ABSTRACT
We recently described a protein O-glycosylation pathway conserved in all species of the Burkholderia genus that results in the synthesis and incorporation of a trisaccharide glycan to membrane-exported proteins. Here, we exploited this system to construct and evaluate a diagnostic tool for glanders. Burkholderia mallei, the causative agent of glanders, is a highly infectious and fatal zoonotic pathogen that infects horses, mules, donkeys, and occasionally humans. A highly sensitive and specific diagnostic tool is crucial for the control, elimination, and eradication of B. mallei infections. We constructed plasmids carrying synthetic genes encoding a modified, previously unannotated Burkholderia glycoprotein containing three glycosylation sequons fused to the cholera toxin B-subunit. The resulting proteins were glycosylated in the B. cenocepacia K56-2 parental strain, but not in glycosylation-deficient mutants, as determined by SDS-PAGE and fluorescent lectin blots. One of these glycoproteins was used as an antigen in ELISA and western blots to screen a panel of serum samples collected from glanders-infected and healthy horses, which were previously investigated by complement fixation test and indirect ELISA based on a semi-purified fraction of B. mallei. We show that ELISA and western blot assays based on our glycoprotein antigen provide 100% specificity, with a sensitivity greater than 88%. The glycoprotein antigen was recognized by serum samples collected from patients infected with B. pseudomallei, B. mallei, B. multivorans, and B. cenocepacia. Our results indicate that protein O-glycosylation in Burkholderia can be exploited as a biomarker for diagnosis of Burkholderia-associated infections.
KEYWORDS: Burkholderia mallei, protein glycosylation, category B agents, complement fixation, peanut agglutinin, horse infections
Introduction
Glanders is a severe zoonotic disease caused by the Gram-negative bacterium Burkholderia mallei. Horse, mules, and donkeys are natural hosts, while transmission from animals to humans has occurred in people who are working closely with infected animals [1]. The signs and symptoms of infection can be either acute or chronic. Acute infections occur frequently in donkeys and mules; they are usually fatal without treatment, showing signs of septicemia, high fever, weight loss, and compromise of the respiratory system. However, glanders generally manifest with a more chronic course in horses [2]. Although the disease has been successfully eradicated in North America, Australia, and Europe, there are reports of glanders in Asia, the Middle East, and South America, and hence it is considered as a reemerging disease [3–7]. Also, B. mallei is considered a category B biothreat agent [8].
Due to insufficient pathognomonic symptoms, especially in the early stages of glanders, diagnosis can be difficult. Direct isolation and molecular identification of B. mallei from infected tissues, cutaneous lesions, and nasal exudates is the most accurate way to confirm the infection. However, this is generally limited by poor sensitivity due to low bacteria load, as subclinical and latent infections are commonly manifested in horses [2]. Mallein and serological tests are frequently used for diagnosis of glanders in endemic areas [9]. The mallein test is a hypersensitive skin test based on a water-soluble protein extracted from the microorganism, but it is not recommended by the World Organization for Animal Health (OIE) due to animal welfare concerns since the mallein antigen needs to be injected into the horse (http://www.oie.int/fileadmin/Home/eng/Health_standards/tahm/3.05.11_GLANDERS.pdf.). Complement fixation test (CFT) is the most accurate and reliable serological test prescribed by the OIE for international trade of equines. Although this test is believed to have a high specificity, a considerable number of false-positive results were observed when different antigens and assay protocols were applied [10,11]; complexity, anti-complementary reactions and poor standardization are other shortcomings of the CFT [12]. The Rose Bengal plate agglutination test is a rapid agglutination assay using a heat-inactivated bacterial suspension colored with Rose Bengal; it is fast and simple but requires antigens purified from B. mallei cultures [9,13].
Recently, several purified protein antigens of B. mallei have been tested in ELISA and western blot showing promising results for diagnosis of glanders. A western blot technique based on a partially purified lipopolysaccharide-containing antigen shows higher specificity compared to CFT [14]. Moreover, indirect ELISAs based on the intracellular motility A protein (BimA) [15,16], the type 6 secreted TssB [17] and Hcp1 [18] proteins, the heat shock protein GroEL [19] and a semi-purified fraction of B. mallei have been developed [11]. However, these methods require more investigation using large-scale sample surveys and optimization to improve specificity and sensitivity [18]. Previous work has identified an O-glycosylation (ogc) gene cluster in B. cenocepacia encoding enzymes for the synthesis of a lipid-linked trisaccharide, which consists of a β-Gal-(1,3)-α-GalNAc-(1,3)-β-GalNAc [20] and is incorporated in membrane-exported Burkholderia proteins by the PglL O-glycosyltransferase (O-Tase) [21]. We also found this pathway is conserved in all members of the Burkholderia genus including B. mallei [20]. More imporantly, we detected glycan-specific antibodies in sera from patients infected with various types of Burkholderia infections including glanders, indicating that natural infection elicits a humoral response against the Burkholderia-specific glycan [20]. In this study, we describe the construction of a glycoengineered antigen that can be exploited as a highly specific diagnostic tool for glanders, and potentially other Burkholderia related infections.
