Abstract
Background & Aims
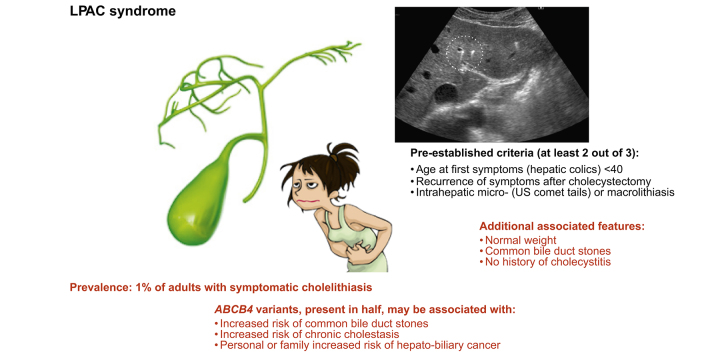
Low-phospholipid-associated cholelithiasis (LPAC) syndrome, a rare genetic form of intrahepatic cholelithiasis in adults, is still poorly understood. We report the results of the largest-ever case-control study of patients with LPAC syndrome aiming to assess the prevalence, clinical features, and comorbidities of the disease.
Methods
We included all LPAC cases diagnosed between 2001 and 2016 in 11 French centres. Controls consisted of all patients who underwent a cholecystectomy for common gallstone disease in a single non-academic centre over 1 year. A logistic regression analysis was used to identify the clinical features associated with LPAC syndrome across several patient strata with increasing levels of diagnostic confidence. The ratio between the incident cases of LPAC syndrome and the total number of cholecystectomies for gallstones was used to assess the relative prevalence of the disease.
Results
In this study, 308 cases and 206 controls were included. LPAC syndrome accounted for 0.5–1.9% of all patients admitted with symptomatic gallstone disease. Age at first symptoms <40 years, absence of overweight, persistence of symptoms after cholecystectomy, intrahepatic micro- or macrolithiasis, common bile duct (CBD) lithiasis, and no history of cholecystitis were independently associated with LPAC diagnosis. ATP-binding cassette subfamily B member 4 (ABCB4) variants, present in 46% of cases, were associated with CBD lithiasis, chronic elevation of gamma-glutamyltransferase (GGT), and personal or family history of hepato-biliary cancer.
Conclusions
In this case-control study, LPAC syndrome accounted for approximately 1% of symptomatic cholelithiasis in adults. In addition to pre-established diagnostic criteria, normal weight, CBD lithiasis, and no history of cholecystitis were significantly associated with the syndrome. ABCB4 gene variations in patients with LPAC were associated with CBD lithiasis, chronic cholestasis, and a personal or family history of hepato-biliary cancer.
Lay summary
In the largest case-control study ever conducted in patients with LPAC syndrome, a rare genetic form of intrahepatic cholelithiasis in young adults, LPAC syndrome was found in approximately 1% of all patients admitted to the hospital for symptomatic gallstones and, in addition to the pre-established characteristics of the syndrome (age at first symptoms <40 years, recurrence of symptoms after cholecystectomy, and/or imaging evidence of intrahepatic microlithiasis), was associated with lower BMI, higher prevalence of common bile duct stones, and lower incidence of acute cholecystitis. ABCB4 gene variants, which were detected in about half of cases, were associated with common bile duct stones and a personal or family history of hepato-biliary cancer.
Keywords: LPAC, ABCB4, Cholestasis, Pregnancy, Metabolic syndrome, Cancer
Abbreviations: ABCB4, ATP-binding cassette subfamily B member 4; CBD, common bile duct; ERCP, endoscopic retrograde cholangiopancreatography; FDR, false discovery rate; GGT, gamma-glutamyltransferase; ICP, intrahepatic cholestasis of pregnancy; LPAC, low-phospholipid-associated cholelithiasis; MRCP, magnetic resonance cholangiopancreatography; UDCA, ursodeoxycholic acid
Graphical abstract
Highlights
-
•
Low-phospholipid-associated cholelithiasis (LPAC) syndrome affects approximately 1% of adults with symptomatic cholelithiasis.
-
•
Normal weight, common bile duct stones, and lack of cholecystitis are clinical features significantly associated with this syndrome.
-
•
ABCB4 variants in patients with LPAC may be associated with an increased personal or family risk of hepato-biliary cancer.
Introduction
Low-phospholipid-associated cholelithiasis (LPAC) syndrome is a rare form of intrahepatic cholelithiasis affecting mainly young adults and characterised by recurrent attacks of biliary colic, acute cholangitis, or pancreatitis that typically recur after cholecystectomy.1,2 This condition has causally been linked to a defect of phospholipid canalicular secretion into bile, leading to impaired solubilisation of biliary cholesterol that precipitates in the form of crystals in canaliculi and intrahepatic bile ducts. Germ-line mutations in the sequence of the ATP-binding cassette subfamily B member 4 (ABCB4) gene, which encodes the phospholipid floppase multidrug resistance type 3, have been reported in 30–50% of patients with this condition,[2], [3], [4], [5], [6] thus including LPAC syndrome in the different disease manifestations associated with ABCB4 variants.7
LPAC syndrome is an elusive clinical entity, and its prevalence remains unknown.8,9 It is admitted that a diagnosis of LPAC syndrome should be considered when at least 2 of the following criteria are met:
-
•
onset of symptoms before the age of 40 years;
-
•
recurrence of symptoms after cholecystectomy; and
-
•
intrahepatic microlithiasis characterised by comet-tail images, hyperechoic foci, or biliary sludge on liver ultrasound.2
These criteria, however, have been proposed based on a very limited number of cases and controls with the aim of predicting ABCB4 gene mutations, which, in fact, are lacking in half of the patients or more.3 As a result, they may not encompass the overall clinical spectrum of the disease, and there is still a need for a more extensive phenotypic characterisation of patients with this syndrome.
