) study was that all studies were non-randomised, not always adjusted, and may suffer from recall and measurement bias (e.g., direct contact in some studies may not be measuring near distance). However, the authors found that unadjusted, adjusted, frequentist, and Bayesian meta-analyses all supported the main findings, and this approach supported the recording of large or very large effects.
Bungaard et al. (2020) recently reported on randomised controlled trial involving Danish participants to assess whether recommending surgical masks use outside the home reduces wearers' risk of SARS-COV-2 infection in a setting where masks were uncommon and not among recommended public health measures. A total of 3030 participants were randomly assigned to the recommendation of wear masks, and 2994 were assigned to the control group; 4862 completed the study. Infection with SARS-CoV-2 occurred in 42 participants recommended to wear masks (1.8%) and 53 control participants (2.1%). Participants were adults spending more than 3 h per day outside the home without occupational mask use. Participants were encouraged to follow social distancing measures for COVID-19, but it is not possible to prove that this as achieved. The primary measurement outcome was detection of SARS-CoV-2 in the mask wearer at 1 month by antibody testing, polymerase chain reaction (PCR), or hospital diagnosis. The secondary outcome was PCR- positivity for other respiratory viruses. The authors concluded that the recommendation to wear surgical masks to supplement other public health measures did not reduce the SARS-CoV-2 rate among wearers by more than 50% in a community with modest infection rates, some degree of social distancing, and uncommon general mask use. Loeb (2020) also described a randomised controlled trial that is ongoing in Canada in which 576 nurses will be randomised to either medical masks, or N95 respirators, when providing care to patients with COVID-19, which is due for completion on April 1, 2021. Inclusion criteria are nurses who work >37 h per week in medical, emergency, paediatric units; while exclusion criteria are nurses with one or more comorbidities, and nurses who cannot pass an N95 respirator fit test. Ultimately, researchers have concluded that globally collaborative and well conducted studies, including randomised trials, of different personal protective strategies are needed regardless of challenges, but the current use of systematic appraisals of best available evidence could be considered to inform interim guidance (Chu et al., 2020).
The WHO (2020b) noted that “all viruses, including SARS-CoV-2, change over time, most without a direct benefit to the virus in terms of increasing its infectiousness or transmissibility, and sometimes limiting propagation. The potential for virus mutation increases with the frequency of human and animal infections. Reducing transmission of SARS-CoV-2 by using established disease control methods as well as avoiding introductions to animal populations, are critical aspects to the global strategy to reduce the occurrence of mutations that have negative public health implications. Preliminary data suggest that the growth rate and effective reproductive number is elevated in areas of the United Kingdom with community circulation of the novel variant VOC-202012/01. In South Africa, genomic data highlighted that the 501Y.V2 variant rapidly displaced other lineages circulating, and preliminary studies suggest the variant is associated with a higher viral load, which may suggest potential for increased transmissibility; however, this, as well as other factors that influence transmissibility, are subject of further investigation”. The WHO has reported that epidemiologic investigations are underway to understand the increase in cases in these communities and the potential role of increased transmissibility of these variants as well as the robustness of implementation of control measures. “While initial assessment suggests that 202012/01 and 501Y.V2 do not cause changes in clinical presentation or severity, if they result in a higher case incidence, this would lead to an increase in COVID-19 hospitalizations and deaths” (WHO, 2020b). More intensive public health measures may be required to control transmission of these variants. Further investigations are required to understand the impact of specific mutations on viral properties and the effectiveness of diagnostics, therapeutics, vaccines along with disinfection and NPI modalities.
Use of risk assessment (RA) to evaluate complex environmental threats is increasing in popularity. For example, Tahar et al. (2017) reported on the development of a semi-quantitative risk assessment model for evaluating the environmental threat posed by three EU watch list pharmaceutical compounds to aquatic ecosystems. This RA model adopts the Irish EPA's Source-Pathway-Receptor concept to define relevant parameters for calculating practical low, medium or high risk scores for each agglomeration of wastewater treatment plant (WWTPs), which includes complex catchment, treatments, operational and management factors. This provides a working example where RA modelling may potentially strategically be used to unlock complex scenarios for policy decisions, such as to identify WWTPs that post a particular risk as regards releasing disproportionally high levels of pharmaceutical chemicals, and to help identify priority locations for introducing or upgrading control counter-measures (Tiedeken et al., 2017; Tahar et al., 2018; Rowan, 2019).
3. Non-pharmaceutical interventions and use of vaccines to deliver safe herd immunity in context of COVID-19 pandemic
Herd immunity is a key concept for epidemic control and is achieved when one infected person in a population generates less than one secondary case on average (Fontanet and Cauchemez, 2020). These authors described a mathematical model for forecast predications on the current COVID-19 pandemic as to how and when immunity can be achieved, and at what cost. This is also risk based, wearing face masks reduce the number of individuals who would also be more likely to get infected and to transmit because they have more contact, such as super spreaders, would be likely to be infected first. Thus, face coverings protect the population of susceptible individuals, who would typically get rapidly depleted, thus slowing the pace of transmission. Population immunity is typically estimated through cross-sectional surveys of representative samples using serological test that measure humoral immunity (Fontanet and Cauchemez, 2020). Surveys performed in countries affected during the COVID-19 epidemic, such as Italy and Spain, suggest a nationwide prevalence of antibodies ranges from 1 to 10%, with up to 15% in heavily affected urban areas Byambasuren et al. (2020). Another unknown, is whether pre-existing immunity to common cold coronaviruses may provide some level of cross-protection. However, Fontanet and Cauchemez (2020) noted that given that we do not know how long naturally acquired immunity to SARS-CoV-2 lasts. Immunity to seasonal coronaviruses is usually relatively short lived, particularly among those who had mild forms of the disease, and it may take several rounds of reinfection before robust immunity is attained.
Wearing face coverings and masks, and adopting other non-pharmaceutical interventions, are important to safeguard citizens prior to, and supplementary to, the use of effective vaccines until herd immunity is achieved. The introduction of the Pzifer-BioNTech vaccine today is a positive news with an efficacy of 95%. It is envisaged that random controlled studies focusing on the added benefits of combined use of NPIs to help manage transition to point where ‘herd immunity’ is achieved would be informative. Commensurately, face masks, and combined use of other NPIs is likely to remain essential for countries in the Northern hemisphere that are entering the autumn/winter seasons due to greater viral circulation, along with addressing greater transmissibility of SARS-CoV-2 variants as emerging in the UK due to spike protein mutation in variant 614G (Volz et al., 2021). Volz et al. (2021) did not find any indication that patients infected with the spike 614G variant have higher COVID-19 mortality or clinical severity, but 614G is associated with higher viral load and younger age of patients.
