Abstract
Background
Hand therapists and health care providers across the spectrum have been profoundly impacted by COVID-19. Greater insight and information regarding how practitioners have been affected by this unparalleled pandemic is important.
Purpose
Survey research was performed to examine the impact of the COVID-19 pandemic on hand therapy practice.
Study design
Online survey research.
Methods
Four constructs guided the development of the survey: psychosocial and financial impact; safety practice patterns; changes in current practice patterns; use of telehealth. The survey was distributed to members of the American Society of Hand Therapists from April 14, 2020 through May 4, 2020. Descriptive demographic data were obtained. Frequencies were examined using ChiSquare, correlations were examined using Spearman Correlation Coefficient, and means were compared via independent t-test.
Results
A total of 719 members responded to the survey. Eighty-six percent of therapists reported feeling more stress than they did prior to the COVID-19 pandemic. This level of stress was similar across ages, practice settings, financial stability or instability, and geographical settings. Older therapists (rs = 0.04) and those that practiced longer (rs = 0.009) felt more comfortable with in-person treatment. Ninety-eight percent of therapists reported a decrease in caseload. Postoperative cases (P= .0001) and patients ages 19-49 were more likely to receive in-person treatment (P= .002). 46% of therapists reported providing telehealth services. Nontraumatic, nonoperative cases (P= .0001) and patients aged 65 or older were more likely to receive telehealth services (P= .0001). Younger therapists (rs = 0.03) and therapists working in outpatient therapist owned, outpatient corporate owned, and outpatient academic medical centers (X2 [4, N = 637] = 15.9463, P= .003) were more likely to utilize telehealth.
Conclusion
Stress was felt globally among hand therapy clinicians regardless of financial security or insecurity, age, practice area, or geographical setting. Therapists saw a drastic decrease in caseloads. In-person caseloads shifted primarily to postoperative cases.
Study Design
Web based survey
Keywords: Covid-19, Stress, Outpatient healthcare workers, Personal protective equipment, Telehealth, Hand therapy
Introduction
Published literature traced the beginning of a highly contagious and quick spreading disease back to the beginning of December 2019 with an inability to identify a causative agent.1 , 2 Since that time the etiology has been linked to the novel virus of the coronavirus (CoV) family and in February 2020, the World Health Organization announced that the disease caused by this new CoV was COVID-19, short for “coronavirus disease 2019.”3 Subsequently, in March 2020 the World Health Organization officially characterized the spread of COVID-19 as a pandemic.4
The impact this virus has had on health care providers across the globe is profound. It is clearly established that front-line workers have seen and experienced the most devastating ramifications with burdensome workloads and escalated risks of infection.2 This pandemic has far reaching effects across the healthcare spectrum notwithstanding the profession of hand therapy.
Traditionally, hand therapists bring a unique perspective to the treatment arena due to the strong psychological component involved with many hand and upper limb conditions, making the hand therapist's role important in the recovery and optimization of a patient's outcome.5 However, due to the recent pandemic hand therapists are faced with an unprecedented situation and extraordinary challenges of determining best practice and responsible patient care in the current environment of personal protective equipment (PPE), sudden utilization of telehealth, physical distancing, and the fear of escalating the spread of a potentially lethal virus. Moreover, hand therapists must also consider the personal health and financial implications for themselves and their families.
As hand therapists continue to navigate their way and understand their role in this tumultuous time, newer concepts such as telehealth and the importance of PPE continue to emerge. Although there is limited information and evidence currently available, research is emerging. In a recent rapid review and recommendations article,6 the use of face masks for allied health workers was discussed. Based on evidence from the influenza virus the authors infer that while surgical masks are not a reliable protector against a patient with COVID-19, the mask is useful to prevent personnel from an accidental aerosol incident from an asymptomatic carrier. Further, the authors explain that reducing the amount of viral load acquired, facemasks are protective as they likely reduce the severity of the illness.6
Telehealth is another service that has entered the arena of hand therapy. Previously telehealth had an extremely limited role and was primarily associated with rural or underserved areas. Prior to COVID-19 Medicare, Medicaid and most private insurance companies did not recognize rehabilitation codes or occupational therapy (OT) or physical therapy (PT) providers, therefore making this an unfamiliar area of practice for most hand therapists. Since the start of the pandemic some progress has been made in this area. However, a lack of clarity remains regarding appropriate coding, documentation guidelines, inconsistent reimbursement, and an unclear future for OT and PT as telehealth providers.
The psychological and emotional impact COVID-19 has had on hand therapists is unclear. However, considering the unusual and dramatic changes this virus has had on the typical work pattern of hand therapists it seems likely that the overreaching stressors from this pandemic will inevitably strike the hand therapy community. One recent publication reported that although health care workers often accept increased risk of infection as part of their chosen profession, they exhibit concern about family transmission, especially involving family members who are elderly, immunocompromized, or have chronic medical conditions.7 Similarly an article addressing anxiety in health care workers during COVID-198 identified several sources of anxiety, which included: access to proper PPE, exposure to the virus and taking it home to family, not having rapid testing if exposed, and fear of propagating the infection at work.8
Another concern is the financial impact that occurs as each state defines an “essential worker” and elective surgeries are prohibited, having a trickle down effect to the hand therapy profession with decreased caseloads, loss of revenue and less need for staff. According to the U.S. Bureau of Labor Statistics, the health care system cut 42,500 jobs in March as the CoV epidemic forced providers to delay an array of nonurgent procedures and doctor visits.9 It is reported that 96% of the health care jobs cut in March were on the outpatient side10 A plethora of information can be found in the literature regarding the impact COVID-19 has had on healthcare providers and the overwhelming challenges they face in delivering care.8 , 11, 12 However, there are no current studies specific to the impact this pandemic has had on hand therapy or the clinicians providing care during this tumultuous time. The purpose of this study was to gather information as to the personal and professional impact COVID-19 has had on the hand therapy community.
Methods
Survey development and design
Three members from the research division and a member of the education division for the American Society of Hand Therapists (ASHT) developed the survey to investigate the impact COVID-19 has had on its members. A 43-item survey regarding the effects COVID-19 has had on practice patterns as it relates to clinical, financial, personal, and psychological factors was developed. The survey included demographic questions, multiple choice questions that allowed for free text comments, and open-ended questions. It was designed to provide a comprehensive scope of how COVID-19 is affecting therapists on a personal and professional level and to better understand what factors may be playing a role in the responses. The questions were based on 4 constructs to explore the impact of COVID-19 on:
-
1.
Hand therapists, both psychosocially and financially
-
2.
Safety practice patterns.
-
3.
Current treatment practice patterns.
-
4.
Use of telehealth services
The survey was sent to other members of the ASHT research division for peer review. Following peer review, the survey and consent were submitted and received Institutional Review Board approval. Please refer to Appendix A for a copy of the survey.
Survey administration
The web-based survey was distributed through Qualtrics (Qualtrics, Salt Lake City, Utah) to active members of ASHT, and administration followed recommendations according to “Checklist for Reporting Results of Internet E-Surveys” (CHERRIES).13 The initial electronic distribution occurred on April 14, 2020 and was open for 21 days with a reminder email sent out on April 20, 2020. The survey closed May 4, 2020. The survey was designed so that it could only be completed one time per respondent. The survey was voluntary, and no incentives were offered for survey completion. Anonymity was maintained as identifiers (email addresses and names) were stored separately in a password protected electronic database.
Data analysis
Descriptive statistics, frequencies, and percentages were calculated using Microsoft Excel. Quantitative data were analyzed using the Statistical Package for the Social Sciences (SPSS version 26) and Microsoft Excel. Relationships between categorical values were analyzed using Chi-Square. Nonparametric correlations were analyzed using Spearman's Rank Correlation Coefficient. Parametric comparison of means were analyzed using an unpaired t-test. Inferential statistics were considered significant at .05 level. The authors examined the answers to the open-ended questions. These answers were read and grouped based on similar meanings. Key terms and interpretation of the meanings allowed categories to progressively emerge. Specific statements were chosen to highlight the communications within each category. Because this study was not a full qualitative study and we did not conduct interviews to fully explore ideas, we were unable to identify codes and themes. Rather, we were only able to categorize statements and utilize those statements to provide additional insight into the quantitative results. No qualitative software program was used.
