Citation:
Aoun R, Kaul M, Sahni A. Excessive daytime sleepiness due to brain tumor. J Clin Sleep Med. 2020;16(12):2117–2119.
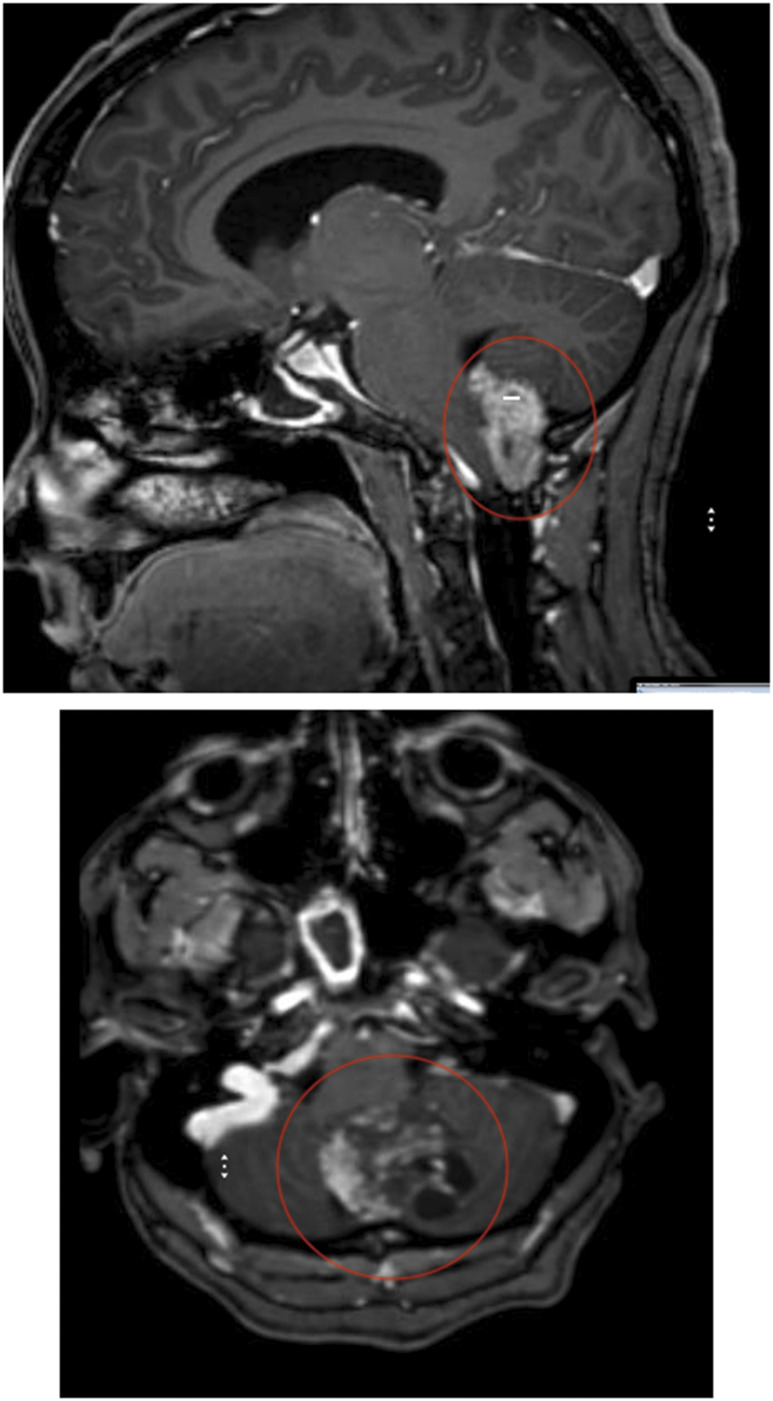
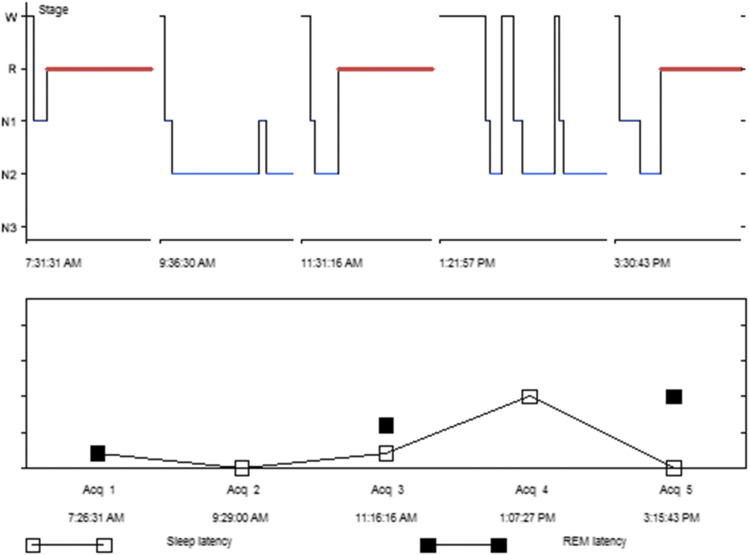
A 41-year-old woman presented to the sleep center for evaluation of excessive daytime sleepiness, which started after resection and brain radiation of a posterior fossa anaplastic ependymoma. She also endorses history of dream enactment at night and hypnogogic hallucinations. The patient does not have classic cataplexy but reported facial weakness with intense stress. She has no neurologic deficits after the treatment of the tumor but continued to have global headaches intermittently with no magnetic resonance imaging (Figure 1) proven recurrence of the disease. She is receiving topiramate for underlying migraine headaches. There is no family history of sleep-related disorders. She denied alcohol use but reports occasional marijuana use once or twice a month. Physical and neurological examinations are unremarkable. She then underwent a polysomnography, which showed no evidence of sleep-disordered breathing. Subsequently, she underwent Multiple Sleep Latency Testing (Figure 2), which revealed a mean sleep latency of less than 5 minutes and 3 sleep-onset rapid eye movement periods. A diagnosis of narcolepsy was made, which is likely associated with her prior central nervous system tumor.