4. Conclusion and recommendations
As the first COVID-19 vaccine is distributed across the UK and other countries, the use of combined non-pharmaceutical interventions (NPIs) will remain important for preventing COVID-19 transmission globally. Wearing of face masks and improvised cloth or face coverings reduce the relative risk of COVID-19, but systematic reviews and limited randomised control studies show that they do not provide 100% protection to susceptible individuals when used alone. There remains pressure on supply chains for medical face masks, and N95 respirators, where many COVID-19 affected countries are increasing greatly in new cases. Use of single-use plastic face masks are polluting the environment that has stimulated a surge in new sustainable innovations, which includes recycling and improved waste management (Ilyas et al., 2020). Globally, deployment of the type and degree of different NPIs, from a measured tiered response approach, will be informed by relative risk evaluations and monitoring of reproduction number (R0), for example, as used by the Republic of Ireland (Government of Ireland, 2020). Mathematical models require verbose data to inform efficacy of NPIs, and potential higher relative risk ‘multiplier factor’ situations.
Recommendations arising from this study include:
Randomised controlled trials are merited to comprehensively evaluate, and validate, the single and combined use of NPIs, along with vaccines, in order to safety reach herd immunity.
Many countries significantly affected by COVID-19 will still need to consider reprocessing of PPE under EUA, where there are critical shortages.
There is pressing need to conduct global collaborative studies to appreciate, and validate new design, functionality and sustainability innovations for face masks that may be informed by life cycle assessment (LCA) and mathematical modelling.
Robust empirical data is required to inform predictive modelling and commensurate efficacy of appropriate combinational use of NPIs, including disinfection approaches, which also addresses emergence of new SARS-CoV-2 variants that appear to be replacing less transmissible variants globally. The emergence of new sustainable design innovations in face masks and coverings need to considered in the context of increasing relative risk scenarios where there is increased pressure on PPE supply chain. Greater transmissibility, and possibility pathogenesis, associated with emerging SARS-CoV-2 variants will necessitate enhanced deployment and monitoring of NPIs.
Improve behavioural change in order to avoid complacency when using face coverings in community settings with emphasis on covering both the nose and mouth, along with maintaining social distance at 2 m, to combat greater threat posed by more transmissible airborne SARS-CoV-2 variants; this can be supplemented with health literacy and education.
There should also be greater use of mathematical modelling, including relative risk assessment, to inform other factors that may potentially affect efficacy of NPIs, such as greater persistence of SARS-CoV-2 variants on surfaces due to colder winter weather, or forecasting for increased person-to-person gatherings due to celebrating religious or culture events.
There are significant opportunities to converge cross-cutting academia with innovators that will be supported and accelerated by an ‘invest and enable’ approach to driving new innovation.
Adjacent social science research is merited at a community level to inform behavioural change that includes emergence of ‘COVID-19 fatigue’, and barriers to new potential innovation (e.g., reprocessing of PPE in the Republic of Ireland for reuse did not occur due mainly to lack of confidence and understanding of new reprocessing technologies by nursing staff). There is increasing evidence that shows growing emotional stress in various cohorts in the context of COVID-19 pandemic (Shanahan et al., 2020); thus, studies such as to discern the influence (if any) of extended, or re-use of PPE to frontline HCWs, including comfort levels, are merited. However, Wang et al. (2020c) compared levels of psychological impact of the pandemic and levels of anxiety and depression between 1210 Chinese 1056 Polish participants who were encouraged and discouraged to wear masks respectively during initial stage of COVID-19. It was observed that use of face masks may safeguard better physical and mental health.
The emergence of strategic climate action and sustainable funding initiatives, such as the EC's Green Deal funding, will provide opportunities to develop clusters of complimentary expertise to deliver solutions: however, it is also envisaged that the efficacy of many of these new innovations may be validated through retrospective random controlled trials, possibly post COVID-19.
Reprocessing technologies for treating single-use PPE in healthcare under emergency conditions are currently limited to using VH2O2, and potentially UVGI, and moist heat. These reprocessing modalities should also be considered for treating new sustainable PPE from initial design stage as materials used may not be compatible with the treatment technologies.
Improvised face coverings appear to contribute to preventing COVID-19 transmission, but potentially carry a higher relative risk compared to that of wearing face masks due to lower filtration efficacy. Further testing of new face covering design innovations, such as multiple layers of materials containing anti-viral bioactive, along with breathability, are required to be met through random controlled trials. There is pressing need to improve and share data in real-time transnationally, such as through use of blockchain, machine learning, IoT, and AI that will harmonize and inform adoption of common and consistent policies. Connecting outputs by combined use of mathematical models and development of IT systems with improve global preparedness and responses to future pandemics. This will also support and enable key challenges and relative risks, such as relationship between emergence of more transmissible SARS-CoV-2 variants and the type of counter-measures to be deployed that includes NPIs in conjunction with vaccination.
Consent for publication
Not applicable.
Declaration of competing interest
The authors declare that they have no competing or conflict of interests.
Acknowledgment
The authors acknowledge the assistance of Chloe Rowan and Gillian Keane in the preparation of graphics used in this review paper.
Editor: Damia Barcelo
References
- AFNOR SPEC S76-001. Masque barrière, Guide d'exigence minimales, de méthode d'essais, de confection et d'usage. 2020. https://masques-barrieres.afnor.org/home/telechargement
- Anfinrud P., Stadnystskyi V., Bax B.E., Bax A. Visualizing speech-generated oral fluid droplets with laser light scattering. N. Engl. J. Med. 2020;382(21):2061–2063. doi: 10.1056/NEJMc2007800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arons M.M., Hatfield K.M., Reddy S.C., Kimball A., James A., Jacobs J.R., et al. Presymptomatic SARS-CoV-2 infections and transmissions in a skilled nursing facility. N. Engl. J. Med. 2020;382:2081–2090. doi: 10.1056/NEJMoa2008457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asadi S., ben Hnia N.G., Barre R.S., Wexler A.S., Ristenpart W.D., Bouvier N.H. Influenza A virus is transmissible via aerosolized fomites. Nat. Commun. 2020 doi: 10.1038/s41467-020-17888-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asadi S., Cappak C.D., Barreda S., Wexler A., Bouvier N.M., Ristenpart W.D. Efficacy of masks and face coverings in controlling outward aerosol particle emission from expiratory activities. Sci. Rep. Nat. Res. 2020 doi: 10.1038/s414598-020-72798-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ASTM F1862M-17 (2017), Standard Test Method for Resistance of Medical Face Masks to Penetration by Synthetic Blood (Horizontal Projection of Fixed Volume at a Known Velocity), ASTM International, West Conshohocken, PA, 2017.
