Abstract
Background
Despite the general guidelines for retreatment, differences in decision making exist for secondary endodontic treatment and may be related to many factors including education, clinical experience, dentist specialty, patient preferences and economic resources. Aim of the study was to evaluate the decision making of the Saudi Board in Restorative Dentistry (SBRD) senior residents in the endodontic retreatment of molar teeth as per the scientific guidelines of the American Association of Endodontists (AAE) and also to identify the causes of retreatment and measure how far they become deviated from their taught retreatment principles and inter-individual variability.
Materials and methods
Case histories have been obtained from the files of cases treated in the SBRD Resident Comprehensive Case Archives in the SCHS from 2003 to 2015 in Riyadh region. The cases were only confined to Complex I and Complex II cases according to RDITN (Restorative Dental Index of Treatment Need), and seen by R3 and R4 residents only. Residents’ diagnosis was recorded as well as their treatment plan and any given notes regarding their decisions to retreat. Differences between the two groups (R3 and R4) residents and within the same group, regarding endodontic retreatment decisions and reasons for their treatment options were analyzed using Chi-Square test and Fisher’s Exact test.
Results
The majority of residents in both R4 and R3 groups followed the recommended guidelines. R3 residents preferred to retreat all cases while R4 chose ‘no to retreat’ in few cases. Although R4 residents preferred nonsurgical retreatment more than R3 residents, the difference was insignificant. R4 residents preferred ‘no therapy’ or ‘follow up’ more frequent than R3 residents. Members of the R3 residents agreed more or less with each other as did those of the R4 residents without significant inter-individual variations within each group regarding the choice of retreatment).
Conclusions
R4 residents appeared more likely, although not significant, to choose no retreatment or follow up than R3 residents. Conventional nonsurgical retreatment had the highest selection by both R3 and R4 residents. No significant inter-individual variations within each group regarding the choice of retreatment. There is a need to establish evidence based guidelines for more uniform management of failed root treated teeth.
Keywords: Endodontic retreatment, Non-surgical endodontic retreatment, SBRD, Decision making for retreatment
1. Introduction
The term endodontic retreatment refers to a procedure performed on a tooth that has undergone prior definitive endodontic treatment, resulting in a condition requiring further intervention to achieve a successful outcome (Hargreaves and Berman, 2016, Cohen et al., 1998). Although well-controlled studies have reported success rates of approximately 90%, population surveys have revealed that 20%–60% of endodontically treated teeth are associated with apical periodontitis, indicating the need for retreatment in several cases (Eriksen et al., 2002, Georgopoulou et al., 2005). It was recently reported that although the incidence of post-treatment disease was very small, it translated into a considerably large number of cases that required further treatment (Hargreaves and Berman, 2016).
There is a consensus that retreatment procedures should be performed in all teeth with persistent pain, swelling, or sinus tracts, and in teeth with periapical disease refractory to primary endodontic therapy (Stabholz and Friedman, 1988). Despite the existence of these general guidelines for retreatment, differences persist in the decision making process for secondary endodontic treatment, which may be related to several factors including education, clinical experience, the dentist’s specialty, the patient’s preferences, and economic resources (Pagonis et al., 2000, Doornbusch et al., 2002). Furthermore, the decision making process is based chiefly on the radiographic findings (Heinikainen et al., 2002), which is accompanied by substantial variation in the interpretation of the presence/absence of periapical disease, measurement of periapical structures, quality of the coronal restoration, and success of endodontic therapy among clinicians (Ray and Trope, 1995). These variations in radiographic interpretations may result in different treatment plans. Generally, the decision to perform retreatment is seldom made for under-filled root canals and in cases with periapical periodontal ligament (PDL) space widening. Moreover, a consensus for retreatment has been reached for symptomatic endodontically treated teeth with an unsuccessful outcome requiring further treatment (Stabholz and Friedman, 1988), but not for asymptomatic treated teeth with associated periapical lesions, a condition which remains controversial (Reit, 2010).
