Abstract
Introduction:
Medicolegal concerns affect the career decisions of obstetrics/gynecology (OB/GYN) residents; however, their exposure to medicolegal education during residency training is virtually unknown.
Objective:
To assess the knowledge, attitudes, and perceptions of medicolegal concepts among OB/GYN residents.
Methods:
All residents in an accredited residency training program in OB/GYN in the United States during the 2017-2018 academic year were invited to complete an anonymous online survey.
Results:
Of the 5152 OB/GYN residents invited to complete the survey; nearly 17% (n = 866) responded. Basic medicolegal knowledge was poor. Almost 60% of respondents (n = 500) could not identify malpractice as a form of tort liability. Among respondents, 44% (n = 378) reported receiving no medicolegal education during residency, 21% (n = 181) were unsure, and 34% (n = 293) reported receiving some education. Of those who reported receiving medicolegal education, the majority, 66% (n = 549), received it informally: by “word of mouth” or by “observing colleagues.” Most (67%, n = 571) of the residents did not believe they had adequate exposure to medicolegal topics, and 19% (n = 163) were unsure. Ninety-two percent of residents (n = 782) reported concerns about being sued, and 67% (n = 571) believed that formal instruction during residency training may prevent lawsuits.
Conclusion:
Exposure to medicolegal topics during OB/GYN residency training is very limited and unstructured. This study showed that residents desire a more formalized medicolegal curriculum during postgraduate training and that implementation may have several benefits.
Keywords: resident education, medicolegal, legal, OB/GYN, obstetrics, gynecologic, education, law, health policy
INTRODUCTION
Medical malpractice influences practice patterns and affects health care delivery in the United States. It is especially relevant in OB/GYN, a medical subspecialty with one of the highest incidences of malpractice suits.1 A recent Medscape survey suggests that 85% of all OB/GYN physicians have been sued.2 In fact, The New England Journal of Medicine reported that by the age of 65 years, 99% of physicians in high-risk specialties will face a malpractice claim.1 As a result, approximately 50% of OB/GYNs have altered the scope of their clinical practice because of the real or perceived risk of malpractice litigation, and 40% report making changes to their clinical practice because of the availability and affordability of professional liability insurance.3 A survey of fourth-year OB/GYN residents identified Pennsylvania and New York as states most likely to be avoided for postresidency practice based on medicolegal risk.4 Historically, resident physicians were safeguarded from malpractice suits, but this same study revealed that 1 in 5 fourth-year OB/GYN residents has been involved in a lawsuit during residency.4
Medicolegal issues are important for any field of medicine, but especially for those in high-risk specialties such as OB/GYN. Arguably, residency is one of the best times to expose physicians to these concepts so they can integrate them into the practice of medicine while they learn the craft unique to their specialty. Despite this noted salience, little is known about the baseline knowledge of all OB/GYN residents and the extent and type of medicolegal education they receive. A survey of OB/GYN residency program directors conducted in 2005 by Hunt-Moreno and Gilbert5 found that 86% of program directors believed they provided formal and informal medicolegal instruction to their residents. Despite this, 88% believed that the curriculum was inadequate and too informal.5 Another study by Blanchard et al4 showed that approximately 50% of fourth-year residents believed they received some education in medical liability risk management in residency, but 80% reported they did not receive training in “next steps” after being named in a lawsuit. Of note, the way the education was delivered was not specified.4 When looking to other medical specialties for some guidance, surveys of internal medicine and family medicine residents illustrate a low level of medicolegal knowledge.6 One study reported that 96% of residents found medicolegal issues to be important, but only 28% believed that these issues were adequately addressed in their residency training.7
When formal medicolegal curricula were piloted in select emergency medicine and pediatric residency programs, residents demonstrated improved communication skills, expanded knowledge base, and increased recognition of documentation pitfalls.8-10 Despite data and dialogue suggesting benefits to implementation of formal medicolegal education during residency training, current medical education is lacking in this regard.11 The Accreditation Council for Graduate Medical Education (ACGME) does not have specific learning objectives or requirements for formal medicolegal curricula.12 There is a dearth of information about what OB/GYN residents know and how they are being exposed to these topics during training. The aim of our study was to describe the medicolegal training experience of OB/GYN residents in ACGME-accredited training programs and to investigate the knowledge, attitudes, and perceptions of medicolegal concepts among OB/GYN residents.
