Intravascular hemolysis is a serious complication developed in many severe infections such as malaria, sepsis,1 typical hemolytic uremic syndrome2 and congenital diseases such as sickle cell disease.3 Hemolysis is accompanied by thrombocytopenia, platelet activation, plateletleukocyte aggregates, inflammation, vascular obstruction and organ damage. During hemolysis, red blood cell destruction leads to the release of molecules such as ADP, hemoglobin and heme which exert potent prothrombotic and proinflammatory actions.
Under physiological conditions, free heme is scavenged by the plasma protein hemopexin, and is subsequently catabolized by heme oxygenase-1 into carbon monoxide, biliverdin and ferrous iron (Fe2+). However, acute or/and chronic hemolysis exhausts the scavenging system leading to an increase in free heme in the blood. Upon release, reduced heme is rapidly and spontaneously oxidized in the blood into ferric (Fe3+) form, hemin, with increased levels observed in hemolytic diseases. It was recently shown that hemin induces human platelet activation and platelet death through ferroptosis, an intracellular iron-mediated cell death.4 However, the mechanisms and receptors involved in platelet activation by hemin are not known.
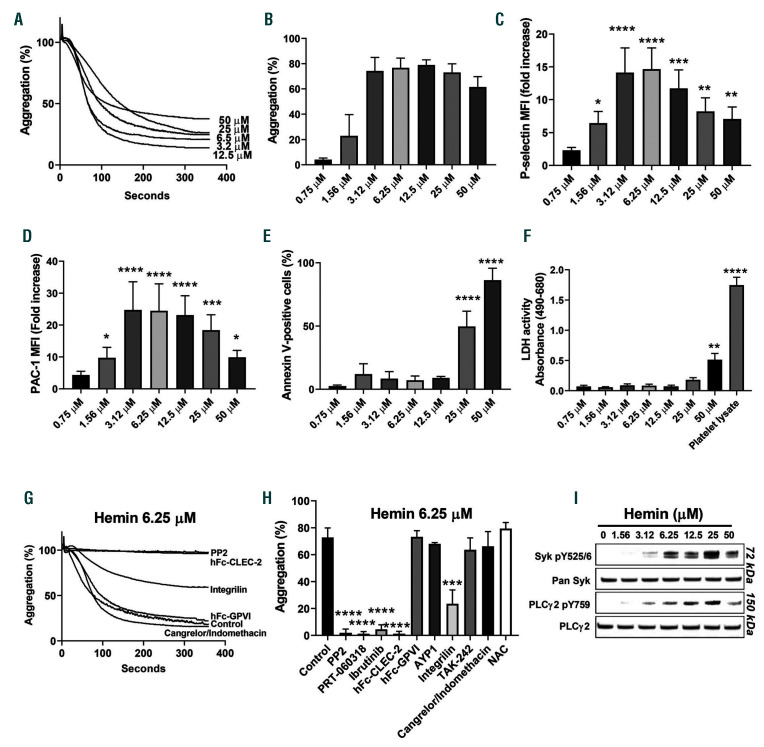
In this study, we investigated hemin-mediated human and mouse platelet activation in vitro. An increase in labile (i.e., weakly bound and free) heme/hemin is detected in patients with hemolytic diseases with plasma concentrations ranging between 2 μM and 50 μM.5,6 Similar concentrations of heme are detected in mice with chronic or acute hemolysis such as sickle cell mice or Escherichia coli-induced hemolysis.1,7 In this study, we show that hemin (2-12 μM) induces rapid aggregation of human washed platelets, while aggregation is slower and reduced in magnitude at higher (≥ 25 μM) concentrations (Figure 1A, B). Platelet aggregation was associated with increased P-selectin expression and GPIIbIIIa activation as measured by flow cytometry (Figure 1C, D). High (≥25 μM) but not lower concentrations of hemin significantly increased phosphatidylserine (PS) exposure on platelets as assessed using Annexin V staining (Figure 1E). Moreover, high concentrations of hemin induced toxicity as measured by increased levels of lactate dehydrogenase (LDH) in the supernatant of activated platelets (Figure 1F). Recent data have shown that a high concentration of hemin (25 μM) triggers lipid peroxidation and human platelet death through ferroptosis but not apoptosis or necroptosis.4 Whether the increase in PS exposure modulates the contribution of platelets to the coagulopathies observed in hemolytic diseases requires further investigation.