- ASTM F201-19 (2019), Standard Test Method for Evaluating the Bacterial Filtration Efficiency (BFE) of Medical Face Mask Materials, Using a Biological Aerosol of Staphylococcus aureus, ASTM International, West Conshohocken, PA. 2019.
- Aziz S., Hosseinzadeh L., Arkan E., Azandaryani A.H. Preparation of electrospun nanofibers based on wheat gluten containing azathioprine for biomedical application. Int. J. Polym. Mater. Polym. Biomater. 2019;68:639–646. [Google Scholar]
- Baker R.E., Peña J.M., Jayamohan J., Jérusalem A. Mechanistic models versus machine learning, a fight worth fighting for the biological community? Biol. Lett. 2018;14:20170660. doi: 10.1098/rsbl.2017.0660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barceló D. An environmental and health perspective for COVID-19 outbreak: meteorology and air quality influence, sewage epidemiology indicator, hospitals disinfection, drug therapies and recommendations. J. Environ. Chem. Eng. 2020;8 doi: 10.1016/j.jece.2020.104006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behzadinasab S., Chin A., Hosseini M., Poon L.L.M., Ducker W.A.A. A surface coating that rapidly inactivates SARS-CoV-2. ACS Appl. Mater. Interfaces. 2020;12:34723–34727. doi: 10.1021/acsami.0c11425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beldomenico P.M. Do superspreaders generate new superspreaders? A hypothesis to explain the progation pattern of COVID. Int. J. Infect. Dis. 2020 doi: 10.1016/j.ijid.2020.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bi Q., Wu Y., Mei S., Ye C., Zou X., Zhang Z., et al. Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study. Lancet Infect Dis. 2020;20:911–919. doi: 10.1016/S1473-3099(20)30287-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blázquez E., Rodríguez C., Ródenas J., Navarro N., Riquelme C., Rosell R., Campbell J., Crenshaw J., Segales U.J., Pujols J., Polo J. Evaluation of the effectiveness of the SurePure Turbulator ultraviolet-C irradiation equipment on inactivation of different enveloped and nonenveloped viruses inoculated in commercially collected liquid animal plasma. PLoS One. 2019;14(2) doi: 10.1371/journal.pone.0212332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourouiba L. Turbulent gas clouds and respiratory pathogen emissions: potential implications for reducing transmission of COVID-19. JAMA. 2020;323(18):1837–1838. doi: 10.1001/jama.2020.4756. [DOI] [PubMed] [Google Scholar]
- Bundgaard H., Bundgaard J.S., Raaschou-Pedersen D.E.T., von Buchwald C., Todsen T., Norsk J.B., Pries-Heje M.M., Vissing C.R., Ringgard A., Anderson P., Goecke N.B., Trebbien R., Skovgaard K., Benfield T., Ullum H., Torp-Pedersen C., Iversen K. Effectiveness of adding a mask recommendation to other public health measures to prevent SARS-CoV-2 infection in Danish mask wearers — a randomized controlled trial. Ann. Intern. Med. 2020 doi: 10.72326/M20-6817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byambasuren O., et al. Estimating the seroprevalence of SARS-CoV-2 infections: systematic review. medRxiv. 2020 doi: 10.1101/2020.07.13.20153163. Preprint at. [DOI] [Google Scholar]
- Calafiore G.C., Novara C., Possieri C. A time-varying SIRD model for the COVID-19 contagion in Italy. Annu. Rev. Control. 2020;50:361–372. doi: 10.1016/j.arcontrol.2020.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan K.H., Sridhar S., Zhang R.R., Chu H., Fung A.Y., Chan G., Chan J.F., To K.K., Hung I.F., Cheng V.C., Yuen K.Y. Factors affecting stability and infectivity of SARS-CoV-2. J. Hosp. Infect. 2020 doi: 10.1016/j.jhin.2020.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chellamani K.P., Veerasubramanian D., Balaji R.S.V. Surgical face masks: manufacturing methods and classification. J. Acad. Indust. Res. 2013;2:320–324. [Google Scholar]
- Chin A.W.H., Chu J.T.S., Perera M.R.A., Hui K.P.Y., Yen H.-L., Chan M.C.W., Peris M., Poon L.L.M. Stability of SARS-Cov-2 in different environmental conditions. Lancet Microbe. 2020;1 doi: 10.1016/S2666-5247(20)30003-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowdhury R., Heng K., Shawon M.S.R., Goh G., Okonofua D., Ochoa-Rosales C., Gonzales-Jaramillo V., Bhuiya A., Reidpath D., Prathapan S., Shahzad S., Athaus C.L., Gonzalez-Jaramillo N., Franco O.H. Dynamic interventions to control COVID-19 pandemic: a multivariate prediction modelling study comparing 16 worldwide countries. Eur. J. Epidemiol. 2020;35:389–399. doi: 10.1007/s10654-020-00649-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu D.K., Akl E.A., Duda S., Solo K., Yaacoub S., Schunemann H.J. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395:1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chua M.H., Cheng W., Goh S.S., Kong J., Li B., Lim J.Y.C., Mao L., Wang S., Xue K., Yang L., Ye E., Zhang K., Cheong W.C.D., Tan B.H., Li Z., Tan B.H., Loh Z.J. Face masks in the new COVID-19 normal: materials, testing and perspectives. AAAS Res. 2020 doi: 10.34133/2020/7286735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chughtai A.A., Seale H., MacIntyre C.R. Use of cloth masks in the practice of infection control — evidence and policy gaps. Int. J. Infect. Control. 2013;9(3) [Google Scholar]