Materials and methods
Bacteria strains and growth conditions
Escherichia coli K-12 strain DH5α was used for cloning experiments to construct the appropriate plasmids. B. cenocepacia K56-2 and the glycosylation-deficient mutants ΔpglL and Δogc [20] were used to produce glycosylated and unglycosylated proteins, respectively. Bacterial strains were grown at 37°C in Luria–Bertani (LB) medium supplemented with appropriate antibiotics. For B. cenocepacia K56-2 and mutants carrying the plasmid pDA12, bacteria were grown with 100 μg ml−1 tetracycline. E. coli DH5α carrying the plasmid pDA12 was grown with 30 μg ml−1 tetracycline. E. coli DH5α carrying the plasmid pRK2013 was grown with 40 μg ml−1 kanamycin.
Plasmid constructions
To obtain high-level expression of recombinant proteins in B. cenocepacia we used the constitutive expression vector pDA12 [22]. The chimeric genes encoding the respective variations of recombinant proteins, BCAL2737a, CtxB-BCAL2737a, BCAL2737a-CtxB were synthesized (Eurofins Genomics) and gene fragments subcloned into pDA12 to generate recombinant plasmids pDA12-BCAL2737a, pDA12-BCAL2737a-CtxB, pDA12-CtxB-BCAL2737a. Positive clones were screened by colony PCR using primer sets: 5ʹ- ACTCTCGCATGGGGAGACCC-3ʹ and 5ʹ-TTTGATGTTATGGAGCAGCAACGAT-3ʹ. The Go Taq® DNA polymerase (Promega, UK) was used for PCR amplification, conditions were 4 min at 95°C, 34 cycles of 95°C for 30 s, 58°C for 40 s, and 72°C for 3 min, and a final extension of 7 min at 72°C.
The resulting recombinant plasmids were mobilized from E. coli DH5α into B. cenocepacia K56-2 and the isogenic mutants ΔpglL and Δogc by triparental mating using E. coli DH5α carrying the helper plasmid pRK2013 [23]. Exconjugants were plated on LB agar plates with 50 μg ml−1 gentamicin, 200 μg ml−1 ampicillin, and 120 μg ml−1 tetracyclineand confirmed by colony PCR, as described above.
Expression and purification of recombinant proteins
For protein expression, bacteria were grown in 1 L of LB medium with 100 μg ml−1 tetracycline overnight at 37°C. For purification, cells were centrifuged for 20 min at 3,220 × g followed by two washes with PBS at 4°C. The pellet was resuspended in 20 ml Tris-HCl buffer (100 mM, pH 8.0). DNAse (5 mg ml −1), lysozyme (1 mg ml −1), protease inhibitors (1 tablet, Roche) were added, and the mixture was incubated for 15 min. Cells were lysed using a cell disrupter (Constant systems Ltd., Northants, UK) with two cycles of 30 kPsi. The lysed cells were centrifuged for 20 min at 17,696 × g at 4°C and the resulting supernatant was immediately filtered through a 0.2-μm membrane (Fisher Scientific, UK). The filtrate was applied to a protein purification system (ÄKTA, GE Healthcare Life Sciences), which was equipped with a His-trap column. Proteins were eluted using a linear gradient of up to 100% elution buffer (100 mM Tris-HCl [pH 8.0], 500 mM NaCl, 500 mM Imidazole, glycerol 2%). The collected fractions were analyzed by 12% SDS-PAGE gels and western blot.
