We report on patterns of neurodevelopment in children with single-ventricle anomalies and the predictive value of early evaluations for behavior at age 6.
Abstract
OBJECTIVES:
To determine if neurodevelopmental deficits in children with single-ventricle physiology change with age and early developmental scores predict 6-year outcomes.
METHODS:
In the Single Ventricle Reconstruction Trial, Bayley Scales of Infant Development, Second Edition, were administered at 14 months of age, and parents completed the Behavior Assessment System for Children, Second Edition (BASC-2) annually from the ages of 2 to 6 years. Scores were classified as average, at risk, or impaired. We calculated sensitivities, specificities, and positive and negative predictive values of earlier tests on 6-year outcomes.
RESULTS:
Of 291 eligible participants, 244 (84%) completed the BASC-2 at 6 years; more Single Ventricle Reconstruction participants than expected on the basis of normative data scored at risk or impaired on the BASC-2 Adaptive Skills Index at that evaluation (28.7% vs 15.9%; P < .001). Children with Adaptive Skills Composite scores <2 SD below the mean at the age of 6 were more likely to have had delayed development at 14 months, particularly on the Psychomotor Development Index (sensitivity of 79%). However, the positive predictive value of the 14-month Mental Development Index and Psychomotor Development Index for 6-year BASC-2 Adaptive Scores was low (44% and 36%, respectively). Adaptive Skills Composite score impairments at the age of 6 were poorly predicted by using earlier BASC-2 assessments, with low sensitivities at the ages of 3 (37%), 4 (48%), and 5 years (55%).
CONCLUSIONS:
Many children with hypoplastic left heart syndrome who have low adaptive skills at the age of 6 years will not be identified by screening at earlier ages. With our findings, we highlight the importance of serial evaluations for children with critical congenital heart disease throughout development.
What’s Known on This Subject:
Children with hypoplastic left heart syndrome and other related single-ventricle anomalies are at risk for neurodevelopmental impairments with a profile of deficits that evolves across different stages of development.
What This Study Adds:
We document increasing deficits in externalizing behavior problems and adaptive function by the age of 6 in children with single-ventricle anomalies. With our findings, we highlight the importance of understanding the implications of these emerging deficits on adaptation to school and learning challenges.
Survival rates for children with hypoplastic left heart syndrome (HLHS) and other single right ventricular anomalies have improved, although neurodevelopmental deficits remain prevalent.1–3 A variety of factors have been shown to contribute to adverse neurodevelopmental outcomes, including altered prenatal brain maturation, genetic anomalies, medical course, medical management strategies, socioeconomic status (SES), and parenting style.4–8 Neurodevelopmental deficits represent the most common long-term morbidity for children with HLHS and other complex congenital heart defects,9 negatively impacting their educational achievement, employability, and quality of life.10,11
Early identification of developmental and behavioral impairments allows for the implementation of therapies to potentially improve longer-term educational and occupational outcomes. Conversely, normal findings on developmental evaluations could provide much needed reassurance to parents of children with this high-risk profile, while also promoting the best use of early childhood resources.
In the Pediatric Heart Network Single Ventricle Reconstruction (SVR) Trial, newborns with HLHS and other related single right ventricular anomalies were prospectively enrolled and randomly assigned to a Norwood procedure by using either a modified Blalock-Taussig shunt or a right ventricle-to-pulmonary artery shunt.12,13 The Single Ventricle Reconstruction Extension Study (SVR-II) managed the initial SVR cohort with annual developmental assessments, completed via parent questionnaires, from 3 through 6 years of age.5,6,14 The purpose of this longitudinal surveillance was to analyze the patterns of neurodevelopmental deficits in this cohort over time, and the predictive value of early developmental and behavioral evaluations for adaptive behavior skills and behavior problems at 6 years of age.
Methods
The SVR Trial design and results of the 14-month and 3-year neurodevelopmental assessments have been reported previously.5,6 The details of the SVR-II trial and 6-year developmental and behavioral outcomes have also been documented.15 Transplant-free survivors from the SVR Trial (n = 373) were eligible to participate in SVR-II. Parents completed annual questionnaire assessments of child development and behavior when patients were 3 to 6 years of age.5 Research coordinators reviewed the medical records and interviewed parents annually to collect and update the medical history. Data collected included sociodemographic factors and information regarding serious adverse events, surgical and catheterization interventions, and participation in developmental therapies.14 The study was approved by the institutional review board of each of the 15 centers that participated. Parents and/or guardians provided written informed consent.
