Abstract
Purpose:
Beckwith–Wiedemann syndrome (BWS) is a human genomic imprinting disorder characterized by lateralized overgrowth, macroglossia, abdominal wall defects, congenital hyperinsulinism, and predisposition to embryonal tumors. One of the molecular etiologies underlying BWS is paternal uniparental isodisomy of chromosome 11p15.5 (pUPD11). About 8% of pUPD11 cases are due to genome-wide paternal uniparental isodisomy (GWpUPD). About 30 cases of live-born patients with GWpUPD have been described, most of whom were mosaic and female. We present male patients with BWS due to GWpUPD, elucidate the underlying mechanism, and make recommendations for management.
Methods:
Three male patients with GWpUPD underwent clinical and molecular evaluation by single-nucleotide polymorphism (SNP) microarrays in different tissues. Previously published cases of GWpUPD were reviewed.
Results:
SNP microarray demonstrated a GWpUPD cell population with sex chromosomes XX and biparental cell population with sex chromosomes XY, consistent with dispermic androgenetic chimerism.
Conclusion:
SNP microarray is necessary to distinguish GWpUPD cases and the underlying mechanisms. The percentage of GWpUPD cell population within a specific tissue type correlated with the amount of tissue dysplasia. Males with BWS due to GWpUPD are important to distinguish from other molecular etiologies because the mechanism indicates risk for germ cell tumors and autosomal recessive diseases in addition to other BWS features.
Keywords: Beckwith–Wiedemann syndrome (BWS), chimera, genome-wide paternal uniparental isodisomy, mosaicism
INTRODUCTION
Beckwith–Wiedemann syndrome (BWS, OMIM 130650) is a human genomic imprinting disorder with a variable phenotypic spectrum including lateralized overgrowth (LO), macroglossia, abdominal wall defects, congenital hyperinsulinism (HI), and predisposition to embryonal tumors.1 One molecular etiology of BWS is paternal uniparental isodisomy of chromosome 11p15.5 (pUPD11), and 8% of these cases may be caused by genome-wide paternal uniparental isodisomy (GWpUPD) (L. Conlin, unpublished data).1 GWpUPD has been described in over 30 live-born infants and is also common in cases of placental mesenchymal dysplasia and molar pregnancies (Supplemental Table 2). In cases of GWpUPD, there may be features of any imprinting disorders caused by paternal uniparental isodisomy (pUPD), including transient neonatal diabetes and intrauterine growth restriction (IUGR) (chromosome 6), Beckwith–Wiedemann syndrome (BWS) (chromosome 11), Kagami–Ogata syndrome (chromosome 14), Angelman syndrome (chromosome 15), and PTH resistance (chromosome 20).2
Since the first human chimera was described in 1962, fewer than 50 have been reported.3 Multiple mechanisms have been proposed leading to GWpUPD. Both mosaicism or chimerism could result in two distinct cell populations (a biparental cell population, and a cell population with paternal isodisomy of every chromosome). Mosaicism suggests a genome-wide mitotic error that happens after fertilization whereas chimerism is generally an error that occurs during fertilization and could involve multiple germ cells.4 Specifically, androgenetic chimerism would involve the diploidization of the paternal genome and may involve up to four gametes including fertilization of a single egg or polar body by one or two sperm. Females with BWS due to GWpUPD were identified by genome-wide single-nucleotide polymorphism (SNP) microarray.5,6 All cases have been reported to have isodisomy in the GWpUPD cell population.1 While females with GWpUPD cell population may either originate from one or two X-bearing sperm, males with GWpUPD would have to have originated from both an X-bearing and Y-bearing sperm as the GWpUPD cell population must be XX in chromosomal sex complement.
We present two male patients with clinical features of BWS and signs of Angelman syndrome due to GWpUPD with comparison with a previously reported third patient.7 Finally, we make additional management recommendations for males with GWpUPD beyond the typical BWS recommendations.