METHODS
All residents undergoing ACGME-accredited residency training in OB/GYN in the United States during the 2017-2018 academic year were invited to complete a voluntary, anonymous 16-question survey. The survey was developed by first identifying topics that were relevant to residents, drafting questions, and then reviewing them. The questions were then pretested on study team members. The team members reviewed the choice options, how the options were described, and the order of the options, and then provided feedback. The knowledge questions were reviewed by a member of the institution’s medicolegal department. The final set of questions was then modified on the basis of this feedback. An online survey (SurveyMonkey) link13 was emailed to OB/GYN residency program directors, program coordinators, or residents, who were asked to forward the survey to the program residents. The survey queried residents regarding their demographics (n = 4), their medicolegal knowledge (n = 4), the type of medicolegal education received during residency (n = 4), and the impact of potential litigation on their clinical practice and career plans (n = 4).
This study received exemption status by the Kaiser Permanente Northern California institutional review board. The primary outcome was the proportion of residents who felt their program’s medicolegal curriculum was insufficient. Secondary outcomes included the basic medicolegal knowledge of the residents, an inventory of current medicolegal curricula, and resident-reported perceptions of the impact of the medicolegal climate on their future practice and career trajectory.
Data were analyzed using descriptive statistics for demographics and survey constructs as well as bivariate analyses to assess demographic variations according to specific survey responses. Chi-squared and Fisher exact tests were used for categorical variables, and the Kruskal-Wallis test was used for continuous variables. The p values for overall comparisons were considered significant at less than 0.05. All analyses were performed using SAS 9.4 software (SAS Institute, Cary, NC).
RESULTS
Of 5152 possible respondents, 866 (17%) completed the survey. The respondents were equally geographically distributed among the 4 regions of the continental US (Table 1), as defined by the US Census Bureau. A similar number of residents from each training level responded to the survey: first year, 28.4% (n = 246); second year, 24.1% (n = 208); third year, 24.9% (n = 216); and fourth year, 22.5% (n = 195). Of the respondents, 86% (n = 738) identified as female, and 14% (n = 122) identified as male. Most respondents (70%, n = 604) were white. Almost 12% (n = 106) were Asian, 6% (n = 49) were black, 8% (n = 65) were Hispanic/Latino, and nearly 5% (n = 40) identified as other.
Table 1.
Survey respondents’ demographic characteristics and baseline knowledge.
| Characteristic | Number (%) |
|---|---|
| Demographic | |
| Sex (n = 864) | |
| Male | 122 (14.12) |
| Female | 738 (85.42) |
| Other | 4 (0.46) |
| Race (n = 866) | |
| Asian | 106 (12.24) |
| Black | 49 (5.66) |
| White | 604 (69.75) |
| Hispanic/Latino | 65 (7.51) |
| Native American | 2 (0.23) |
| Other | 40 (4.62) |
| Region (n = 865) | |
| Northeast | 255 (29.48) |
| Midwest | 242 (27.98) |
| South | 182 (21.04) |
| West | 186 (21.5) |
| Year of residency (n = 865) | |
| First | 246 (28.44) |
| Second | 208 (24.05) |
| Third | 216 (24.97) |
| Fourth | 195 (22.54) |
| Baseline knowledge | |
| Malpractice cap question (n = 836) | |
| Yes | 162 (19.38) |
| No/unsure | 674 (80.62) |
| Body of law question (n = 837) | |
| Correct (torts law) | 337 (40.31) |
| Wrong/unsure | 499 (59.69) |
| Alternative dispute question (n = 832) | |
| Yes | 75 (9.01) |
| No/unsure | 757 (88.99) |
| Malpractice claim question (n = 837) | 63 (7.53) |
| Yes | |
| No/unsure | 774 (92.47) |
Residents’ baseline medicolegal knowledge was poor. Most respondents (80%, n = 674) were not aware of whether their state law included a cap on medical malpractice damages, although respondents from the South and West regions were more familiar with damage caps in their states. Sixty percent (n = 500) could not name the body of law that encompasses medical malpractice. Only 9% of residents (n = 75) were familiar with the process of alternative dispute resolution, and 91% (n = 757) were unfamiliar or unsure. Only 8% (n = 63) of the respondents could name all 4 elements that plaintiffs must prove to make a successful medical malpractice claim (Table 1). The correct answer to the body of law question for medical malpractice was significantly different by year of residency (p = 0.004). Those who did know the correct answer were more likely to be third-year or fourth-year residents (Table 2).