Early diagnosis of LPAC syndrome is of crucial importance, as the management of this condition is different from that of common gallstone disease. LPAC syndrome is an intrahepatic cholelithiasis by nature. Accordingly, cholecystectomy as a first strategy is not rational, whereas dramatic reduction in symptoms and complications has been widely observed in response to ursodeoxycholic acid (UDCA) therapy. In addition, LPAC patients may require specific attention and monitoring, as there is a potential risk of intrahepatic cholestasis of pregnancy (ICP) in women and of chronic cholestatic disease and related complications, including cirrhosis and hepato-biliary cancers, in men and women.
Herein, we report the results of the largest retrospective cohort and case-control study of patients with LPAC syndrome to date. Our aims were to assess the prevalence rate of LPAC syndrome among adult patients admitted for symptomatic gallstone disease; define more precisely the characteristics of this condition based on a large panel of patients and controls; evaluate the influence of ABCB4 gene variations on disease phenotype; and explore the significance of key comorbidities, such as overweight, metabolic syndrome, ICP, and hepato-biliary cancer.
Patients and methods
Case and control populations
All patients who had been considered for a diagnosis of LPAC syndrome between 2001 and 2016 within 11 French hospitals (1 academic referral centre and 10 non-academic hospitals) were included in this retrospective cohort study. To be eligible, the patients had to fulfil at least 2 of the following features:
-
•
onset of symptoms before the age of 40 years;
-
•
recurrence of symptoms after cholecystectomy;
-
•
intrahepatic cholelithiasis, including either macro- or microlithiasis, the latter being defined on liver ultrasound by the presence of comet-tail images, hyperechoic foci, or biliary sludge alongside intrahepatic bile ducts.2
The entire case population constituted the first diagnostic stratum for primary analysis. Subpopulations of patients with higher levels of diagnostic confidence, including those with typical imaging features (second diagnostic stratum) and those with both typical imaging features and potentially pathogenic ABCB4 variant (third diagnostic stratum), were used for specificity analyses.
The control population consisted of all participants who underwent a cholecystectomy for gallstone disease in 1 of the participating non-academic hospitals (Bry-sur-Marne, France) during the year 2013. This was supported by the availability and quality of locally recorded data and the proper representativeness of the sample population. The year 2013 was chosen to ensure a minimum 4-year follow-up period after surgery. All patients who underwent cholecystectomy for other gallbladder diseases, including cholangiocarcinoma and HIV- or sickle-cell-anaemia-associated biliary tract disorders, were excluded from the control population.
This study was conducted in accordance with the Declaration of Helsinki. The protocol was approved by the local ethical committee. Informed consent was obtained from all participants with LPAC syndrome and controls.
Data collection
Data collection was performed retrospectively using the same standardised case report form. The recorded variables included birthdate; gender; height; weight at diagnosis; date of symptom onset; date of diagnosis; acute complications: biliary colic (with or without concomitant rise in biochemical liver tests, including aminotransferases, alkaline phosphatase, gamma-glutamyltransferase [GGT], and total and conjugated bilirubin), acute cholangitis, liver abscess, acute pancreatitis, acute cholecystitis, sporadic jaundice, and/or pruritus; biochemical liver tests outside symptomatic periods; radiological investigations, including ultrasound with or without a liver expert operator, CT scan, magnetic resonance cholangiopancreatography (MRCP) or endoscopic retrograde cholangiopancreatography (ERCP), or endoscopic ultrasound, and corresponding reports: gallbladder stones or sludge, intrahepatic microlithiasis (defined as comet-tail images, hyperechoic micro-spots, or sludge), intra- or extrahepatic macrolithiasis (defined as hyperechoic spots with acoustic shadowing in ultrasound, high-intensity signal on T1 weighting in MRCP, or gallstones identified and removed during ERCP) with or without related biliary dilatation, liver dysmorphia, and focal hepatic lesions; history of treatment: UDCA therapy, cholecystectomy, endoscopic sphincterotomy, hepatectomy, and biliary-enteric anastomosis; recurrence of acute complications after cholecystectomy; personal history of metabolic syndrome as defined by at least 1 of the following conditions: diabetes, hypertension, or dyslipidaemia; family history of cholelithiasis; and personal or family history of ICP and hepato-biliary cancer (cholangiocarcinoma or hepatocellular carcinoma).