MATERIALS AND METHODS
Three patients were enrolled into an Institutional Review Board–approved protocol with informed consent at The Children’s Hospital of Philadelphia (IRB 13–010658), including informed consent for publication of patient photographs. Evaluation included multiple specialists, laboratory and imaging studies, with clinical chromosomal microarray studies carried out using either Illumina (patient 1, 3 liver and blood) or Applied Biosystems (patient 2, patient 3 toe) SNP microarrays. The B-allele frequencies were examined to calculate the percent of cells with uniparental disomy.8 The Illumina CytoSNP850Kv1.1 BeadChip has over 840,000 SNP probes with a backbone resolution averaging one probe every 4 kb. The Applied Biosystems CytoScan HD array contains 2.6 million genetic markers (including approximately 750k SNP probes) covering the human genome at the mean spacing of one marker per kilobase.
RESULTS
Patient 1 was born at 31 weeks 5 days gestation after spontaneous vaginal delivery to a 27-year-old gravida 4 para 2 to 3 mother. The pregnancy was naturally conceived. Prenatal medications included prenatal vitamin and sertraline. Ultrasound at 20 weeks gestational age showed large cystic placenta, polyhydramnios, cystic kidneys, cardiac biventricular hypertrophy, and macrosomia. The pregnancy was complicated by gestational diabetes managed by diet (fasting plasma glucose ranged 80–120 mg/dL), polyhydramnios requiring two amnioreductions, and premature contractions. Due to the placental and fetal anomalies, amniocentesis was performed. Interphase fluorescence in situ hybridization (iFISH) for sex chromosomes X, Y, 13, 18, and 21 showed XY in 159 of 200 cells, and 41 of 200 cells showed XX. G-banded chromosome analysis showed 46,XX[6]/46,XY[9]. SNP microarray from amniocytes showed that 67% were XY while 33% were XX. Short tandem repeat (STR) analysis of chromosome 11 and chromosome 14 showed paternal UPD. Taken together, these results were consistent with GWpUPD.
At birth, patient 1 was 92nd percentile for weight. Physical exam at 4 weeks of age showed average size, open sagittal suture, dark blond hair, light blue eyes, wide-spaced nipples, palpable liver, left inguinal hernia with palpable testes, left LO, and toe abnormalities (Fig. 1a–c). His hospital course included hyperbilirubinemia treated with phototherapy, severe HI requiring a 90% pancreatectomy with persistent hypoglycemia, bilateral cardiac hypertrophy, anemia, thrombocytosis, adrenal cortical cytomegaly with histologic indication of pUPD11 by p57 staining, hepatic cysts, and inguinal hernia repair with removal of Meckel’s diverticulum. The biopsied pancreas showed increased endocrine tissue with admixed acinar and ducts with nodular architecture and fibrosis, typical for BWS. His α-fetoprotein (AFP) peaked at 503,000 ng/ml and declined. Hormonal testing at 9.5 weeks of age to screen for mixed gonadal dysgenesis included antimullerian hormone (226.800 ng/ml, no ref range for age, but 6–11 months male 56.677–495.299 ng/ml), ultrasensitive follicle-stimulating hormone (FSH) (0.118 mIU/mL, ref range male 4 weeks–11 months 0.16–4.1), ultrasensitive luteinizing hormone (LH) (0.349 mIU/mL, ref range 0.02–7.0), and total serum testosterone (103 ng/dL, ref range for 31–35 weeks gestation 37–198). He continued to have adrenal cytomegaly and lateralized overgrowth. Chest x-ray did not show bell-shaped thorax. At 14 months of age, he has developed seizures. He is crawling but not walking, does not like putting weight on his feet, and has three words and a happy disposition. He has heterochromia, esotropia, and strabismus. Postnatally, SNP microarray performed in different tissue types demonstrated GWpUPD ranging from 5% to 85% (Fig. 1h, i).
Fig. 1. Clinical and molecular features of patients.