Figure 1. MRI brain imaging showing post-resection (circled) area of previously located posterior fossa ependymoma.
MRI = magnetic resonance imaging.
Figure 2. Multiple Sleep Latency Test hypnogram.
REM = rapid eye movement, W = wake.
After establishing the diagnosis, the patient was counseled about nonpharmacological interventions including scheduled naps as well as options for pharmacological stimulant therapies. She was started on low-dose modafinil with a plan to slowly titrate the dose upwards every week. She eventually reached 200 mg of modafinil twice per day. Regular sleep medicine follow-ups were scheduled.
QUESTION:
1. Can posterior fossa tumors cause narcolepsy? 2. Can brain radiation cause sleep disorders?
ANSWER:
1. Yes. 2. Yes.
DISCUSSION
Secondary narcolepsy and hypersomnia due to a medical condition are not uncommon and have been frequently reported in children with brain tumors. Symptoms may emerge near the time of tumor diagnosis or during treatment. Patients with tumors located in the sellar and thalamic/hypothalamic regions, particularly those with craniopharyngiomas, are especially vulnerable to developing these disorders.1,2 This is due to the close proximity of the tumor to the orexin-producing cells in the hypothalamus, which are crucial in regulating wakefulness. These cells may be damaged by the tumor itself, during surgery, and during focal or whole-brain radiation.3
Studies show that patients tend to have more severe sleep disturbances when they are treated at a younger age, were given a radiation dose of more than 35 Gy, or had craniopharyngiomas.4 Hypersomnia and narcolepsy were also more common with midline tumors and radiation doses higher than 30 Gy in other studies. On the other hand, posterior fossa tumor location was found to be protective against the development of these sleep disturbances, which makes the presented case particularly interesting. There yet is no clear relationship between antiepileptic drug use and the development of sleep disorders in this patient population.3 A study by Armstrong et al5 showed that more than 90% of patients with primary brain tumor undergoing radiation therapy have reported hypersomnia.
SLEEP MEDICINE PEARLS
When patients with primary brain tumor present with excessive daytime sleepiness with no identifiable secondary contributors, hypersomnia and narcolepsy due to their medical condition should be suspected.
DISCLOSURE STATEMENT
All authors have participated in, read, and approved this manuscript. The authors report no conflicts of interest.
REFERENCES
- 1.Maloney M, Lewinter K, Ward SD, Perez I. Sleep disorders in children with central nervous system tumors. OBM Neurobiol. 2018;2(4):1–18. [Google Scholar]
- 2.Weil AG, Muir K, Hukin J, Desautels A, Martel V, Perreault S. Narcolepsy and hypothalamic region tumors: presentation and evolution. Pediatr Neurol. 2018;84:27–31. 10.1016/j.pediatrneurol.2017.12.016 [DOI] [PubMed] [Google Scholar]
- 3.Khan RB, Merchant TE, Sadighi ZS, et al. Prevalence, risk factors, and response to treatment for hypersomnia of central origin in survivors of childhood brain tumors. J Neurooncol. 2018;136(2):379–384. 10.1007/s11060-017-2662-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gapstur R, Gross CR, Ness K. Factors associated with sleep-wake disturbances in child and adult survivors of pediatric brain tumors: a review. Oncol Nurs Forum. 2009;36(6):723–731. 10.1188/09.onf.723-731 [DOI] [PubMed] [Google Scholar]
- 5.Armstrong TS, Shade MY, Breton G, et al. Sleep-wake disturbance in patients with brain tumors. J Neurooncol. 2017;19(3):323–335. [DOI] [PMC free article] [PubMed] [Google Scholar]