Abstract
Objective
To explore the activity changes in neurology clinical practice that have occurred in tertiary public hospitals during the COVID-19 pandemic.
Methods
Outpatient and inpatient data from the neurology department were extracted from the electronic medical record system of three tertiary Grade A hospitals in Wenzhou. Data were analyzed across 5 months following the beginning of the pandemic (from January 13 to May 17) and compared with the same period in 2019. Data on reperfusion therapy for acute infarction stroke were extracted monthly from January to April.
Results
The number of outpatients declined from 102,300 in 2019 to 75,154 in 2020 (26.54%), while the number of inpatients in the three tertiary Grade A hospitals decreased from 4641 to 3437 (25.94%). The latter trend showed a significant drop from the 3rd week to the 7th week. The number of patients in these hospitals decreased significantly, and a significant drop was seen in the neurology department. As usual, stroke was the most common disease observed; however, anxiety/depression and insomnia increased dramatically in the outpatient consultation department.
Conclusions
The results of our study revealed the effects of the COVID-19 pandemic in the clinical practice of neurology in Wenzhou during the outbreak. Understanding the pandemic’s trends and impact on neurological patients and health systems will allow for better preparation of neurologists in the future.
Keywords: COVID-19, Impact, Neurology department, Clinic practice, Healthcare systems
Introduction
The coronavirus disease 2019 (COVID-19) outbreak has resulted in a significant reallocation of health resources [1], and healthcare services are at the frontlines of this change [2]. The rapid spread of the pandemic has dramatically affected neurological clinical practice. Hospitals and departments have been quickly converted to COVID-19 care centers since the beginning of the outbreak. Patients with neurological conditions have still required clinical follow-up during the pandemic. However, visiting the hospital increases the risk of becoming infected with the virus. Therefore, the COVID-19 has led to an extreme shortage of healthcare availability [3].
Wenzhou is located in southeastern China, which has a population of 9.3 million. Many Wenzhou residents are business professionals and frequently travel from city to city for work. In the first stage of the pandemic, Wenzhou, which is not a provincial capital, became the most affected region outside of Hubei [4] due to the high volume of travel between it and Wuhan [5]. In total, there were 504 confirmed cases of COVID-19 in Wenzhou based on data published by the local health commission [6]. The three hospitals are comprehensive, tertiary Grade A hospitals in the center of Wenzhou, and each hospital covers multiple districts. To cope with the COVID-19 period, two of the three hospital districts were designated by the local government as treatment centers for COVID-19 patients.
The purpose of this study was to describe the changes in neurological clinical practice and the impact of the COVID-19 outbreak on the clinical management of neurological patients to find potential solutions to issues arising during the crisis in Wenzhou.
Materials and methods
Study design
This study was carried out retrospectively by analyzing the numbers and diagnoses of patients who requested the neurology department consultations in three tertiary Grade A hospitals in Wenzhou, Zhejiang. The three tertiary Grade A hospitals were selected from among eight tertiary Grade A hospitals using a computer-generated random number. Two of these hospitals were designated hospitals for COVID-19. Historical data of primary diagnosis were extracted from the electronic medical record system of hospitals from January 13 and May 17 in 2020 and for the corresponding period in 2019. In addition, data on reperfusion therapy for acute infarction stroke were extracted for each month from January to April. The diagnostic criteria of the diseases were based on the ICD-10 criteria. Two well-trained and experienced neurologists (JJ Z and Y L) confirmed the diagnoses.
Approval was obtained by the institutional review board, and informed consent was waived because of using anonymous data flows.
The first COVID-19 case in Wenzhou was identified on January 17, 2020. Limitations on public gatherings and home-based or centralized isolation were implemented on January 24. On February 1, restriction on residential areas and the control of public traffic were implemented by the government. On February 21, Wenzhou lifted its limitations on public gatherings and gradually resumed economic activities. Starting on April 30, all patients who were hospitalized were asked to undergo testing for COVID-19. The Spring Festival was on January 25, 2020, and February 5, 2019. We designated January 13–19 as the first week in our study for data collection.
Statistical analysis
Data are presented as actual numbers or as percentages. Data were analyzed by χ2 test to compare the groups. All statistical analyses were conducted using Statistical Package for the Social Sciences (SPSS) (version 23), with p values < 0.05 indicating statistical significance.