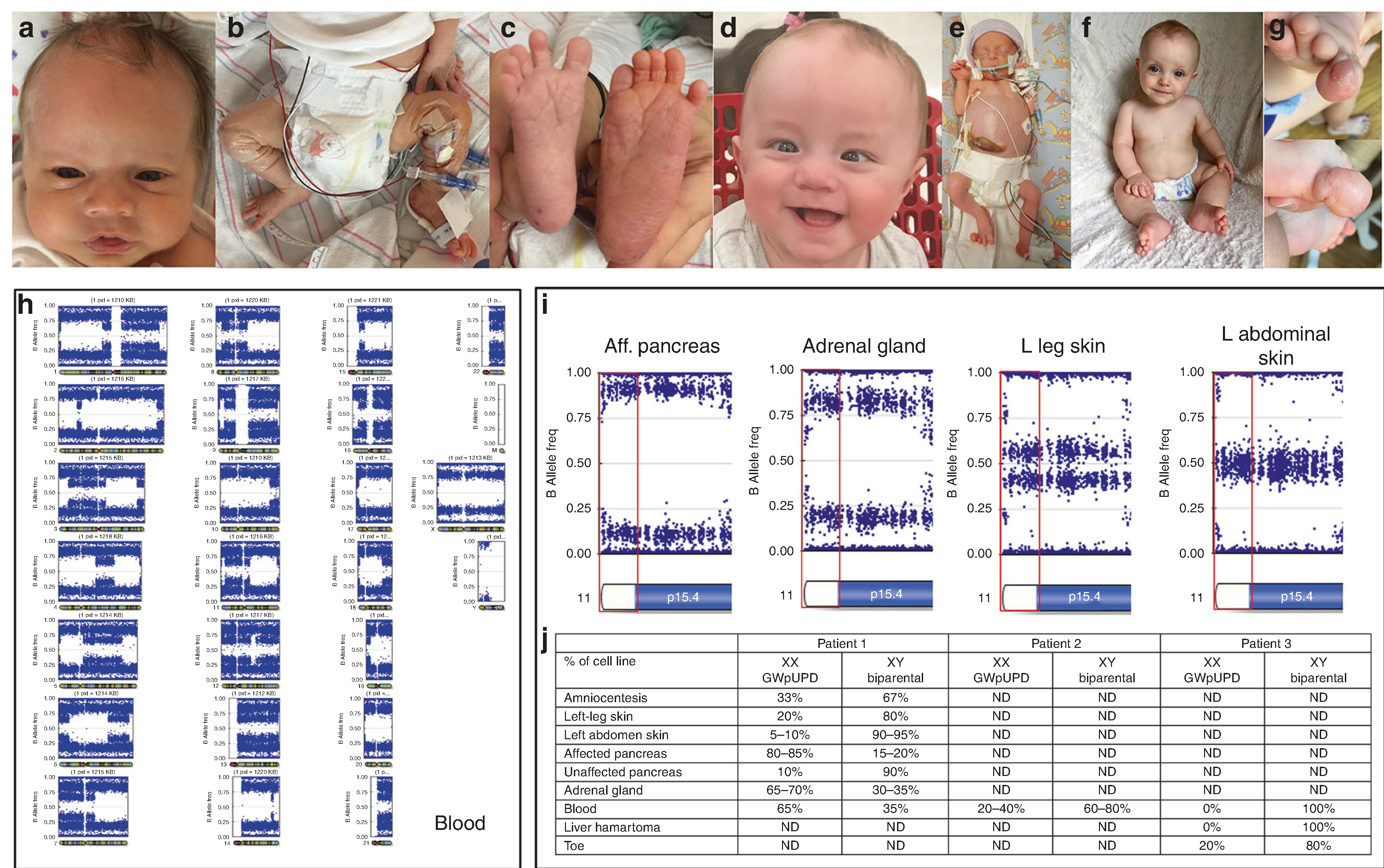
a–c. Patient 1 at 4 weeks of age. Lateralized overgrowth (LO) of the (a) left cheek, (b) leg, and (c) foot with toes lengthening from great toe to fourth toe with space between fourth and fifth toe on larger left foot with bilateral feet with deep creases on plantar surface. Right foot measured 7 cm × 2.7 cm. Left foot measured 7.2 cm × 3.1 cm. d. Patient 1 at 9 months of age with esotropia, heterochromia, and LO of the left cheek. e Patient 3, critically ill with distended abdomen, diastasis recti, and right fifth toe hamartoma. f Patient 3, alive and well. g Patient 3, toe from multiple views. h Genome-wide view of single-nucleotide polymorphism (SNP) array B-allele frequency for patient 1 from blood. Genome-wide paternal uniparental isodisomy (GWpUPD) quantified to be 65%. i SNP array data viewed for part of chromosome 11 in order of highest percentage of GWpUPD to lowest: affected pancreas (80–85% GWpUPD), adrenal gland (65–60%), left leg skin (20%), and left side abdominal skin (5–10%). 11p15 is highlighted by the red box. j Percentage of GWpUPD by cell type in patients. ND not done.