Measures
Patients completed the Bayley Scales of Infant Development, Second Edition (BSID-II) at 14 months of age. The BSID-II is a standardized measure of developmental skills for children from ages 1 to 42 months.16 It provides a Psychomotor Development Index (PDI) and a Mental Development Index (MDI) (normative mean = 100; SD = 15). Higher scores indicate better performance.
Developmental (Ages and Stages Questionnaires [ASQ]) and behavioral (Behavior Assessment System for Children, Second Edition [BASC-2])17 instruments were completed by parents of participants at 3, 4, and 5 years of age. Parents also completed the BASC-2 when the participant reached age 6. The BASC-2 parent report is used to measure the parent’s view of the child’s adaptive skills and problem behaviors in community and home settings. From 14 subscales, 4 composite scores are calculated (normative mean = 50, SD = 10): Internalizing Problems (eg, anxiety and depression), Externalizing Problems (eg, hyperactivity and aggression), Behavioral Symptoms Index (the overall level of problem behaviors), and Adaptive Skills Index (eg, functional communication and activities of daily living). For the purposes of this analysis, the Adaptive Skills Composite of the BASC-217 was the primary outcome measure of interest. For scales measuring behavioral problems, higher scores indicate a worse performance (ie, more problems); for scales measuring adaptive skills, higher scores indicate a better performance (ie, better skills).
The ASQ18 is a series of parent-completed questionnaires used to assess development in the areas of communication, gross motor skills, fine-motor skills, problem-solving, and personal-social skills. Different versions of the questionnaire are available for ages between 1 and 66 months. Each scale is scored as pass, at risk, or impaired, on the basis of age-specific cutoff points. There is good evidence to support the reliability and validity of this measure.19,20
Statistical Methods
BASC-2 scores were compared to population norms and were classified as follows: at least average (<1 SDs worse than the population mean), at risk (1–2 SDs worse than the population mean) and impaired (>2 SDs worse than the population mean). The categorization of BASC-2 scores was chosen to mimic ASQ categories and reflect clinical practice and decision-making. χ2 tests were used to assess whether the SVR-II cohort differed from expected on the basis of the normal distribution of population norms. Repeated measures logistic regression was used to test for changes over time in the proportion at risk or impaired (combined), compared to the average, in the population. To assess within-subject changes, we calculated sensitivities, specificities, positive predictive values (PPVs), and negative predictive value (NPVs) for measures administered at 14 months (BSID-II) and 3, 4, and 5 years (ASQ and BASC-2), predicting outcomes at the age of 6 years (BASC-2 Adaptive Skills). All analyses were conducted using SAS 9.4 (SAS Institute, Inc, Cary, NC), and statistical significance was tested at the level of 0.05.
Results
Participants
Among the 373 transplant-free survivors in the original SVR cohort, 325 enrolled in the Extension Study; of these, 14 had died by the age of 6 years, 14 underwent cardiac transplant, 3 were ineligible because they had undergone a biventricular repair, and 3 had withdrawn from the study before reaching the age of 6 years. Of the remaining 291 participants, 249 (86%) completed the BASC-2 at 6 years of age (Table 1). Compared with eligible patients who did not participate, those who completed the BASC-2 had a higher SES, were less likely to have a genetic syndrome, and tended to have had a higher score on the BSID-II MDI at 14 months of age (P < .05).
TABLE 1.