The Strindberg criteria were based on the absence or presence of periapical radiolucencies on periapical radiographs, which recommended a 4-year follow-up period as the cutoff point, before categorizing a case as successful or failed (Strindberg, 1956). Dentists use these criteria, which have been challenged, and a cutoff point defined by personal opinions and factors such as treatment costs, quality of the coronal seal, and accessibility to the root canal system to make decisions regarding retreatment (Kvist et al., 2004). Another dilemma with respect to the decision to perform retreat is the advancement in retreatment techniques on one hand and the evolution of implant surgery on the other. The choice between preserving an endodontically treated tooth with associated post-treatment disease and extracting it and replacing it with an implant creates wide inter-individual treatment variability and different decisions (Dechouniotis et al., 2010). The aim of the present study was to evaluate the decision making process of the senior residents (R3 and R4) of the Saudi Board in Restorative Dentistry (SBRD) in the endodontic retreatment of molars, as per the scientific guidelines of the American Association of Endodontists (AAE). An attempt was made to identify the reasons for retreatment, evaluate the extent of deviation from the established retreatment principles, and inter-individual variability.
2. Materials and methods
2.1. Study design and characteristics
This observational retrospective study assessed the endodontic treatment decision making process of senior residents (R3 and R4) of the SBRD. Ethics approval was obtained from the Research Ethical Committee of Riyadh Colleges of Dentistry and Pharmacy. Patient records were treated in a highly confidential manner and the names of residents and patients were anonymized. Furthermore, as a routine practice, every patient treated at SBRD accredited training centers signed a consent form for the use of their records and radiographs for teaching or publication purposes.
2.2. Sample selection
Comprehensive dental records of patients who received treatment at the dental center at King Saud Medical city, Riyadh region, Kingdom of Saudi Arabia between October 2003 and October 2015 by R3 and R4 residents from the SBRD program were included in this study. Out of 476 records, only 200 records were randomly selected from the archives of comprehensive cases. Treatment planning was reviewed with a focus on endodontic decisions and choices. Only cases treated by R3 and R4 of the SBRD were selected to ensure conformity of the educational and training backgrounds and that residents had approximately similar clinical experience in managing patients with endodontic problems. Only Complex I and Complex II cases (according to the Restorative Dental Index of Treatment Need) of molar teeth indicated for non-surgical root canal retreatment without any retreatment prior to selection were included in this study. Cases that were not treated within the time period (2003–2015), those with important data files missing that might affect the understanding of the resident’s treatment choice, and cases selected for extraction or for surgical root canal treatment were excluded.
2.3. Data collection
The case histories were obtained from these patient records. A wide variety of clinical conditions including clinical symptoms (pain, swelling, or sinus tract), chronic apical periodontitis, under-filled canals, over-filled canals, missed canals, inadequate compaction, silver cones, fractured instruments, inadequate flare, loss of coronal restorations, and perforations were included whenever possible.
A customized spreadsheet was prepared. The data collected included the personal history (age, sex), dental history (date when primary endodontic treatment failure was detected, duration of endodontic treatment and the patient’s complaints such as pain, swelling, fracture, or sinus formation), and relevant medical history. Special attention was paid to cases where the onset after obturation, severity, duration, initiation, and relieving factors of pain were fully described. The collected data also included the results of the clinical examination (percussion, mobility, and furcation involvement). Pre and post treatment periapical radiographs of the primary endodontic treatment were examined by the researcher. The pulp status, peri-radicular status with the resident’s diagnosis and treatment plan were recorded to evaluate their decisions on retreatment. The present and planned restorations were also mentioned in addition to the number of teeth that needed retreatment. We analyzed the residents’ consultations with their supervisors and whether retreatment was performed (yes or no) in comparison with the AAE guidelines.
2.4. Statistical analysis
Data were presented as the mean and standard deviation. Differences regarding the decision to perform endodontic retreatment and reasons for the treatment option chosen between the two groups and within each group were analyzed using the Chi-squared and Fisher’s exact tests, respectively. The results were considered statistically significant if p < 0.05.
3. Results
The analysis of patients’ files revealed that non-surgical retreatment was used in a majority (95%) of cases and no treatment or follow-up was selected for the remaining (5%) (Fig. 1).
Fig. 1.
Decision making by all residents.