Patient 2 was from a naturally conceived pregnancy and born at 32 weeks gestation by caesarean section for nonreassuring fetal status. Pregnancy was complicated by polyhydramnios requiring amnioreduction, pregnancy induced hypertension, and placental abruption. Amniocentesis showed a normal male karyotype. At birth, he weighed 2.115 kg (83%ile). His physical exam at 3 weeks old demonstrated average size, anterior anus, hepatomegaly, umbilical hernia, and sacral dimple with hair tuft and visible base. After birth, echocardiogram showed midseptal interatrial communication, mild right atrial/right ventricle enlargement, a large patent ductus arteriosus (PDA) with bidirectional flow, and mild tricuspid regurgitation. The PDA spontaneously closed and the right heart enlargement resolved on subsequent echocardiogram. Abdominal imaging revealed an infantile hemangioendothelioma in the liver, which was treated with propranolol. Abdominal imaging showed renal asymmetry, renal malrotation renal cysts, adrenal hyperplasia, and unremarkable pancreas. He had thymic hyperplasia requiring thymectomy. His HI was initially managed with glucose infusion rate of 19 mg/kg/min, followed by continuous feeds, and finally feeds were condensed around 5 months of age. His HI resolved without need for pancreatectomy. His hospital course was complicated by intubation, grade 1 germinal matrix hemorrhage, and IV infiltrate leading to left upper extremity compartment syndrome requiring a fasciotomy. He has chronic lung disease. His AFP peaked at 159,000 ng/ml and declined. Hormonal testing was not completed. Chest x-ray did not demonstrate bell-shaped chest. Microarray from blood showed a female GWpUPD cell population (20–40%) and a normal biparental male cell population (60–80%) (Fig. 1j). At 10 months of age, he is developmentally delayed. He has hypotonia and sits with support, smiles, fixes gaze, but is not yet rolling. At 18 months of age, he has not had seizures. Patient 3 was from a naturally conceived pregnancy and born at 33 weeks gestation due to placental abruption caused by placental mesenchymal dysplasia. Clinical features included congenital hypothyroidism, thrombocytopenia, transient hypoglycemia, hepatomegaly with hepatic mesenchymal hamartoma, macrodactyly of right fifth digit on the foot with pathology showing a benign vascular lesion, multiple hemangiomas, and diastasis recti (Fig. 1e–g). Hormonal testing was not completed. Microarray detected 20% GWpUPD in the toe, and no GWpUPD in the liver hamartoma or blood (Fig. 1i), similar to previous reported findings.7 STR analysis in the placenta demonstrated 40% GWpUPD.
The genotyping pattern for all patients was consistent with the presence of two paternal haplotypes and one maternal haplotype and showed the presence of recombination between the two paternal haplotypes (patient 1 shown in Fig. 1h). The genotyping patterns demonstrate evidence of crossing over with regions with either one or two paternal haplotypes. The number of haplotypes at the centromeres showed a random pattern, consistent with the involvement of two independent sperm. Fertilization of an egg by a diploid sperm is unlikely as this would result in a consistent genotyping pattern at the centromeres, as expected with a meiosis II or meiosis I error.
Taken together, this suggests that these patients are androgenetic chimeras, with two different cells populations, likely due to fertilization occurring between an X-bearing egg and Y-bearing sperm and an anuclear polar body and an X-bearing sperm, followed by haploidy rescue of the X-bearing male pronucleus.