Demographic and Clinical Characteristics
| Completed BASC-2 at 6 y (n = 249) | Did Not Complete BASC-2 at 6 y (n = 106) | P | |||
|---|---|---|---|---|---|
| n | Mean ± SD or % | n | Mean ± SD or % | ||
| Race | .510 | ||||
| White | 205 | 82 | 82 | 77 | |
| Black | 33 | 13 | 19 | 17 | |
| Other | 10 | 4 | 4 | 4 | |
| Missing | 1 | 0.4 | 1 | 0.4 | |
| Ethnicity | .318 | ||||
| Hispanic | 40 | 1 | 22 | 21 | |
| Not Hispanic | 205 | 82 | 84 | 82 | |
| Missing | 4 | 2 | 0 | 2 | |
| Sex | .701 | ||||
| Male | 152 | 61 | 67 | 63 | |
| Female | 97 | 39 | 39 | 37 | |
| Genetic syndrome | .005 | ||||
| Yes | 6 | 2 | 8 | 8 | |
| No | 198 | 79 | 62 | 59 | |
| Missing | 45 | 18 | 36 | 34 | |
| Hollingshead score, SES | 233 | 41 ± 15 | 71 | 35 ± 16 | .004 |
| Norwood LOS, d | 249 | 31 ± 29 | 106 | 38 ± 40 | .111 |
| Age at Fontan, y | 241 | 3 ± 1 | 77 | 3 ± 1 | .100 |
| BSID-II MDI score | 229 | 90 ± 17 | 62 | 85 ± 17 | .062 |
| BSID-II PDI score | 229 | 75 ± 19 | 61 | 74 ± 20 | .687 |
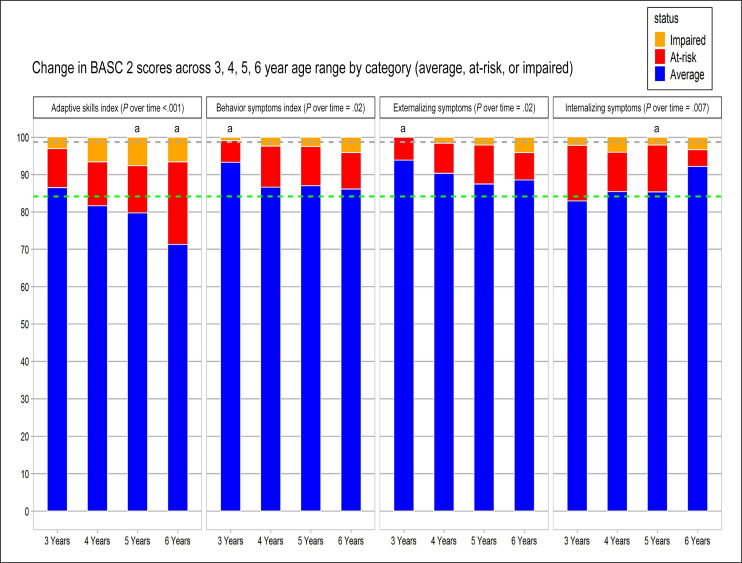
Changes Over Time in BASC-2 Profile
Behavior Symptoms Index
The greatest increase in the proportion of children characterized as being at risk or impaired occurred between the ages of 3 and 4 years (Fig 1; Table 2). This was largely due to the fact that parents of 3-year-old children with HLHS reported a lower rate of problem behaviors on the Behavior Symptoms Index than found in population norms (P = .007); the rate of reported behavior problems in children at 4 years of age was no different from expected from population norms. Parents were more likely to report behavior problems in their children at age 6 than at younger ages (P = .02).
FIGURE 1.
Longitudinal BASC-2 scores. The distribution of average (blue), at-risk (red), and impaired (orange) scores in each of the composite indices of the BASC-2 at 3, 4, 5, and 6 years of age is shown. The green and gray dotted lines represent the anticipated distribution of average and impaired individuals on the basis of a normal distribution. aBased on normal distribution you would expect 84.134% average, 13.59% at risk, and 2.275% impaired.
TABLE 2.