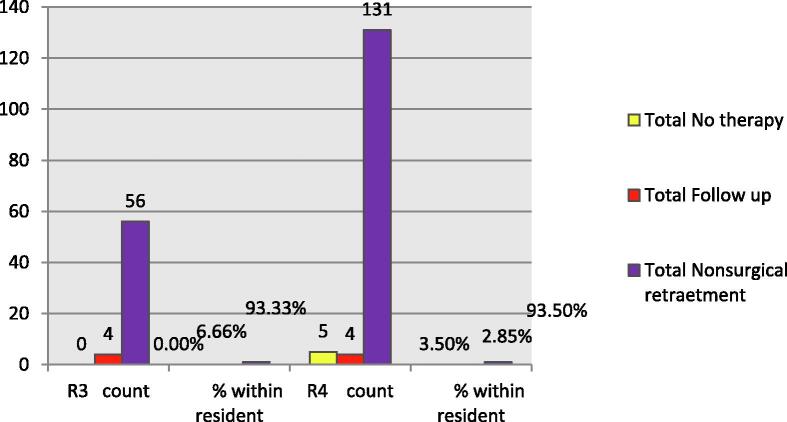
Two-way cross-tabulation showed that R3 residents were more likely to choose non-surgical retreatment than were R4 residents. R3 residents chose to “retreat” all cases. R4 residents were more likely to choose “no therapy” than were R3 residents. However, Fisher’s exact test showed that this association was statistically insignificant (Fig. 2).
Fig. 2.
Comparison of decision making choices between R3 and R4 residents.
There was no statistically significant association between treatments chosen by residents and the patient’s complaint (p > 0.05) (Fig. 3).
Fig. 3.
Association between treatment choice and patient complaints.
The analysis of the patients’ records revealed that consultation was performed in all cases except one in the R4-resident group (Table 1). Furthermore, a majority of residents in the R4 and R3 groups followed the recommended guidelines (Table 2). Fisher’s exact test showed no statistically significant association between the level of residency, consultation, and adherence to the recommended guidelines.
Table 1.
Number and frequencies of consultation done by R3 and R4 residents.
| Resident | Consultation |
Total | |||
|---|---|---|---|---|---|
| Yes | No | ||||
| R3 | Count | 60 | 0 | 60 | |
| % within Resident | 100.0% | 0.0% | 100.0% | ||
| R4 | Count | 139 | 1 | 140 | |
| % within Resident | 99.3% | 0.7% | 100.0% | ||
| Total | Count | 199 | 1 | 200 | |
| % within Resident | 99.5% | 0.5% | 100.0% | ||
Table 2.
Number and frequencies of residents following the recommended guidelines.
| Resident | Recommended guidelines |
Total | |||
|---|---|---|---|---|---|
| Yes | No | ||||
| R3 | Count | 59 | 1 | 60 | |
| % within Resident | 98.3% | 1.7% | 100.0% | ||
| R4 | Count | 139 | 1 | 140 | |
| % within Resident | 99.3% | 0.7% | 100.0% | ||
| Total | Count | 198 | 2 | 200 | |
| % within Resident | 99.0% | 1.0% | 100.0% | ||
Comparing R3 and R4 residents regarding periapical diagnoses, R3 residents were more likely to make a diagnosis of acute apical periodontitis while R4 residents were more likely to diagnose that absence of a lesion; however, the difference between R3 and R4 residents was not statistically significant (p > 0.05) (Table 3).
Table 3.
Comparison of R3 and R4 residents regarding the periapical diagnosis in patients.
| Periapical diagnosis |
Total | |||||||
|---|---|---|---|---|---|---|---|---|
| No lesion | Radiolucency | Acute Apical Periodontitis | Chronic Apical Periodontitis | Subacute Apical Periodontitis | ||||
| Resident | R3 | Count | 25 | 2 | 30 | 2 | 1 | 60 |
| % within Resident | 41.7% | 3.3% | 50.0% | 3.3% | 1.7% | 100.0% | ||
| R4 | Count | 77 | 2 | 49 | 3 | 9 | 140 | |
| % within Resident | 55.0% | 1.4% | 35.0% | 2.1% | 6.4% | 100.0% | ||
| Total | Count | 102 | 4 | 79 | 5 | 10 | 200 | |
| % within Resident | 51.0% | 2.0% | 39.5% | 2.5% | 5.0% | 100.0% | ||
R4 residents diagnosed poorly executed endodontic treatment more often (69.9%) than did R3 residents (30.1%). This was also true for under-filled canals, apical radiolucency, and periodontal ligament space widening (Table 4).