Western blot analysis of protein glycosylation and equine serum samples
The presence of the trisaccharide glycan in purified proteins was analyzed by western blot using biotinylated peanut agglutinin (PNA), a lectin that recognizes the terminal disaccharide of the Burkholderia glycosylation trisaccharide [20,24]. Purified proteins were run on 12% SDS-PAGE gels and then blotted onto nitrocellulose membranes using the BIO-RAD Trans-Blot® Turbo™ Transfer System. Membranes were incubated overnight in casein solution (Sigma-Aldrich) diluted in Tris-buffered saline, 0.1% Tween 20 (TBST). Mouse anti-His antibody (1:12,000) (Sigma-Aldrich) and biotinylated PNA (1:6000) (Vector Laboratories) were applied as primary antibodies. The mouse anti-His antibody was added first and incubated at room temperature for 1 h. Biotinylated PNA was added to this solution followed by incubation for another 30 min. After four washes with TBST, IRDye® 680RD goat anti-mouse antibody (1:12,000) (Li-Cor, Biosciences) and IRDye® 800CW Streptavidin (1:12,000) (Li-Cor, Biosciences) were applied as secondary antibodies. The goat anti-mouse antibody was applied first and incubated at room temperature for 30 min. Streptavidin was added to the solution and further incubated for 20 min. After four washes, as before, the membranes were visualized using the Odyssey Infrared Imaging System (Li-Cor, Biosciences).
To detect antibodies in equine serum samples, an optimized western blot protocol was established. Briefly, the same protocol was used for preparing nitrocellulose membranes with purified proteins. The membranes were cut into regular strips, and each strip was incubated in a final volume of 2 ml of unabsorbed serum sample, diluted 1:1000 in TBST for 1 h at room temperature. After four washes with TBST, the membranes were incubated with biotinylated goat anti-horse IgG antibody (1:12,000) (Abcam, UK). After four more washes, the membranes were stained with IRDye® 800CW Streptavidin for 30 min and visualized in the Odyssey Infrared Imaging System.
ELISA to detect antibodies toward glycan in equine serum samples
An optimized ELISA protocol was established after several trials to determine the optimal antigen concentration and serum dilutions. To reduce background, serum samples were adsorbed with unglycosylated protein by incubating the samples with the unglycosylated CtxB-BCAL2737a at a concentration of 1 μg ml−1 for 2 h at 37°C and overnight at 4°C in a 96-well Nunc MaxiSorp plate. Serum samples were then collected and used for detection by ELISA using the following procedure: 96-well Nunc MaxiSorp plates were coated with 50 μl of purified glycosylated and unglycosylated proteins diluted in coating buffer (carbonate/bicarbonate, 100 mM, pH 9.6) to reach a final concentration of 31 pg ml−1. The plates were covered by plastic adhesive film and incubated at 4°C overnight. Coating solution was removed and plates were washed with 300 μl phosphate buffer saline (PBS) containing 0.05% Tween 20 (PBST). Additional blocking was achieved by adding 300 μl of blocking buffer (BSA 5% in PBS). Plates were covered and incubated at room temperature for 1 h and washed 3 times with PBST. Fifty μl of each serum sample, diluted in half-strength blocking buffer, was added to the wells and incubated for 90 min at room temperature. Biotinylated PNA and PBST were used as positive and negative controls. Plates were washed 4 times with PBST. Fifty μl of biotinylated rabbit anti-horse IgG secondary antibody (Abcam, UK) diluted to 1:5000 was added and incubated for 1 h at room temperature. Plates were washed 5 times with PBST. Fifty μl of Streptavidin-Horseradish Peroxidase diluted 1:200 in PBS was added to each well and incubated for 1 h in the dark at room temperature. After washing 4 times with PBST, 50 μl of the substrate solution 3,3ʹ,5,5ʹ-tetramethylbenzidine was added per well and incubated in the dark at room temperature for 10 min. After enough color development, 30 μl of stop solution (2 N H2SO4) was added and the absorbance of each well was read with POLARstar Omega microplate reader (BMG LABTECH, Ortenberg, Germany) at 450 nm.
Horse and human serum samples
Thirty-two serum samples from horses naturally and experimentally infected with B. mallei, and healthy controls were used for analysis. Positive samples were characterized by the complement fixation test (CFT). An indirect ELISA based on a semi-purified fraction of B. mallei described previously [18] was carried out for comparison. The CFT was performed according to the OIE manual. The indirect ELISA was performed according to the manufacturer’s instructions (IDvet, Grabels, France). Optical density (OD) was read at 450 nm and results were expressed according to the manufacturer’s instructions as follows: S/P = (OD_Sample-OD_Negative control)/(OD_Positive control-OD_Negative control) x 100. S/P values over 40% were considered positive.
Nine serum samples from Burkholderia-infected patients that were previously reported to interact with O-glycan [20] were selected for western blot analysis performed as described above. Among these samples, two are from B. multivorans-infected patients, three samples are from B. cenocepacia-infected patients, one sample is from a B. mallei-infected patient, and three samples are from B. pseudomallei-infected patients.