Change in BASC 2 Scores Across the 3, 4, 5, and 6 Years Age Range by Category (Average, At Risk, or Impaired)
| 3 y | 4 y | 5 y | 6 y | Population Norma | |
|---|---|---|---|---|---|
| BASC 2 Behavior Symptoms Index | |||||
| Average, % | 93 | 87 | 87 | 86 | 84 |
| At risk, % | 6 | 11 | 10 | 10 | 14 |
| Impaired, % | 1 | 2 | 2 | 4 | 2 |
| P compared with norms | .007 | .67 | .53 | .36 | — |
| P over time | .02 | — | — | — | — |
| BASC 2 externalizing symptoms | |||||
| Average, % | 94 | 90 | 87 | 89 | 84 |
| At risk, % | 6 | 8 | 11 | 7 | 14 |
| Impaired, % | 0 | 2 | 2 | 4 | 2 |
| P compared with norms | .001 | .10 | .50 | .07 | — |
| P over time | .02 | — | — | — | — |
| BASC 2 internalizing symptoms | |||||
| Average, % | 83 | 85 | 85 | 92 | 84 |
| At risk, % | 15 | 11 | 13 | 4 | 14 |
| Impaired, % | 2 | 4 | 2 | 3 | 2 |
| P compared with norms | .89 | .50 | .87 | .002 | — |
| P over time | .007 | — | — | — | — |
| BASC 2 Adaptive Skills Index | |||||
| Average, % | 86 | 82 | 80 | 71 | 84 |
| At risk, % | 10 | 12 | 13 | 22 | 14 |
| Impaired, % | 3 | 6 | 8 | 7 | 2 |
| P compared with norms | .58 | .15 | .04 | .004 | — |
| P over time | <.001 | — | — | — | — |
—, not applicable.
Expected on the basis of the normal distribution of these normed scales.
Adaptive Skills Index
The most significant deviations from population norms were noted on the measure of adaptive skills, for which the developmental trajectory revealed worsening scores with age (P = .001) and significant differences from norms at ages 5 and 6. At 3 years of age, 87% were classified as demonstrating age-appropriate adaptive skills, but, by the age of 6 years, only 71% of children were classified as demonstrating age-appropriate adaptive skills; at the age of 6 years, 22% (vs 14% expected on the basis of normal distribution) of children were rated as being at risk in terms of their adaptive skills, whereas nearly 7% (vs 2% expected) were rated as falling within the impaired range.
Externalizing Symptoms
The developmental trajectories for externalizing symptoms documented that, at 3 years of age, children were less likely to be reported by their parents as being at risk or impaired, compared to population norms (P = .001); overall, the percentage of children falling within the impaired range for externalizing symptoms increased with age (P = .02).
Internalizing Symptoms
The percentage of children classified as average, at risk, or impaired for internalizing symptoms was similar to population norms, with the exception that fewer children were classified as at risk for internalizing symptoms at 6 years of age (P = .002). The percent of scores in the average range increased over time (P = .007).
Early Predictors of At-Risk or Impaired BASC-2 Adaptive Skills at Age 6
Among the 29% of children who demonstrated at-risk or impaired adaptive skills at the age of 6 years, only 54% were within the at-risk or impaired range on the MDI at 14 months, whereas 79% had scored within this range on the PDI (Table 3). Of the children who scored within the at-risk or impaired range at the age of 6 on the Adaptive Skills Index, only 37% had been classified in this way at the age of 3, 48% at the age of 4, and 55% at the age of 5. The sensitivity of ASQ scores was also low (Table 4). Of the children showing at-risk or impaired adaptive skills at 6 years of age, the strongest finding was that 68% at the age of 4 and 63% at the age of 5 would have been classified as “fail” on the ASQ fine-motor index.
TABLE 3.