Table 4.
Comparison between R4 and R3 residents in diagnosis with regard to x ray findings.
| Resident |
Total | ||||
|---|---|---|---|---|---|
| R3 | R4 | ||||
| Weak RCT | 56 | 130 | 186 | ||
| 30.1% | 69.9% | ||||
| Voids | 10 | 34 | 44 | ||
| 22.7% | 77.3% | ||||
| Short | 27 | 78 | 105 | ||
| 25.7% | 74.3% | ||||
| Empty space | 4 | 8 | 12 | ||
| 33.3% | 66.7% | ||||
| Apical radiolucency | 7 | 11 | 18 | ||
| 38.9% | 61.1% | ||||
| Sinus tract | 1 | 1 | 2 | ||
| 50.0% | 50.0% | ||||
| Bone loss | 1 | 0 | 1 | ||
| 100.0% | 0.0% | ||||
| Extended GP | 0 | 1 | 1 | ||
| 0.0% | 100.0% | ||||
| PDL widening | 0 | 3 | 3 | ||
| 0.0% | 100.0% | ||||
| Missing canal | 0 | 1 | 1 | ||
| 0.0% | 100.0% | ||||
| Total | Count | 60 | 140 | 200 | |
4. Discussion
We utilized a retrospective approach to test the actual clinical retreatment choices made by the R3 and R4 residents in the SBRD program in an actual hospital setting in the present study. This approach differs from the approach widely used previously, in which investigators used questionnaires and radiograph-based clinical cases to evaluate practitioners’ retreatment decisions and the various factors influencing them. In such studies, questionnaires were distributed to participants (clinicians or students) including clinical information and radiographs (Balto and Al-Madi, 2004, Dechouniotis et al., 2010). Testing the decision-making process in an actual hospital setting is important and realistic compared with an approach where case scenarios are presented to the clinicians in an examination-like manner. The actual hospital setting reflects the complexity of clinical situation and the interaction between the different variables in the decision-making process including those related to patients and clinicians. However, for example, interactions between various factors such as patient preferences cannot be estimated with the questionnaire-based approach and the chosen treatment option may not be one preferred by the patient. Only molar teeth were included in the present study, since it is not an uncommon to miss a canal while performing endodontic treatment, especially in molars where the “one root, one canal” formula is frequently over ruled by the fact that the number of canals may exceed the number of roots (Hoen and Pink, 2002, Wolcott et al., 2002).
In the present study, R4 residents were more likely to diagnose the causes for retreatment especially substandard endodontic treatment, recurrent caries, defective restorations, and broken instruments than were R3 residents. This is an assumption and not a true observation because the R4 and R3 residents studied did not evaluate the same patients. R4 residents were more likely to diagnose poor performed endodontic treatment (69.9%) than were R3 residents (30.1%). This is also true for under-filled canals, apical radiolucencies and PDL space widening. These findings may signify that R4 residents exhibited a greater ability to interpret and diagnose the radiographic findings than did R3 residents. However, this conclusion is purely an assumption and not a definitive finding, because R4 and R3 residents did not evaluate the same radiographs. The design of the present study did not allow the evaluation of this aspect. The decision-making process in endodontic retreatment and the selection of the appropriate therapeutic option require excellent evidence-based knowledge, which may not be available for every clinical case. Moreover, this process may be influenced by subjective factors related to the clinician or the patient (Kvist et al., 2004), or sometimes both. Education and clinical experience are significant factors that have been demonstrated to direct the treatment plans in cases needing endodontic retreatment (Doornbusch et al., 2002, Pagonis et al., 2000). However, the participants in the present study had almost the same clinical experience and educational background, as they belonged to the same educational program. Therefore, this study could not test the influence of these factors on the decision-making process. Despite this fact, the absence of significant differences between residents from both groups supports previous studies that have emphasized the importance of the level of experience and its significant role in the decision-making process (Dechouniotis et al., 2010).