Results
The impact of the pandemic on outpatient activity
The overall number of outpatients in the three hospitals declined from 102,300 in 2019 to 75,154 (26.54%) in 2020. The mean age (SD) of outpatients was 54.6 years (16.3) in 2019 and 55.8 years (16.5) in 2020. Moreover, the percentage of outpatient patients from the Wenzhou urban area increased significantly in 2020 (p < 0.001) (Table 1). The number of outpatients showed a major drop from week 3 to week 7 due to the regional lockdown. (Fig. 1). The number of patients declined, but the distribution of reasons for requesting a neurology consultation changed significantly. As usual, stroke was the most common disease cited; however, compared with the proportion of patients, citing dizziness and a headache decreased significantly from 2019 to 2020 (p < 0.001). However, the number of patients with anxiety/depression, insomnia, and epilepsy increased dramatically (p < 0.001) (Table 1).
Table 1.
The outpatient of neurology department in the same period of 2019 and 2020 in three hospitals
| Subtype | Year | Age (x ± s) | Men (%) | Urban area (%) | Number | Percentage (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Stroke | Dizziness | Headache | Anxiety/depression | PN | Insomnia | Epilepsy | Dementia | PD | Others | ||||||
| Outpatient | 2019 | 54.6 ± 16.3 | 42.7 | 51.2 | 102300 | (16.9) | (16.2) | (16.0) | (13.7) | (10.3) | (9.4) | (3.3) | (2.3) | (5.3) | (6.6) |
| 2020 | 55.8 ± 16.5 | 43.2 | 55.8 | 75154 | (16.8) | (13.7) | (12.3) | (15.9) | (9.8) | (12.3) | (5.1) | (2.6) | (5.0) | (6.5) | |
| χ2 | 1.49 | 90.78 | 0.02 | 51.58 | 1.22 | 43.53 | 2.58 | 94.19 | 54.67 | 4.05 | 1.82 | 1.32 | |||
| P | 0.22 | 0.00 | 0.88 | 0.00 | 0.00 | 0.00 | 0.11 | 0.00 | 0.00 | 0.04 | 0.18 | 0.25 | |||
Pearson’s Chi-square test and relative p value were performed to compare the proportion in 2019 and 2020. p < 0.05 was considered statistically significant. PN: peripheral neuropathy, PD: Parkinson/parkinsonism diseases
Fig. 1.
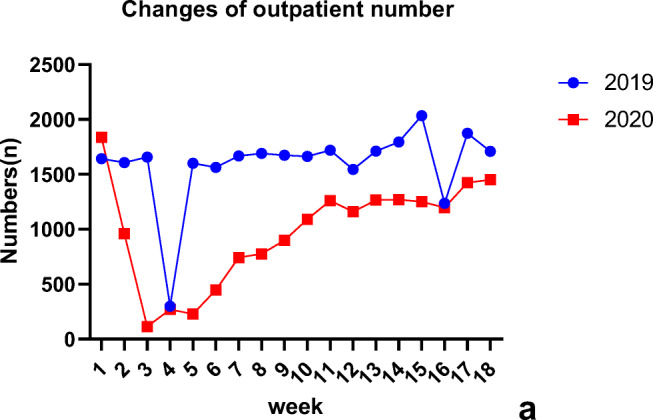
Changes of outpatient numbers in the same period of 2019 and 2020
Number and type of admissions
The number of inpatients in 2019 (4641) declined to 3437 in 2020 in three hospitals. The mean ages (SD) of the inpatients were 65.16 years old (13.9) in 2019 and 63.91 years old (15.6) in 2020 respectively. The total number of admissions during the 18 weeks decreased when compared with that in 2019, as shown in Fig. 2. However, starting in week 3 in 2020, a continuous reduction in the number of inpatients due to the pandemic and related restrictions was observed. Because hospital 1 and hospital 2 were designated COVID-19 hospitals, the decline in patients lasted longer (Fig. 2a, Fig. 2b). Table 2 shows the changes in the number of patients with stroke receiving reperfusion therapy each month from January to April. Comparing the total number of thrombolysis and thrombectomy cases in 2020 to that in 2019 shows a decreasing trend. During the 4-month period, February saw the highest decrease in thrombolysis and thrombectomy (66.67% and 68.18%, respectively). Stroke was still the primary cause of hospitalization, and the proportion increased in the three hospitals. The proportion of Parkinson’s disease/parkinsonism and peripheral neuropathy patients decreased significantly in hospital 1 and hospital 2, but not in hospital 3 (Fig. 3). According to an analysis of the mean value of time the admission process took, there was a significant increase in the duration of the admission process from April 30 from the 3 weeks before that date and in 2019 (p = 0.002; p = 0.001) (supplement) (Tables 2 and 3).