Hemin is known to bind to Toll-like receptor (TLR) TLR4 on endothelial cells resulting in endothelial cell activation including secretion of Weibel-Palade bodies.3 However, blocking TLR4 signaling in platelets using TAK-242 did not alter activation by hemin, suggesting a TLR-4-independent pathway of activation (Figure 1H). At low concentrations, human platelet aggregation by hemin was blocked by inhibitors of Syk (PRT-060318), Src family kinases (PP2) and Btk (Ibrutinib), and partially by GPIIbIIIa inhibitor eptifibatide (Integrilin) (Figure 1G, H). These results suggest that hemin induces human platelet activation via an immunoreceptor-tyrosine-based activation-motif (ITAM) receptor-based pathway.8 Indeed, low concentrations of hemin provoked phosphorylation of Syk and PLCγ2 (Figure 1I). In order to identify the receptor triggering platelet activation by hemin, we used recombinant dimeric forms of C-type-lectin-like receptor-2 (CLEC-2) and collagen receptor glycoprotein VI (GPVI) (hFc-CLEC-2 and hFc-GPVI, respectively) as a blocking strategy. Pre-incubation of hemin with hFc- CLEC-2 but not hFc-GPVI abolished platelet aggregation by hemin identifying CLEC-2 as the receptor mediating human platelet activation by hemin (Figure 1G, H). These results also suggest a direct interaction between hemin and CLEC-2. However, while we believe that the inhibition is likely the result of competition between recombinant and platelet CLEC-2, we cannot rule out that recombinant CLEC-2-hemin complex may interfere with CLEC-2 clustering thereby inhibiting platelet activation. Platelet aggregation was not altered by AYP1, 9, an antibody that blocks the interaction between CLEC-2 and podoplanin, providing indirect evidence that hemin binds to a distinct site on CLEC-2 to podoplanin (Figure 1H). Protoporphyrin IX, the precursor of heme, and cobalt hematoporphyrin were shown to bind to CLEC-2 and inhibit podoplanin-CLEC-2 interaction without inducing platelet activation.10 The type of interactions by which different porphyrins selectively bind to CLEC-2 and induce platelet activation requires further investigation. Platelet aggregation mediated by low concentrations of hemin (6.25 μM) was not altered by cyclooxygenase (COX) (indomethacin) or P2Y12 (cangrelor) inhibitors, showing that, in contrast to podoplanin, secondary mediators are not required for hemin-mediated platelet activation (Figure 1G, H). This may reflect the ability of hemin to induce higher oligomers of CLEC-2 increasing signal transduction. Platelet aggregation does not depend on oxidative stress as hemin-mediated platelet aggregation was not altered by the antioxidant N-acetyl cysteine (NAC) (Figure 1H; Online Supplementary Figure S1). At higher concentrations (>25 μM), platelet aggregation was not inhibited by integrilin or inhibitors of Src, Syk and Btk, suggesting that higher concentrations of hemin induce agglutination (Online Supplementary Figure S2). Increasing the concentrations of inhibitors did not alter platelet agglutination/aggregation (not shown). The distinct mechanisms of platelet activation by low and high concentrations of hemin might be related to formation of hemin aggregates at high concentrations, which might exert different activities as compared to monomeric or dimeric hemin present at low concentrations.