Balto et al. reported that there were no significant differences in the educational background, clinical experience, or place of work (Balto and Al-Madi, 2004) among the participating endodontists. Similar results were obtained by a previous study, which reported that the treatment decisions made by general practitioners (GDP) were independent of the place of work or other practice-related characteristics (Heinikainen et al., 2002). In agreement with these results, Pagnosis et al. reported that there was no significant differences between the retreatment options chosen by GDP and post-graduate students. However, Balto et al. found that GDP underestimated the option of conventional retreatment (Balto and Al-Madi, 2004). As a matter of fact, in the present study, it was not possible for R4 or R3 to perform “better” than the others, because there is usually no cutoff “treatment of choice” in endodontic retreatment. Therefore, the current literature is the gold standard guide to treatment options in each particular case, which is influenced by the patient’s history, clinical data, and radiographic findings. This reflects the complexity of the decision-making process in endodontic retreatment, which can be tackled at least partially by robust and thorough clinical training, along with acquiring sound and whenever possible, evidence-based clinical knowledge.
Recent reports suggest that GDPs were more hesitant to choose retreatment compared to endodontists, who chose retreatment to a greater extent (Balto and Al-Madi, 2004). This difference can be attributed to the access to better equipment to perform difficult endodontic retreatment procedures and specialty training. However, the authors attributed this difference to the underestimation of retreatment options by GDPs. This finding was not demonstrated in the present study, where differences between the R3 and R4 groups for the decision to retreat were statistically insignificant. R3 residents preferred to retreat all cases while R4 chose “not to retreat” in a few cases. There was no such hesitancy to “retreat” in R3 residents. Both R3 and R4 residents had the same access to the requisite equipment when needed. However, one should consider the fact that because of the design of the present study, R3 and R4 residents did not evaluate the same clinical cases.
Little can be said about the level of knowledge in endodontic decision-making process of R3 and R4 residents involved in the present study, as both belonged to the same teaching school and had access to the same consultation, which was provided from the same teaching pool. Any differences among them should then be attributed to the level of difficulties of the clinical cases. In fact, retreatment is an option that can be confronted in the daily clinical setting, not because of the high failure rate of the primary endodontic treatment, but because of the high percentage of endodontically treated teeth, among which a minority will suffer from failed treatment. However, this minor percentage of endodontic failures actually constitutes a large number of patients (Eriksen et al., 2002).
Farzaneh et al. and de Chevigny et al. indicated that the quality of the previous root-canal filling (length and density) was the most important outcome predictor and when the previous root filling was inadequate, 86% of cases healed compared with only 50% when the previous root filling was adequate (Farzaneh et al., 2004, De Chevigny et al., 2008). The present study recorded that 83% of endodontically treated cases were inadequate. In endodontics, clinical outcomes and treatment prognosis are among the factors affecting the decision to perform retreatment. A comparison of the clinical outcomes of different treatment modalities including non-surgical retreatment, periapical surgery, and implants may not be sound because each treatment modality addresses different clinical scenarios. This has been stated by Iqbal and Kim, who emphasized that implant placement requires the absence of periapical disease, while root canal treatment, whether surgical or non-surgical, addresses the presence of disease (Iqbal and Kim, 2007).
This study showed that non-surgical retreatment was the preferred treatment modality for both R3 and R4 residents; it was the highest percentage (100% and 96.4% respectively) of treatment chosen by the residents. This is in agreement with recent studies, which found that endodontists preferred nonsurgical retreatment above other treatment options (Dechouniotis et al., 2010). Non-surgical orthograde retreatment is the first therapeutic option for a majority of failed previously treated teeth and surgery should be performed only in strictly selected cases, as stated by Carrotte et al (Carrotte, 2000). Although R3 residents preferred non-surgical retreatment more than R4 residents did, the difference was statistically insignificant. A one-year difference in training (experience) between R4 and R3 residents is insufficient to be reflected as a difference in their clinical decision-making process, especially when they were still under training. Future studies should evaluate whether this difference is augmented and becomes more apparent with an increase in experience in the absence of clinical supervision.