To analyze state data, COVID-19 prevalence data were gathered on May 11, 2020 from two websites.14 , 15 The states (including the District of Columbia) with the lowest and highest COVID-19 cases per 100K were identified. Data from both websites was the same, and thus this data were used to examine the COVID-19 “hot spots” and non “hot spots” during the timeframe of the survey.
Results
Demographic data
Two separate e-mailings were sent to ASHT members (n = 2919; n = 2953). The emails were sent to active ASHT members; however, members were only allowed to take the survey once despite receiving two emails alerting them to the survey. A total of 877 members agreed to participate in the survey. However, due to a technical error in the initial hours of distribution, which was corrected quickly, only 719 responses were considered complete and eligible to be included in the survey. Not all 719 respondents completed 100% of the survey. If a respondent did not answer a question, then that individual answer was not included in any analysis. The total number of respondents per survey question is represented in tables, graphs, and text. Demographic data are represented in Table 1 .
Table 1.
Demographics
| N | Responses | Frequency (%) | |
|---|---|---|---|
| Profession | 756 | Occupational Therapist | 652(86) |
| Physical Therapist | 55(7) | ||
| Other* | 49(7) | ||
| Do you practice in the US | 702 | Yes | 687(98) |
| No⁎⁎ | 15(2) | ||
| Are you a certified hand therapist? | 710 | Yes, certification through HTCC | 598 (84) |
| No, but pursuing certification | 90(13) | ||
| Not currently, but previously held | 4(1) | ||
| No | 18(3) | ||
| Practice Setting | 686 | Outpatient-Hospital Based | 252(37) |
| Outpatient-Therapist Owned | 171(25) | ||
| Outpatient-Physician Owned | 146(21) | ||
| Outpatient- Corporate Owned | 80(12) | ||
| Outpatient - Academic Medical Center | 15(2) | ||
| Other | 22(3) | ||
| Practice Setting location | 685 | Urban | 234(34) |
| Suburban | 348(51) | ||
| Rural | 95(14) | ||
| Other | 8(1) | ||
| Position | 683 | Staff Therapist | 268(39) |
| Senior Therapist | 122(18) | ||
| Clinical Specialist | 117(17) | ||
| Clinical Supervisor or Specialist | 73(11) | ||
| Practice Owner | 62(9) | ||
| Other | 41(6) |
Most of other included CHTs 39/49.
Canada = 5; Australia = 3; New Zealand = 1; Bhutan = 1; Mexico = 1; No country listed = 4.
The average age of participants was 49.62 years (range 24-79). Therapists were licensed as either an OT or PT for an average of 24.61 years (range 0-52). A total of 646/680 therapists (95%) considered hand therapy an essential service. All states were represented with the exception of Arkansas and Rhode Island. The District of Columbia and Puerto Rico, along with Canada, Australia, New Zealand, Bhutan, and Mexico were also represented. See Table 2 for state data.
Table 2.
Represents distribution of respondent by state (some respondents reported working in more than one state)
| Respondents |
Respondents |
||||
|---|---|---|---|---|---|
| State | Percentage | Number | Percentage | Number | |
| Alabama | 0.44% | 3 | Montana | 0.44% | 3 |
| Alaska | 0.73% | 5 | Nebraska | 0.29% | 2 |
| Arizona | 2.19% | 15 | Nevada | 0.29% | 2 |
| Arkansas | 0.00% | 0 | New Hampshire | 0.44% | 3 |
| California | 10.53% | 72 | New Jersey | 4.24% | 29 |
| Colorado | 3.07% | 21 | New Mexico | 0.58% | 4 |
| Connecticut | 1.61% | 11 | New York | 5.12% | 35 |
| Delaware | 0.58% | 4 | North Carolina | 1.75% | 12 |
| District of Columbia | 0.58% | 4 | North Dakota | 0.29% | 2 |
| Florida | 5.26% | 36 | Ohio | 2.19% | 15 |
| Georgia | 2.92% | 20 | Oklahoma | 0.73% | 5 |
| Hawaii | 0.44% | 3 | Oregon | 3.07% | 21 |
| Idaho | 0.44% | 3 | Pennsylvania | 5.26% | 36 |
| Illinois | 4.97% | 34 | Puerto Rico | 0.00% | 0 |
| Indiana | 2.19% | 15 | Rhode Island | 0.00% | 0 |
| Iowa | 1.32% | 9 | South Carolina | 1.90% | 13 |
| Kansas | 1.02% | 7 | South Dakota | 0.15% | 1 |
| Kentucky | 0.88% | 6 | Tennessee | 1.46% | 10 |
| Louisiana | 1.02% | 7 | Texas | 3.36% | 23 |
| Maine | 0.73% | 5 | Utah | 1.17% | 8 |
| Maryland | 2.63% | 18 | Vermont | 1.02% | 7 |
| Massachusetts | 3.07% | 21 | Virginia | 3.65% | 25 |
| Michigan | 3.65% | 25 | Washington | 3.80% | 26 |
| Minnesota | 2.34% | 16 | West Virginia | 0.58% | 4 |
| Mississippi | 0.88% | 6 | Wisconsin | 1.90% | 13 |
| Missouri | 1.90% | 13 | Wyoming | .88% | 6 |
Quantitative analysis
The 4 constructs that guided development of the survey also guided analysis of the data.
Stress
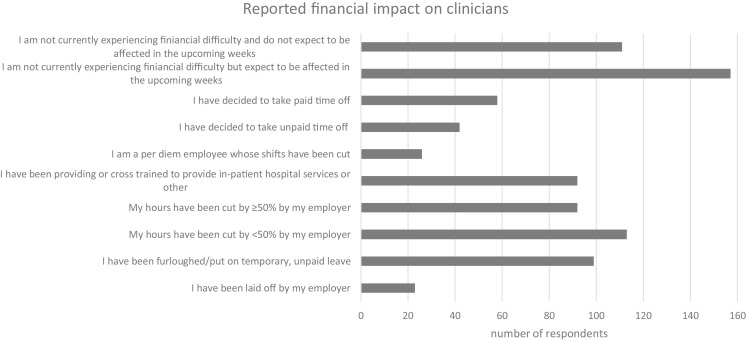
A total of 86% of therapists reported feeling more stress than they did prior to the COVID-19 pandemic (n = 549/642). Additionally, many therapists reported a financial impact during this time. See Figure 1 .
Fig. 1.
Reported financial impact on clinicians. *n = 556; multiple answers allowed.
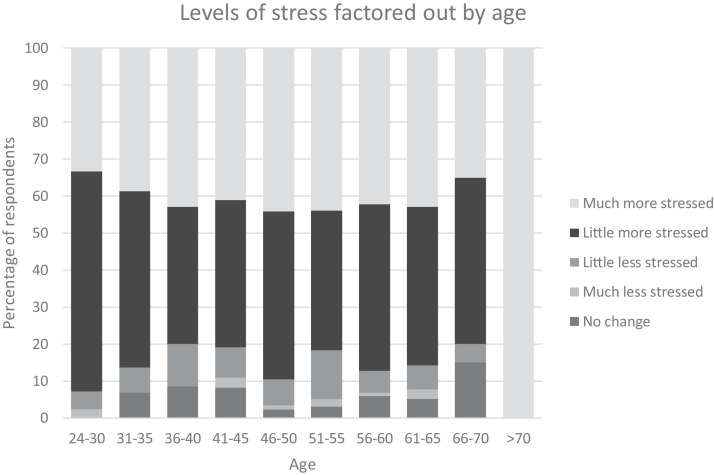
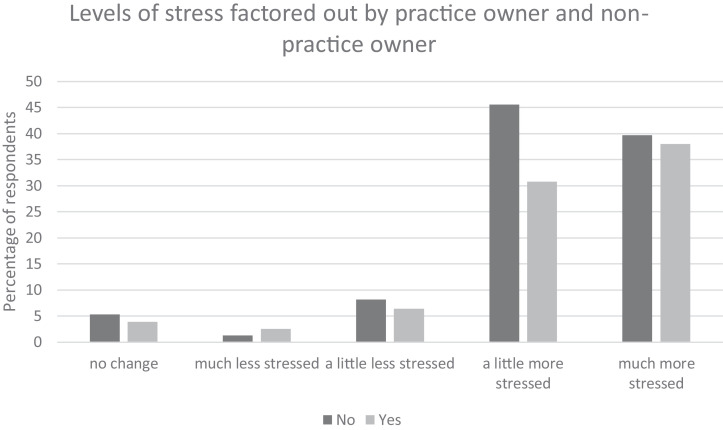
All levels of stress were compared to age, practice setting, and practice versus nonpractice owners. See Fig. 2, Fig. 3, Fig. 4 . None of these variables were found to be statistically significant. However, when just the higher levels of stress (“a little more stress,” “much more stress”) were factored out for those that owned a practice and those that did not, there was a statistically significant relationship between nonpractice owners and higher levels of stress (Fig. 4). See Table 3 for all correlation coefficients.