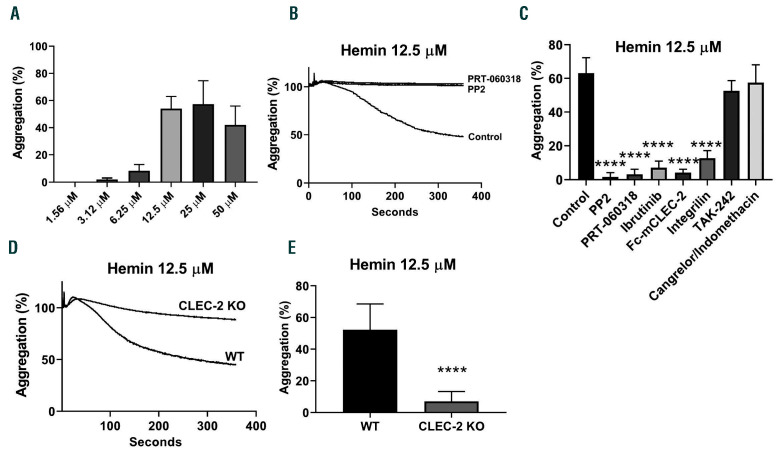
Hemin induces mouse platelet aggregation, albeit at a slightly higher concentration (Figure 2A). Similar to human platelets, aggregation by low concentrations of hemin was inhibited by inhibitors of Src, Syk and Btk tyrosine kinases, recombinant mouse Fc-mCLEC-2 and GPIIbIIIa blockade (Figure 2B, C). In contrast, inhibitors of TLR4, COX and P2Y12 had no effect on platelet aggregation by hemin (Figure 2C). Platelet aggregation by hemin was significantly reduced in CLEC-2-deficient platelets confirming a key role for CLEC-2 (Figure 2D, E). However, deletion of CLEC-2 did not inhibit platelet shape change suggesting that one or more other receptors support platelet activation by hemin in mice.
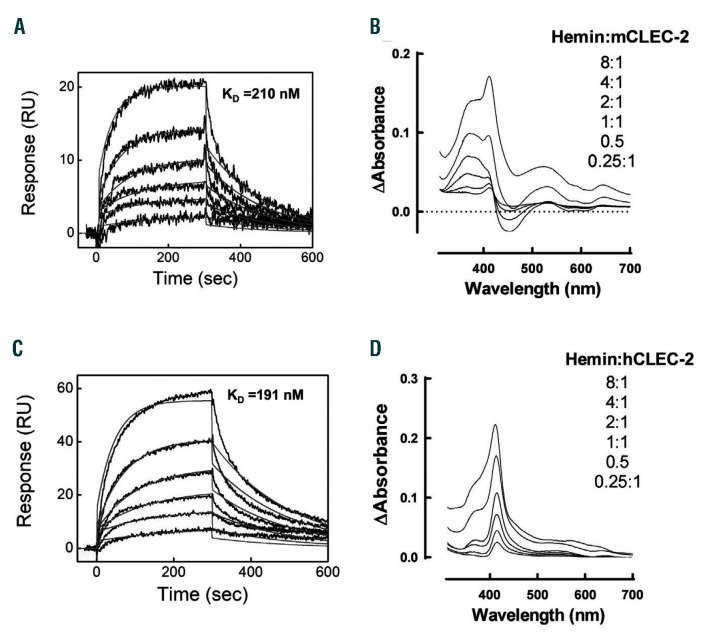
The fact that recombinant CLEC-2 inhibits heminmediated platelet aggregation suggests a direct interaction between hemin and CLEC-2. Using surface plasmon resonance-based technique, we demonstrated that hemin binds to both murine and human recombinant CLEC-2 with KD values of ~200 nM in both cases (Figure 3A, C). Hemin binding to mouse CLEC-2 was characterized by kinetic rate association (ka) and dissociation (kd) constants of ka=2.77±0.08×104 mol-1 s-1 and 5.76±0.09×10-3 s-1. Similar values of kinetic rate constants were determined for hemin binding to human CLEC-2, ka=2.65±0.09×104 mol-1 s-1 and kd=5.06±0.05×10-3 s-1. The interaction of hemin with human and mouse CLEC-2 was further confirmed by UV-vis absorbance spectroscopy (Figure 3B, D). The differential absorbance spectra profiles revealed significant shifts of the spectra of hemin towards higher wavelength by human and mouse CLEC-2 demonstrating a direct binding. The differences in the spectral changes of hemin in the presence of human and mouse CLEC-2 can be explained by distinct residues coordinating heme’s iron. The blue shift in the Soret region observed with mCLEC-2 suggests the involvement of sulfur containing amino acid (cysteine)11 whereas the red shift observed with human CLEC-2 suggests histidine coordination.