- Cook T.M. Personal protective equipment during coronavirus disease (COVID) 2019 pandemic - a narrative review. Anaesthesia. 2020;75(7):920–927. doi: 10.1111/anae.15071. [DOI] [PubMed] [Google Scholar]
- Cullen P. Ireland may see 1,200 more Covid-19 deaths by 2021 if face mask use doesn't improve — US experts. 2020. https://www.irishtimes.com/news/health/ireland-may-see-1-200-more-covid-19-deaths-by-2021-if-face-mask-use-doesn-t-improve-us-experts-1.4347042
- Das O., Neiziany R.E., Capezza A.J., Hedenqvist M.S., Forsth M., Xu Q., Jiang L., Ji D., Ramakrishna S. The need for fully bio-based facemasks to counter-coronavirus outbreaks: a perspective. Sci. Total Environ. 2020:736. doi: 10.1016/j.scitotenv.2020.139611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies A., Thompson K.A., Giri K., Kafotas G., Walker J., Bennett A. Testing the efficacy of homemade masks; would they protect in an influenza pandemic? Dis. Med. Publ. Health Prep. 2013;7(4):413–418. doi: 10.1017/dmp.2013.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dbouk T., Drikakis D. On repiratory droplets and face masks. Phys. Fluids. 2020;32 doi: 10.1063/5.0015044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dbouk T., Drikakis D. On coughing and airborne droplet transmission in humans. Phys. Fluids. 2020;32(5) doi: 10.1063/5.0011960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derraik Y.G.B., Anderson W.A., Connelly E.A., Anderson Y.C. Rapid review of SARS-CoV-1 and SARS-CoV-2 viability, susceptibility to treatment, and the disinfection and reuse of PPE, particularly filtering facepiece respirators. Int. J. Environ. Res. Public Health. 2020;17:6117. doi: 10.3390/ijerph17176117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dev Kumar G., Mishra A., Dunn L., Townsend I., Oguadinma C., Bright K.R., Gerba C.P. Biocides and novel antimicrobial agents for the mitigation of coronaviruses. Front. Microbiol. 2020;11:1351. doi: 10.3389/fmicb.2020.01351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhandayuthapani B., Mallampati R., Sriramulu D., Dsouza R.F., Valiyaveettil S. PVA/gluten hybrid nanofibres for removal of nanoparticles from water. ACS Sustain. Chem. Eng. 2014;2:1014–1021. [Google Scholar]
- Diaz D. U.K. begings nationwide coronavirus immunization, latest in nation's history. 2020. https://www.npr.org/sections/coronavirus-live-updates/2020/12/08/944125280/u-k-begins-nationwide-coronavirus-immunization-largest-in-nations-history?t=1607636443459
- Donmez B.B. US: model predicts 400,000 COVID-19 deaths by January. 2020. https://www.aa.com.tr/en/americas/us-model-predicts-400-000-covid-19-deaths-by-january/1963459
- Driessche K.V., Hens N., Tilley P., Quon B.S., Chilvers M.A., deGroot R., Cotton M.F., Marais B.J., Speert D.P., Zlosnik J.E.A. Surgical masks reduce air-borne spread of Pseudomonas aeruginosa in colonized patients with cystic fibrosis. Am. J. Respir. Crit. Care Med. 2015;192:897–899. doi: 10.1164/rccm.201503-0481LE. [DOI] [PubMed] [Google Scholar]
- Eikenberry S.E., Mancuso M., Iboi E., Phan T., Eikenberry K., Kuang Y., Kostelich E., Gumel A.B. To mask or not to mask: modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infect. Dis. Modell. 2020;5:293–308. doi: 10.1016/j.idm.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eker S. Validity and usefulness of COVID-19 models. Human. Soc. Sci. Commun. 2020 doi: 10.1057/s41599-020-00535-4. [DOI] [Google Scholar]
- El-Atab N., Qaiser N., Badghaish H., Shaikh S.F., Hussain M.M. Flexible non-porous template for the design and development of reusable anti-COVID-19 hydrophobic face masks. ACS Nano. 2020;14:7659–7665. doi: 10.1021/acsnano.0c03976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- European Centre for Disease Prevention and Control New COVID-19 situation dashboard. 2020. https://www.ecdc.europa.eu/en/covid-19-pandemic (accessed 11th October, 2020)
- European Centre for Disease Prevention and Control Cloth face masks and masks sterilisation as options in case of shortage of surgical masks and respirators. 2020. https://www.ecde.europa.eu/en/publications-data/cloth-masks-sterilisation-options-shortage-surgical-masks-respirators Available on 8th September 2020 at.