Fig. 2.
Percentage of those feeling different levels of stress and age. *Nonsignificant (rs = 0.30).
Fig. 3.
Percentage of those feeling different levels of stress based on practice setting location. *Nonsignificant (X2 [8,N = 633] = 2.6405, = P-.95).
Fig. 4.
Percentage of those feeling different levels of stress and hand therapy practice owner or nonpractice owner. *Nonsignificant (X2 [4,N = 640] = 8.254006, =P-.08) for all levels of stress. *Significant (X2 [1,N = 547] = 6.766878, =P -.009) for higher levels of stress (a little more stressed and much more stressed).
Table 3.
Correlation coefficients
| Correlation coefficient | Significance | |
|---|---|---|
| Age and stress | 0.22 | .30 |
| Age and comfort with in-person treatment | −0.08 | .04 |
| Age and telehealth | 0.78 | .03 |
| Years of practice and comfort with in-person treatment | −0.107 | .009 |
*Bold indicates significance.
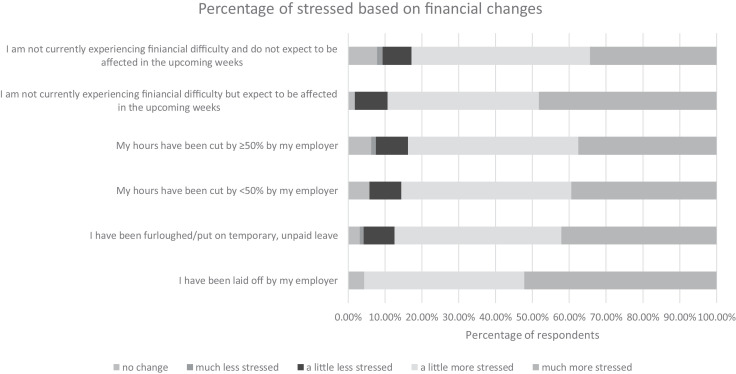
There were a limited number of responses in the “no change,” “much less stress,” and “a little less stress” categories. Therefore, only the higher stress level categories) were analyzed. The analyzed categories included those that reported financial impact due to a change in job status (hours cut by > or < than 50%, furloughed, or laid off) and those that expected or did not expect a financial impact. In both cases, none of these variables were found to be statistically significant (Fig. 5 ).
Fig. 5.
Percentage of those feeling different levels of stress based on changes in financial status. *Nonsignificant (X2[1,N = 103] = 1.609376,=P-.20) for expected or nonexpected financial impact and “a little more stressed,” “much more stressed.” *Nonsignificant (X2 [3,N = 261] = 0.712441,=P-.87) for change in work hours (reduction in work hours, furloughed, laid off) and “a little more stressed,” “much more stressed.”
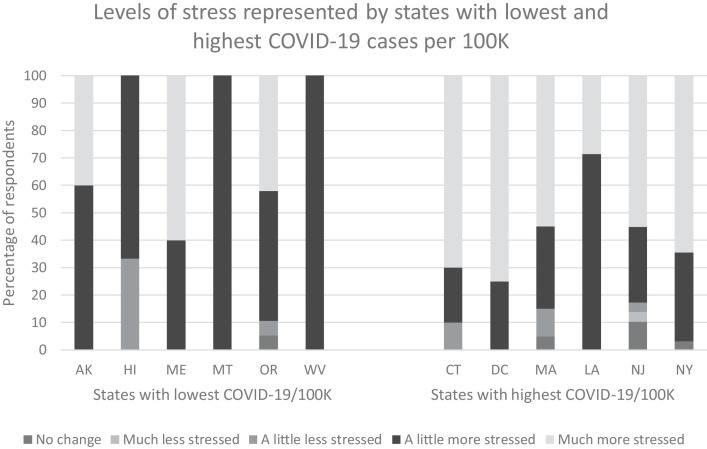
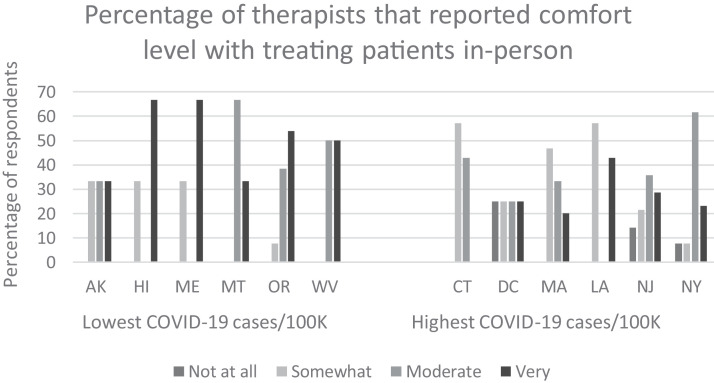
Visually, differences in stress levels appear increased in states with the highest cases of COVID-19 per 100K compared to states with the lowest cases of COVID-19 per 100K. Similarly, therapists in states with highest cases of COVID-19 per 100K appear to feel less comfortable treating patients however, due to the low number of respondents these findings were only analyzed descriptively. See Figures 6 and 7 .
Fig. 6.
Percentage of those feeling different levels of stress in lowest and highest COVID-19 cases per 100K. *Represents 6 states with lowest COVID-19 cases per 100,000 and 6 states with highest COVID-19 cases per 100,000.
Fig. 7.
Percentage of therapists that reported comfort level when treating patients in-person. *Represents 6 states with lowest COVID-19 cases per 100,000 and 6 states with highest COVID-19 cases per 100,000.
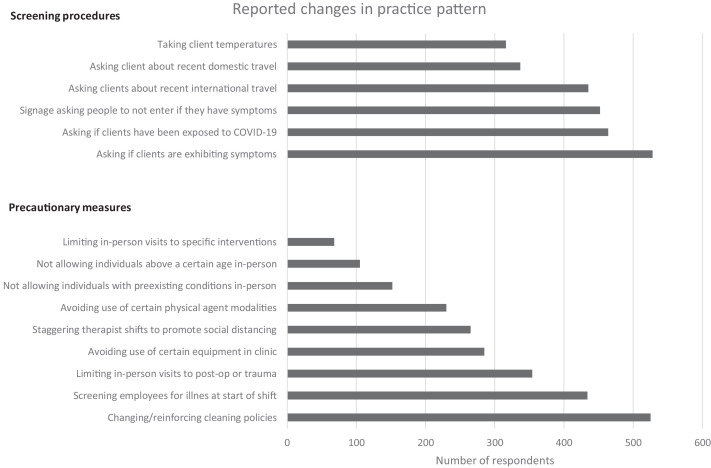
Safety measures
Only two respondents reported that no safety measures were being implemented at their facility, indicating that the majority of therapists experienced increased safety measures to improve safety of clients and staff. Refer to Figure 8 for safety measures implemented in practice settings.
Fig. 8.
Number of respondent answers regarding changes in practice patterns. *n = 580 (screening procedures); multiple answers allowed. *n = 585 (precautionary measures); multiple answers allowed.
Most therapists reported receiving PPE from their employer (n = 436/522; 84%). Surgical masks (n = 439) and gloves (n = 372) were the most common reported PPE. Additional PPE reported included homemade mask (n = 176), N95 respirator mask (n = 85), goggles (n = 42), face shield (n = 38), and gown (n = 10).