Fig. 2.
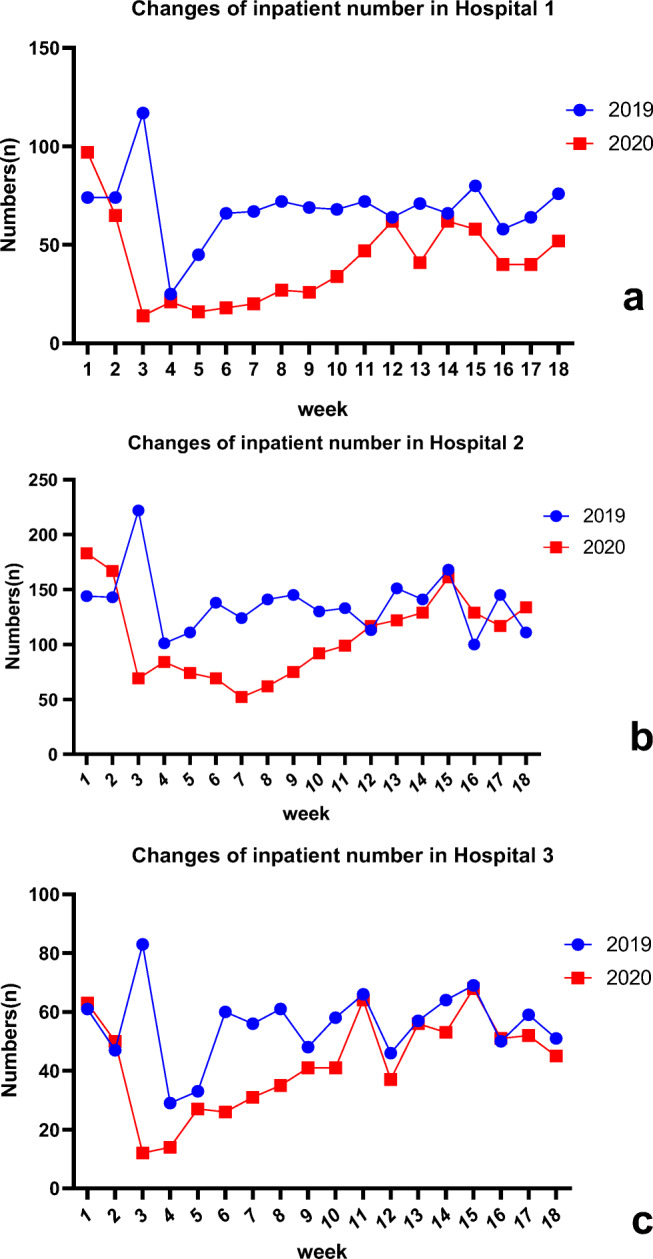
Changes of inpatient numbers in three hospitals in the same period of 2019 and 2020
Table 2.
Changes in thrombolysis and thrombectomy in three hospitals from January to April in 2019 and 2020
| Year | January | February | March | April | |
|---|---|---|---|---|---|
| Thrombolysis | 2019 | 36 | 45 | 44 | 32 |
| 2020 | 30 | 15* | 28* | 29 | |
| Percentage of change | − 16.67% | − 66.67% | − 36.36% | − 9.38% | |
| Thrombectomy | 2019 | 22 | 22 | 20 | 23 |
| 2020 | 18 | 7* | 19 | 22 | |
| Percentage of change | − 18.18% | − 68.18% | − 5.00% | − 4.35% |
*p < 0.0001 increases or decreases as compared with the same period of the previous year
Fig. 3.