Altogether, these results show that hemin is an endogenous agonist for CLEC-2 leading to platelet activation through activation of integrin GPIIbIIIa at low concentrations and agglutination at high concentrations. Recombinant CLEC-2 inhibits platelet activation by both mechanisms suggesting that this may represent a novel form of therapeutic intervention to inhibit platelet activation in hemolytic disease.
Figure 1.
Hemin mediates human platelet activation through C-type-lectin-like receptor-2. (A, B) Human washed platelets (2x108/mL) were incubated with increasing concentrations of hemin in the presence of Ca2+ (2 mM). Platelet aggregation was assessed for 6 minutes (min) using light transmission aggregometry (n=5). (C, D) For flow cytometry analysis, 1x106 platelets were incubated with different concentrations of hemin for 20 min at 37oC. Platelet activation was determined by flow cytometry using (C) anti-P-selectin and (D) GPIIbIIIa PAC-1 antibodies (n=4). Data is shown as fold increase of median of fluorescence (MFI) of treated platelets over control (absence of hemin). (E) Phosphatidylserine exposure was assessed using Annexin V staining. (F) Lactate dehydrogenase (LDH) levels were measured in the supernatant following platelet aggregation (6 min). Platelet lysate was used to detect the total level of LDH in platelets. (G, H) Platelet aggregation by hemin was assessed using Btk inhibitor Ibrutinib (500 nM), Src family kinase inhibitor PP2 (20 μM), Syk inhibitor PRT-060318 (20 μM), TLR4 inhibitor TAK-242 (10 μM), P2Y12 inhibitor Cangrelor (10 μM) or cyclooxygenase inhibitor indomethacin (10 μM). Platelets were pre-incubated with different inhibitors for 5 min at 37 oC prior to the addition of hemin. Dimeric C-type-lectin-like receptor-2 (CLEC-2) (hFc-CLEC-2, 20 mg/mL) or dimeric collagen receptor glycoprotein VI (GPVI) (hFc-GPVI, 20 mg/mL) were pre-incubated with hemin for 20 min at 37 oC prior to addition to platelets (n=5). (H) Histogram data are shown as mean ± standard deviation. (I) Protein levels of the phosphorylation of Syk and PLCγ2, and total Syk and PLCγ2 in platelet lysates were determined by western blotting after 6 min aggregation. Western blots are representative of five independent experiments. The statistical significance was analyzed using a one-way ANOVA with Tukey’s multiple comparisons test using Prism 8 (GraphPad Software Inc, USA). Significance is shown compared to control (absence of hemin), *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001.
Figure 2.
Hemin induces mouse platelet aggregation. (A) Mouse washed platelets (2x108/mL) were incubated with increasing concentrations of hemin in the presence of Ca2+ (2 mM). Platelet aggregation was assessed using light transmission aggregometry. (B, C) Hemin-mediated platelet aggregation (12.5 μM hemin) was assessed in the presence of Ibrutinib (2 μM), PP2 (20 μM), PRT-060318 (20 μM), TAK-242 (10 μM), Cangrelor (10 μM), recombinant mouse C-typelectin- like receptor-2 (CLEC-2) (Fc-mCLEC-2, 10 μg/mL) (n=4). (D, E) Washed platelets from wild-type (WT) or Clec-2 deficient (Clec-1bfl/fl PF4cre, Clec-2 KO) were incubated with hemin (12.5 μM) in the presence of Ca2+ (2 mM) (n=5). (E) Histogram data are shown as mean ± standard deviation. The statistical significance was analyzed using a one-way ANOVA with Tukey’s multiple comparisons test using Prism 8. Significance is shown compared to control ****P<0.0001.