Comfort level treating patients in-person was also assessed and findings indicated that older therapists (rs = 0.04) and those that practiced longer (rs = 0.009) felt more comfortable with in-person treatment. Refer to Table 3.
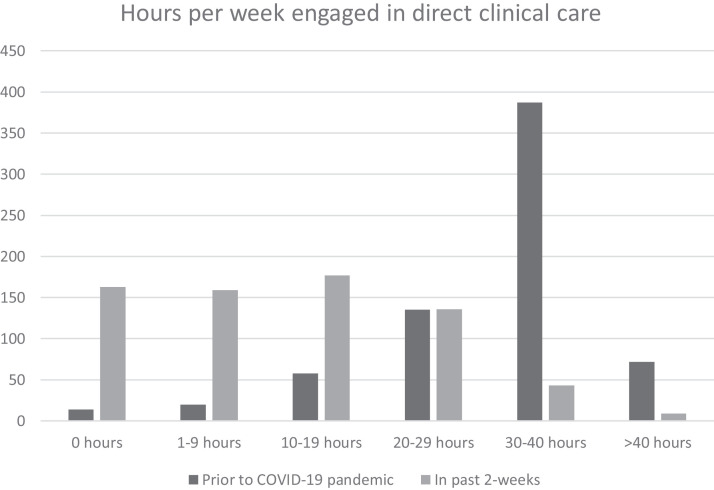
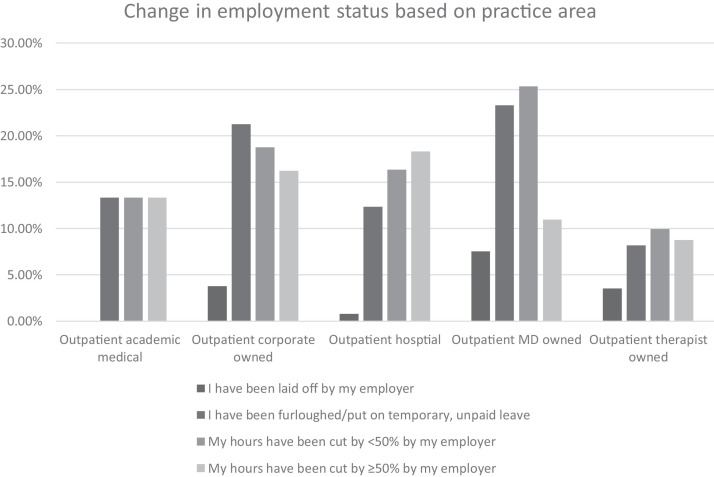
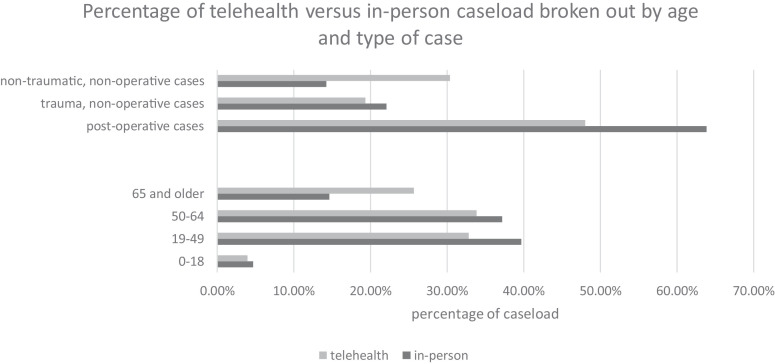
Practice changes
A total of 98% (671/684) of therapists reported caseloads decreasing during the pandemic. There was also a decrease reported in hours per week of direct clinical care and changes to employment status as captured during the survey timeframe of April 14, 2020-May 4, 2020. See Figures 9 and 10 . Postoperative cases were more likely to receive in-person treatment (t[738] = 6.84, P= .0001) and nontraumatic, nonoperative cases were more likely to receive telehealth services (t[730] = 7.94, P= .0001). Patients ages 19-49 were more likely to receive in-person treatment (t[745] = 3.1694, P= .002) and patients aged 65 or older were more likely to receive telehealth services (t[743] = 6.12, P= .0001). Refer to Figure 11 .
Fig. 9.
Number of hours in direct clinical care prior to and during COVID-19 pandemic (April 14, 2020 - May 4, 2020 timeframe). *n = 686 (prior to COVID-19 pandemic). *n = 687 (in past 2-weeks).
Fig. 10.
Percentage of respondents reporting change in employment status broken out by practice area. *n = 300 answered; multiple answers allowed. *n = 15 - outpatient academic medical; n = 80 - outpatient corporate owned; n = 251 - outpatient hospital; n = 146 - outpatient MD owned; n = 171 - outpatient therapist owned.
Fig. 11.
Percentage of telehealth versus in-person caseload broken out by age and type of case. Type of case: Postoperative cases t(738) = 6.84, P= .0001; Trauma, nonoperative cases t(727) = 1.723, P= .08; Nontraumatic, nonoperative cases t(730) = 7.94, P = .0001. Age: 0-18 t(745) = 0.76, P = .45; 19-49 t(745) = 3.1694, P = .001; 50-64 t(744) = 71.68, P = .09; 65 and older t(743) = 6.12, P = .0001.
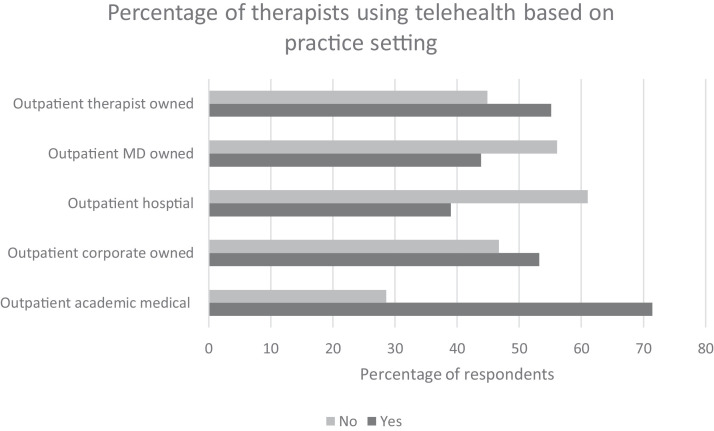
Telehealth
Only 28 therapists reported using telehealth prior to the COVID-19 pandemic. During the COVID-19 pandemic, 305 reported providing telehealth services in the past 2-weeks whereas 354 did not. More therapists reported receiving some telehealth training versus not (yes = 171; no = 123). Younger therapists were more likely to use telehealth than older therapists (rs = 0.03; Refer to Table 3). Therapists working in outpatient therapist owned clinics, outpatient corporate owned clinics, and outpatient academic medical centers were more likely to utilize telehealth and was confirmed statistically. See Figure 12 .
Fig. 12.
Percentage of therapists using telehealth based on practice setting
*Significant: (X2 [4, N = 637] = 15.9463, P = .003).
The most commonly used telehealth platform was Zoom (91%), followed by Doxy.me (71%), and Facetime (41%). Specific to reimbursement of telehealth services 66% of therapists expect the source to be from insurance companies while 34% were unsure. The most frequent codes or modifiers used for billing telehealth services included: GO, GT, and 95 modifiers, n = 71; Therapeutic exercise/97110, n = 56; Codes per insurance company, n =16. A total of 41 therapists stated they were unsure how to bill and 26 were not billing. The majority of therapists are not using a specific telehealth documentation system (70%). Strategies used to support clients who are not attending in person therapy included phone calls and email, with many in both groups reporting mailing supplemental home program materials.
Findings from open ended questions
To garnish a more complete picture of the impact of COVID-19 on hand therapy practice, there were opportunities for members to share reflections on how the COVID-19 pandemic is currently affecting or will affect future hand therapy practice. Several categories emerged from these open-ended questions.