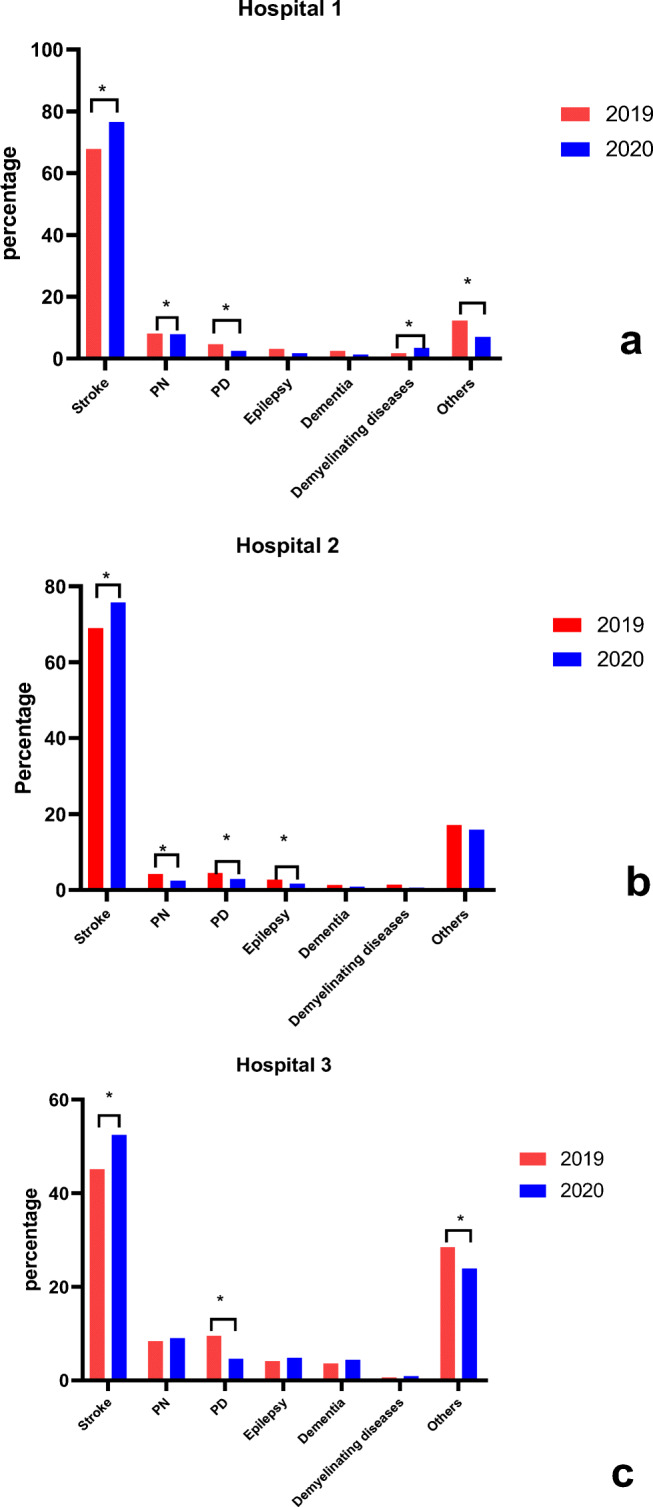
Changes of percentage of consultation reason in inpatient ward in three hospitals. *p < 0.05 was considered statistically significant. PN peripheral neuropathy, PD Parkinson/parkinsonism disease
Table 3.
Changes in types of reasons for requesting in neurology ward of three hospitals in the same period of 2019 and 2020
| Year | Stroke | Peripheral neuropathy | Parkinson/parkinsonism | Epilepsy | Dementia | Demyelinating diseases | Others | |
|---|---|---|---|---|---|---|---|---|
| Hospital 1 | 2019 | 824 | 98 | 56 | 38 | 29 | 21 | 149 |
| 2020 | 571 | 58 | 18 | 13 | 9 | 25 | 52 | |
| Hospital 2 | 2019 | 1697 | 103 | 108 | 66 | 32 | 34 | 421 |
| 2020 | 1465 | 46 | 56 | 32 | 17 | 11 | 308 | |
| Hospital 3 | 2019 | 435 | 81 | 92 | 40 | 35 | 6 | 275 |
| 2020 | 397 | 68 | 35 | 36 | 33 | 7 | 181 |
Discussion
The outbreak of COVID-19 has influenced every aspect of life globally [7, 8], especially the healthcare system. To the best of our knowledge, this is the first study that changes in the neurology department in tertiary public hospital centers during the COVID-19 pandemic. Our study revealed that the number of patients in the neurology department decreased significantly during the outbreak. Compared with the same time period in 2019, the number of medical clinics and admission numbers were reduced in our hospital, except for on holidays (Spring Festival and International Labor Day). As the restrictions were lifted, the number of outpatients and inpatients increased gradually to a similar level to that in the previous year.