Sensitivity, Specificity, PPV, and NPV of At-Risk and Impaired Scores at the Age of 14 Months or 3, 4, or 5 Years Predicting At-Risk or Impaired BASC-II Adaptive Skills Scores at the Age of 6 Years
| At Risk or Impaired | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|
| BSID-II MDI, 14 mo | 54 | 73 | 44 | 80 |
| BSID-II PDI, 14 mo | 79 | 45 | 36 | 85 |
| BASC-2 Behavior Symptoms Index, 3 y | 26 | 98 | 70 | 89 |
| BASC-2 Behavior Symptoms Index, 4 y | 32 | 91 | 35 | 90 |
| BASC-2 Behavior Symptoms Index, 5 y | 41 | 94 | 54 | 90 |
| BASC-2 externalizing symptoms, 3 y | 22 | 96 | 45 | 90 |
| BASC-2 externalizing symptoms, 4 y | 30 | 93 | 35 | 92 |
| BASC-2 externalizing symptoms, 5 y | 36 | 91 | 35 | 91 |
| BASC-2 internalizing symptoms, 3 y | 19 | 84 | 10 | 92 |
| BASC-2 internalizing symptoms, 4 y | 37 | 85 | 18 | 94 |
| BASC-2 internalizing symptoms, 5 y | 41 | 89 | 24 | 94 |
| BASC-2 Adaptive Skills Index, 3 y | 37 | 98 | 91 | 79 |
| BASC-2 Adaptive Skills Index, 4 y | 48 | 97 | 84 | 83 |
| BASC-2 Adaptive Skills Index, 5 y | 55 | 96 | 84 | 85 |
The sensitivity is the hit rate percent impaired at age 6 who were impaired at age 14 months or 3, 4, or 5 years. The specificity is the percent not impaired at age 6 who were not impaired at age 14 months or 3, 4, or 5 years. The PPV is the precision percent impaired at 14 months or 3, 4, or 5 years who will be impaired at age 6. The NPV is the percent not impaired at 14 months or 3, 4, or 5 years who will remain not impaired at age 6.
TABLE 4.
Sensitivity, Specificity, PPV, and NPV of Pass and Fail ASQ Scores at Age 3, 4 or 5 Years Predicting At-Risk or Impaired BASC-II Adaptive Skills Scores at Age 6 Years
| ASQ Pass or Fail | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|
| ASQ communication, 3 y | 48 | 95 | 81 | 82 |
| ASQ communication, 4 y | 51 | 94 | 77 | 83 |
| ASQ communication, 5 y | 36 | 95 | 76 | 79 |
| ASQ gross motor, 3 y | 46 | 79 | 48 | 78 |
| ASQ gross motor, 4 y | 42 | 86 | 54 | 80 |
| ASQ gross motor, 5 y | 38 | 84 | 49 | 77 |
| ASQ fine motor, 3 y | 46 | 79 | 48 | 78 |
| ASQ fine motor, 4 y | 68 | 72 | 48 | 85 |
| ASQ fine motor, 5 y | 63 | 80 | 54 | 85 |
| ASQ problem-solving, 3 y | 46 | 90 | 66 | 80 |
| ASQ problem-solving, 4 y | 47 | 94 | 75 | 83 |
| ASQ problem-solving, 5 y | 43 | 97 | 84 | 81 |
| ASQ personal-social, 3 y | 35 | 94 | 70 | 78 |
| ASQ personal-social, 4 y | 22 | 99 | 93 | 77 |
| ASQ personal-social, 5 y | 34 | 96 | 78 | 79 |
The sensitivity is the hit rate percent at risk or impaired at age 6 who were impaired (fail) at age 3, 4, or 5 years. The specificity is the percent not impaired at age 6 who were not impaired (pass) at age 3, 4, or 5 years. The PPV is the precision percent fail at 3, 4, or 5 years who will be at risk or impaired at age 6. The NPV is the percent not impaired (pass) at 14 months or 3, 4, or 5 years who will remain not impaired at age 6.
Data related to the predictive value of early scores document that ∼44% of children with an at-risk or impaired MDI score at 14 months will reveal impaired adaptive skills at the age of 6 years. Only 36% of children with an at-risk or impaired PDI score at 14 months will go on to have impaired adaptive function skills at the age of 6 years. On the other hand, of those children who fell within the average range on the basis of their MDI score at 14 months, 20% went on to show at-risk or impaired adaptive skills at 6 years of age. For children obtaining an average range PDI score at 14 months, 15% went on to show impairments in adaptive functioning at 6 years of age.
Early at-risk or impaired BASC-2 Adaptive Skills Composite scores were strongly predictive of later scores at 6 years of age (Table 3), with values of 91% for the 3-year score and 84% at the ages of 4 and 5. The PPV of early ASQ scores on at-risk or impaired BASC-2 Adaptive Skills Composite scores at 6 years was strongest for the personal-social, problem-solving and communication scales (Table 4); in particular, the predictive value of a “fail” rating on the problem-solving scale for adaptive functioning increased from 66% to 84% from 3 to 5 years of age (Table 4).