Regarding control participants, every patient was contacted and invited to provide additional information when not found in medical records, such as evolution of symptoms after cholecystectomy, family history of cholelithiasis, and personal or family history of ICP or hepato-biliary cancer. In addition, volunteers were offered an expert ultrasound scan of the liver performed by an experienced radiologist (M.-P.H.) who is used to look for and detect ultrasound signs of intrahepatic microlithiasis and who has already been involved as a liver ultrasound specialist in a previous study on LPAC syndrome.4
ABCB4 gene analysis
ABCB4 is currently the only gene causally linked with LPAC syndrome. Other biliary transporter genes, including ABCB11 for example, may play an additional role, but their pathogenicity is still uncertain. Accordingly, we limited this study to the potentially pathogenic variants of ABCB4. ABCB4 was screened by Sanger sequencing until 2010, and then by next-generation sequencing. With regard to the latter, exons and flanking intronic sequences of ABCB4 were captured from fragmented genomic DNA with the SeqCap EZ enrichment protocol (Roche NimbleGen). Paired-end massively parallel sequencing was achieved on a MiSeq platform (Illumina). Bioinformatic analysis was performed using the SOPHiA Genetics DDM pipeline®. Variants were confirmed either by Sanger sequencing (BigDye™ Terminator Sequencing Kit; SeqScape® version 2.7 software; Applied Biosystems) or by quantitative PCR (SYBR Green; ViiA™ 7 real-time PCR system; Applied Biosystems). ABCB4 variations were defined as potentially pathogenic variants when they met 1 of the following criteria: nonsense single-point variation; frameshift variation resulting from the deletion or insertion of 1 or several nucleotides; rare (<1%) missense single-point variation previously reported to be associated with the disease or to alter significantly the function of ABCB4 transporter either in vivo, in vitro, or as predicted by mutation-prediction software, including SIFT,10 PolyPhen-2,11 MutationTaster,12 Alamut® Visual (Interactive Biosoftware, Rouen, France), InterVar,13 and MutPred.14
Statistical analysis
Qualitative and quantitative variables were expressed as n (%) and median (range), respectively. Comparisons were performed using Fisher’s exact test for qualitative variables and Mann-Whitney U-test for quantitative variables. The variables individually associated with LPAC syndrome were subjected to a multiple logistic regression analysis, and independent variables were identified using a backward stepwise selection procedure. Results were expressed as false discovery rate (FDR) LogWorth (–log10[FDR p value]) or odds ratios and corresponding 95% CIs. To avoid convergence failures, some interacting variables were grouped as follows: intrahepatic comet tails or hyperechoic foci, intrahepatic sludge, and intrahepatic micro- or macrolithiasis were designated as features of intrahepatic lithiasis; attacks of hepatic colic with transaminase raise, acute pancreatitis, imaging evidence of common bile duct (CBD) lithiasis, and endoscopic sphincterotomy were designated as clinical and/or imaging evidence of CBD lithiasis. The primary analysis was performed based on the whole case population (first diagnostic stratum). The robustness of the results was assessed using specificity analyses performed in 2 subpopulations of cases with increasing levels of diagnostic confidence (i.e. the second and third diagnostic strata) (see subpopulations in "Case and control population" paragraph). To complete these results, the features associated with the presence of ABCB4 variants were identified in the case population with available genetic testing using a multiple logistic regression analysis. The relative prevalence of LPAC syndrome was estimated in each centre by the ratio between the total number of cases diagnosed during the 5-year period preceding the last patient included and the total number of patients who underwent a cholecystectomy for symptomatic gallstone disease during this period. The latter was evaluated based on the French hospital discharge database (Programme de Médicalisation des Systèmes d'Information) using the International Statistical Classification of Diseases and Related Health Problems, 10th Revision and the following research criteria: cholecystectomy, gallstone, and hepatic colic. Analyses were performed with SPSS software version 24.0 (SPSS Inc., Chicago, IL, USA). All tests were 2-sided, and p values of <0.05 were considered to indicate statistical significance.
Results
Disease prevalence
In total, 514 patients (308 patients with LPAC syndrome and 206 controls) were included. Three quarters of LPAC patients (n = 233) were recruited from the tertiary referral centre (Saint-Antoine Hospital, Paris, France). The remaining quarter of LPAC patients (n = 73) was distributed across non-academic hospitals as follows: Bry-sur-Marne (37 patients), Orléans (13 patients), Aix-en-Provence (11 patients), Saint-Denis (4 patients), Créteil (2 patients), Montfermeil (2 patients), Marne-la-Vallée (1 patients), Lannion (1 patients), Pau (1 patients), and La Rochelle (1 patients). In Saint-Antoine Hospital, 101 patients with LPAC syndrome were diagnosed from 2012 to 2016, while 1,338 patients underwent a cholecystectomy for cholelithiasis during the same period. Accordingly, a 7.5% (101:1,338) prevalence rate of LPAC syndrome among adult patients with symptomatic gallstone disease was estimated from this tertiary referral centre. By contrast, the prevalence rate estimated from the 3 main non-academic hospitals (Bry-sur-Marne, Orléans, and Aix-en-Provence) was 1.9% (17:891), 0.5% (8:1,525), and 0.5% (4:791), respectively. LPAC syndrome, therefore, accounted for approximately 1% of patients admitted in non-academic centres for symptomatic cholelithiasis.
Disease characteristics and comorbidities
The characteristics of the LPAC patients are summarised in Table 1. This cohort consisted of 308 cases of whom 85% had undergone a cholecystectomy before diagnosis. LPAC patients were mainly female (77%) with a median age of 27 years at first symptoms and 36 years at diagnosis. Twelve percent of patients experienced first symptoms before the age of 18 (minimum, 8) years and 12% after the age of 40 years (maximum, 69). Median BMI was 23 kg/m2. Almost all patients (95%) experienced attacks of hepatic colic. Concomitant elevation of transaminases, acute cholangitis, pancreatitis, and cholecystitis were reported in 47%, 24%, 14%, and 7% of cases, respectively. Intrahepatic micro- or macrolithiasis, gallbladder lithiasis (when information available), and CBD lithiasis were evidenced in 91%, 31%, and 26%, respectively. A history of cholecystectomy, endoscopic sphincterotomy, hepatectomy, or biliary-enteric anastomosis was reported in 85%, 32%, 6%, and 3%, respectively. Recurrence of biliary symptoms after cholecystectomy was reported in 86% at diagnosis. Overweight, obesity, hypercholesterolaemia, hypertension, and diabetes were present at diagnosis in 30%, 13%, 8%, 7%, and 4%, respectively. No case of cirrhosis was observed. A history of ICP was reported in 42% of women who had been pregnant. A family history of cholelithiasis was reported in 61% of index cases and in 48% when only first-degree relatives were considered.
Table 1.