Proteomic analysis
Gel separated CtxB-BCAL2737a samples were excised and destained in destaining solution (100 mM NH4HCO3, 50% ethanol (EtOH), pH 8.0) for 20 min at room temperature with shaking (750 rpm). Destained gel samples were then washed with 100% EtOH for 10 min at room temperature and dried by vacuum centrifugation for 20 min. Dried gel samples were rehydrated with 10 mM dithiothreitol in 100 mM NH4HCO3 and disulfide reduction carried out for 60 min at 56°C with shaking. The reducing buffer was removed, and the gel samples were washed twice in 100% EtOH for 10 min to remove residual dithiothreitol. Samples were alkylated with 55 mM iodoacetamide in 50 mM NH4HCO3 in the dark for 45 min at room temperature. Alkylated samples were washed with 100 mM of NH4HCO3 for 10 min at room temperature with shaking and then dehydrated with 100% EtOH before being vacuum centrifugation for 20 min. Dried reduced/alkylated samples were then rehydrated with 20 ng/µl trypsin in 100 mM NH4HCO3 (Promega, Madison WI) on ice for 1 h. Excess trypsin solution was removed, gel pieces covered in 40 mM NH4HCO3 and then incubated overnight at 37°C. The supernatant, containing peptides of interest, was concentrated and desalted using C18 stage tips [25,26] before analysis by liquid chromatography-mass spectrometry.
Desalted tryptic peptides were resuspended in Buffer A* (0.1% trifluoroacetic acid, 2% Acetonitrile) and separated using a two-column chromatography set up composed of a PepMap100C18 20 mm × 75 μm trap and a PepMap C18 500 mm × 75 μm analytical columns (Thermo Scientific, San Jose CA). Samples were concentrated onto the trap column at 5 μl min−1 for 5 min with buffer A (0.1% formic acid, 2% acetonitrile) and infused into an LTQ-Orbitrap Elite (Thermo Scientific, San Jose CA) at 300 nl min−1 via the analytical column using a Dionex Ultimate 3000UPLC (Thermo Scientific). A 90-min gradient was run from 2% Buffer B (0.1% formic acid, 80% acetonitrile) to 32% B over 51 min, then from 32% B to 40% B in the next 5 min, then increased to 100% B over 2 min period, held at 100% B for 2.5 min, and then dropped to 0% B for another 20 min. The LTQ-Orbitrap Elite was operated in a data-dependent mode automatically switching between mass spectrometry (MS), collision-induced dissociation (CID), electron transfer dissociation (ETD), and higher energy collision-induced dissociation (HCD) MS-MS.
Identification of glycopeptides in CtxB-BCAL2737a was accomplished using MaxQuant (v1.5.3.30) [27]. Searches were performed against the predicted amino acid sequence of CtxB-BCAL2737a with carbamidomethylated cysteine set as a fixed modification. Searches were performed with trypsin allowing two missed cleavage events and the variable modifications of oxidation of methionine, the Burkholderia glycans (Glycan 1; 568.211 Da elemental composition: C22H36O15N2 and Glycan 2; 668.227 Da elemental composition C26H40O18N2) and acetylation of protein N-termini. The precursor mass tolerance was set to 20 parts-per-million (ppm) for the first search and 10 ppm for main search, with a maximum false discovery rate of 1.0% set for protein and peptide identifications. The resulting outputs were processed within the Perseus (v1.4.0.6) [28] analysis environment to remove reverse matches and common proteins contaminate prior to further analysis. Glycopeptide identified were manually assessed according to the guidelines of Chen et al. [29], annotated manually with the aid of Protein Prospector tool MS-Product (http://prospector.ucsf.edu/prospector/cgi-bin/msform.cgi?form=msproduct). The MS proteomics data were deposited in the ProteomeXchange Consortium via the PRIDE partner repository [30,31] with the dataset identifier PXD018788. Data can be accessed under username: reviewer60750@ebi.ac.uk, password: C7kqIWps.
Analysis of BCAL2737a degradation in Burkholderia strains
As BCAL2737a was not annotated in the reference B. cenocepacia strain J2315 (see Results), we re-analyzed the previously published B. cenocepacia K56-2 peptidome datasets (Pride accession: PXD014614) [32] including BCAL2737a. Searches were performed against the predicted amino acid sequence of BCAL2737a and the K56-2Valvano proteome (NCBI: Taxonomy ID: 985,076) with identical setting as above. The resulting outputs were processed in the Perseus (v1.5.0.9) analysis environment to remove reverse matches and common protein contaminates prior to further analysis. Peptides identified across samples were visualized in heat maps using R (https://www.r-project.org/).