Discussion
Children with HLHS and other complex congenital heart defects are at high risk for a variety of poorer outcomes; neurodevelopmental and behavioral deficits represent the most common long-term morbidities. By surveying a cohort of children with single-ventricle physiology through 6 years of age, the SVR-II has provided a unique opportunity to assess change over time in rates of neurodevelopmental deficits and address whether performance on measures of early development can predict adaptive function skill outcomes at 6 years of age.
We found that, by parent report of behavior symptoms, children were rated as experiencing fewer externalizing behavior problems, such as hyperactivity, aggression, and rule-breaking, at 3 and 4 years of age, in comparison with population norms and that they were rated by their parents as showing more externalizing behavior challenges at 6 years of age. This is consistent with findings reported by others revealing increased externalizing difficulties in children with age21 and in association with the experience of learning challenges at school.22 In contrast with externalizing behavior challenges, parents did not rate their children as showing elevations in internalizing behavior problems (eg, anxiety, depression) at any of the ages assessed; this has also been reported by others documenting parent ratings of child internalizing difficulties within the normal range for a similar age group.21
One of our most important findings relates to the trajectory of scores on the Adaptive Skills Index. Adaptive functioning refers to how an individual copes with the demands of everyday life and their level of personal independence relative to expectations for someone their age. Parent ratings of adaptive functioning in this cohort point to a significant decrease in these skills with age, such that by 6 years of age significantly more children were rated as falling within the at-risk or impaired range in this domain, in comparison to population norms. Rather than necessarily implying a regression or worsening of skills, this finding may, alternatively, reflect the fact that parents have an increased opportunity for social comparison with peers as their children enter school and they begin to appreciate differences in their independence and social functioning relative to other children their age.
Well-developed adaptive function skills are important in allowing children to successfully negotiate the early school years. Given the increased rates of impairment in our population at 6 years of age, our data provided a unique opportunity to explore whether early predictors of impaired adaptive skills at 6 years could be identified on the basis of performance on earlier measures of functioning (14 months and 3, 4, and 5 years). Our findings suggest that parent ratings of deficits in problem-solving skills and communication skills were strongly related to the rating of poor adaptive skills at 6 years of age. This underscores the importance of these early skills in promoting independence across a range of age-appropriate daily life skills. Our findings also point to the importance of early fine-motor skill development on later adaptive functioning. Children with weaker fine-motor skills are more likely to struggle in the early school years when there is emphasis on the child’s ability to print letters and numbers with ease, allowing them to focus on learning new concepts. Children who are still focusing on the process of forming letters and numbers are more likely to miss out on important concepts being taught and may begin to avoid tasks requiring written output. In turn, there is evidence that children who are making poor academic progress in the early school years are more likely to show greater parent-rated behavior problems.22
Although, with our findings, we do identify concerns related to adaptive functioning at the age of 6, we also document that a significant proportion of children (77%–85%; Table 4) who do not show early impairments on the ASQ remain unimpaired at the age of 6 years. This finding should provide some important reassurance for parents as they are counseled to continue to promote their child’s development.
The strength of this research was our ability to prospectively assess a large group of children from multiple centers across North America. Findings of this research, however, are limited by the fact that, with the exception of the 14-month Bayley Scales of Infant Development assessment, all assessments were completed by parent and/or guardian questionnaires and not by in-person evaluations. In the absence of objective, standardized evaluations, the data are subject to parent response bias. In addition, because not all parents returned questionnaires provided, the possibility of a selection bias remains. Importantly, our findings reveal that participants had fewer risk factors for impaired neurodevelopment and higher PDI and MDI at 14-months, compared with nonparticipants; in particular, participants reported a significantly higher SES than did nonparticipants. Given the well-documented, robust association between low SES and behavior problems in children,23 our results may in fact underestimate the degree of impairment in the single-ventricle population. An additional limitation relates to the fact that we were not able to determine the impact of access to early intervention services on outcome scores. Despite this, our findings suggest that it remains important to monitor and reassess even those children who benefit from and are discharged from early intervention because new concerns may emerge throughout development.