Table 2.
Body of law for medical malpractice
| Year of residency | Correct (torts law), number (%) | Wrong/unsure, number (%) | Total, number | p valuea |
|---|---|---|---|---|
| First | 84 (35.4) | 153 (64.5) | 237 | 0.004 |
| Second | 69 (34.3) | 132 (65.6) | 201 | |
| Third | 90 (42.8) | 120 (57.1) | 210 | |
| Fourth | 94 (50.0) | 94 (50.0) | 188 | |
| Total | 337 (40.3) | 499 (59.6) | 836 |
a Chi-squared test.
Only about one third of respondents (35%, n = 293) reported receiving at least some formal medicolegal training. When asked about whether the training included formal lectures, 81% (n = 693) reported fewer than 3 hours of didactics, and 19% (n = 158) reported 3 or more hours of education, with little difference in response to this question by region. When asked to further describe the type of training offered by their residency programs, 29% of residents (n = 258) reported it was conveyed by physician faculty in formal lecture, and 30% (n = 262) reported that medicolegal attorneys or other experts gave formal lectures. However, 46% (n = 556) reported that education was delivered informally by “word of mouth” or by observing colleagues or mentors, and 15% (n = 131) reported no education at all. Most study participants (87%, n = 734) were either unsure or did not believe they received an appropriate level of exposure to medicolegal issues in their residency training, and 67% (n = 571) believed that education on medicolegal issues during residency would help prevent lawsuits during their medical career (Table 3).
Table 3.
Training characteristics
| Question or topic | Number (%) |
|---|---|
| Formal training question (n = 852) | |
| Yes | 293 (34.39) |
| No/unsure | 559 (65.61) |
| Hours of training question (n = 851), hours | |
| < 3 | 693 (81.43) |
| ≥ 3 | 158 (18.57) |
| Training provided believed sufficient question (n =847) | |
| Yes | 113 (13.34) |
| No/unsure | 734 (86.66) |
| Source of medical traininga (n = 1207) | |
| Attending physicians via formal lectures | 258 (29.79) |
| Medicolegal attorneys or other experts via formal lectures | 262 (30.25) |
| Word of mouth and observing colleagues or mentors | 556 (64.2) |
| No education about medicolegal issues | 131 (15.12) |
| Impact of training on career | |
| Prevent getting sued question (n = 849) | |
| Yes | 571 (67.26) |
| No/unsure | 278 (32.74) |
| Worry about being sued question (n = 852) | |
| Yes | 782 (91.78) |
| No/unsure | 70 (8.22) |
a Respondent could make multiple choices.