Characteristics of LPAC cases and controls.
| Characteristics | Cases (n = 308) | Controls (n = 206) | p value |
|---|---|---|---|
| Demographics | |||
| Female gender | 237/308 (77.0) | 128/206 (62.1) | <0.001 |
| Age at first symptoms (yr) | 27 (6–76) | 47 (12–93) | <0.001 |
| Age at diagnosis (yr) | 36 (14–80) | 47 (12–93) | <0.001 |
| Age at cholecystectomy (yr) | 30 (6–76) | 49 (14–93) | <0.001 |
| BMI at diagnosis (kg/m2) | 23 (16–43) | 27 (19–58) | <0.001 |
| Clinical manifestations | |||
| First symptoms before the age of 40 yr | 273/308 (88.6) | 72/206 (35.0) | <0.001 |
| Hepatic colic | 289/304 (95.1) | 187/206 (90.8) | 0.057 |
| Hepatic colic with transaminase elevation | 127/271 (46.9) | 37/206 (18.0) | <0.001 |
| Acute cholangitis | 73/301 (24.3) | 14/206 (6.8) | <0.001 |
| Acute cholecystitis | 22/297 (7.4) | 86/206 (41.8) | <0.001 |
| Acute pancreatitis | 42/299 (14.1) | 28/206 (13.6) | 0.885 |
| Recurrence after cholecystectomy | 216/250 (86.4) | 22/166 (13.3) | <0.001 |
| Imaging features | |||
| Gallbladder lithiasis | 32/102∗ (31.4) | 202/206 (98.1) | <0.001 |
| Intrahepatic lithiasis | 271/299 (90.6) | 0/206 (0.0) | <0.001 |
| Intrahepatic microlithiasis | 228/299 (76.3) | 0/206 (0.0) | <0.001 |
| Intrahepatic macrolithiasis | 130/299 (43.5) | 0/206 (0.0) | <0.001 |
| Common bile duct lithiasis | 78/299 (26.1) | 14/206 (6.8) | <0.001 |
| Comorbidities and familial history | |||
| Overweight | 69/230 (30.0) | 126/203 (62.1) | <0.001 |
| Obesity | 29/230 (12.6) | 61/203 (30.1) | <0.001 |
| Diabetes | 10/228 (4.4) | 27/205 (13.2) | 0.001 |
| Hypercholesterolaemia | 18/228 (7.9) | 40/205 (19.5) | <0.001 |
| Hypertension | 16/228 (7.0) | 60/205 (29.3) | <0.001 |
| ICP in women with a history of pregnancy | 54/129 (41.9) | 2/79 (2.5) | <0.001 |
| History of cholelithiasis in first-degree relatives | 138/288 (47.9) | 57/166 (34.3) | 0.005 |
| Personal/family history of hepato-biliary cancer | 14/284 (4.9) | 0/206 (0.0) | <0.001 |
| Surgery and endoscopy | |||
| Cholecystectomy | 252/296 (85.1) | 206/206 (100.0) | <0.001 |
| Endoscopic sphincterotomy | 95/300 (31.7) | 20/206 (9.7) | <0.001 |
| Hepatectomy | 17/298 (5.7) | 0/206 (0.0) | <0.001 |
| Biliary-enteric anastomosis | 9/297 (3.0) | 0/206 (0.0) | 0.013 |
Qualitative variables are expressed as n/N (%) and quantitative variables as median (range). The p values for Mann-Whitney U test or Fisher’s exact tests. ICP, intrahepatic cholestasis of pregnancy; LPAC, low-phospholipid-associated cholelithiasis.
Data not available in 206 cases who had a cholecystectomy before diagnosis with no further details.
A personal or family history of hepato-biliary cancer was recorded in 14 out of 284 (4.9%) patients. All liver cancers reported in index patients (n = 5; 2.4 per 1,000 patient-years) occurred beyond the age of 50 years (median age 60 years) and were intrahepatic cholangiocarcinomas developed on a symptomatic macrolithiasis form of the disease with segmental dilatation of large intrahepatic bile ducts filled with gallstones. Sporadic cases of cholangiocarcinoma, or hepatocellular carcinoma complicating cholestatic or idiopathic cirrhosis, were reported in some first- or second-degree relatives (n = 9). All hepato-biliary cancers reported in index cases or relatives are summarised in Table 2.
Table 2.
Hepato-biliary cancers in unrelated index cases and relatives.
| Case no. | Patient | Gender (family link for relatives) | Age (yr) | Cancer (location or context) |
|---|---|---|---|---|
| LPAC0004 | Index | Female | 59 | Cholangiocarcinoma (intrahepatic) |
| LPAC0019 | Index | Female | 74 | Cholangiocarcinoma (intrahepatic) |
| LPAC0043 | Index | Male | 60 | Cholangiocarcinoma (intrahepatic) |
| LPAC0063 | Index | Female | 55 | Cholangiocarcinoma (intrahepatic) |
| LPAC0122 | Index | Female | 68 | Cholangiocarcinoma (intrahepatic) |
| LPAC0006 | Relative | Female (mother) | 53 | Hepatocellular carcinoma (cirrhosis) |
| LPAC1002 | Relative | Male (uncle) | 62 | Cholangiocarcinoma (NS) |
| LPAC0048 | Relative | Female (grandmother) | n.a. | Cholangiocarcinoma (NS) |
| LPAC0054 | Relative | Male (first cousin) | n.a. | Cholangiocarcinoma (CBD) |
| LPAC0065 | Relative | Male (father) | 75 | Cholangiocarcinoma (intrahepatic) |
| LPAC0238 | Relative | Male (father) | n.a. | Cholangiocarcinoma (NS) |
| LPAC1001 | Relative | Female (grandmother) | n.a. | Hepatocellular carcinoma (cirrhosis) |
| LPAC0073 | Relative | Female (sister) | 46 | Cholangiocarcinoma (NS) |
| LPAC0072 | Relative | Female (sister) | n.a. | Hepatocellular carcinoma (cirrhosis) |
CBD, common bile duct; LPAC, low-phospholipid-associated cholelithiasis; n.a., not available; NS, not specified.