Statistical analysis
Means and standard deviations were calculated using GraphPad Prism 8 software (GraphPad Prism 8; GraphPad Software, USA). Three independent repeats were tested for every sample in ELISA. The cutoff value is calculated based on OD450 nm value of samples tested negative in CFT (excluding inconclusive results). Samples were considered positive when the absorbance reading exceeds the cutoff value computed by two standard deviations above the mean of the negative control. The specificity and sensitivity of the ELISA and western blot tests were determined using the CFT as a standard according to the following formulas:
Inconclusive CFT results were not considered for these calculations.
Results
Identification of a protein–glycan glycoconjugate antigen for antibody detection
In a previous study characterizing the general protein glycosylation system in B. cenocepacia, one of the most abundant and highly glycosylated glycopeptides found, designated A0K9U9, could not be ascribed to any annotated protein in the database of the type strain J2315 [21]. To localize the gene encoding this peptide, its 71-amino acid sequence was used as query in Artemis [33] to search the translations in all frames for B. cenocepacia type strain J2315. This resulted in the identification of a short open reading frame in chromosome 1 (at base pairs 3,008,284–3,008,496) located in the intergenic region between BCAL2737 (encoding a putative pseudouridine synthase) and BCAL2738 (encoding a putative exported protein), which was preceded by a ribosomal binding site sequence (Figure 1); we designated this open reading frame BCAL2737a. The predicted BCAL2737a gene encoded a 71-amino acid polypeptide; it also contained a 21-amino acid signal peptide, predicted by SignalP v.5.0 [34], as expected for a glycosylated protein since glycosylation takes place in the periplasm. The BCAL2737a protein did not show any homology with known proteins in the database. The mature polypeptide contained three serine residues (Figure 1) that become O-glycosylated based on experimental evidence by mass spectrometry [21]. Therefore, the BCAL2737a polypeptide was selected for further analysis since because of its small mass, combined with three glycosylation sites, it could be an appropriate antigen to detect antibodies against Burkholderia O-glycans.
Figure 1.
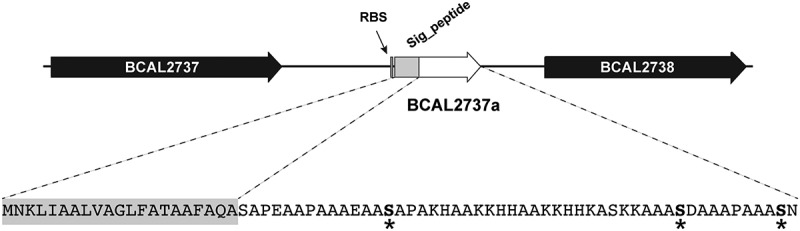
Localization of BCAL2737a in the large chromosome of B. cenocepacia J2315. BCAL2737a, encoding a short polypeptide of unknown function, was identified in the intergenic region between BCAL2737 (encoding a putative pseudouridine synthase) and BCAL2738 (encoding a putative exported protein. The gene is preceded by a Shine-Dalgarno sequence (RBS). The BCAL2737a polypeptide has a signal peptide (Sig_peptide) as predicted by SignalP v.5.0, resulting in a 50-amino acid mature protein; the O-glycosylation sites, experimentally determined by mass spectrometry [21], are indicated by asterisks
Unglycosylated BCAL2737a can be stabilized as a protein fusion with the cholera toxin B subunit (CtxB)
BCAL2737a was expressed as a 10x-His tag C-terminal fusion (Figure 2a) and examined for glycosylation using PNA, and for protein expression using an anti-His monoclonal antibody. This experiment indicated that BCAL2737a can be detected by both methods when expressed in the parental B. cenocepacia K56-2 (Figure 2b). The lectin blots showed also several nonspecific bands attributable to endogenous biotinylated bacterial proteins in the lysate, which were detected by the secondary fluorescent streptavidin (Figure 2c, and asterisks in Figure 2b and D). However, the BCAL2737a was undetectable in both the Δogc and ΔpglL mutants, which lack the biosynthetic cluster for the glycan assembly and the PglL O-Tase, respectively (Figure 2b and D). This was not unexpected since a subset of the Burkholderia glycoproteome is proteolytically degraded [32]. Therefore, as a strategy to stabilize BCAL2737a, we also generated versions of these proteins that were N- and C-terminally fused with the cholera toxin B subunit (CtxB) and contained a C-terminal 10x-His tag (Figure 2a). Both proteins were expressed and glycosylated in K56-2, but only the CtxB-BCAL2737a fusion protein remained stable in the glycosylation-defective mutants (Figure 2b,D). These results suggest that in the absence of glycosylation BCAL2737a can only be stabilized when it is C-terminally fused to CtxB. Therefore, we continued our studies with this fusion protein.