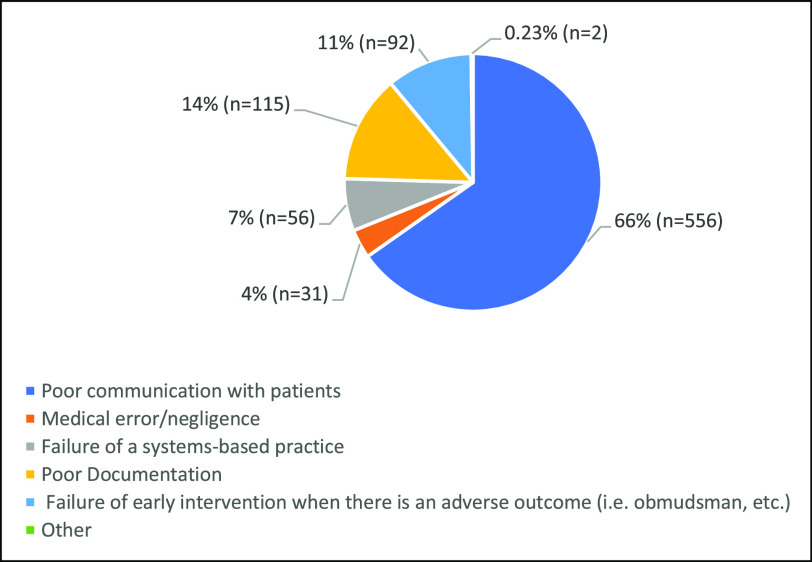
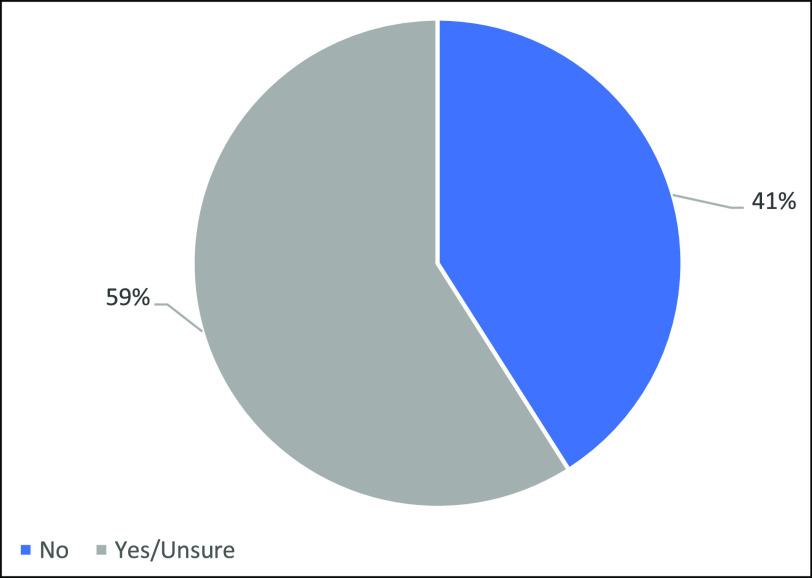
Of the respondents, 92% (n = 782) expressed concern over being sued during their OB/GYN career (Table 3). This rate was similar across the geographic regions (p = 0.41) and increased with each year of residency (Table 4). When asked their opinions on what inspired the most lawsuits in the field of OB/GYN, 66% of respondents (n = 556) listed poor communication, 14% (n = 115) named poor documentation, 11% (n = 92) identified failure of early intervention by risk management or an ombudsman during an adverse outcome, 7% (n = 56) believed it was due to a systems-based practice failure, 4% (n = 31) believed it was the result of medical error or negligence, and 0.23% (n = 2) believed suits were caused by other reasons (Figure 1). Almost 60% (59%, n = 491) of OB/GYN residents either believed medical malpractice trends might influence their choice of geographic location for their clinical practice or were unsure (Figure 2). The bivariate analysis showed that this response did not statistically differ by region (p = 0.19). There was no significant difference in response to the questions regarding the presence of formal medicolegal training (p = 0.76), hours of instruction, and exposure (p = 0.37) to education by region, but senior residents felt less hopeful that education may help prevent lawsuits (Table 5).
Table 4.
Residents’ concern over being sued
| By demographic characteristic | Number (%) | p valuea |
|---|---|---|
| Geographic region | 0.41 | |
| Northeastb | ||
| Yes | 228 (90.12) | |
| No | 12 (4.74) | |
| Unsure | 13 (5.14) | |
| Midwest | ||
| Yes | 216 (92.31) | |
| No | 13 (5.56) | |
| Unsure | 5 (2.14) | |
| South | ||
| Yes | 165 (92.18) | |
| No | 7 (3.91) | |
| Unsure | 7 (3.91) | |
| West | ||
| Yes | 173 (92.97) | |
| No | 10 (5.41) | |
| Unsure | 3 (1.67) | |
| Year of residency | 0.01 | |
| First | ||
| Yes | 214 (88.8) | |
| No | 13 (5.39) | |
| Unsure | 14 (5.81) | |
| Second | ||
| Yes | 186 (90.29) | |
| No | 17 (8.25) | |
| Unsure | 3 (1.46) | |
| Third | ||
| Yes | 196 (92.89) | |
| No | 8 (3.79) | |
| Unsure | 7 (3.32) | |
| Fourth | ||
| Yes | 186 (95.9) | |
| No | 4 (2.07) | |
| Unsure | 4 (2.07) |
a Chi-squared test.
b A few of the northeasterners did not respond to this question.
Figure 1.
Respondents’ opinions on causes of lawsuits.
Figure 2.
Impact of litigation on future geographic location of practice.
Table 5.