DISCUSSION
Initially, these three male patients primarily demonstrated the phenotype of BWS due to GWpUPD. However, due to the unknown contribution of GWpUPD in different tissues they are at risk for other imprinting disorders. They do not have features of transient neonatal diabetes and IUGR (pUPD chromosome 6), the bell-shaped chest associated with Kagami–Ogata syndrome (pUPD chromosome 14 [pUPD14]), or PTH resistance (pUPD chromosome 20).2 However patient 1 is beginning to show signs of Angelman syndrome (pUPD chromosome 15 [pUPD15]).2 Patient 2 does have developmental delay and hypotonia, which could be a manifestation of pUPD15, however this could also be due to his prolonged and complicated hospitalization after birth. In agreement with the phenotypes seen in these patients, the literature suggests the prominent phenotype in GWpUPD patients is BWS followed by pUPD14 and pUPD15 (Supplemental Table 1). Interestingly, there are other reports of patients with GWpUPD with opposite phenotypes of those expected, for example IUGR instead of macrosomia.9,10 It is likely that the phenotypes are dictated by the percentage and distribution of the GWpUPD cell population within certain tissues.4 This may be why patient 3, with GWpUPD only in the toe overgrowth, is not demonstrating clinical symptoms of Angelman syndrome. There may be a threshold above which a specific pUPD phenotype will be expressed or that GWpUPD is not compatible with life when present at high levels in certain tissues, such as the brain. Alternatively, there may be other modifying factors, such as homozygosity for pathogenic variants in the isodisomic cells, or others not yet discovered that affect these phenotypes. Thus, further research is needed to study what epigenetic/genetic factors modify the phenotype.
Several considerations must be taken for management of GWpUPD patients. If GWpUPD is suspected in a fetus, mothers should be cautioned about premature labor due to the median gestation at delivery of 33 weeks (Supplemental Table 1). Recent guidelines estimate about 8% of all BWS patients will have an embryonal tumor.1 However, 50% of the patients in the literature with BWS due to GWpUPD have experienced a typical BWS tumor, and 69% have some sort of tumor or mass (Supplemental Table 1). Moreover, six of the seven patients reported at an age greater than seven years old developed tumors after this age, suggesting extension of screening beyond seven seven years old.2,5,11–14 This could be due to the level of the GWpUPD in each tissue type, supported by the fact that the tissues with dysplasia in our patients have a higher proportion of GWpUPD cells compared with the normal biparental cell population (Fig. 1j).
Due to the GWpUPD, these patients are at risk for paternally carried autosomal recessive diseases.11,15,16 Exome sequencing was performed for patient 3 due to the congenital hypothyroidism.7 This identified a paternally inherited pathogenic deletion in DUOX2, c.2895_2898delGTTC (p. Phe966Serfs*29).7 However, there was no clinical indication to obtain thyroid tissue in this patient, thus the degree of GWpUPD in the thyroid tissue is unknown. Patients 1 and 2 have had no clinical signs or symptoms to suggest other diseases at this time and thus will be monitored closely for manifestations of other disorders with additional genetic testing if indication arises.
Patients with XY/XX chimerism are at risk for germ cell tumors.17 Interestingly, hormone screening labs in patient 1 are consistent with normal male values. Interestingly, although mixed gonadal dysgenesis has been reported for 45,X/46,XY patients,18 our patients did not display signs of this based on imaging for all three patients and laboratory testing for patient 1. We hypothesize this again may be due to the degree of GWpUPD in the gonadal tissue. The Consensus Statement does not specifically include recommendations for chimeric 46,XY/46, XX patients.19 Thus management will be similar to 45,X/46,XY males with gonadal dysgenesis. If the testes are descended, screening can be performed by physical exam. However, if the testes are intra-abdominal, ultrasound may be used for surveillance prior to surgery for cryptorchidism with biopsy. After puberty, ultrasound should be performed yearly. Natural history studies of patients with GWpUPD are needed to help guide management into adulthood, but infertility and nonclassical BWS tumors need to be considered.11,13,20
SNP microarray allows for insight into the developmental mechanism and timing of chromosome aneuploidy mosaicism and uniparental disomy.8 SNP microarray demonstrates dispermic chimerism. The fertilization event occurs between an X-bearing egg, an X-bearing sperm, and a Y-bearing sperm to create an androgenetic chimera (Fig. 2). In one proposed mechanism, a Y-bearing sperm fertilizes an X-bearing egg and an X-bearing sperm fertilizes an anuclear polar body. The X-bearing male pronucleus then would undergo haploidy rescue or endoreduplication resulting in an androgenetic chimera (Fig. 2a). In another similar proposed mechanism, two sperm fertilize a single egg, but the X-bearing male pronucleus could fail to fuse, be expulsed from the fertilized egg, and undergo endoreduplication to a GWpUPD (XX) cell population with a different paternal haplotype (Fig. 2b). Another proposed mechanism is fusion of the three pronuclei, followed by diploidization of the triploid embryo (Fig. 2c). GWpUPD is highly unlikely in a triploidy rescue event given that delayed incorporation is the main mechanism for triploidy.21 The first mechanism is most likely, supported by the fact that an egg is more likely to developmentally progress with a higher amount of anuclear fragmentation in the polar body compared with an intact polar body.22 These mechanisms contrast to GWpUPD due to a single sperm (as previously described6).