Conclusions
Our findings suggest that, although early measures of behavior problems can be helpful in identifying problems in behavior and adaptive skills for early school-aged children with HLHS, many children with HLHS who exhibit weaknesses in adaptive skills at the age of 6 years are not identified on the basis of assessments at an earlier age. Consistent with the concept of “growing into their deficits,” this is not surprising, given that the challenges noted at school age are emerging deficits that would not have been appreciated in early measures of development. A similar pattern of emerging deficits with age has been identified in infants experiencing other forms of early critical illness.24 With our findings, we further highlight the importance of considering how challenges may emerge and change with development and the expectations of different environments at different ages, therefore emphasizing the importance of serial evaluations and routine follow-up for children with congenital heart disease throughout the life span. Further studies are needed to elucidate the relationship between parent reports of child function and the child’s actual academic achievement and social functioning. To begin to address this need, evaluation of the Single Ventricle Reconstruction cohort (SVR-III trial) at 10 to 12 years of age is currently underway and will examine the relationship between findings at 6 years of age to later school-aged outcomes, including standardized in-person evaluations of child functioning.
Glossary
- ASQ
Ages and Stages Questionnaires
- BASC-2
Behavior Assessment System for Children, Second Edition
- BSID-II
Bayley Scales of Infant Development, Second Edition
- HLHS
hypoplastic left heart syndrome
- MDI
Mental Development Index
- NPV
negative predictive value
- PDI
Psychomotor Development Index
- PPV
positive predictive value
- SES
socioeconomic status
- SVR
Single Ventricle Reconstruction
- SVR-II
Single Ventricle Reconstruction Extension Study
Footnotes
Drs Sananes, Brosig, Goldberg, and Newburger conceptualized the study design, interpreted the results, drafted the manuscript, and worked with the other authors to revise the manuscript; Ms Hu and Dr Trachtenberg were involved with the study design, conducted the analysis, and edited the manuscript; Drs Gaynor, Mahle, Miller, Uzark, Mussatto, Pizarro, Jacobs, Cnota, Atz, Lai, Burns, Milazzo, and Votava-Smith were involved with the study design and interpretation of the results and participated in critical editing of the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by grants (HL068270, HL068290, HL 109673, HL109737, HL109741, HL109741, HL109743, HL109777, HL109778, HL109781, HL109816, and HL109818) from the National Heart, Lung, and Blood Institute, National Institutes of Health. The contents of this work are solely the responsibility of the authors and do not necessarily represent the official views of the National Heart, Lung, and Blood Institute. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPER: A companion to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2020-033043.
References
- 1.Goldberg CS, Schwartz EM, Brunberg JA, et al. . Neurodevelopmental outcome of patients after the Fontan operation: a comparison between children with hypoplastic left heart syndrome and other functional single ventricle lesions. J Pediatr. 2000;137(5):646–652 [DOI] [PubMed] [Google Scholar]
- 2.Mahle WT, Clancy RR, Moss EM, Gerdes M, Jobes DR, Wernovsky G. Neurodevelopmental outcome and lifestyle assessment in school-aged and adolescent children with hypoplastic left heart syndrome. Pediatrics. 2000;105(5):1082–1089 [DOI] [PubMed] [Google Scholar]
- 3.Tabbutt S, Gaynor JW, Newburger JW. Neurodevelopmental outcomes after congenital heart surgery and strategies for improvement. Curr Opin Cardiol. 2012;27(2):82–91 [DOI] [PubMed] [Google Scholar]