Medicolegal issues in curriculum by geography
| n | % | p valuea | |
|---|---|---|---|
| Medicolegal issues present Northeast | 0.76 | ||
| Yes | 88 | 34.78 | |
| No/unsure | 165 | 65.22 | |
| Midwest | |||
| Yes | 86 | 36.75 | |
| No/unsure | 148 | 63.25 | |
| South | |||
| Yes | 60 | 33.52 | |
| No/unsure | 119 | 66.48 | |
| West | |||
| Yes | 59 | 31.89 | |
| No/unsure | 126 | 68.11 | |
| Number of hours of instruction in curriculum Northeast, hours |
0.37 | ||
| < 3 | 206 | 81.42 | |
| ≥ 3 | 47 | 18.58 | |
| Midwest | |||
| < 3 | 195 | 83.33 | |
| ≥ 3 | 39 | 16.67 | |
| South | |||
| < 3 | 138 | 77.09 | |
| ≥ 3 | 41 | 22.91 | |
| West | |||
| < 3 | 153 | 83.15 | |
| ≥ 3 | 32 | 16.85 |
a Chi-squared test.
DISCUSSION
Our study found that OB/GYN residents are unfamiliar with basic medicolegal concepts. This supported the findings of Blanchard et al4 but provided a more in-depth analysis by quantifying and qualifying the deficit in knowledge previously identified. Although that prior study assessed only chief residents, this one studied all years of residency, quantified hours of training, qualified how the training was delivered, and examined differences by training level and location. Most residents were unaware of the body of law that malpractice falls under and the elements that constitute liability in a malpractice suit. Most residents were uninformed about caps on malpractice damage claims, although this varied by region, with respondents from the South and West regions exhibiting more knowledge about caps than those from the Northeast and Midwest. Despite the use of processes such as arbitration by health systems to settle malpractice claims, most residents were not familiar with alternative dispute resolution. Our study results show that OB/GYN residents are highly unprepared from a knowledge standpoint for potential lawsuits in the litigious climate in which they work.
Among those residents who reported receiving some medicolegal education, the minority reported that it was formal. The percentage of residents reporting exposure to medicolegal topics increased by year of training, suggesting they are more likely to be exposed in the latter part of residency training. When asked the quantity of time dedicated to medicolegal training, most residents reported 3 or fewer hours of instruction, and many specified it was by “word of mouth.” This corroborates the results of the studies by Blanchard et al4 and Hunt-Moreno and Gilbert,5 showing that even if instruction was given, it was inadequate. The bivariate analyses indicated that there was no statistically significant difference by region either in exposure to medicolegal topics or number of hours spent in teaching, suggesting that the deficiency in medicolegal training during OB/GYN residency may be nationwide.
Residents in OB/GYN across the United States do not believe they have adequate medicolegal education during residency and fear being sued in the course of their careers. Based on practitioner data about the prevalence of lawsuits, that fear is well founded. Although most survey respondents believed that education in residency may help in preventing lawsuits, the proportion of those answering “yes” was more likely to be junior residents. However, more senior residents expressed concern over being sued at some point during their careers, suggesting that as physicians progress in training, they have more exposure to a climate of lawsuits or feel more susceptible.
When asked about the most likely cause of lawsuits, most residents indicated poor communication or poor documentation. A smaller proportion believed that lawsuits are provoked by failure of a systems-based practice or failure of the hospital/medical group to provide a mediator when there are adverse outcomes. Respondents were given the option of an open-ended reply in naming other reasons for suits. The most commonly entered response was that the United States has a litigious society. Only 4% of OB/GYN residents thought lawsuits actually involved medical malpractice and erroneous physician-directed care. The 2017 Medscape study suggests that when all medical specialties are considered, the most common reasons for suits are a failure to diagnose a condition and a delay in diagnosis of a condition.2 However, when surgical specialties are considered independently, the most lawsuits originate from complications from surgery or treatment. Poor outcomes or disease progression was the next most common reply.2 Interestingly, for those sued, 22% wished they had better chart documentation, and 16% wished they had some improvement in communication or spent more time with the patient. Many wished they had known more about the overall processes and procedures involved in litigation. This shows that although the residents’ perceptions of what ultimately leads to suits may be misplaced, they are still accurate in identifying important contributing factors such as documentation and communication. Additionally, only 5% of the physicians in the Medscape study thought the lawsuit was warranted.2 This finding was similar to what the residents in the present study thought.