To reduce the spread of COVID-19 in Wenzhou, the local government implemented multiple community containment strategies starting on January 24, 2020, including quarantine, traffic control isolation, and social distancing [4]. Isolation, quarantine, and the restriction of the movement prevented individuals from being exposed to the contagious disease [9]. The emphasis on these control measures might have unintentionally caused patients with milder neurological symptoms to delay or avoid seeking medical consultation due to fear of contacting the disease. Moreover, the healthcare system and, in particular, hospital emergency services were overloaded due to the large volume of patients suspected of having contracted COVID-19. This situation was exacerbated by public transport system restrictions, which discouraged patients who live far from hospitals from coming to the hospital for consultation. In addition, the latest technological advances in communication have allowed the use of telemedicine services, which can be used to meet the growing demand from patients for healthcare services [10]. The utility of tele-healthcare services encouraged doctors to provide simple medical services via hospital cloud-based consultation systems, thus also reducing clinical practice activities with patients.
The number of outpatients and inpatients decreased dramatically. However, the most common reason in this survey for seeking a consultation with the neurology department was stroke. Baracchini et al. noted a 50% reduction in minor strokes, TIAs, and transfers [11] from primary stroke units. However, other Italian experience revealed that no relevant difference was observed between 2019 and 2020 in the total number of patients admitted [12, 13]. We observed a 39% decrease in outpatient care and a 30% decrease in admission numbers, in accordance with previous reports [14, 15]. Patients with acute stroke had not come to the hospital for consultation previously; nonetheless, such visits became more frequent during this period. Isolation may have decreased the probability of friends and family members detecting that their relatives were suffering from cerebrovascular diseases. Stroke patients did not go to the hospital until their symptoms were more severe, which may have led to an increase in stroke-related disability cases. Another explanation may be that patients are reluctant to seek hospital care for fear of becoming infected. Moreover, if patients do seek medical care, they may consult with local health clinics, which are not stroke centers. Doctors may be diagnosing fewer cases of stroke or not referring all cases to the hospital as they did before. Furthermore, the drop in the absolute number of therapeutic interventions had a profound negative impact on stroke. Our concerning results should encourage governments, professional societies, and other relevant groups to take action to improve stroke knowledge related to the COVID-19 pandemic.
The proportion of patients with anxiety, depression, and insomnia increased significantly in our study. These results revealed that the pandemic had a negative effect on psychological status, which is consistent with the findings of previous studies [16, 17]. As the pandemic spread, there was a growing recognition of the psychiatric implications of the disease [18], including for healthcare workers [19] and the public [20]. Both infected and noninfected populations might be vulnerable as a result of the uncertain situation, which causes widespread anxiety, and social isolation. People were anxious that the healthcare system could not cope with the demand caused by the pandemic and the ensuing unemployment and financial problems due to the global economic crisis [21]. Another possible explanation may be related to information overload, including misinformation from different authorities, experts, and scientists [22]. Globally, disasters such as earthquakes, floods, and pandemics pose an extreme risk to the public’s physical and mental health [23]. Neurologists should be aware that prevention and early identification are just as important as treatment. It is vital to provide timely support through hotline teams, media, online education programs, and mental health professionals [24].
The reduction in the number of people seeking consultations due to dizziness and headache suggests that patients with relatively mild symptoms were less willing to go to the hospital during this period. The number of outpatient epilepsy patient is close to last year, but there was an increase from 2019 to 2020 in the percentage. Epilepsy is one of the most common neurological diseases globally and is a major cause of disability and mortality that requires long-term management. Both objective and subjective stress are believed to exacerbate seizures in some patients with epilepsy [25]. The outbreak was undoubtedly a stressful event and served as a relatively epilepsy-specific source of emotional stress that promoted seizures [26]. Moreover, anti-epileptic drug (AED) requires medical prescriptions and authorization [27] and could not be delivered to patients in time due to decreased supply and staff, resulting in an increase in the number of consultations. On the other hand, telephone consultations have been shown to be both effective and efficient in providing a remote epilepsy service [28], and physical exercise at home is recommended for people with epilepsy [29]; this has decreased the number of chronic epilepsy patients. The extent to which the reduction in admissions of other common neurological conditions, such as Parkinson’s disease and peripheral neuropathy, is related to the population’s behavior or to changes in the healthcare system is unclear. More research needs to be conducted to investigate their relationship.