Figure 2.
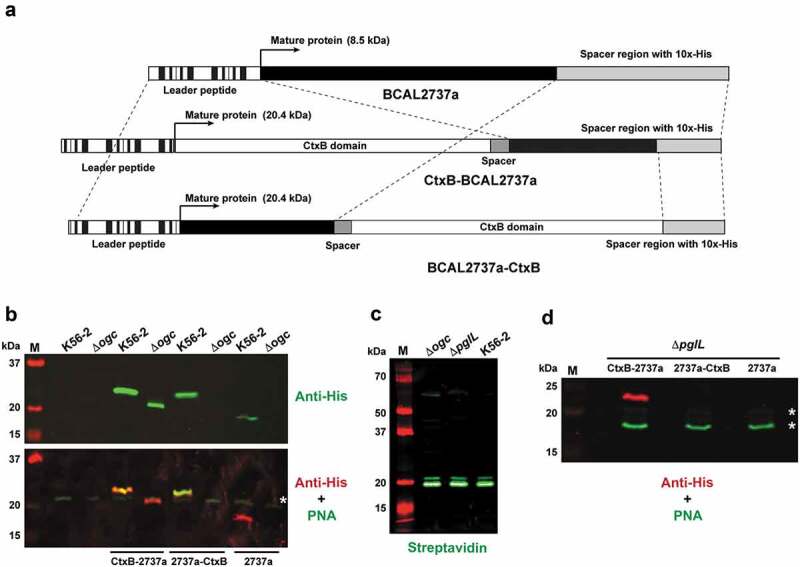
Protein constructs containing BCAL2737a and western blots demonstrating the effects of a lack of glycosylation in Δogc and ΔpglL strains. (a) Map of the CtxB-BCAL2737a, BCAL2737a-CtxB and BCAL2737a recombinant polypeptides indicating their functional domains. Maps are not drawn to scale. (b) Comparison of protein expression and glycosylation in K56-2 and Δogc strains with no plasmid and with plasmids expressing CtxB-BCAL2737a (CtxB-2737a), BCAL2737a-CtxB (2737a-CtxB), and BCAL2737 (2737a). (c) Detection of endogenously biotinylated proteins by direct application of fluorescent streptavidin to the western blot. Lanes M, molecular mass markers, kDa, kilodaltons. (d) Protein expression and glycosylation in ΔpglL using the same plasmids as in panel B. Asterisks in panels B and D, indicate the most abundant nonspecific, endogenously biotinylated proteins
To confirm that CtxB-BCAL2737a is efficiently glycosylated, the protein was purified by Ni2+-affinity chromatography from K56-2 and from ΔpglL as a control. Western blot analysis revealed that purified CtxB-BCAL2737a expressed in ΔpglL exhibited decreased electrophoretic mobility, suggesting it corresponded to an unglycosylated form (Figure 3a), in agreement with the results found with crude lysates (Figure 2b, D). Similarly, only the protein expressed in K56-2 was detected with PNA, indicating the correct trisaccharide glycan residues were present. Glycosylation was also verified by mass spectrometry confirming at least three serine residues within BCAL2737a are glycosylated (Figure 3b, Supplementary Dataset). To further support the degradation of unglycosylated BCAL2737a peptidome datasets from Oppy et al. [32] were reanalyzed against a K56-2 proteome containing the BCAL2737a protein sequence. The new analysis identified multiple peptide breakdown products previously not assigned to known proteins, which were more abundant and intense in the glycosylation null strain ΔpglL compared to K56-2 and the pglL complemented strain (Figure 3c). Together, the results of these experiments demonstrate that CtxB-BCAL2737a is glycosylated at three sites, as the native protein and BCAL2737a is proteolytically degraded in the absence of glycosylation.
Figure 3.