Disease-specific features
The 308 cases were compared with 206 control participants who consecutively underwent a cholecystectomy for gallstone disease over 1 year in a single non-academic centre (Table 1). In a univariate analysis, the clinical features associated with LPAC syndrome included female gender, younger age at first symptoms (with a confirmed optimal discriminating threshold of 40 years), younger age at diagnosis, lower BMI at diagnosis, hepatic colic with transaminase elevation, absence of cholecystitis history, acalculous gallbladder, intrahepatic micro- or macrolithiasis, CBD lithiasis, recurrence of symptoms after cholecystectomy, acute cholangitis, history of endoscopic sphincterotomy, history of hepatectomy, absence of metabolic syndrome, history of ICP, and first-degree relative history of cholelithiasis.
In the primary multivariate analysis, including the entire case population (first diagnostic stratum), the features independently associated with a diagnosis of LPAC syndrome included imaging evidence of intrahepatic micro- or macrolithiasis, recurrence of symptoms after cholecystectomy, age at first symptoms before 40 years (all 3 features consisting in historical criteria of LPAC syndrome), absence of overweight, and clinical and/or imaging evidence of CBD lithiasis (Table 3). Similar results were obtained across the second (patients with typical imaging features) and third (patients with typical imaging features and ABCB4 variant) more specific diagnostic strata from the case population (Table 3), the absence of acute cholecystitis history being identified as an additional independent associated feature in these 2 subgroups with higher levels of diagnostic confidence. When CBD lithiasis was defined based on imaging features only, it remained significantly and independently associated with the diagnosis of LPAC syndrome within all diagnostic strata (Table S1).
Table 3.
Multiple regression analysis of clinical features associated with LPAC diagnosis.
| Clinical features | FDR LogWorth (95% CI) |
||
|---|---|---|---|
| All cases (n = 308) | Cases with typical imaging features (n = 272) | Cases with typical imaging features and ABCB4 variant (n = 106) | |
| Imaging evidence of intrahepatic micro- or macrolithiasis | 53.8 (52.1–55.5) | — | — |
| Recurrence of symptoms after cholecystectomy | 15.3 (14.8–15.8) | 28.0 (27.1–28.8) | 13.7 (13.0–14.3) |
| Age at first symptoms before 40 yo | 4.8 (4.4–5.1) | 15.5 (14.8–16.2) | 10.9 (10.4–11.4) |
| Clinical and/or imaging evidence of CBD lithiasis | 6.3 (5.9–6.7) | 2.5 (2.2–2.8) | 2.4 (2.1–2.7) |
| No history of obesity or overweight | 2.0 (1.8–2.2) | 6.8 (6.4–7.2) | 6.0 (5.6–6.4) |
| No history of acute cholecystitis | NS | 6.0 (5.7–6.4) | 3.3 (3.0–3.6) |
The FDR LogWorth is a quantitative measure of how strong the association is between diagnosis and clinical features in multiple logistic regression analysis. It is defined as –log10(FDR p value for the likelihood ratio Chi-square test). A value that exceeds 2 is significant at the 0.01 level. ABCB4, ATP-binding cassette subfamily B member 4; CBD, common bile duct; FDR, false discovery rate; LPAC, low-phospholipid-associated cholelithiasis; NS, not significant at the 0.05 level.
ABCB4-related features
The relationships between ABCB4 variations and the clinical features and comorbidities of LPAC syndrome were assessed from the entire cohort. ABCB4 gene variations were detected in 122 (45%) out of 269 LPAC patients with a genotyping test available (87% of all patients), including 63% missense variants and 37% nonsense or frame-shift truncating variants (for more details, see Table S2). The vast majority (95%) of ABCB4 variants were in the heterozygous state. In a univariate analysis, the features associated with the presence of ABCB4 gene variations included history of CBD lithiasis (34.5% vs. 20.0%; p = 0.008), history of endoscopic sphincterotomy (39.3% vs. 25.5%; p = 0.017), chronic elevation of GGT (33.3% vs. 14.2%; p <0.001), and personal or family history of hepato-biliary cancer (10.1% vs. 2.2%; p = 0.011). Patients with ABCB4 pathogenic variants showed more frequently chronic elevation of transaminases than those without (16.1% vs. 8.5%), but the difference did not reach the level of significance (p = 0.065). In the female population with a pregnancy history, no significant association was found between a history of ICP and the presence of ABCB4 gene variations (48.4% vs. 40.4%; p = 0.40). In a multivariate analysis adjusted for age and sex, the features independently associated with the presence of ABCB4 gene variation were a history of CBD lithiasis, a chronic elevation of GGT, and a personal or family history of hepato-biliary cancer (Table 4). Among all patients exhibiting ABCB4 gene variations, those with truncating variants were not different from those with missense variants, except for a more frequent family history of symptomatic cholelithiasis in first-degree relatives (71.1% vs. 45.5%; p = 0.012).
Table 4.