This study has several limitations: (1) Our study was a descriptive study, with a limited sample size; thus, our results might not be representative of other regions. (2) Our study is a regional retrospective study, which might affect its universal validity, particularly regarding the criteria and triggers for neurology consultations and admission. (3) The findings in the present study might not be generalizable to other countries. Healthcare systems in different countries might handle the pandemic differently, and thus, the effects on clinical practice may differ as well.
Conclusion
The number and distribution of reasons for neurology department referrals have been affected by the COVID-19 outbreak. Our study shows that the impact of COVID-19 may affect the healthcare system, especially the neurology department. Our study may serve as a blueprint for further research and healthcare management.
Authors’ contributions
YG.C, Y.L, and KY.C are the main authors and assisted with distribution as well as data collation and analysis.
Formal analysis, Y.L and YG.C. Data curation, MM.S, XD.L, J.S, JJ.Z, XY.H, and ZC.C. Writing—original draft, YG.C and KY.C. Writing—review and editing, Y.L and KY.C. Supervision, KY.C.
Funding
The study was supported by funding from Research Program of Zhejiang Provincial Department of Education (Y202044361).
Compliance with ethical standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Patient consent
Informed consent was waived because of using anonymous data flows.
Ethics approval
This study was approved by the Ethics Committee of The Second Affiliated Hospital of Wenzhou Medical University.
Data sharing statement
All data and code generated or used during the study appear in the submitted article. No additional supplement is available.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yun-Gang Cao and Yan Li contributed equally to this work.
References
- 1.Tsai J, Wilson M. COVID-19: a potential public health problem for homeless populations. Lancet Public Health. 2020;5(4):e186–e187. doi: 10.1016/S2468-2667(20)30053-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Willan J, King AJ, Jeffery K, Bienz N. Challenges for NHS hospitals during covid-19 epidemic. BMJ. 2020;368:m1117. doi: 10.1136/bmj.m1117. [DOI] [PubMed] [Google Scholar]
- 3.French JA, Brodie MJ, Caraballo R, Devinsky O, Ding D, Jehi L, et al. Keeping people with epilepsy safe during the COVID-19 pandemic. Neurology. 2020;94(23):1032–1037. doi: 10.1212/WNL.0000000000009632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Han Y, Liu Y, Zhou L, Chen E, Liu P, Pan X, Lu Y. Epidemiological assessment of imported coronavirus disease 2019 (COVID-19) cases in the most affected city outside of Hubei Province, Wenzhou, China. JAMA Netw Open. 2020;3(4):e206785-e206785. doi: 10.1001/jamanetworkopen.2020.6785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395(10225):689–697. doi: 10.1016/S0140-6736(20)30260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Health Commission of Wenzhou Outbreak of novel coronavirus pneumonia in Wenzhou (daily updates) 2020; Available from: http://wjw.wenzhou.gov.cn/
- 7.Chen KY, Li T, Gong FH, Zhang JS, Li XK. Predictors of health-related quality of life and influencing factors for COVID-19 patients, a follow-up at one month. Front Psychiatry. 2020;11:668. doi: 10.3389/fpsyt.2020.00668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 2020;27(2):taaa020. doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dubas-Jakóbczyk K, Domagała A, Mikos M. Impact of the doctor deficit on hospital management in Poland: a mixed-method study. Int J Health Plann Manag. 2019;34(1):187–195. doi: 10.1002/hpm.2612. [DOI] [PubMed] [Google Scholar]