Financial concerns
The keywords that emerged from this category were associated with loss and decrease, most frequently linked to revenue, although there was also an association to the idea of losing staff. One member expressed, “I have a 70% loss of revenue overall” while another participant stated, “Loss of income, planning for when and how my practice will reopen” and another member added, “Going broke, hoping to get the PPP loan so I can keep my staff.” Financial concerns were prevalent among both private practice owners as well as nonpractice owners.
Balancing sudden changes at home
The keywords that emerged from this category were centered around working from home and balancing multiple roles of homeschooling, several people working in the household, and childcare. Participants expressed concern over needing to continue to work in the clinic, but also having children at home that needed home schooling and care. Responses included this becoming a financial concern as they needed to take time off to tend to family members suddenly home, but did not have enough vacation time to get paid.
One person answered the open-ended question regarding further reflections about the overall impact of the pandemic with “too many…but as a single mom with little support, I don't have the time to delve into this question!” A participant echoed this feeling of uncertainty by stating “I'm not sure when I can return to work without childcare due to schools and daycares being still closed.”
Uncertainty about the future
Key words that surfaced in this category were- do not know/unknown, concern, and future. Numerous participants expressed uneasiness about the future ranging from indecision surrounding when schools and childcare may open, to vagueness around when, or if clinics will reopen. The following were remarks shared by respondents: “I am not sure how I can go back to work if my kids are still home” along with, “I don't know what the future holds, possibly a second wave of the virus” and another stated,” “Staff morale is low due to uncertainty about future events.” As with other categories, stress was a common thread as noted by this response: “Mentally the unknown situation and frequently changing situation is draining.” In other statements there was an unsettledness about whether clinics would survive or if they would have a job as a therapist in the future as shared by this response: “Other than being a mother and a wife I love being a hand therapist/ occupational therapist! I miss my patients and I don't know when I will get back to work. It doesn't look like it's going to end anytime soon.”
Practice changes
An overarching category related to practice changes emerged, and included subcategories such as decline in caseload, precautionary measures for hygiene, telehealth and loss of the human touch with patients. Many of the responses had a general undertone of ambiguity about permanency of the change. One of these concerns was the impact of social distancing as a sustainable practice pattern. As stated by one participant, “Staff are scared. Productivity will be decreased due to social distancing of patients. This is not a profitable model.” Another wrote “Patient care will be prioritized to manual therapy, wound care, and orthoses.” While another therapist stated that “I think it will affect offices that are overstaffed.”
Decline in caseload/services
Keywords that unfolded within this subcategory centered around the ideas of decreased/drop volume/referral, postpone, elective surgery. The primary thoughts expressed by participants focused on decreased volume associated with cancelation of elective surgeries, followed by modification of therapy services to include only postoperative or trauma patients, and lastly the recommendation for older adults to limit public outings. One member offered this thought: “Pending return of elective surgery our clinic may or may not return to pre pandemic status.” Similarly another participant summed up the change in caseload as this: “We are directly linked to physician practice, and most patients are traumatic or post op. I would anticipate severe loss of revenue stream until states are able to enter into Phase 1 of recovery, and elective surgeries are resumed. I believe my practice will decrease in volume due to the high percentage of elderly in my typical case load.”
Precautionary measures
Key words associated with this subcategory included- use of masks, physical distancing, and sanitization/cleanliness and how that may impact what techniques and equipment are used therapeutically. Many participants reported that they feel as though physical distancing, changes in disinfectant practices, and PPE are here to stay and will become a standard in the hand clinic. As stated by one participant, “I think we are going to have a new normal of wearing face masks and scrubs when treating patients.” Another participant indicated that precautionary measures may impact how long patients continue therapy- “Patients may choose to switch over to a HEP sooner than recommended to limit exposure.” Therapists also identified the strict disinfecting regimen as critical for preventing the spread of the virus while also recognizing the extra time required to complete this task- “Despite seeing fewer patients due to more 1:1, I won't have any extra time due to the amount of cleaning and sanitizing I will need to do.” Several therapists mentioned the idea of plexiglass dividers becoming typical in the clinic and that Fluidotherapy may become “a thing of the past.” Therapists expressed concern about contracting COVID-19 as well as the fear of exposing family members. One therapist who was furloughed said “I am very stressed as I have family and friends who are very sick with Covid, including therapists who did contract it from patients in facilities that were not using proper precautions so I am very nervous of when I return.” “I worry about bringing something home to them or getting sick myself.” A response that sums up most of the open-ended answers regarding hand therapy hygiene, disinfectant and PPE practices is: “I believe we will need to continue strict precautions including face shield and mask. We work in such close contact with patients that unless this COVID-19 is irradiated I believe precautions will be long standing for patient and staff protection.”
Role of telehealth services
Key words revealed in this subcategory were specific to the topic- telehealth, telerehab, and e-visits. There was some dichotomy in the responses regarding telehealth. Many participants expressed skepticism and were troubled that virtual visits would replace traditional therapy, as acknowledged by this response: “I am concerned that tele-health will be justified by insurance companies and attempt to take the place of in person visits, which I believe is not comparable.” Others embraced the idea of e-visits and telehealth as described in this response: “Hoping the use of e-visits and telehealth use for this pandemic will be used as an advocacy strategy to again advocate for the therapies to be included on a permanent basis,” while another indicated “We need to establish better resources and training for telehealth services at the clinician and organizational level, it should be standard practice to have telehealth as an option for clients.”The open-ended comments about telehealth were the most frequently observed of all qualitative categories. Several participants echoed the statement “Telerehab is probably here to stay, in one form or another.”
Human touch/physical contact
Key words emerging with this subcategory included- manual therapy, touch, face to face, and hands-on. The members expressed concern over face to face hands on care being greatly reduced after stay at home and other restrictions or COVID-19 are lifted, and that this change may affect quality of care and professional enjoyment as a hand therapist. This category overlaps with the telehealth category as several members linked the two stating that with the inevitable advent of increased telehealth by hand therapists, the face to face, hands on care in the clinic will decrease. The concern for human touch being an integral part of success in therapy is expressed in the following quotes taken from the survey: “I'm afraid that manual therapy will be under emphasized and the face to face contact may not be appreciated,” and “I feel that one of the most important parts of hand therapy is the touch and relationship that is achieved in the clinic,” with even stronger statements of “Very difficult to provide or allow for tactile input to the patients’ hands, which is crucial in neuromuscular and sensorimotor re-education”, and “manual hands on therapy is our bread and butter.” One therapist expressed that “manual treatment is one of the biggest interventions that sets us apart.” Another said, “The services we offer are best performed in proximity to the patient through hands on care and when will this return?”
Discussion
The survey results captured the significant changes that occurred in the hand therapy profession from April 14, 2020 to May 4, 2020. During this timeframe, the majority of states had implemented stay-at-home orders, school closures, and restricted business operations.14 , 15 Additionally, many countries around the world were implementing strategies to address the pandemic. We refer to this timeframe as the height of the spring 2020 COVID-19 pandemic. Our survey revealed that during this timeframe, therapists experienced increased stress, feelings of uncertainty, and significant practice pattern changes.
The Department of Homeland Security deemed both occupational and physical therapy services essential during the COVID-19 response and described these jobs as essential for continued national critical infrastructure viability.16 Research supports that for many upper extremity musculoskeletal conditions, interventions within the scope of therapy increase function and decrease pain.17, 18, 19 However, how these essential services are delivered in the future may be different as a result of the COVID-19 pandemic. During our survey timeframe, individuals who had surgery received significantly more in person treatment then telehealth. While the majority of the respondents deem hand therapy as essential (95%), some therapists acknowledged in the open-ended questions that not all hand therapy services are essential. It is important during a pandemic to recognize that many of our services are essential; however, the lessons learned during the spring 2020 COVID-19 pandemic may help the hand therapy profession to better delineate essential services, and identify those services that need to be delivered in-person versus ones that can be effectively delivered via telehealth.