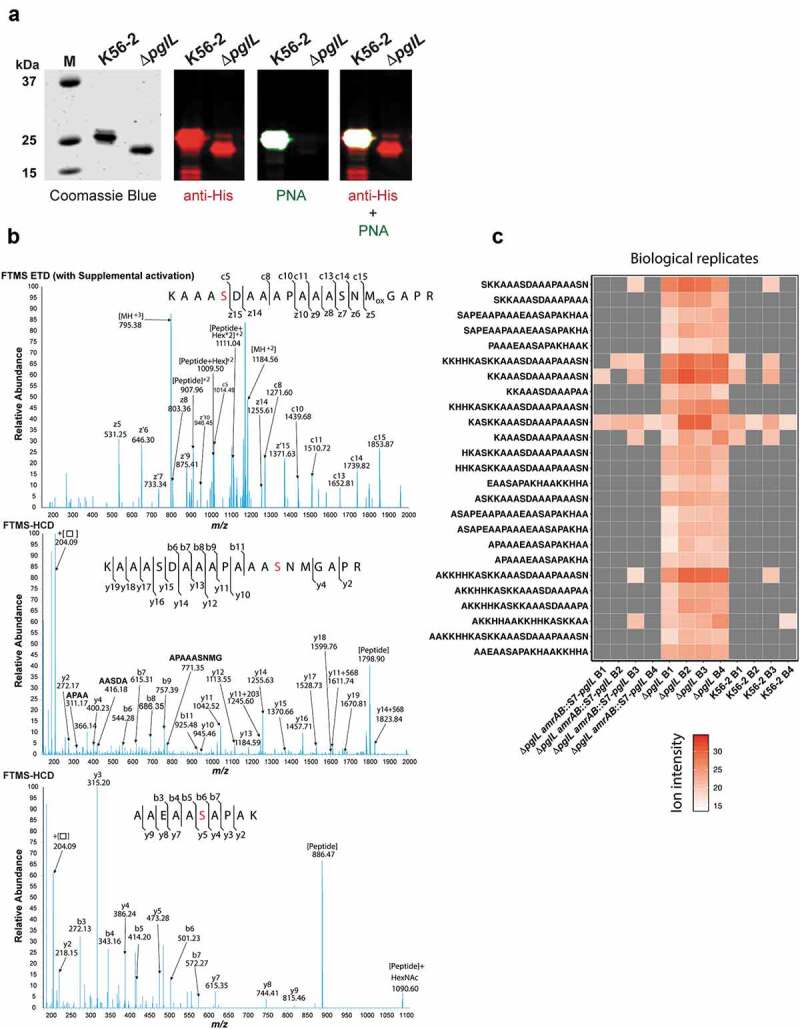
Characterization of purified CtxB-BCAL2737a. (a) CtxB-BCAL2737a was purified from strains K56-2 and ΔpglL by Ni2+-affinity chromatography and analyzed by SDS-PAGE (Coomassie Blue) and by western blot with anti-His and PNA, as indicated. M, molecular mass standards; kDa, kilodaltons. (b) The band corresponding to glycosylated BCAL2737a (purified from strain K56-2) was extracted from the gel, processed as indicated in the “Material“s and Methods” section, and the glycopeptides analyzed by MS-MS in an Orbitrap Fourier transform mass spectrometer (FTMS) with electron transfer dissociation (ETD) and higher energy collision-induced dissociation (HCD). The data confirm all three serine residues previously reported [21], also indicated in Figure 1, are modified in CtxB-BCAL2737a. The modified serine residues are shown in red. (c) Heatmap of BCAL2737a peptides observed in peptidome preparations of B. cenocepacia K56-2. Peptidome datasets from Oppy et al. [32] were reanalyzed against a K56-2 proteome containing the BCAL2737a protein sequence, resulting in the identification of multiple peptide breakdown products previously not assigned to known proteins, which are clearly both more numerous and more intense in the glycosylation null strain ΔpglL compared to K56-2 and the pglL complemented strain [32]. B, Biological replicate
Glanders-infected horse serum samples contain anti-O-glycan antibodies
An indirect ELISA was employed to evaluate if glycosylated CtxB-BCAL2737a can be used for diagnosis of glanders. The ELISA was first optimized to determine the optimal antigen concentration and serum dilutions that could allow for a differentiation of positive vs. negative results using purified glycosylated and unglycosylated CtxB-BCAL2737a protein antigen and serum sample 19–5577_37 which was shown strong positive in both CFT and an indirect ELISA based on semi-purified B. mallei (Table 1 and Figure 4a). From these results, we chose 31 pg/ml as the optimal antigen concentration and 1:1000 as the optimal serum dilution. Next, we performed the ELISA against the glycosylated CtxB-BCAL2737a protein using unabsorbed serum samples from 32 horses diagnosed with glanders and healthy controls, previously tested by CFT and an indirect ELISA based on semi-purified B. mallei (Table 1). This assay provided appropriate separation of positive vs. negative results, except in three samples (Figure 4b, arrows). Two of these samples, MRI#1 and Horse_3-2604, were positive by ELISA with unadsorbed sera, as indicated by OD value slightly higher than the cutoff value. However, MRI#1 was negative in CFT but positive by indirect ELISA based on semi-purified B. mallei; Horse_3-2604 was positive in both CFT and indirect ELISA based on semi-purified B. mallei. Further, serum 19–5577_4 has a higher background in our indirect ELISA based on CtxB-BCAL2737a. To improve specificity, serum samples were adsorbed with unglycosylated CtxB-BCAL2737a protein (see the “Materials and Methods”” section) and retested. The results showed that 12 samples testing positive