Our study found that medicolegal issues can affect resident career trajectories, a finding consistent with the studies by the American College of Obstetricians and Gynecologists3 and Blanchard et al.4 Forty percent of those surveyed reported that malpractice considerations may influence where they practice after residency, and 20% were unsure. Our study supports the previously identified notion that the medicolegal climate and state-specific medical malpractice laws will continue to have an impact on health care access, as providers continue to choose to work in states and system locations with more protections for health care providers. These results may be generalizable. Although our study examined only the OB/GYN specialty, it is reasonable to conclude that similar trends may be seen in other high-risk fields, such as neurosurgery or emergency medicine.
In addition to showing the effects of malpractice on career choices, these data also highlight the toll that litigation may take on practitioners individually. An older 2015 Medscape survey reported that approximately 50% of physicians (in all specialties) stated that being sued was a either a “horrible” experience or the “worst” experience of their lives.14 Other studies suggest that litigation may also lead physicians to leave the practice of medicine.15 Moreover, data suggest that women are more likely to be negatively affected by litigation than men.2 This is a concerning statistic because the OB/GYN field is becoming increasingly dominated by women, which implies that litigation may have a magnified effect on the OB/GYN provider population. The physician shortage is a well-known phenomenon facing the United States, and it limits patient access to care, especially in underserved areas. Our study findings support the idea that litigation may be one of the contributing factors to this shortage and highlight the need for education and the increasing importance of malpractice reform.
Recommendations
This conclusion then begs the question of what that curriculum should contain. Although some litigation may be unavoidable as the result of poor health outcomes or surgical complications, suits that originate from poor clinician documentation or communication may be remediable. A graduate medical education curriculum that focuses on communication and documentation would be an excellent place to start because it would likely serve to mitigate these risks and simultaneously assist with better delivery of patient care. Additionally, because most OB/GYN physicians find themselves involved in a lawsuit at some point in their careers, preparing OB/GYN residents with sufficient medicolegal knowledge and giving them exposure to the medicolegal process may make the process more familiar and less traumatic. As such, in addition to addressing documentation and communication, a good curriculum might also include legal basics and an overview of the litigation process from filing suit to judgment. The findings of Drukteinis et al8 and Harrison et al9 showed that exposing residents to a mock trial and a workshop on deposition preparation, respectively, were well received. A study by Evans and Refrow-Rutala16 implemented a more thorough, multiday intensive course, which included didactics covering legal basics, a practice case in a mock trial, a trip to the county courthouse, and question-and-answer panels with experts. The surgical residents who participated believed it was “essential” for graduating residents.16 If a national curriculum is put in place, future studies could then evaluate the short-term and long-term effects of the instituted curriculum such as determining whether the intervention of education does reduce the incidence of malpractice suits brought against those educated or whether they are able to cope better with the process as a result of their exposure to the curriculum.
Study Limitations and Strengths
Our study is not without limitations. Our response rate was 17%, which was not unexpected, given the study population and inherent difficulty with survey response. Of note, this response rate is typical for an external survey. However, the net number of respondents neared 1000, which allowed us to achieve statistical significance when comparing some of our subgroups and to provide precise estimates of the statistics. Additionally, all geographic regions and year of residency were well represented, and the makeup of the study population by sex mirrored national OB/GYN residency statistics.17 It was difficult to find national statistics on the complete, racial composition of the OB/GYN residency population, but the study population resembled the racial composition of OB/GYNs in practice.18
CONCLUSION
Residents in OB/GYN lack basic medicolegal knowledge, and they report inadequate exposure to medicolegal topics during training. Overwhelmingly, the results of this study show that residents desire more formal medicolegal instruction during residency.
Acknowledgments
Kathleen Louden, ELS, of Louden Health Communications performed a primary copy edit. We acknowledge Eve Zaritksy, MD, Miranda Weintraub, PhD, and Debbie Postlethwaite for assistance with developing the survey, organization of the project, and reviewing the manuscript.
Footnotes
Disclosure Statement: The author(s) have no conflicts of interest to disclose.
References
- 1.Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N Engl J Med 2011 Aug;365(7):629-36. 10.1056/NEJMsa1012370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Levy S, Kane L. Medscape malpractice report 2017. Published November 15, 2017. Accessed February 17, 2020. https://www.medscape.com/slideshow/2017-malpractice-report-6009206.