Increased levels of stress were reported by most of the participants, and this increased stress level appeared consistent across practice areas, financial stability, current job status, age, and geographical areas despite the fact that during April 14, 2020-May 4, 2020, some states were experiencing a significant crisis and major restrictions (eg, NY and NJ), while other states experienced few cases and very little restrictions (eg, MT and AK). Most clinicians experienced a significant decrease in direct client hours and many had a reduction in overall work hours. Even therapists that were not impacted financially and did not expect to be impacted financially experienced the same levels of stress. Just following the COVID-19 pandemic outbreak in China, two large scale20 , 21 surveys and one smaller scale survey22 were distributed to understand the scope of psychological distress among the general population during the height of their pandemic. Results indicated that 35% of the general population experienced increased psychological distress,20 54% reported a moderate or severe psychological impact21 and general increased levels of anxiety were similar despite whether one had the virus, was in quarantine, or was part of the general public.22 Women,20 , 21 migrant workers,20 college age students,21 people with poor health,21 and people in the middle region of China20 (which was at the epicenter of the pandemic), reported significantly higher levels of psychological distress. The general public and those that had the virus exhibited significantly more anxiety-like behaviors.22 Similar to these studies from China, we found global increased levels of stress across all therapists.
In an attempt to further understand the construct of stress during the COVID-19 pandemic, 2 sets of authors23 , 24 have designed, and started the process of validating surveys associated with stress and fear during the COVID-19 pandemic. Both of these surveys are still in the infancy phase and have yet to be utilized, thus it is challenging to fully understand the constructs that contribute to increased stress during the COVID-19 pandemic. Healthcare workers during a pandemic are at risk for increased stress and anxiety just by the nature of their work.25 , 26 In addition to their work setting, there are other factors such as overall health status, age, and financial security that would appear to lead to increased levels of stress during the COVID-19 pandemic; however, there are mixed results in the literature related to how much these variables were associated with increased stress during this time.20, 21, 22 In our study, some less obvious factors such as children being home from school and learning via distance education, families suddenly all working together in the house, and daycares closed were identified through open-ended survey questions and may be hidden stress variables yet to be captured in the literature. These sudden changes to work/life balance were also reported descriptively by Sahu et al27 in their survey of orthopedic surgeons in India during the 3-week lockdown in that country. These stresses centered around the need to suddenly dual task (home school and work from home) and needing to work in the clinic while kids were home along with the stress of potentially bringing the virus to the household are stressors that are worth exploring in greater detail.
There were significant changes in clinical practice during the COVID-19 pandemic. Changes ranged from a drastic caseload reduction, to a decrease of full-time direct clinical care hours per week, to the implementation of precautionary measures in clinical settings, to the sudden use of telehealth. Physical distancing, the ban on elective surgeries in many states28 and the prioritizing of trauma and non-elective post-surgical cases caused a sudden decrease in direct clinical care, which led to the reorganization of staff resulting in people being laid off, furloughed, or assuming a reduction in work hours. While the long-term implications of such drastic changes in clinical practice in such a short period of time are unknown, some interesting short-term findings emerged from the survey. In our study, 98% of therapists reported a caseload decrease during the height of the spring 2020 COVID-19 pandemic, and only 43 participants reported 30-40 hours/week of direct clinical care compared to 387 prior to the height of the spring 2020 COVID-19 pandemic. A higher percentage of therapists that practice in outpatient, physician-owned practices were laid off than in other practice areas. In-person treatment changed with people aged 19-49 and postoperative cases more likely to receive in-person treatment. To our knowledge, this sudden change in practice in outpatient rehabilitation was reported in only one other survey.27
One of the more drastic practice changes observed in this study was the sudden move to telehealth rehabilitation. Telehealth in rehabilitation had been slowly gaining traction as a viable method of conducting orthopedic assessments29 , 30 and receiving needed therapy services.31, 32, 33 However, the COVID-19 pandemic resulted in a drastic, unexpected, and unplanned swing to telehealth, as a result of sudden state restrictions and the Centers for Disease Control and Prevention's recommendation to explore alternatives to face-to-face visits with a specific recommendation of “promoting the increased use of telehealth.”34 In our survey, only 28 therapists reported using telehealth prior to the COVID-19 pandemic. During the height of the spring 2020 COVID-19 pandemic, that number rose to 305. Other practice settings also reported a sudden increase in telehealth visits during the COVID-19 pandemic.35 Those more likely to receive telehealth services were non-traumatic, non-operative clients and clients aged 65 or older.
In the present survey, there was a significant relationship between age and therapists’ utilization of telehealth. From a clinical perspective, this relationship between age and telehealth is worth exploring. A recent study aimed at assessing readiness of use of medical apps from physicians in Australia found that younger physicians used more medical apps at work and yielded higher readiness for telehealth scores than physicians over age 44.36 In our study, we also found that younger therapists were more likely to use telehealth. There is speculation that older clinicians may feel less comfortable utilizing telehealth; however, this is only speculation as our survey did not examine variables that influence the utilization of telehealth. In a literature review Dziechciaz and Fillip37 (p847) presented the aging processes of humans and changes in bio-psycho-social areas. In their study they found that “with age, there are increasing difficulties in adapting to new situations.” Perceived apprehension in this age group could be related to the need to learn several new technologies and during the case of the COVID-19 pandemic, learning these technologies at a rapid pace of change.
Perceived apprehension in this age group could also be the result of paradigms engrained regarding service delivery through years of providing therapy in person. In an account of a thoracic surgery practice transitioning to almost exclusive telehealth outpatient practice during the COVID-19 outbreak, they describe one of their challenges as “some providers may not have adequate experience in this modality and there may be a learning curve associated with engaging patients through the telehealth platform.”38 (p7)
Training and experience have been shown to increase positive attitudes toward telehealth in providers39 , 40 while lack of training, resistance to change, technically challenged staff, and age, among other themes, were identified in a systematic review as barriers.41 Implementing telehealth at short notice was a response to COVID-19 stay at home orders and concern over spreading the disease rather than a service that was provided customarily in most clinics. In an article discussing the use of telehealth in global emergencies, the authors stress the need to implement telehealth proactively in order to be better prepared for pandemics and other emergencies.42 These authors also suggest that formal telehealth strategies are needed and that it would be important to include telehealth in medical curricula. These findings and suggestions are echoed in an article describing the use of telemedicine in an orthopedic practice that performs primarily total joint arthroplasties.43 In our study, only 171 therapists reported receiving some telehealth training. However, it is important to note that the switch to telehealth during the COVID-19 pandemic was sudden and adequate training was likely not plausible. Variables that predict clients liking or preferring telehealth include lack of medical insurance, female gender, an understanding of telehealth, and convenience.44 Recognizing these variables and providing education and training to all clinicians along with having guidelines in place proactively may reduce stress around use of telehealth in times of emergency and may help with a paradigm shift to an accepted delivery model of telehealth.
In addition to appropriate training to provide telehealth services, appropriate remuneration for services is also necessary.42 In response to COVID-19 the passage of the CARES Act (P.L. 116-136) allowed the Centers for Medicare and Medicaid Services (CMS) to waive telehealth restrictions and recognize therapy Current Procedural Terminology (CPT) codes. Initially, OTs and PTs were not recognized as providers of telehealth services, however on April 30, 2020 it was announced that CMS would recognize OT and PT as providers for the duration of the pandemic and retroactive to March 1, 2020. Although many private insurance companies and workers’ compensation are recognizing OT and PT as telehealth providers, the guidelines have significant variations between companies and most insurance companies including CMS have not committed to OT and PT telehealth services as part of a long-term member benefit.
Therapist's comfort level treating patients in person was examined in the present study and it was found that older therapists and therapists with more years of experience felt more comfortable treating patients in-person during the COVID-19 pandemic. This is an interesting finding given that older individuals are considered more “at risk” with the COVID-19 virus than younger individuals. Other studies have shown that experience with past epidemics and knowledge on proper use of PPE has decreased stress about treating infected patients45 , 46 and overall decreased anxiety.21 Older therapists have most likely had experience with human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/Aids), the severe acute respiratory syndrome outbreak, and Methicillin-resistant Staphylococcus aureus, and could therefore feel more prepared from past encounters and acquired knowledge. Studies have also found that older adults in general worry less than younger adults47 , 48 and worry less than younger adults following other natural disasters and terrorist attacks.49 , 50 Therefore, because the older cohort of therapists may be less worried about in-person delivery than the younger therapists, it may explain a perceived preference for in-person treatment vs telehealth.