Fig. 2. Hypothesized mechanisms for genome-wide paternal uniparental isodisomy (GWpUPD).
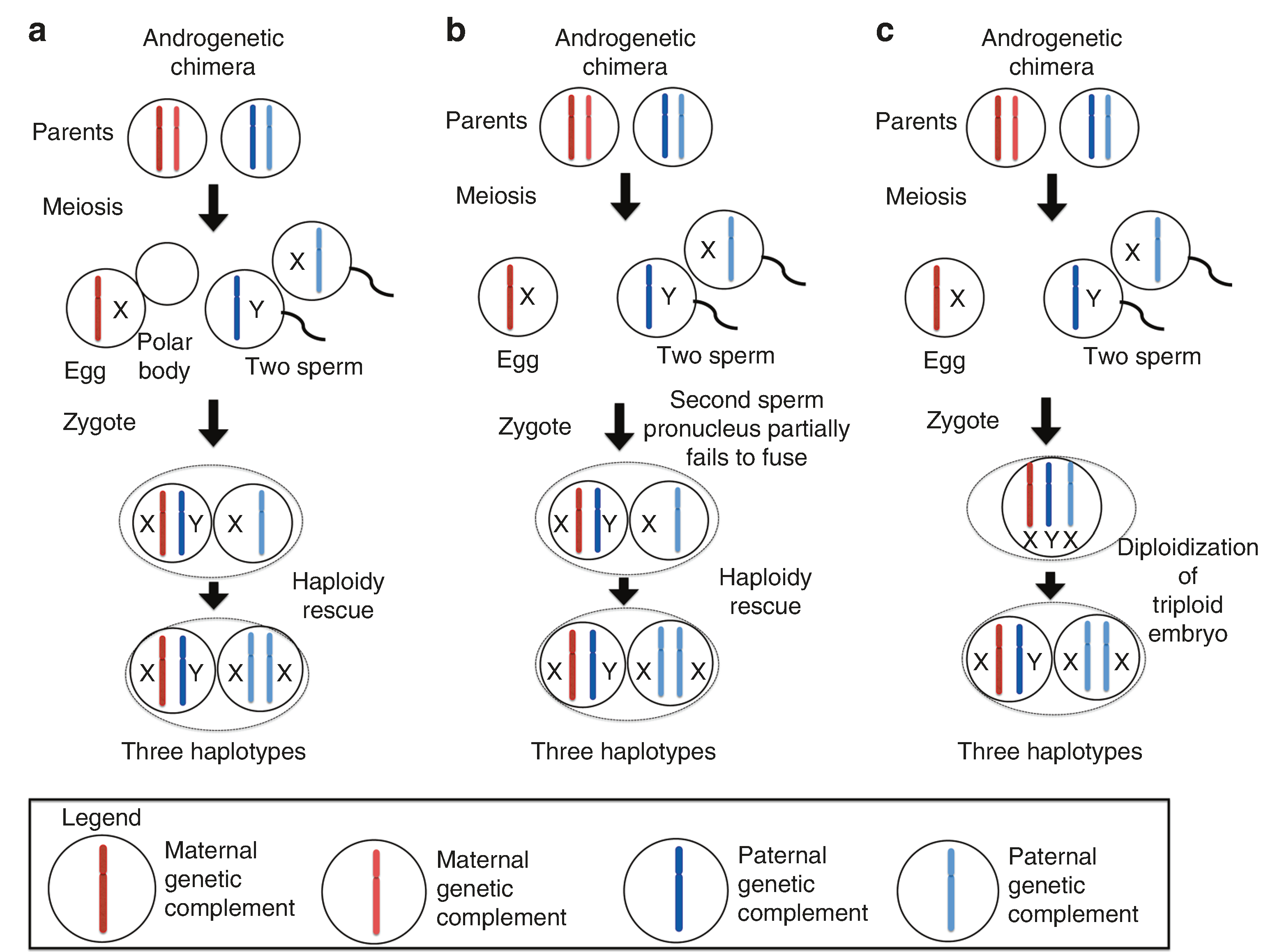
Legend: each bar represents a maternal or paternal haplotype. The X or the Y next to the bar indicates the associated sex chromosome. a Androgenetic chimera. Fertilization occurs between an egg with an anuclear polar body and two sperm. Haploidy rescue occurs leading to two cell line populations with three different haplotypes. b Androgenetic chimera. Fertilization occurs between an egg and two sperm. The second sperm pronucleus partially fails to fuse. Haploidy rescue occurs leading to two cell populations with three different haplotypes. c Androgenetic chimera. Fertilization occurs between an egg and two sperm to create a triploid embryo that undergoes diploidization. This is extremely unlikely as the main mechanism of triploidy is delayed incorporation. The zygote contains three haplotypes.
Taken together, the clinical features and SNP microarrays demonstrate GWpUPD due to dispermic chimerism with the primary clinical manifestations being consistent with BWS. If BWS is suspected, a SNP microarray will provide insights about pUPD11, GWpUPD, and the number of maternal and paternal chromosomal complements. This data is important for assessing mechanism and additional management considerations. These patients will continue standard BWS tumor screening with additional consideration of germ cell tumors and extension past seven years old, as well as clinical surveillance for other autosomal recessive or pUPD syndromes.
Supplementary Material
ACKNOWLEDGEMENTS
We thank the patients and their families for sharing their stories. J.M.K. is supported by the National Institutes of Health (K08 CA193915), Alex’s Lemonade Stand Foundation, St. Baldrick’s Foundation, and the University of Pennsylvania Orphan Disease Center.
Footnotes
SUPPLEMENTARY INFORMATION
The online version of this article (https://doi.org/10.1038/s41436-019-0551-9) contains supplementary material, which is available to authorized users.
DISCLOSURE
The authors declare no conflicts of interest.
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
REFERENCES