- 4.Licht DJ, Shera DM, Clancy RR, et al. . Brain maturation is delayed in infants with complex congenital heart defects. J Thorac Cardiovasc Surg. 2009;137(3):529–536–537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Newburger JW, Sleeper LA, Bellinger DC, et al.; Pediatric Heart Network Investigators . Early developmental outcome in children with hypoplastic left heart syndrome and related anomalies: the Single Ventricle Reconstruction trial. Circulation. 2012;125(17):2081–2091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goldberg CS, Lu M, Sleeper LA, et al.; Pediatric Heart Network Investigators . Factors associated with neurodevelopment for children with single ventricle lesions. J Pediatr. 2014;165(3):490–496.e8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cassedy A, Drotar D, Ittenbach R, et al. . The impact of socio-economic status on health related quality of life for children and adolescents with heart disease. Health Qual Life Outcomes. 2013;11:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rempel GR, Harrison MJ. Safeguarding precarious survival: parenting children who have life-threatening heart disease. Qual Health Res. 2007;17(6):824–837 [DOI] [PubMed] [Google Scholar]
- 9.Wernovsky G. Current insights regarding neurological and developmental abnormalities in children and young adults with complex congenital cardiac disease. Cardiol Young. 2006;16(suppl 1):92–104 [DOI] [PubMed] [Google Scholar]
- 10.Azakie T, Merklinger SL, McCrindle BW, et al. . Evolving strategies and improving outcomes of the modified Norwood procedure: a 10-year single-institution experience. Ann Thorac Surg. 2001;72(4):1349–1353 [DOI] [PubMed] [Google Scholar]
- 11.Wernovsky G, Newburger J. Neurologic and developmental morbidity in children with complex congenital heart disease. J Pediatr. 2003;142(1):6–8 [DOI] [PubMed] [Google Scholar]
- 12.Ohye RG, Sleeper LA, Mahony L, et al.; Pediatric Heart Network Investigators . Comparison of shunt types in the Norwood procedure for single-ventricle lesions. N Engl J Med. 2010;362(21):1980–1992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ohye RG, Gaynor JW, Ghanayem NS, et al.; Pediatric Heart Network Investigators . Design and rationale of a randomized trial comparing the Blalock-Taussig and right ventricle-pulmonary artery shunts in the Norwood procedure. J Thorac Cardiovasc Surg. 2008;136(4):968–975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Newburger JW, Sleeper LA, Gaynor JW, et al.; Pediatric Heart Network Investigators . Transplant-free survival and interventions at 6 years in the SVR trial. Circulation. 2018;137(21):2246–2253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goldberg CS, Hu C, Brosig C, et al.; PHN Investigators . Behavior and quality of life at 6 years for children with hypoplastic left heart syndrome. Pediatrics. 2019;144(5):e20191010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bayley N. Bayley Scales of Infant Development, 2nd ed San Antonio, TX: The Psychological Corporation; 1993 [Google Scholar]
- 17.Reynolds CR, Kamphaus RW. Behavior Assessment System for Children, 2nd ed Minneapolis, MN: Pearson; 2010 [Google Scholar]
- 18.Squires J, Potter L, Bricker D. The ASQ User’s Guide for the Ages and Stages Questionnaires: A Parent-Completed Child Monitoring System, 2nd ed Baltimore, MD: Brookes Publishing; 1999 [Google Scholar]
- 19.Squires J, Bricker D, Potter L. Revision of a parent-completed development screening tool: Ages and Stages Questionnaires. J Pediatr Psychol. 1997;22(3):313–328 [DOI] [PubMed] [Google Scholar]
- 20.Skellern CY, Rogers Y, O’Callaghan MJ. A parent-completed developmental questionnaire: follow up of ex-premature infants. J Paediatr Child Health. 2001;37(2):125–129 [DOI] [PubMed] [Google Scholar]
- 21.Brosig CL, Mussatto KA, Kuhn EM, Tweddell JS. Psychosocial outcomes for preschool children and families after surgery for complex congenital heart disease. Pediatr Cardiol. 2007;28(4):255–262 [DOI] [PubMed] [Google Scholar]
- 22.Bellinger DC, Newburger JW, Wypij D, Kuban KCK, duPlesssis AJ, Rappaport LA. Behaviour at eight years in children with surgically corrected transposition: the Boston Circulatory Arrest Trial. Cardiol Young. 2009;19(1):86–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reiss F. Socioeconomic inequalities and mental health problems in children and adolescents: a systematic review. Soc Sci Med. 2013;90:24–31 [DOI] [PubMed] [Google Scholar]
- 24.McNally H, Bennett CC, Elbourne D, Field DJ; UK Collaborative ECMO Trial Group. United Kingdom collaborative randomized trial of neonatal extracorporeal membrane oxygenation: follow-up to age 7 years. Pediatrics. 2006;117(5). Available at: www.pediatrics.org/cgi/content/full/117/5/e845 [DOI] [PubMed] [Google Scholar]