Uncertainty for the future was a consistent undertone in many of the free text statements. Relative to this emotion, in a recent psychology review uncertainty was described as the precision with which a prediction can be made based on the available information.51 Specific to uncertainty and the COVID-19 pandemic, a correlational study investigated the role of uncertainty on the psychological wellbeing of individuals. The authors’ findings suggest that the feeling of uncertainty in the current pandemic might provoke fear of COVID-19 via rumination, and consequently have a negative impact on psychological wellbeing.52 Further, a narrative review highlighted the most relevant data which may contribute to developing psychological distress and other mental health symptoms in relation to prior epidemics and the current pandemic. The authors suggest that the disease characteristics of the current COVID-19 pandemic provoked a generalized climate of wariness and uncertainty, particularly among health professionals.53 These findings were attributed to a range of causes such as the rapid spread of COVID-19, the severity of symptoms it can cause in a segment of infected individuals, the lack of knowledge of the disease, and deaths among health professionals.53
Limitations
The survey was not without technical flaws. Shortly after the electronic distribution of the survey it was reported that two questions that permitted a “check all that apply” response did not allow the participants to do so. Therefore, the survey was paused for 12 minutes to allow for remediation of this issue and necessitated the discarding of 158 responses. In addition, 2 questions (43 and 44) had a 0-response rate due to incorrect coding rendering these questions void from inclusion in the analysis or results of the study.
Response bias is a potential consideration in this study due to the conditions or factors that may have impacted a therapist's ability to respond to the survey. Not all ASHT members chose to open the email or respond to the survey, therefore the results may not accurately represent the opinion of all ASHT members.
Although, the number of members agreeing to participate in the survey was good compared to other professional surveys, the length of the survey and the amount of free text responses along with open ended questions may have contributed to survey fatigue.
When designing the survey, we did not define stress. It was our bias that increased stress levels would have a negative implication, but without offering qualifying information related to stress in the survey, the bias that increased stress is negative is an assumption on our part.
Finally, although we received responses from therapists in other countries, we did not receive enough responses to perform any analysis on that data. Thus, we were not able to elaborate on this data.
Conclusion
The hand therapy profession underwent a significant change as a result of the COVID-19 pandemic. Therapists reported a sudden decrease in working hours and in-person treatment, and a sudden shift to telehealth medicine. These sudden changes resulted in increased stress levels regardless of financial security or insecurity, age, practice setting, or geographical setting. Therapists reported uncertainty that ranged from the utilization of new safety precautions to the future of the profession to balancing work with schools and closure of childcare. Results of this survey provide insight into the far-reaching effects this pandemic has had on the hand therapy community. These findings may provide an understanding of the changes, considerations, and adaptations that may be necessary as we continue to move our profession forward.
Future research
Future research regarding the long-term effects of these changes would be of value so that the true impact of the COVID-19 pandemic can be understood, and lessons can be gleaned for the future. Understanding telehealth from the perspective of therapist apprehension and barriers regarding providing telehealth services would be beneficial so that facilities can addresses these concerns and ensure quality telehealth services are provided. Future economic ramifications of the pandemic and the impact on the employment of hand therapy professionals would be beneficial to study especially in relation to employers receiving funding from the Paycheck Protection Program.
Acknowledgments
We would like to acknowledge Brocha Stern for her assistance in developing the survey used in this study.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jht.2021.01.007.
JHT Read for Credit
Quiz: # 897
Record your answers on the Return Answer Form found on the tear-out coupon at the back of this issue or to complete online and use a credit card, go to JHTReadforCredit.com. There is only one best answer for each question.
-
# 1.The survey was sent to
-
a.CHTs in England and the US
-
b.ASHT members
-
c.AOTA and APTA members
-
d.attendees of the 2020 Philadelphia Hand Rehab Conference
-
a.
-
# 2.The survey looked at
-
a.practice patterns
-
b.use of telehealth
-
c.financial impact
-
d.all of the above
-
a.
-
# 3.Concerning therapists’ comfort levels in providing in-person therapy
-
a.therapists working in hospital settings were the most comfortable
-
b.there was no difference in comfort levels between the older therapists and the youngest group
-
c.older, more experienced therapists were more comfortable
-
d.newer CHTs were the most comfortable
-
a.
-
# 4.Telehealth was more commonly practiced by
-
a.older therapists
-
b.younger therapists
-
c.hospital-based therapists
-
d.non-CHTs
-
a.
-
# 5.Those studied reported a significant reduction in caseload, and those who did attend therapy tended to be postop patients
-
a.true
-
b.false
-
a.
When submitting to the HTCC for re-certification, please batch your JHT RFC certificates in groups of 3 or more to get full credit.
Appendix. Supplementary materials
References
- 1.Cascella M, Rajnik M, Cuomo A, Dulebohn S, Features NR. StatPearls [Internet. StatPearls Publishing; Treasure IslandFL: 2020 Jan. Evaluation and treatment coronavirus (COVID-19) [Updated 2020 Mar 20] Available from https://www.ncbi.nlm.nih.gov/books/NBK554776/ [Google Scholar]
- 2.Zhang Z., Liu S., Xiang M., et al. Protecting healthcare personnel from 2019-nCoV infection risks: lessons and suggestions. Front Med. 2020 doi: 10.1007/s11684-020-0765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Novel Coronavirus (2019-nCoV): Situation Report – 22. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. Accessed March 16, 2020.
- 4.World Health Organization. Coronavirus disease 2019 (COVID-19) situation report –51. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. Accessed March 16, 2020.
- 5.J Hand Ther. 2009:361–376. ASHT Scope of Practice; 2011. [Google Scholar]
- 6.Viswanath A., Monga P. Working through the COVID-19 outbreak: rapid review and recommendations for MSK and allied health personnel. J Clin Ortho Trauma. 2020 doi: 10.1016/j.jcot.2020.03.014. ASHT Scope of Practice; 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adams J, Walls R. Supporting the healthcare workforce during the COVID-19 global pandemic. JAMA. 2020;12 doi: 10.1001/jama.2020.3972. Published online March. [DOI] [PubMed] [Google Scholar]
- 8.Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. 2020 doi: 10.1001/jama.2020.5893. Published online. [DOI] [PubMed] [Google Scholar]
- 9.U.S.Department of Labor Bureau of Statistics https://www.dol.gov/coronavirus. Published April 2, 2020. Accessed April 7, 2020.
- 10.Owens C. Special report: Healthcare workers versus coronavirus. April 6, 2020. https://www.axios.com/health-care-worker-coronavirus. Accessed April 7, 2020.
- 11.Jessop ZM, Dobbs TD, Ali SR, et al. Personal protective equipment (PPE) for surgeons during COVID-19 pandemic: a systematic review of availability, usage, and rationing [published online ahead of print, 2020 May 12] Br J Surg. 2020 doi: 10.1002/bjs.11750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lima CKT, Carvalho PMM, Lima IAAS, et al. The emotional impact of Coronavirus 2019-nCoV (new Coronavirus disease) Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet E-surveys (CHERRIES) J Med Internet Res. 2004;6:334. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coronavirus in the U.S. New York Times; 2020. Latest Map and Case Count. May 11 https://www.nytimes.com/interactive/2020/us/coronavirus-us-cases.html Accessed May 11, 2020. [Google Scholar]
- 15.Elflein J. Rates of U.S. Coronavirus (COVID-19) cases as of May 15, 2020. Statista [database online] https://www.statista.com/statistics/1109004/coronavirus-covid19-cases-rate-us-americans-by-state/ Accessed May ??, 2020.
- 16.Krebs C. Memorandum on identification of essential critical infrastructure workers during COVID-19 response. U.S. department of homeland security cybersecurity and infrastructure security agency. Published March 19, 2020. Accessed: May 15, 2020.