Figure 3.
Hemin binds to mouse and human recombinant C-typelectin- like receptor-2. (A, C) For surface plasma resonance, realtime interaction profiles were obtained after injection of increasing concentrations of hemin (19.5–625 nM) over recombinant mouse (A) and human (C) C-type-lectin-like receptor-2 (CLEC-2) immobilized on CM5 sensor chip. The association and dissociation phases were followed for 5 minutes, each. The black lines show the experimental data, the grey lines depict the fit obtained using Langmuir global analyses model. (B, D) For UV-vis absorbance spectroscopy, differential spectra were generated after titration of (B) mouse or (D) human dimeric CLEC-2 (2 μM) with increasing concentrations of hemin (0.5–16 μM). The differential spectra were obtained after subtraction of the spectra of hemin at a given concentration from the spectra of the same concentration of hemin in the presence of the protein. The measurements were done at 25°C in optical cell with 10 mm light path.
Ethical approval for collecting blood from healthy volunteers was granted by Birmingham University Internal Ethical Review (ERN_11-0175). Mice experiments were performed in accordance with UK laws (Animal [Scientific Procedures] Act 1986) with approval of the local ethical committee and UK Home Office approval (PPL P0e98D513).
Human and mouse washed platelets were prepared as previously described.12,13 Platelet aggregation was assessed using light transmission aggregometry for 6 minutes (ChronoLog, Havertown, PA, USA). Fresh synthetic hemin solution was freshly prepared (Frontiers Scientific, USA) for each experiment. PP2 (Tocris/Biotechne Ltd), PRT-060318 (Caltag medsystems), indomethacin (Sigma-Aldrich), cangrelor (The Medicines Company), Ibrutinib (Stratech Scientific), NAcetyl- L-cysteine (Sigma-Aldrich) and TAK-242 (Sigma- Aldrich) were preincubated for 5 minutes (min) at 37ºC with platelets prior to addition of hemin. Human (h) and mouse (m) CLEC-2 and GPVI were produced as Fc fusion proteins (hFc-CLEC-2, hFc-GPVI, Fc-mCLEC-2) in human embryonic kidney HEK293 cells and purified using chromatography affinity. Recombinant human and mouse CLEC-2 were preincubated with hemin for 15 min at 37ºC before addition to platelets. Following aggregation, platelets were centrifuged at 1,000g for 10 min and LDH was measured in the supernatant using CyQUANT™ LDH Cytotoxicity Assay (ThermoFisher Scientific). Clec- 2 deficient mice (Clec-1bfl/fl PF4cre) and littermate controls were previously described.14
Platelet activation (106 platelets) by different concentrations of hemin (20 min at 37ºC) was assessed by flow cytometry with antibodies against CD62P (PE/Cy5 antihuman CD62P antibody, biolegend) and activated GPIIbIIIa (Alexa Fluor® 647 anti-human CD41/CD61 antibody PAC1, Biolegend) using BD Accuri C6 Plus flow cytometer (BD Bioscience). For western blotting, Phospho-Syk (Tyr525/526) (C87C1) Rabbit mAb (#2710), Phospho-PLCγ2 (Tyr759) antibody (#3874), Syk antibody (#2712) and PLCγ2 antibody (#3872) were used (Cell signalling). Protein phosphorylation was assessed after 6 min of aggregation as previously described.12
The binding of human and mouse dimeric CLEC-2 to hemin was performed at 25°C and assessed using surface plasma resonance and UV-spectroscopy methods.15
Supplementary Material
Acknowledgments
The authors would like to thank Dr B. Grygielska for genotyping of mice.