- 1.Brioude F, Kalish JM, Mussa A, et al. Expert consensus document: clinical and molecular diagnosis, screening and management of Beckwith–Wiedemann syndrome: an international consensus statement. Nat Rev Endocrinol. 2018;14:229–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Romanelli V, Nevado J, Fraga M, et al. Constitutional mosaic genomewide uniparental disomy due to diploidisation: an unusual cancer-predisposing mechanism. J Med Genet. 2011;48:212–216. [DOI] [PubMed] [Google Scholar]
- 3.Gartler SM, Waxman SH, Giblett E. An XX/XY human hermaphrodite resulting from double fertilization. Proc Natl Acad Sci USA 1962;48:332–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Malan V, Vekemans M, Turleau C. Chimera and other fertilization errors. Clin Genet. 2006;70:363–373. [DOI] [PubMed] [Google Scholar]
- 5.Inbar-Feigenberg M, Choufani S, Cytrynbaum C, et al. Mosaicism for genome-wide paternal uniparental disomy with features of multiple imprinting disorders: diagnostic and management issues. Am J Med Genet A. 2013;161A:13–20. [DOI] [PubMed] [Google Scholar]
- 6.Kalish JM, Conlin LK, Bhatti TR, et al. Clinical features of three girls with mosaic genome-wide paternal uniparental isodisomy. Am J Med Genet A. 2013;161A:1929–1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Repnikova E, Roberts J, Kats A, et al. Biparental/androgenetic mosaicism in a male with features of overgrowth and placental mesenchymal dysplasia. Clin Genet. 2018;94:564–568. [DOI] [PubMed] [Google Scholar]
- 8.Conlin LK, Thiel BD, Bonnemann CG, et al. Mechanisms of mosaicism, chimerism and uniparental disomy identified by single nucleotide polymorphism array analysis. Hum Mol Genet. 2010;19:1263–1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Robinson WP, Lauzon JL, Innes AM, Lim K, Arsovska S, McFadden DE. Origin and outcome of pregnancies affected by androgenetic/biparental chimerism. Hum Reprod. 2007;22:1114–1122. [DOI] [PubMed] [Google Scholar]
- 10.Kaiser-Rogers KA, McFadden DE, Livasy CA, et al. Androgenetic/ biparental mosaicism causes placental mesenchymal dysplasia. J Med Genet. 2006;43:187–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ohtsuka Y, Higashimoto K, Sasaki K, et al. Autosomal recessive cystinuria caused by genome-wide paternal uniparental isodisomy in a patient with Beckwith–Wiedemann syndrome. Clin Genet. 2015;88:261–266. [DOI] [PubMed] [Google Scholar]
- 12.Wilson M, Peters G, Bennetts B, et al. The clinical phenotype of mosaicism for genome-wide paternal uniparental disomy: two new reports. Am J Med Genet A. 2008;146A:137–148. [DOI] [PubMed] [Google Scholar]