- 17.Marik TL, Roll SC. Effectiveness of occupational therapy interventions for musculoskeletal shoulder conditions: a systematic review. Am J Occup Ther. 2017;71 doi: 10.5014/ajot.2017.023127. 7101180020p1-7101180020p11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raman J., MacDermid J.C., Grewal R. Effectiveness of different methods of resistance exercises in lateral epicondylosis–a systematic review. J Hand Ther. 2012;25:5–26. doi: 10.1016/j.jht.2011.09.001. [DOI] [PubMed] [Google Scholar]
- 19.Roll S.C., Hardison M.E. Effectiveness of occupational therapy interventions for adults with musculoskeletal conditions of the forearm, wrist, and hand: a systematic review. Am J Occup Ther. 2017;71 doi: 10.5014/ajot.2017.023234. 7101180010p1-7101180010p12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations [published correction appears in. Gen Psychiatr. 2020;33 doi: 10.1136/gpsych-2020-100213. Apr 27e100213corr1]. Gen Psychiatr. 2020;33(2):e100213. Published 2020 Mar 6. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. Published 2020 Mar 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang J, Lu H, Zeng H, et al. The differential psychological distress of populations affected by the COVID-19 pandemic [published online ahead of print, 2020 Apr 15] Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.04.031. S0889-1591(20)30535-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Taylor S, Landry CA, Paluszek MM, Fergus TA, McKay D, Asmundson GJG. Development and initial validation of the COVID stress scales. J Anxiety Disord. 2020;72 doi: 10.1016/j.janxdis.2020.102232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation [published online ahead of print, 2020 Mar 27] Int J Ment Health Addict. 2020:1–9. doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chew NWS, Lee GKH, Tan BYQ, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak [published online ahead of print, 2020 Apr 21] Brain Behav Immun. 2020:30523–30527. doi: 10.1016/j.bbi.2020.04.049. S0889-1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wu W, Zhang Y, Wang P, et al. Psychological stress of medical staffs during outbreak of COVID-19 and adjustment strategy. [published online ahead of print, 2020 Apr 21] J Med Virol. 2020 doi: 10.1002/jmv.25914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sahu D, Agrawal T, Rathod V, Bagaria V. Impact of COVID 19 lockdown on orthopaedic surgeons in India: a survey [published online ahead of print, 2020 May 12] J Clin Orthop Trauma. 2020 doi: 10.1016/j.jcot.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oliver E. April 10, 2020. 35 States Canceling Elective Procedures. Becker's ASC Review. https://www.beckersasc.com/asc-transactions-and-valuation-issues/35-states-canceling-elective-procedures.html Accessed May ?, 2020. [Google Scholar]
- 29.Grandizio LC, Foster BK, Klena JC. Telemedicine in hand and upper-extremity surgery. J Hand Surg Am. 2020;45:239–242. doi: 10.1016/j.jhsa.2019.09.007. [DOI] [PubMed] [Google Scholar]
- 30.Buvik A, Buffe E, Knutsen G, Smabrekke A, Wilsgaard T. Quality of care for remote orthopaedic consultations using telemedicine: a randomized controlled trial. BMC Health Serv Res. 2016;16:483. doi: 10.1186/s12913-016-1717-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cason J. Telehealth: a rapidly developing service delivery model for occupational therapy. Int J Telerehabil. 2014;6:29–35. doi: 10.5195/ijt.2014.6148. Published 2014 Sept 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Calouro C, Kwong MW, Gutierrez M. An analysis of state telehealth laws and regulations for occupational therapy and physical therapy. Int J Telerehabil. 2014;6:17–23. doi: 10.5195/IJT.2014.6141. Published 2014 Sep 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Teneford A, Hefner J, Kodish-Wachs J, Laccarino M, Paganoni S. Telehealth in physical medicine and rehabilitation: a narrative review. PM R. 2017;9:551–558. doi: 10.1016/j.pmrj.2017.02.013. [DOI] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention May 25, 2020. “Outpatient and ambulatory care settings: responding to community transmission of COVID-19 in the United States”. https://www.cdc.gov/coronavirus/2019-ncov/hcp/ambulatory-care-settings.html.
- 35.Loeb AE, Rao SS, Ficke JR, Morris CD, Riley LH, 3rd, Levin AS. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J Am Acad Orthop Surg. 2020;28:e469–e476. doi: 10.5435/JAAOS-D-20-00380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hofer F., Haluza D. Are Austrian practitioners ready to use medical apps? Results of a validation study. BMC Med Inform Decis Mak. 2019;19:88. doi: 10.1186/s12911-019-0811-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dziechciaż M, Filip R. Biological psychological and social determinants of old age: bio-psycho-social aspects of human aging. Ann Agric Environ Med. 2014;21(4):835–838. doi: 10.5604/12321966.1129943. [DOI] [PubMed] [Google Scholar]
- 38.Grenda TR, Whang S, Evans NRI. Transitioning a surgery practice to telehealth during COVID-19. Ann Surg. 2020 doi: 10.1097/SLA.0000000000004008. Publish Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Goodarzi M, Torabi M, Safdari R, Dargahi H, Naeimi S. Innovation network development model in telemedicine: a change in participation. Healthc Inform Res. 2015;21:265–270. doi: 10.4258/hir.2015.21.4.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hanson D, Calhoun J, Smith D. Changes in provider attitudes toward telemedicine. Telemed J E-Health Off J Am Telemed Assoc. 2009;15:39–43. doi: 10.1089/tmj.2008.0052. [DOI] [PubMed] [Google Scholar]
- 41.Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. 2018;24:4–12. doi: 10.1177/1357633X16674087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19) [published online ahead of print, 2020 Mar 20] J Telemed Telecare. 2020 doi: 10.1177/1357633X20916567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rao SS, Loeb AE, Amin RM, Golladay GJ, Levin AS, Thakkar SC. Establishing telemedicine in an academic total joint arthroplasty practice: needs and opportunities highlighted by the COVID-19 pandemic. Arthroplasty Today. 2020 doi: 10.1016/j.artd.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Polinski JM, Barker T, Gagliano N, Sussman A, Brennan TA, Shrank WH. Patients' satisfaction with and preference for telehealth visits. J Gen Intern Med. 2016;31:269–275. doi: 10.1007/s11606-015-3489-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tan BYQ, Chew NWS, Lee GKH, et al. Psychological Impact of the COVID-19 Pandemic on Health Care Workers in Singapore [published online ahead of print, 2020 Apr 6] Ann Intern Med. 2020:M20–1083. doi: 10.7326/M20-1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li Z, Ge J, Yang M, et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control [published online ahead of print, 2020 Mar 10] Brain Behav Immun. 2020;S0889-1591:30303–30309. doi: 10.1016/j.bbi.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Barber S.J, Kim H. COVID-19 worries and behavior changes in older and younger men and women. J Gerontol. 2020 doi: 10.1093/geronb/gbaa068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Basevitz P, Pushkar D, Chaikelson J, Conway M, Dalton C. Age-related differences in worry and related processes. Int J Aging Hum Dev. 2008;66:283–305. doi: 10.2190/AG.66.4.b. [DOI] [PubMed] [Google Scholar]
- 49.Scott SB, Poulin MJ, Silver RC. A lifespan perspective on terrorism: age differences in trajectories of response to 9/11. Dev Psychol. 2013;49:986–998. doi: 10.1037/a0028916. [DOI] [PubMed] [Google Scholar]
- 50.Shrira A, Palgi Y, Hamama-Raz Y, Goodwin R, Ben-Ezra M. Previous exposure to the World Trade Center terrorist attack and posttraumatic symptoms among older adults following Hurricane Sandy. Psychiatry. 2014;77:374–385. doi: 10.1521/psyc.2014.77.4.374. [DOI] [PubMed] [Google Scholar]
- 51.Hirsh JB, Mar RA, Peterson JB. Psychological entropy: a framework for understanding uncertainty-related anxiety. Psychol Rev. 2012;119:304–320. doi: 10.1037/a0026767. [DOI] [PubMed] [Google Scholar]
- 52.Satici B, Saricali M, Satici SA, Griffiths MD. Intolerance of uncertainty and mental wellbeing: serial mediation by rumination and fear of COVID-19 [published online ahead of print, 2020 May 15] Int J Ment Health Addict. 2020:1–12. doi: 10.1007/s11469-020-00305-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.El-Hage W, Hingray C, Lemogne C, et al. Health profressisonal facing the coronavirus disease 2019 (COVID-19) pandemic: what are the mental health risks? Encephale. 2020 doi: 10.1016/j.encep.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.