Funding Statement
Funding: this work was supported by a BHF Accelerator Award (AA/18/2/34218), BHF programme grant (RG/13/18/30563), Wellcome Trust 4 year studentship (204951), Wellcome Trust Joint Investigator Award (204951/Z/16/Z) and the Centre of Membrane Proteins and Receptors. JDD hold an H2020 ERC starting grant (CoBABATI 678905). SPW holds a BHF Chair (CH/03/003).
References
- 1.Martins R, Maier J, Gorki AD, et al. Heme drives hemolysis-induced susceptibility to infection via disruption of phagocyte functions. Nat Immunol. 2016;17(12):1361-1372. [DOI] [PubMed] [Google Scholar]
- 2.Frimat M, Tabarin F, Dimitrov JD, et al. Complement activation by heme as a secondary hit for atypical hemolytic uremic syndrome. Blood. 2013; 122(2):282-292. [DOI] [PubMed] [Google Scholar]
- 3.Belcher JD, Chen C, Nguyen J, et al. Heme triggers TLR4 signaling leading to endothelial cell activation and vaso-occlusion in murine sickle cell disease. Blood. 2014;123(3):377-390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.NaveenKumar SK, SharathBabu BN, Hemshekhar M, Kemparaju K, Girish KS, Mugesh G. The Role of Reactive Oxygen Species and Ferroptosis in Heme-Mediated Activation of Human Platelets. ACS Chem Biol. 2018;13(8):1996-2002. [DOI] [PubMed] [Google Scholar]
- 5.Muller-Eberhard U, Javid J, Liem HH, Hanstein A, Hanna M. Plasma concentrations of hemopexin, haptoglobin and heme in patients with various hemolytic diseases. Blood. 1968;32(5):811-815. [PubMed] [Google Scholar]
- 6.Gouveia Z, Carlos AR, Yuan X, et al. Characterization of plasma labile heme in hemolytic conditions. FEBS J. 2017;284(19):3278-3301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Belcher JD, Chen C, Nguyen J, et al. Haptoglobin and hemopexin inhibit vaso-occlusion and inflammation in murine sickle cell disease: Role of heme oxygenase-1 induction. PLoS One. 2018; 13(4):e0196455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rayes J, Watson SP, Nieswandt B. Functional significance of the platelet immune receptors GPVI and CLEC-2. J Clin Invest. 2019;129(1):12-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gitz E, Pollitt AY, Gitz-Francois JJ, et al. CLEC-2 expression is maintained on activated platelets and on platelet microparticles. Blood. 2014; 124(14):2262-2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tsukiji N, Osada M, Sasaki T, et al. Cobalt hematoporphyrin inhibits CLEC-2-podoplanin interaction, tumor metastasis, and arterial/venous thrombosis in mice. Blood Adv. 2018;2(17):2214-2225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kuhl T, Wissbrock A, Goradia N, et al. Analysis of Fe(III) heme binding to cysteine-containing heme-regulatory motifs in proteins. ACS Chem Biol. 2013;8(8):1785-1793. [DOI] [PubMed] [Google Scholar]
- 12.Nicolson PLR, Hughes CE, Watson S, et al. Inhibition of Btk by Btk-specific concentrations of ibrutinib and acalabrutinib delays but does not block platelet aggregation mediated by glycoprotein VI. Haematologica. 2018;103(12):2097-2108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hughes CE, Pollitt AY, Mori J, et al. CLEC-2 activates Syk through dimerization. Blood. 2010;115(14):2947-2955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Finney BA, Schweighoffer E, Navarro-Nunez L, et al. CLEC-2 and Syk in the megakaryocytic/platelet lineage are essential for development. Blood. 2012;119(7):1747-1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wiatr M, Merle NS, Boudhabhay I, et al. Anti-inflammatory activity of intravenous immunoglobulin through scavenging of heme. Mol Immunol. 2019;111:205-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.