- 3.Carpentieri AM, Lumalcuri JJ, Shaw J, Joseph GF. Overview of the 2015 ACOG survey on professional liability. ACOG Clin Rev 2015. Nov;20(6):1-4. https://protectpatientsnow.org/wp-content/uploads/2016/02/ACOG2015PLSurveyNationalSummary11315.pdf [Google Scholar]
- 4.Blanchard MH, Ramsey P, Gala R, Gyamfi-Bannerman C, Srinivas S, Hernandez-Rey A. Impact of the medical liability crisis on postresidency training and practice decisions in obstetrics-gynecology. J Grad Med Educ 2012 Jun;4(2):190-5. DOI: 10.4300/JGME-D-11-00135.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hunt-Moreno C, Gilbert W. Current status of obstetrics and gynecology resident medical-legal education; A survey of program directors. Obstet Gynecol 2005 Dec;106(6):1382-1384. DOI: 10.1097/01.AOG.0000187895.59463.5b. [DOI] [PubMed] [Google Scholar]
- 6.Salstone S, Salstone R, Rowe B. Knowledge of medical-legal issues; survey of Ontario family medicine residents. Can Fam Physician 1997 Apr;43:669-3. PMID: 9111983 PMCID: PMC2255506 [PMC free article] [PubMed] [Google Scholar]
- 7.Kollas C. Exploring internal medicine chief resident’s medicolegal knowledge. J Leg Med 1997 Mar;18:47-61. DOI: 10.1080/01947649709511026 [DOI] [PubMed] [Google Scholar]
- 8.Drukteinis D, O’Keefe K, Sanson T, Orban D. Preparing emergency physicians for malpractice litigation: A joint emergency medicine residency-law school mock trial competition. J Emerg Med 2014 Jan;46(1):95-103. DOI: 10.1016/j.jemermed.2013.08.017. [DOI] [PubMed] [Google Scholar]
- 9.Harrison D, Hughes M, Teitlebaum H, Clark M, Omondi P, Palmer C, et al. Method of preparing emergency medicine residents for giving legal depositions. J Am Osteopath Assoc 1999 Jan;99(1):28-33. DOI: 10.7556/jaoa.1999.99.1.28 [DOI] [PubMed] [Google Scholar]
- 10.Otillio J, Park D, Hewett K, Losek J. Effectiveness of medicolegal lecture on risk-reduction medical record documentation by pediatric residents. Clin Pediatr (Phila) 2014 May;53(5): 479-85. DOI: 10.1177/0009922814527500 [DOI] [PubMed] [Google Scholar]
- 11.Gee R, Lockwood C; Medical Education and Health Policy. What is important for me to know, how do I learn it and what are the gaps? Obstet Gynecol 2013;121(1): 9-11. 10.1097/AOG.0b013e31827a099d [DOI] [PubMed] [Google Scholar]
- 12.The Obstetrics and Gynecology Milestone Project: A joint initiative of the Accreditation Council for Graduate Medical Education, the American Board of Obstetrics and Gynecology, and the American College of Obstetrics and Gynecology. Published September 2015. Accessed Feb 17, 2020. https://www.acgme.org/Portals/0/PDFs/Milestones/ObstetricsandGynecologyMilestones.pdf. [Google Scholar]
- 13.SurveyMonkey Inc Web site. Accessed Feb 17, 2020. https://www.surveymonkey.com. [Google Scholar]
- 14.Peckham C. Medscape malpractice report 2015: Why most doctors get sued. Published December 9, 2015. Accessed Feb 17, 2020. https://www.medscape.com/features/slideshow/public/malpractice-report-2015#page=27. [Google Scholar]
- 15.Studdert DM, Spittal MJ, Zang Y, Wilkinson DS, Singh H, Mello M. Changes in practice among physicians with malpractice claims. N Engl J Med 2019 Mar;380:1247-55. DOI: [DOI] [PubMed] [Google Scholar]
- 16.Evans, A, Refrow-Rutala, D. Medico-legal education: A pilot curriculum to fill the identified knowledge gap, J Grad Med Educ. 2010 Dec; 2(4): 595–599. DOI: 10.1056/NEJMsa1809981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Association of American Medical Colleges (AAMC) . ACGME residents and fellows by sex and specialty, 2015. Accessed Feb 17, 2020. https://www.aamc.org/data/workforce/reports/458766/2-2-chart.html.
- 18.Peckham C. Medscape Ob/Gyn lifestyle report 2017: Race and ethnicity, bias and burnout.. Published January 11, 2017. Accessed Feb 17, 2020. https://www.medscape.com/features/slideshow/lifestyle/2017/womens-health#page=6.