- FDA Emergency use authorization (EUA) information, and list of all current EUAs. 2020. https://www.fda.gov/emergency-preparedness-and-response/mcm-legal-regulatory-and-policy-framework/emergency-use-authorization#covidppe (Accessed 8th October, 2020)
- Feng S., Shen C., Xia N., Song W., Fan M., Cowling B. Rational use of face masks in the COVID-19 pandemic. Lancet Respir. Med. 2020;8:434–436. doi: 10.1016/S2213-2600(20)30134-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson N., Laydon D., Nedjati-Gilani G., Imai N., Ainslie K., Baguelin M., Bhatia S., Boonyasiri A., Cucunubá Z., Cuomo-Dannenburg G., Dighe A., Dorigatti I., Fu H., Gaythorpe K., Green W., Hamlet A., Hinsley W., Okell L.C., van Elsland S., Thompson H., Wang H., Wang Y., Walker P.G.T., Walters C., Winskill P., Whittaker C., Donnelly C.A., Riley S., Ghani A.C. Report 9: impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand. Imp. Coll. Lond. 2020;10:77482. [Google Scholar]
- Figueroa A., Hauck R., Saldias-Rodriguez J., Gallardo R.A. Combination of quaternary ammonium and glutaraldehyde as a disinfectant against enveloped and non-enveloped viruses. J. Appl. Poul. Res. 2017;26:491–497. [Google Scholar]
- Fischer E.P., Fischer M.C., Grass D., Henrion I., Warren S.W., Westman E. Low cost measurement of facemask efficiency for following expelled droplets during speed. Sci. Adv. 2020 doi: 10.1126/sciadv.abd3083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flaxman S., et al. Estimating the effects of non-pharmaceutical interventions of COVID-19 in Europe. Nature. 2020;584:257–261. doi: 10.1038/s41586-020-2405-7. [DOI] [PubMed] [Google Scholar]
- Fontanet A., Cauchemez S. COVID-19 herd immunity: where are we? Nat. Rev. Immunol. 2020 doi: 10.1038/s41577-020-00451-5. (October, 2020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandhi M., Rutherford G.W. Facial masking for Covid-19 — potential for “variolation” as we await a vaccine. N. Engl. J. Med. 2020 doi: 10.1056/NEJMp2026913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giordano G., Blanchini F., Bruno R., Colaneri P., Di Filippo A., Di Matteo A., Colaneri M. Modelling the COVID-19 epidemic and implementation of population-wide interventions in Italy. Nat. Med. 2020;26:855–860. doi: 10.1038/s41591-020-0883-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of Ireland Latest charts and maps on COVID-19 in Ireland. 2020. https://www.gov.ie/en/service/0039bc-view-the-covid-19-coronavirus-dashboard-showing-the-latest-stats-and/ (Accessed 8th December, 2020)
- Government of Ireland Ireland placed on level 5 of the plan for living with COVID-19. 2020. https://www.gov.ie/en/press-release/66269-ireland-placed-on-level-5-of-the-plan-for-living-with-covid/ (Accessed 8th December, 2020)
- Government of Ireland . 2020. Resilience and Recovery 2020–2021 — Plan for Living With COVID-19. file:///C:/Users/Neil/Downloads/87128_0d3f8c17-2c95-40c3-9311-e3fbb2c0fae5.pdf (Accessed 8th December, 2020) [Google Scholar]
- Guan D., Wang D., Hallegatte S., Davis S.J., Huo S., Li L., Bai Y., Lei T., Xue Q., Coffiman D., Cheng D., Chen P., Liang X., Xu B., Lu X., Wang S., Hubacek K., Cong P. Global supply-chain effects of COVID-19 control measures. Nat. Hum. Behav. 2020 doi: 10.1038/s41562-020-0896-8. [DOI] [PubMed] [Google Scholar]
- Gupta S., Raghuwanshi G.S., Chanda A. Effect of weather on COVID-19 spread in the US: a prediction model for India in 2020. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamner L., Dubbel P., Capron I., Ross A., Jordan A., Lee J., et al. High SARS-CoV-2 attach rate following exposure at a choir practice – Skagit County, Washington, March 2020. MMWR Morb. Mortal. Wkly Rep. 2020;89:606–610. doi: 10.15585/mmwr.mm6919e6. [DOI] [PubMed] [Google Scholar]
- Haug N., Geyrhofer L., Londei A., Dervic E., Desvars-Larrive A., Loreto V., Pinior B., Thurner S., Klimek P. Ranking the effectiveness of worldwide COVID-19 government interventions. Nat. Hum. Behav. 2020;4(12):1303–1312. doi: 10.1038/s41562-020-01009-0. [DOI] [PubMed] [Google Scholar]
- He S., Peng Y., Sun K. SEIR modeling of the COVID-19 and its dynamics. Nonlin. Dynam. 2020;101:1667–1680. doi: 10.1007/s11071-020-05743-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He X., Lau E.H., Wu P., Deng X., Wang J., Hao X., Lau Y.C., Wong J.Y., Guan Y., Tan X., Mo X., Chen Y., Liao B., Chen W., Hu F., Zhang Q., Zhong M., Wu Y., Zhao L., Zhang F., Cowling B.J., Li F., Leung G.M. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat. Med. 2020;26(5):672–675. doi: 10.1038/s41591-020-0869-5. [DOI] [PubMed] [Google Scholar]
- Ho K.-F., Lin L.-Y., Weng S.-P., Weng S.-P., Chuang K.J. Medical mask versus cotton masks for preventing respiratory droplet transmission in micro-environments. Sci. Total Environ. 2020 doi: 10.1016/j.scitotenv.2020.139510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hui D.S., Chow B.K., Chu L., Ng S.S., Lee N., Gin T., Chan M.T.V. Exhaled air dispersion during coughing with and wearing surgical or N95 mask. PLoS One. 2012;7 doi: 10.1371/journal.pone.0050845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutten I.M. In: Handbook of Nonwoven Filter Media. 2nd ed. Hutten I.M., editor. Butterworth-Heineman Publishers; 2016. Chapter 6 — Testing of nonwoven filter media; pp. 343–408. [Google Scholar]
- Ilyas S., Srivastava R.R., Kim H. Disinfection technology and strategies for COVID-19 hospital and bio-medical waste management. Sci. Total Environ. 2020;749 doi: 10.1016/j.scitotenv.2020.141652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin Z., Du X., Xu Y., Deng Y., Liu M., Zhao Y., et al. Structure-based drug design, virtual screening and high-throughput screening rapidly identify antiviral leads targeting COVID-19. bioRziv. 2020 doi: 10.1101/2020.02.26.964882. [DOI] [Google Scholar]
- Johns Hopkins University . 2020. New cases of COVID-19 in word countries (7 day moving average)https://coronavirus.jhu.edu/data/new-cases [Google Scholar]
- Johnson G.R., Morawska L. The mechanism of breath aerosol formation. J. Aerosol. Med. 2009;22:229–237. doi: 10.1089/jamp.2008.0720. [DOI] [PubMed] [Google Scholar]