- 13.Gogiel M, Begemann M, Spengler S, et al. Genome-wide paternal uniparental disomy mosaicism in a woman with Beckwith–Wiedemann syndrome and ovarian steroid cell tumour. Eur J Hum Genet. 2013;21:788–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bertoin F, Letouzé E, Grignani P, et al. Genome-wide paternal uniparental disomy as a cause of Beckwith–Wiedemann syndrome associated with recurrent virilizing adrenocortical tumors. Horm Metab Res. 2015;47:497–503. [DOI] [PubMed] [Google Scholar]
- 15.Borgulová I, Soldatova I, Putzová M, et al. Genome-wide uniparental diploidy of all paternal chromosomes in an 11-year-old girl with deafness and without malignancy. J Hum Genet. 2018;63:803–810. [DOI] [PubMed] [Google Scholar]
- 16.Kapur RP, Cole B, Zhang M, Lin J, Fligner CL. Placental mesenchymal dysplasia and fetal renal-hepatic-pancreatic dysplasia: androgeneticbiparental mosaicism and pathogenesis of an autosomal recessive disorder. Pediatr Dev Pathol. 2013;16:191–200. [DOI] [PubMed] [Google Scholar]
- 17.Cools M, Drop SLS, Wolffenbuttel KP, Oosterhuis JW, Looijenga LHJ. Germ cell tumors in the intersex gonad: old paths, new directions, moving frontiers. Endocr Rev. 2006;27:468–484. [DOI] [PubMed] [Google Scholar]
- 18.Farrugia MK, Sebire NJ, Achermann JC, Eisawi A, Duffy PG, Mushtaq I. Clinical and gonadal features and early surgical management of 45,X/46, XY and 45,X/47,XYY chromosomal mosaicism presenting with genital anomalies. J Pediatr Urol. 2013;9:139–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee PA, Nordenström A, Houk CP, et al. Global disorders of sex development update since 2006: perceptions, approach and care. Horm Res Paediatr. 2016;85:158–180. [DOI] [PubMed] [Google Scholar]
- 20.Sugawara N, Kimura Y, Araki Y. Successful second delivery outcome using refrozen thawed testicular sperm from an infertile male true hermaphrodite with a 46, XX/46, XY karyotype: case report. Hum Cell. 2012;25:96–99. [DOI] [PubMed] [Google Scholar]
- 21.Carson JC, Hoffner L, Conlin L, et al. Diploid/triploid mixoploidy: a consequence of asymmetric zygotic segregation of parental genomes. Am J Med Genet A. 2018;176:2720–2732. [DOI] [PubMed] [Google Scholar]
- 22.Fancsovits P, Tóthné ZG, Murber A, Takács FZ, Papp Z, Urbancsek J. Correlation between first polar body morphology and further embryo development. Acta Biol Hung. 2006;57:331–338. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