Multiple regression analysis of clinical features associated with ABCB4 gene variations in patients with LPAC syndrome.
| Clinical features | Estimate | SE | OR (95% CI) | p value |
|---|---|---|---|---|
| History of CBD lithiasis | 0.57 | 0.17 | 3.1 (1.6–6.2) | <0.001 |
| Chronic elevation of GGT | 0.58 | 0.18 | 3.2 (1.6–6.6) | 0.001 |
| Personal/family history of hepato-biliary cancer | 0.80 | 0.38 | 5.0 (1.2–25.5) | 0.026 |
The p values for the likelihood ratio Chi-square test. ABCB4, ATP-binding cassette subfamily B member 4; CBD, common bile duct; GGT, gamma-glutamyltransferase; LPAC, low-phospholipid-associated cholelithiasis; OR, odds ratio.
Expert ultrasound examination of controls
A third of controls (68/206) accepted to have an expert ultrasound of the liver around 2 years after cholecystectomy. One of them (1.5% of screened controls, a percentage in keeping with the prevalence estimated previously) showed typical signs of LPAC syndrome with diffuse intrahepatic comet-tail images and hyperechoic foci. This was a male aged 44 years at first symptoms. He reported recurrent hepatic colic after cholecystectomy and was retrospectively diagnosed with LPAC syndrome. He had no ABCB4 gene variation.
Discussion
The present study is the largest-ever cohort and case-control study of patients with LPAC syndrome. It provides the first estimation of the overall prevalence of this condition among patients with symptomatic cholelithiasis. We found an approximately 1% prevalence rate of LPAC syndrome in adult patients admitted to non-academic healthcare centres for symptomatic gallstone disease. Not surprisingly, a higher prevalence was observed in the tertiary centre participating in this study, likely because of a referral bias. A relative rarity of the LPAC syndrome is what one would expect from a genetic disorder. However, if we consider that 10–20% of individuals in the general population are gallstone carriers; that 10–20% of them are symptomatic;15,16 and, based on current findings, that 1% of the latter have LPAC syndrome, we can estimate that the overall prevalence of this syndrome is approximately 10–40 per 100,000, which is more frequent than previously anticipated. The real prevalence is likely even higher, as this disease is still poorly known, underdiagnosed, and characterised by a broad clinical spectrum. Of particular importance with respect to patients’ care, considering that 100,000 individuals undergo cholecystectomy each year in France17 and assuming that this procedure is likely to be ineffective in individuals with intrahepatic lithiasis, such as LPAC patients, we postulate that cholecystectomy could be spared in a thousand of them if LPAC syndrome was correctly diagnosed.
In this large case-control study, new clinical features associated with LPAC syndrome have been found, including CBD lithiasis, normal weight, and no history of acute cholecystitis. These results notably suggest that, in young patients presenting with CBD stones, a careful and expert ultrasound exploration of the liver should absolutely be performed to rule out an intrahepatic microlithiasis before any decision of cholecystectomy. Although the presumed failure of cholecystectomy vs. UDCA to cure LPAC syndrome remains non-evidence based (a randomised trial comparing these 2 options in the future seems more than unlikely), the use of a non-invasive pharmacological approach for this hepato-biliary disease not limited to the gallbladder makes more sense. Based on our clinical experience, we recommend against first-line surgery in patients diagnosed with LPAC syndrome and gallbladder stones. In these patients, once UDCA therapy has been initiated, the need for cholecystectomy in our experience is anecdotal. In fact, as shown in this study, a third only of LPAC patients had authenticated stones in the gallbladder on ultrasound. The low incidence rate of acute cholecystitis reported in LPAC patients is consistent with this finding and suggests that cholecystectomy may also not be needed to prevent post-sphincterotomy cholecystitis in these patients.18
The LPAC syndrome typically affects young women with normal BMI and no metabolic syndrome.4 The present study confirms these characteristic features of the disease. It should be noted, however, that a significant proportion of LPAC patients (approximately 15%) was diagnosed after the age of 40 years, and that a third of controls underwent cholecystectomy before this age. Additionally, 30% of cases were overweight at diagnosis and 13% were obese. Therefore, an age above 40 years or the presence of overweight should not preclude a diagnosis of LPAC syndrome. The adult onset of the disease (median age 27 years) may explain that common acquired risk factors for gallstones, including overweight, diabetes, or dyslipidaemia, could be present at diagnosis and might even worsen cholelithiasis in these patients. Interestingly, a first-degree relative history of symptomatic cholelithiasis was not found as an independent diagnostic feature of LPAC syndrome. Almost half of the cases did not report a family history of cholelithiasis, whereas a third of controls with common gallstone disease did. An incomplete penetrance of gene defects and contribution of modifier genes may explain this result in LPAC cases, while both acquired and low-impact genetic factors may account for cholelithiasis family history in controls. Finally, in the female population, ICP was confirmed to be associated with LPAC syndrome, although statistical significance in multivariate analysis was not achieved, likely because of a lack of power. This highlights the need for considering a diagnosis of LPAC syndrome specifically in women with cholelithiasis and a history of ICP.