- Kampf G. Efficacy of ethanol against viruses in hand disinfection. J. Hosp. Infect. 2018;98(4):331–338. doi: 10.1016/j.jhin.2017.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kampf G., Todt D., Pfaemder S., Steinmann E. Persistence of coronavirus on inanimate surfaces and their inactivation with biocidal agents. J. Hosp. Infect. 2020;104(3):246–257. doi: 10.1016/j.jhin.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasloff S.B., Strong J.E., Funk D., Cutts T.A. Stability of SARS-Cov-2 on critical personal protective equipment. MedRxiv. 2020 doi: 10.1101/2020.06.11.20128884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katul G.G., Mrad A., Bonetti S., Monoli G., Parolari J. Global convergence of COVID-19 basic reproduction number and estimation from early-time SIR dynamics. PLoS One. 2020;15(9) doi: 10.1371/journal.pone.0239800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katul G.G., Mrad A., Bonetti S., Monoli G., Parolari J. Global convergence of COVID-19 basic reproduction number and estimation from early-time SIR dynamics. PLoS One. 2020;15(9) doi: 10.1371/journal.pone.0239800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenyon C. The prominence of asymptomatic superspreaders in transmission mean universal face masking should be part of COVID-19 de-escalation strategies. Int. J. Infect. Dis. 2020 doi: 10.1016/j.ijid.2020.05.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kermack W.O., McKendrick A.G. A contribution to the mathematical theory of epidemics. Proc. R. Soc. Lond. Ser. A. 1927;115:700–721. [Google Scholar]
- Koyama T., Platt D., Parida L. Variant analysis of SARS-CoV-2 genomes. Bull. World Health Org. 2020;98(7):495–504. doi: 10.2471/BLT.20.253591. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7375210/pdf/BLT.20.253591.pdf July 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S., Kim T., Lee E., Lee C., Kim H., Rhee H., Park Y.P., Son H.-J., Yu S., Park J.W., Choo E.J., Park S., Loeb M., Kim T.H. Clinical course and molecular viral shredding among asymptomatic and symptomatic patients with SARS-CoV-2 infection in a community treatment Centre in the Republic of Korea. JAMA Intern. Med. 2020;180(1):1447–1452. doi: 10.1001/jamainternmed.2020.3862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung N.H.L., Chu D.K.W., Shiu E.Y.C., et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat. Med. 2020;26(5):676–680. doi: 10.1038/s41591-020-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Zhou J., Yao J., Zhang Z., Li L., Zu X., Wang B., Fu S., Niu T., Wan U.J., Shi Y., Ren Z., Niu J., Zhu W., Li S., Luo B., Zhang K. Impact of meteorological factors on the COVID-19 transmission: a multi-city study in China. Sci. Total Environ. 2020;726:138513. doi: 10.1016/j.scitotenv.2020.138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeb M. Medical masks versus N95 respirators to prevent 2019 Novel Coronavirus Disease (COVID-19) in healthcare workers: a randomized trial. 2020. https://ichgcp.net/clinical-trials-registry/NCT04296643
- Loey M., Monogaran G., Taha M.H.N., Khalifa N.E.M. A hybrid deep transfer learning model with machine learning methods for face mask detection in the era of the COVID-19 pandemic. Measurement. 2021;167 doi: 10.1016/j.measurement.2020.108288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López L., Rodó X. A modified SEIR model to predict the COVID-19 outbreak in Spain and Italy: simulating control scenarios and multi-scale epidemics. Results in Physics. 2020;25 doi: 10.1016/j.rinp.2020.103746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lv D., Wang R., Tang G., Mou Z., Lei J., Han J., Smedt S., Xiong R., Huang C. Eco-friendly electrospun membranes loaded with visible-light response nano-particles for multi-functional usages; high-efficient air filtration, dye scavenger, and bactericide. ACS Appl. Mater. Interfaces. 2019;11:12880–12889. doi: 10.1021/acsami.9b01508. [DOI] [PubMed] [Google Scholar]
- Ma Y., Zhao Y., Liu J., He X., Wang B., Fu S., Yan J., Niu J., Zhou J., Luo B. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Sci. Total Environ. 2020;724:138226. doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao N. In: Fibrous Filter Media. Brown P.J., Cox C.L., editors. Woodhead Publishing; 2017. Nonwoven fabric filters; pp. 133–171. [Google Scholar]
- Masterson C.M., Murphy E., Gonzalez H., Major I., McCarthy S.D., O’Toole D., Laffey J.G., Rowan N.J. Purified β-glucans from the Shiitake mushroom ameliorates antibiotic-resistant Klebsiella pneumoniae-induced pulmonary sepsis. Lett. Appl. Microbiol. 2020 doi: 10.1111/lam.13358. [DOI] [PubMed] [Google Scholar]
- McEvoy B., Rowan N.J. Terminal sterilization of medical devices using vaporized hydrogen peroxide: a review of current methods and emerging opportunities. J. Appl. Microbiol. 2019;127(5):1403–1420. doi: 10.1111/jam.14412. [DOI] [PubMed] [Google Scholar]
- Michie S., West R., Harvey N. The concept of “fatigue” in tackling covid-19. BMJ. 2020 doi: 10.1136/bmj.m4171. [DOI] [PubMed] [Google Scholar]
- Milton D.K., Fabian M.P., Cowling B.J., Grantham M.L., McDevitt J.J. Influenza virus aerosols in human exhaled breath: particle size, culturability, and effect of surgical masks. PLoS Pathog. 2013;9 doi: 10.1371/journal.ppat.1003205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy E., Masterson C., Rezoagli E., Major I., Stack G., O’Toole D., Laffey J.G., Rowan N.J. 2020. β-Glucan Extracts From the Same Edible Shiitake Mushroom Lentinus edodes Produce Differential In-vitro Immunomodulatory and Pulmonary Cytoprotective Effects — Implications for Coronavirus Disease (COVID-19) Immunotherapies. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy E., Rezoagli E., Major I., Laffey J.G., Rowan N.J. β-Glucan metabolic and immunomodulatory properties and potential for clinical application. J. Fungi. 2020;6:356. doi: 10.3390/jof6040356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neupane B.B., Mainali S., Sharma A., Giri B. Optical microscopic study of surface morphology and filtering performance of face masks. PeerJ. 2019;7 doi: 10.7717/peerj.7142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nzediaegwu C., Chang S.X. Improper solid waste management increases potential for COVID-19 spread in developing countries. Resour. Conserv. Recycl. 2020 doi: 10.1016/j.resconrec.2020.104947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliveira T.P., Moral R.A. Global short term forecasting of Covid-19 cases. arXiv:2006.00111. 2020 doi: 10.1038/s41598-021-87230-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagat A.-M., Seux-Goepfort R., Lutsch C., Lecouturier V., Saluzzo J.-F., Kuster I.C. Evaluation of SARS-coronavirus decontamination procedures. Appl. Biosafety. 2007;12:100–108. [Google Scholar]