In the present study, both R3 and R4 residents agreed on the need for retreating teeth with clinical signs and symptoms, and also canals that appeared under-filled on radiographs. This was in agreement with the findings of Balto et al. and Van Nieuwenhuysen et al., who considered clinical signs and symptoms as important factors that determined the need for retreatment; no retreatment or observation was chosen in the absence of clinical findings, (Balto and Al-Madi, 2004, Van Nieuwenhuysen et al., 1994). There is obviously a consensus in the field of endodontics that retreatment should be performed at least in all cases with persistent pain, clinical signs such as swelling or sinus tract, and in teeth with periapical pathosis refractory to endodontic therapy (Stabholz and Friedman, 1988, Padmaja et al., 2015).
Kvist et al. suggested a concept different from that of Strindberg and the Praxis Concept in an attempt to explain the high inter-individual variation in clinical retreatment strategies (Kvist et al., 2004). This concept considers periapical disease as a continuum, which is perceived at different stages on a continuous health scale, based on radiographic appearances. Therefore, a larger radiolucency is thought to represent a more serious condition than a smaller one, based on this concept. Kvist et al. stated that according to the Praxis Concept, the placement of the cut-off point on the periapical health continuum depends on the practitioner’s personal opinions (Kvist et al., 2004). Moreover, Reit and Kvist found that although practitioners agree on several factors such as the healing potential of the lesion and risks, they still make different treatment choices (Kvist et al., 2004).
5. Conclusion
R4 residents appeared more likely, although not significantly, to choose no retreatment or follow-up than did R3 residents. Conventional nonsurgical retreatment had the highest frequency of selection by both R3 and R4 residents. There was no significant difference between R3 and R4 residents with respect to the factors guiding their retreatment decisions. There were no significant inter-individual variations within each group with respect to the choice of retreatment. Evidence-based guidelines need to be established to ensure greater uniformity in the management of failed endodontically treated teeth. Recommendations including the establishment of continuous intensive development in the SBRD programs, implementation of quality clinical training to provide facilities for the acquisition of sound clinical knowledge, and establishment of evidence-based guidelines for the management of endodontic failures should be considered. Further research is needed to clarify the relationship between the residents’ opinions and their decision-making abilities for retreatment.
Ethical statement
The study was conducted upon ethical approval from LCBE under the guidelines of Helsinki practices.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Peer review under responsibility of King Saud University.
References
- Balto H.A.G., Al-Madi E.M. A comparison of retreatment decisions among general dental practitioners and endodontists. J. Dent. Educ. 2004;68:872–879. [PubMed] [Google Scholar]
- Carrotte P.V. Current practice in endodontics: 4. A review of techniques for canal preparation. Dental Update. 2000;27:488–493. doi: 10.12968/denu.2000.27.10.488. [DOI] [PubMed] [Google Scholar]
- Cohen S., Burns R.C., Walton R., Torabenijad M. Pathways of the Pulp (1) Learning. 1998;30:10. [Google Scholar]
- De Chevigny C., Dao T.T., Basrani B.R., Marquis V., Farzaneh M., Abitbol S., Friedman S. Treatment outcome in endodontics: the Toronto study—phases 3 and 4: orthograde retreatment. J. Endod. 2008;34:131–137. doi: 10.1016/j.joen.2007.11.003. [DOI] [PubMed] [Google Scholar]