In accordance with previous reports,3,5 variations in ABCB4 gene were found in approximately half of patients with LPAC syndrome. Some disease features were found to be ABCB4 related, including a history of CBD lithiasis, chronic elevation of GGT, and personal or family history of hepato-biliary cancer. The latter 2 findings are consistent with the results of genome-wide association studies showing close associations between ABCB4 variants and the risk of developing cirrhosis and/or hepato-biliary malignancies.19,20 They are also in line with the long-term risk of cirrhosis or cholangitis reported in women with ICP.7,21 In the present study, most of the cancers diagnosed in index cases or their relatives were cholangiocarcinomas, but a few cases of hepatocellular carcinoma developed on cholestatic or idiopathic cirrhosis were reported in relatives. It remains unclear whether these ABCB4-associated cancers necessarily result from underlying gallstones and/or cholestatic liver disease, or can occur in the absence of any prior liver condition. In Saint-Antoine Hospital, the few cholangiocarcinomas observed in LPAC patients were constantly developed on symptomatic intrahepatic macrolithiasis cholangiopathy,22 supporting the role of secondary sclerosing cholangitis in the pathogenesis of these cancers, while progression from micro- to severe macrolithiasis cholangiopathy has virtually never been observed after UDCA treatment had been initiated.23 Based on these observations, an imaging surveillance programme may be considered in LPAC patients with macrolithiasis disease, most specifically in those with ABCB4 gene variation. Finally, variants in ABCB4 gene were not found to be more frequent in LPAC women with a history of ICP than in those who have been pregnant without ICP. The significance of this result, which contrasts with previous reports in ICP, remains unclear.24
Our study has some limitations mainly related to its retrospective design and the use of pre-established criteria for diagnosis. As no gold standard for LPAC phenotype exists, we necessarily had to select patients based on historical diagnostic criteria, a method that was intrinsically associated with a selection bias.2 To overcome this issue and test the robustness of our results, we explored case populations with different levels of diagnostic confidence based on imaging and/or genetic reports. Some data were unavailable, especially when cholecystectomy was performed long before LPAC syndrome was diagnosed. ABCB4 genotype was not available in controls; thus, we could not exclude the presence of low-pathogenic variants of this gene in control patients. Finally, we limited our genetic exploration to ABCB4, which currently is the only established predisposition gene for LPAC syndrome, and did not investigate other potential candidate genes, such as ABCB11, ATP8B1, or ABCG5/G8.25
Our study has several important strengths. First, the large number of patients and controls allowed us to get robust results and to identify additional clinical features associated with this syndrome. Second, our control group was exhaustive and representative of non-academic hospital real-world practice. All controls were re-evaluated for supplementary data. A third of them were specifically examined for ultrasound signs of LPAC syndrome. One of them had clear evidence of intrahepatic microlithiasis and was retrospectively diagnosed with LPAC syndrome, a result that was consistent with our estimation of the relative prevalence of the disease among patients with symptomatic gallstone disease. Third, the large number of patients with ABCB4 genotype testing enabled us to identify ABCB4-associated features, including chronic elevation of GGT and personal or family increased risk of hepato-biliary cancer. Importantly also, the study provides the first estimation of the prevalence of the disease within the whole symptomatic gallstone disease.
In conclusion, LPAC syndrome accounts for approximately 1% of adult patients presenting with symptomatic gallstone disease. In addition to pre-established diagnostic criteria, normal weight, CBD stones, and no cholecystitis history are clinical features significantly associated with this syndrome. LPAC patients with ABCB4 gene variation may be at increased risk of CBD stones, persistent abnormal liver tests, and personal or family hepato-biliary cancer.
Financial support
This study was supported by a grant (COMAD) from the French National Society of Gastroenterology (SNFGE).
Authors’ contributions
Study concept and design: B.C., C.C., C.D., M.P.-C. Data acquisition: V.B., O.C., B.C., C.C., C.D., F.G., M.-P.H., C.H., A.M., B.N., L.A., M.P.-C., R.P., P.P., D.Z. Data analysis: C.D, C.C. Statistical analysis: Y.C., C.C.Drafting of paper: C.D., C.C. All the authors had access to the study data and approved the final paper.
Data availability
The data that support the findings of this study are available upon request from the authors.
Conflict of interest
The authors declare no conflicts of interest that pertain to this study.
Please refer to the accompanying ICMJE disclosure forms for further details.
Footnotes
Supplementary data to this article can be found at https://doi.org/10.1016/j.jhepr.2020.100201.
Supplementary data
References
- 1.Rosmorduc O., Hermelin B., Poupon R. MDR3 gene defect in adults with symptomatic intrahepatic and gallbladder cholesterol cholelithiasis. Gastroenterology. 2001;120:1459–1467. doi: 10.1053/gast.2001.23947. [DOI] [PubMed] [Google Scholar]
- 2.Rosmorduc O., Hermelin B., Boelle P.Y., Parc R., Taboury J., Poupon R. ABCB4 gene mutation-associated cholelithiasis in adults. Gastroenterology. 2003;125:452–459. doi: 10.1016/s0016-5085(03)00898-9. [DOI] [PubMed] [Google Scholar]
- 3.Poupon R., Rosmorduc O., Boelle P.Y., Chretien Y., Corpechot C., Chazouilleres O. Genotype-phenotype relationships in the low-phospholipid-associated cholelithiasis syndrome: a study of 156 consecutive patients. Hepatology. 2013;58:1105–1110. doi: 10.1002/hep.26424. [DOI] [PubMed] [Google Scholar]