- Peebles L. What the data say about wearing face masks. Nature. 2020;586:186–189. doi: 10.1038/d41586-020-02801-8. [DOI] [PubMed] [Google Scholar]
- Pellett P.E., Mitra S., Holland T.C. In: Handbook of Clinical Neurology. Tselis A.C., Booss J., editors. Vol. 123. Elsevier; 2014. Chapter 2 — Basics of virology; pp. 45–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perencevich E.N., Diekema D.J., Edmond M.B. Moving personal protective equipment into the community — face shields and containment of COVID-19. JAMA. 2020;323(2) doi: 10.1001/jama.2020.7477. [DOI] [PubMed] [Google Scholar]
- Pinon A., Vialette M. Survival of viruses in water. Intervirology. 2018;61:214–222. doi: 10.1159/000484899. [DOI] [PubMed] [Google Scholar]
- Rengasamy S., Eimer B., Shaffer R.E. Simple respiratory protection — evaluation of the filtration performance of cloth masks and common fabric materials against 20–1000 nm size particles. Ann. Occup. Hyg. 2010;54:789–798. doi: 10.1093/annhyg/meq044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riddell S., Goldie S., Hill A., Eagle D., Drew T.W. The effect of temperature on persistence of SARS-CoV-2 on common surfaces. Virol. J. 2020;17 doi: 10.1186/s12985-020-01418-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Palacios A., Conger M., Cominelli F. Germ-free mice under two-layer textiles are fully protected from bacterial in sprayed microdroplets: a functional in vivo test method of facemask/filtration materials. Front. Med. 2020;7:504. doi: 10.3389/fmed.2020.00504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotter M.L. Arguments of alcoholic hand disinfection. J. Hosp. Infect. 2001;48:S4–S8. doi: 10.1016/s0195-6701(01)90004-0. [DOI] [PubMed] [Google Scholar]
- Rowan N.J. Pulsed light as an emerging technology to cause disruption for food and adjacent industries — quo vadis? Trends Food Sci. Technol. 2019;88:316–332. [Google Scholar]
- Rowan N.J., Galanakis C.M. Unlocking challenges and opportunities presented by COVID-19 pandemic for cross-cutting disruption in agri-food and green deal innovations: quo vadis? Sci. Total Environ. 2020;748:141362. doi: 10.1016/j.scitotenv.2020.141362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowan N.J., Laffey J.G. Challenges and solutions for addressing critical shortage of supply chain for personal and protective equipment (PPE) arising from coronavirus disease (COVID19) pandemic — case study from the Republic of Ireland. Sci. Total Environ. 2020;725(2020) doi: 10.1016/j.scitotenv.2020.138532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowan N.J., Laffey J.G. Unlocking the surge in demand for personal and protective equipment (PPE) and improvised face coverings arising from coronavirus disease (COVID-19) pandemic — implications for efficacy, re-use and sustainable waste management. Sci. Total Environ. 2020;752(2020) doi: 10.1016/j.scitotenv.2020.142259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubio-Romero J.C., del Carmen M., Ferreira P., Torrecilla J.A., Santiago G., Castro C. Disposable masks: disinfection and sterilization for reuse, and non-certified manufacturing, in the face of shortages during the COVID-19 pandemic. Sci. Total Environ. 2020 doi: 10.1016/j.ssci.2020.104830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Secon H. Bus. Insid. 2020. People are racing to buy face masks amid the coronavirus outbreak, but they probably won’t protect you from illness.https://ww.businessinsider.com/wuhan-coronavirus-face-masks-not-entirely-effective-2020-1 Available from. [Google Scholar]
- Shanahan L., Steinhoff A., Bechtiger L., Murray A.L., Nivette A., Hepp U., Ribeaud D., Eisner M. Emotional distress in young adults during COVID-19 pandemic: evidence of risk and resilience from a longitudinal cohort study. Psychol. Med. 2020:1–10. doi: 10.1017/S003329172000241X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sickbert-Bennett E.E., Samet M., Clapp P.W. Filtration efficiency of hospital face mask alternatives available for use during the COVID-19 pandemic. JAMA Intern. Med. 2020 doi: 10.1001/jamaintermed.2020.4221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva A.L.P., Prata J.C., Walker T.R., Campos T.R.W., Duarte A.C., Soares A.M.V.M., Barceló D., Rocha-Santos T. 2020. Rethinking and Optimising Plastic Waste Management Under COVID-19 Pandemic: Policy Solutions Based on Redesign and Reduction of Single-use Plastics and Personal Protective Equipment. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Son B.C., Park C.H., Kim C.S. Fabrication of antimicrobial nanofiber air filter using activated carbon and cinnamon essential oil. J. Nanosci. Nanotechnol. 2020;20(7):4376–4380. doi: 10.1166/jnn.2020.17597. [DOI] [PubMed] [Google Scholar]
- Stadnytsky V., Bax B.E., Bax A., Anfinrud A. The airborne lifetime of small speech droplets and their potential importance in SARS-CoV-2 transmission. Proc. Natl. Acad. Sci. 2020;117(22):11875–11877. doi: 10.1073/pnas.2006874117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockwell R.E., Knibbs M.E., He C., Sherrard L.J., Ballard E.I., Kidd T.J., Johnson G.R., Knibbs L.D., Morawska L., Bell S.C. Face masks reduce the release of Pseudomonas aeruginosa cough aerosols when worn for clinically relevant periods. Am. J. Respir. Crit. Care Med. 2018;198:1339–1342. doi: 10.1164/rccm.201805-0823LE. [DOI] [PubMed] [Google Scholar]
- Strain I.N., Wu Q., Pourrahimi A.M., Hedenqvist M.S., Olsson R.T., Andersson R.I. Electrospinning of recycled PET to generate tough mesomorphic fibre membranes for smoke filbration. J. Mater. Chem. 2015;A3:1632–1640. [Google Scholar]