- Dechouniotis G., Petridis X.M., Georgopoulou M.K. Influence of specialty training and experience on endodontic decision making. J. Endod. 2010;36:1130–1134. doi: 10.1016/j.joen.2010.03.023. [DOI] [PubMed] [Google Scholar]
- Doornbusch H., Broersma L., Boering G., Wesselink P. Radiographic evaluation of cases referred for surgical endodontics. Int. Endod. J. 2002;35:472–477. doi: 10.1046/j.1365-2591.2002.00510.x. [DOI] [PubMed] [Google Scholar]
- Eriksen H.M., Kirkevang L.L., Petersson K. Endodontic epidemiology and treatment outcome: general considerations. Endod. Top. 2002;2:1–9. [Google Scholar]
- Farzaneh M., Abitbol S., Friedman S. Treatment outcome in endodontics: the Toronto study. Phases I and II: Orthograde retreatment. J. Endod. 2004;30:627–633. doi: 10.1097/01.don.0000129958.12388.82. [DOI] [PubMed] [Google Scholar]
- Georgopoulou M., Spanaki-Voreadi A., Pantazis N., Kontakiotis E. Frequency and distribution of root filled teeth and apical periodontitis in a Greek population. Int. Endod. J. 2005;38:105–111. doi: 10.1111/j.1365-2591.2004.00907.x. [DOI] [PubMed] [Google Scholar]
- Hargreaves K.M., Berman L. 11th ed. Elsevier; St. Louis: 2016. Cohens Pathways of the Pulp. [Google Scholar]
- Heinikainen M., Vehkalahti M., Murtomaa H. Retreatment in endodontics: treatment decisions by general practitioners and dental teachers in Finland. Int. Dent. J. 2002;52:119–124. doi: 10.1111/j.1875-595x.2002.tb00615.x. [DOI] [PubMed] [Google Scholar]
- Hoen M.M., Pink F.E. Contemporary endodontic retreatments: an analysis based on clinical treatment findings. J. Endod. 2002;28:834–836. doi: 10.1097/00004770-200212000-00010. [DOI] [PubMed] [Google Scholar]
- Iqbal M.K., Kim S. For teeth requiring endodontic treatment, what are the differences in outcomes of restored endodontically treated teeth compared to implant-supported restorations? Int. J. Oral Maxillofac. Implants. 2007:22. [PubMed] [Google Scholar]
- Kvist T., Heden G., Reit C. Endodontic retreatment strategies used by general dental practitioners. Oral Surgery, Oral Med., Oral Pathol., Oral Radiol., Endodontol. 2004;97:502–507. doi: 10.1016/j.tripleo.2003.09.006. [DOI] [PubMed] [Google Scholar]
- Padmaja K., Shah A., Malpani S., Kakkar M., Thakkar R. Retreatment in endodontics: a review. J. Adv. Med. Dental Sci. Res. 2015;3:205. [Google Scholar]
- Pagonis T.C., Fong C.D., Hasselgren G. Retreatment decisions—a comparison between general practitioners and endodontic postgraduates. J. Endod. 2000;26:240–241. doi: 10.1097/00004770-200004000-00012. [DOI] [PubMed] [Google Scholar]
- Ray H., Trope M. Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. Int. Endod. J. 1995;28:12–18. doi: 10.1111/j.1365-2591.1995.tb00150.x. [DOI] [PubMed] [Google Scholar]
- Reit C. Textbook of Endodontology. 2nd ed. Blackwell Publishing; Oxford: 2010. Endodontic decision making; pp. 301–313. [Google Scholar]
- Stabholz A., Friedman S. Endodontic retreatment—case selection and technique. Part 2: treatment planning for retreatment. J. Endod. 1988;14:607–614. doi: 10.1016/S0099-2399(88)80058-X. [DOI] [PubMed] [Google Scholar]
- Strindberg L.Z. The dependence of the results of pulp therapy on certain factors-an analytical study based on radiographic and clinical follow-up examination. Acta Odontol. Scand. 1956;14:1–175. [Google Scholar]
- Van Nieuwenhuysen J.P., Aouar M., D’hoore W. Retreatment or radiographic monitoring in endodontics. Int. Endod. J. 1994;27:75–81. doi: 10.1111/j.1365-2591.1994.tb00234.x. [DOI] [PubMed] [Google Scholar]
- Wolcott J., Ishley D., Kennedy W., Johnson S., Minnich S. Clinical investigation of second mesiobuccal canals in endodontically treated and retreated maxillary molars. J. Endod. 2002;28:477–479. doi: 10.1097/00004770-200206000-00016. [DOI] [PubMed] [Google Scholar]