- 4.Condat B., Zanditenas D., Barbu V., Hauuy M.P., Parfait B., El Naggar A. Prevalence of low phospholipid-associated cholelithiasis in young female patients. Dig Liver Dis. 2013;45:915–919. doi: 10.1016/j.dld.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 5.Pasmant E., Goussard P., Baranes L., Laurendeau I., Quentin S., Ponsot P. First description of ABCB4 gene deletions in familial low phospholipid-associated cholelithiasis and oral contraceptives-induced cholestasis. Eur J Hum Genet. 2012;20:277–282. doi: 10.1038/ejhg.2011.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huynh M.T., Nguyen T.T., Grison S., Lascols O., Fernandez E., Barbu V. Clinical characteristics and genetic profiles of young and adult patients with cholestatic liver disease. Rev Esp Enferm Dig. 2019;111:775–788. doi: 10.17235/reed.2019.6168/2019. [DOI] [PubMed] [Google Scholar]
- 7.Stattermayer A.F., Halilbasic E., Wrba F., Ferenci P., Trauner M. Variants in ABCB4 (MDR3) across the spectrum of cholestatic liver diseases in adults. J Hepatol. 2020;73:651–663. doi: 10.1016/j.jhep.2020.04.036. [DOI] [PubMed] [Google Scholar]
- 8.Rosmorduc O., Poupon R. Low phospholipid associated cholelithiasis: association with mutation in the MDR3/ABCB4 gene. Orphanet J Rare Dis. 2007;2:29. doi: 10.1186/1750-1172-2-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goubault P., Brunel T., Rode A., Bancel B., Mohkam K., Mabrut J.Y. Low-phospholipid associated cholelithiasis (LPAC) syndrome: a synthetic review. J Visc Surg. 2019;156:319–328. doi: 10.1016/j.jviscsurg.2019.02.006. [DOI] [PubMed] [Google Scholar]
- 10.Sim N.L., Kumar P., Hu J., Henikoff S., Schneider G., Ng P.C. SIFT web server: predicting effects of amino acid substitutions on proteins. Nucleic Acids Res. 2012;40:W452–W457. doi: 10.1093/nar/gks539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adzhubei I.A., Schmidt S., Peshkin L., Ramensky V.E., Gerasimova A., Bork P. A method and server for predicting damaging missense mutations. Nat Methods. 2010;7:248–249. doi: 10.1038/nmeth0410-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schwarz J.M., Cooper D.N., Schuelke M., Seelow D. MutationTaster2: mutation prediction for the deep-sequencing age. Nat Methods. 2014;11:361–362. doi: 10.1038/nmeth.2890. [DOI] [PubMed] [Google Scholar]
- 13.Li Q., Wang K. InterVar: clinical interpretation of genetic variants by the 2015 ACMG-AMP guidelines. Am J Hum Genet. 2017;100:267–280. doi: 10.1016/j.ajhg.2017.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li B., Krishnan V.G., Mort M.E., Xin F., Kamati K.K., Cooper D.N. Automated inference of molecular mechanisms of disease from amino acid substitutions. Bioinformatics. 2009;25:2744–2750. doi: 10.1093/bioinformatics/btp528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Portincasa P., Moschetta A., Palasciano G. Cholesterol gallstone disease. Lancet. 2006;368:230–239. doi: 10.1016/S0140-6736(06)69044-2. [DOI] [PubMed] [Google Scholar]
- 16.Shabanzadeh D.M., Sorensen L.T., Jorgensen T. A prediction rule for risk stratification of incidentally discovered gallstones: results from a large cohort study. Gastroenterology. 2016;150:156–167. doi: 10.1053/j.gastro.2015.09.002. e1. [DOI] [PubMed] [Google Scholar]
- 17.Bray F., Balcaen T., Baro E., Gandon A., Ficheur G., Chazard E. Increased incidence of cholecystectomy related to gallbladder disease in France: analysis of 807,307 cholecystectomy procedures over a period of seven years. J Visc Surg. 2019;156:209–215. doi: 10.1016/j.jviscsurg.2018.12.003. [DOI] [PubMed] [Google Scholar]
- 18.Boerma D., Rauws E.A., Keulemans Y.C., Janssen I.M., Bolwerk C.J., Timmer R. Wait-and-see policy or laparoscopic cholecystectomy after endoscopic sphincterotomy for bile-duct stones: a randomised trial. Lancet. 2002;360:761–765. doi: 10.1016/S0140-6736(02)09896-3. [DOI] [PubMed] [Google Scholar]
- 19.Gudbjartsson D.F., Helgason H., Gudjonsson S.A., Zink F., Oddson A., Gylfason A. Large-scale whole-genome sequencing of the Icelandic population. Nat Genet. 2015;47:435–444. doi: 10.1038/ng.3247. [DOI] [PubMed] [Google Scholar]
- 20.Reichert M.C., Lammert F. ABCB4 gene aberrations in human liver disease: an evolving spectrum. Semin Liver Dis. 2018;38:299–307. doi: 10.1055/s-0038-1667299. [DOI] [PubMed] [Google Scholar]
- 21.Marschall H.U., Wikstrom Shemer E., Ludvigsson J.F., Stephansson O. Intrahepatic cholestasis of pregnancy and associated hepatobiliary disease: a population-based cohort study. Hepatology. 2013;58:1385–1391. doi: 10.1002/hep.26444. [DOI] [PubMed] [Google Scholar]
- 22.Benzimra J., Derhy S., Rosmorduc O., Menu Y., Poupon R., Arrive L. Hepatobiliary anomalies associated with ABCB4/MDR3 deficiency in adults: a pictorial essay. Insights Imaging. 2013;4:331–338. doi: 10.1007/s13244-013-0243-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Poupon R., Barbu V., Chamouard P., Wendum D., Rosmorduc O., Housset C. Combined features of low phospholipid-associated cholelithiasis and progressive familial intrahepatic cholestasis 3. Liver Int. 2010;30:327–331. doi: 10.1111/j.1478-3231.2009.02148.x. [DOI] [PubMed] [Google Scholar]
- 24.Dixon P.H., Weerasekera N., Linton K.J., Donaldson O., Chambers J., Egginton E. Heterozygous MDR3 missense mutation associated with intrahepatic cholestasis of pregnancy: evidence for a defect in protein trafficking. Hum Mol Genet. 2000;9:1209–1217. doi: 10.1093/hmg/9.8.1209. [DOI] [PubMed] [Google Scholar]
- 25.Droge C., Bonus M., Baumann U., Klindt C., Lainka E., Kathemann S. Sequencing of FIC1, BSEP and MDR3 in a large cohort of patients with cholestasis revealed a high number of different genetic variants. J Hepatol. 2017;67:1253–1264. doi: 10.1016/j.jhep.2017.07.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available upon request from the authors.