- Stutt R.O., Retkute R., Bradley M., Gilligan C.A., Colvin J. A modelling framework to assess the likely effectiveness of facemasks in combination with ‘lock-down’in managing the COVID-19 pandemic. Proc. Royal Soc. A. 2020;476(2238):20200376. doi: 10.1098/rspa.2020.0376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tahar A., Tiedeken E.J., Clifford E., Cummins E., Rowan N. Development of a semi-quantitative risk assessment model for evaluating environmental threat posed by the three first EU watch-list pharmaceuticals to urban wastewater treatment plants: an Irish case study. Sci. Total Environ. 2017;603–604:627–638. doi: 10.1016/j.scitotenv.2017.05.227. [DOI] [PubMed] [Google Scholar]
- Tahar A., Tiedeken E.J., Rowan N.J. Occurrence and geodatabase mapping of three contaminants of emerging concern in receiving water and at effluent from waste water treatment plants — a first overview of the situation in the Republic of Ireland. Sci. Total Environ. 2018;616–617:187–197. doi: 10.1016/j.scitotenv.2017.11.021. [DOI] [PubMed] [Google Scholar]
- Tang J.W., Liebner T.J., Craven B.A., Settles G.S. A Schlieren optical study of the human cough with and without wearing mask for aerosol infection control. J. R. Soc. Interface. 2009;6:727–736. doi: 10.1098/rsif.2009.0295.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tellier R., Li Y., Cowling B.J., Tang J. Recognition of aerosol transmission of infectious agents: a commentary. BMJ Infect. Dis. 2019;19:101. doi: 10.1186/s12879-019-3707-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiedeken E.J., Tahar A., McHugh B., Rowan N.J. Monitoring, sources, receptors, and control measures for the three European Union watch list substances of emerging concern in receiving waters — a 20 year systematic review. Sci. Total Environ. 2017;574:1140–1163. doi: 10.1016/j.scitotenv.2016.09.084. [DOI] [PubMed] [Google Scholar]
- Tino R., Moore R., Antoline S., Ravi P., Wake N., Ionita C.N., Morris J.M., Decker S.J., Sheikh A., Rybicki F.J., Chepelev L.L. COVID-19 and the role of 3D printing in medicine. 3D Print Med. 2020 doi: 10.1186/s41205-020-00064-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toda A.A. Susceptible-infected-recovered (SIR) dynamics of COVID-19 and economic impact. arXiv:2003.11221. 2020 [Google Scholar]
- Van Doremalen, N., Bushmaker, T., Morris, D., Holbrook, M., Gamble, A., Williamson, B. et al. 2020. Aerosol and surface stability of HCoV-19 (SARS-CoV-2) compared to SARS-CoV-1. N. Engl. J. Med. 382, 1564–1267. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed]
- Vespignani A., Tian H., Dye C., Lloyd-Smith J.O., Eggo R.M., Shrestha M., Scarpino S.V., Gutierrez B., Kraemer M.U., Wu J., Leung K., Leung G.M. Modelling COVID-19. Nat. Rev. Phys. 2020;2:279–281. doi: 10.1038/s42254-020-0178-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volz E., Hill V., McCrone J.T., Price A., Jorgensen D., O’Toole A., Southgate J., Johnson R., Jackshon B., Nascimento F.F., Rey S.M., Nicholls S.M., Colquhoun R.M., Filipe A., Shepherd J., Pascall D.J., Shah R., Jesudason N., Li K., Jarrett R., Pacchiarini N., Bull N., Geidelbergy L., Siveroni I. Evaluating the effects of SARS-CoV-2 spike mutation D614G on transmissibility and pathogenicity. Cell. 2021;184(1):64–75. doi: 10.1016/j.cell.2020.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Chudzicka-Czupala A., Grabowski D., Pan R., Adamus K., Wan X., Hetnal M., Tan Y., Olszewska-Guisso A., Xu L., McIntyre R.S., Quek J., Ho R., Ho C. The association between physical and mental health and face mask use during the COVID-19 pandemic: a comparison of two countries with different views and practices. Front. Psychiat. 2020;11:569981. doi: 10.3389/fpsyt.2020.569981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Shen J., Ye D., Yan X., Zhang Y., Yang W., Li X., Wang J., Zhang L., Pan L. Disinfection technology of hospital waste and wastewater suggestions for disinfection strategy during Coronavirus Disease-2019 (COVID-19) pandemic in China. Environ. Pollut. 2020;262 doi: 10.1016/j.envpol.2020.114665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Tian H., Zhang L., Zhang M., Guo D., Wu W., Zhang X., Kan G.L., Jia L., Hoo D., Liu B., Wang X., Sun Y., Wang Q., Yang P., MacIntyre R. Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: a cohort study in Beijing, China. BMJ Glob. Health. 2020;5 doi: 10.1136/bmjgh-2020-002794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wibisono Y., Fadila C.R., Saiful S., Bilad M.R. Facile approaches of polymeric face masks reuse and reinforcements for micro-aerosol droplets and virus filtration: a review. Polymers. 2020;12:2516. doi: 10.3390/polym12112516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worby C.J., Chang H.H. Face mask use in the general population and optimal resource allocation during the COVID-19 pandemic. Nat. Commun. 2020;11(1):1–9. doi: 10.1038/s41467-020-17922-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization Advice on the use of masks in the context of COVID-19 pandemic. Interim guidance 4 July, 2020. 2020. https://apps.who.int/iris/rest/bitstreams/1279750/retrieve accessed 10th October, 2020.
- World Health Organization SARS-CoV-2 variants — emergencies preparedness response. 2020. https://www.who.int/csr/don/31-december-2020-sars-cov2-variants/en/ (accessed 31 December, 2020)
- World Health Organization Transmission of SARS-CoV2: implications for infection control prevention. 2020. https://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions accessed 25th August, 2020.
- Yao B.G., Wan Y.-X., Ye X.-Y., Zhang F., Peng Y.-L. Impact of structural features on dynamic breathing resistance of healthcare face mask. Sci. Total Environ. 2019;689:743–753. doi: 10.1016/j.scitotenv.2019.06.463. [DOI] [PubMed] [Google Scholar]
- Zeroual A., Harrou F., Dairi A., Sun Y. Deep learning methods for forecasting COVID-19 time-series data: a comparative study. Chaos, Solitons Fractals. 2020;140:110121. doi: 10.1016/j.chaos.2020.110121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong H., Zhu Z., Lin J. Reusable and recyclable graphene masks with outstanding superhydrophobic and photothermal performances. ACS Nano. 2020;14(5):6213–6221. doi: 10.1021/acsnano.0c02250. [DOI] [PubMed] [Google Scholar]
- Zhu M., Han J., Hang F., Shao W., Xiong R., et al. Electrospun nanofibers membranes for effective air filtration. Macromol. Mater. Eng. 2017;302:1600353. [Google Scholar]
- Zhu Y., Zie J., Huang F., Cao L. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci. Total Environ. 2020;727:138704. doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]