- 11.Baracchini C, Pieroni A, Viaro F, Cianci V, Cattelan AM, Tiberio I, Munari M, Causin F. Acute stroke management pathway during Coronavirus-19 pandemic. Neurol Sci. 2020;41(5):1003–1005. doi: 10.1007/s10072-020-04375-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Frisullo G, Brunetti V, Di Iorio R, Broccolini A, Caliandro P, Monforte M, Morosetti R, Piano C, Pilato F, Calabresi P, Della Marca G, STROKE TEAM Collaborators Effect of lockdown on the management of ischemic stroke: an Italian experience from a COVID hospital. Neurol Sci. 2020;6:1–5. doi: 10.1007/s10072-020-04545-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Caproni S, Di Schino C, Costantini F, Parisi G, Colosimo C. Letter to the editor: "COVID-19 does not reduce stroke-related emergencies". Acta Neurol Belg. 2020;120(5):1259–1260. doi: 10.1007/s13760-020-01444-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thornton J. Stroke: “striking reductions” are seen in number of people with symptoms seeking help. BMJ. 2020;269:m1406. doi: 10.1136/bmj.m1406. [DOI] [PubMed] [Google Scholar]
- 15.Bersano A, Pantoni L. On being a neurologist in Italy at the time of the COVID-19 outbreak. Neurology. 2020;94:905–906. doi: 10.1212/WNL.0000000000009508. [DOI] [PubMed] [Google Scholar]
- 16.Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;S0889–1591(20):30845-X. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Voitsidis P, Gliatas I, Bairachtari V, Papadopoulou K, Papageorgiou G, Parlapani E, et al. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Res. 2020;289:113076–113076. doi: 10.1016/j.psychres.2020.113076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.(2020) Send in the therapists? Lancet Psychiatry 7(4):291. 10.1016/S2215-0366(20)30102-4 [DOI] [PMC free article] [PubMed]
- 19.Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. 2020;368:m1211. doi: 10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]
- 20.Liu X, Luo WT, Li Y, Li CN, Hong ZS, Chen HL, Xiao F, Xia JF. Psychological status and behavior changes of the public during the COVID-19 epidemic in China. Infect Dis Poverty. 2020;9(1):58. doi: 10.1186/s40249-020-00678-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chaves C, Castellanos T, Abrams M, Vazquez C. The impact of economic recessions on depression and individual and social well-being: the case of Spain (2006–2013) Soc Psychiatry Psychiatr Epidemiol. 2018;53(9):977–986. doi: 10.1007/s00127-018-1558-2. [DOI] [PubMed] [Google Scholar]
- 22.de Girolamo G, Cerveri G, Clerici M, Monzani E, Spinogatti F, Starace F et al (2020) Mental health in the coronavirus disease 2019 emergency-the Italian response. JAMA Psychiatry. 10.1001/jamapsychiatry.2020.1276 [DOI] [PubMed]
- 23.North CS, Pfefferbaum B. Mental health response to community disasters: a systematic review. JAMA. 2013;310(5):507–518. doi: 10.1001/jama.2013.107799. [DOI] [PubMed] [Google Scholar]
- 24.Xiang Y-T, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7(3):228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baldin E, Hauser WA, Pack A, Hesdorffer DC. Stress is associated with an increased risk of recurrent seizures in adults. Epilepsia. 2017;58(6):1037–1046. doi: 10.1111/epi.13741. [DOI] [PubMed] [Google Scholar]
- 26.Huang S, Wu C, Jia Y et al (2020) COVID-19 outbreak: the impact of stress on seizures in patients with epilepsy. Epilepsia. 10.1111/epi.16635 [DOI] [PMC free article] [PubMed]
- 27.Vancini RL, de Lira CAB, Andrade MS, Arida RM (2020) CoVID-19 vs. epilepsy: it is time to move, act, and encourage physical exercise. Epilepsy Behav:107154–107154. 10.1016/j.yebeh.2020.107154 [DOI] [PMC free article] [PubMed]
- 28.Kissani N, Lengané YTM, Patterson V, et al. Telemedicine in epilepsy: how can we improve care, teaching, and awareness? Epilepsy Behav. 2020;103(Pt A):106854. doi: 10.1016/j.yebeh.2019.106854. [DOI] [PubMed] [Google Scholar]
- 29.Kai SJRA. Ameliorating effects of traditional Chinese medicine preparation, Chinese materia medica and active compounds on ischemia/reperfusion induced cerebral microcirculatory disturbances and neuron damage. Acta Pharm Sin B. 2015;5(1):8–24. doi: 10.1016/j.apsb.2014.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]