in both CFT and B. mallei indirect ELISA also gave positive results in the ELISA based on glycosylated CtxB-BCAL2737a. They included seven samples (14–566_1831, 14–566_1850, 14–566_1861, 14–566_1899, 14–566_1917, 16–2439_81, 16–2439_85) from South America (all from confirmed cases of glanders at different locations), and five samples (19–5577_3, 19–5577_4, 19–5577_6, 19–5577_37, 19–5577_38) from the Middle East (from an outbreak in the same farm). However, three of the positive samples (19–5577_3, 19–5577_6, 16–2439_81) showed nonspecific interactions with the unglycosylated control, as indicated by slightly higher OD values than the cutoff value (Figure 4). The remaining positive samples had strong interaction with glycosylated protein only, indicating these serum samples contained specific anti-glycan antibodies. Further, two samples (18–1575/2905, 19–5577_39) gave inconclusive results by CFT, but these two samples test negative in the indirect ELISA based on semi-purified B. mallei (Table 1). Based on the negative results by the ELISA using glycosylated CtxB-BCAL2737a, we considered these samples as negative. Interestingly, three samples (Horse_1(Océane) D19/04, Horse_2(Poupée) D19/04, and Horse_3(Princese) D26/04) from an immunization trial with heat-inactivated B. mallei tested negative in ELISA based on glycosylated CtxB-BCAL2737a as opposed to the results in CFT and ELISA based on semi-purified B. mallei (Table 1). From these results, we concluded that the ELISA based on glycosylated CtxB-BCAL2737a was accurate with sensitivity and specificity of 88.23% and 100%, respectively (Table 2).
Table 1.
Comparison of antibody detection in 32 horse serum samples by CFT, indirect ELISA (iELISA) based on semi-purified B. mallei, and iELISA and Western blot based on glycosylated CtxB-BCAL2737a
| Sample | Origin | CFTa | iELISAb- semi-purified B. mallei (S/P%) |
iELISAc CtxB-BCAL2737a |
Western blot CtxB-BCAL2737a |
|---|---|---|---|---|---|
| 18–117/302 | France | - | - (3%) | - | - |
| 18–1575/2905 | France | ± (1) | - (4%) | - | - |
| 13–3290/7936 | Ireland | - | - (3%) | - | - |
| 13–3290/7937 | Ireland | - | - (1%) | - | - |
| 13–3290/7938 | Ireland | - | - (0%) | - | - |
| 13–3290/7939 | Ireland | - | - (12%) | - | - |
| 13–3290/7940 | Ireland | - | - (1%) | - | - |
| 18–103/214 | Tunisia | - | - (7%) | - | - |
| 18–103/215 | Tunisia | - | - (3%) | - | - |
| 18–103/216 | Tunisia | - | - (4%) | - | - |
| 18–103/218 | Tunisia | - | - (7%) | - | - |
| 14–566_1831 | South America | + (421) | + (149%) | + | + |
| 14–566_1850 | South America | + (44,431) | + (128%) | + | + |
| 14–566_1861 | South America | + (42) | + (180%) | + | + |
| 14–566_1899 | South America | + (4) | + (134%) | + | + |
| 14–566_1917 | South America | + (432) | + (173%) | + | + |
| 16–2439_81 | South America | + (44,442) | + (63%) | + | + |
| 16–2439_85 | South America | + (4442) | + (146%) | + | + |
| 19–5577_3 | Middle East | + (444,443) | + (73%) | + | - |
| 19–5577_4 | Middle East | + (4442) | + (107%) | + | + |
| 19–5577_6 | Middle East | + (444,441) | + (119%) | + | + |
| 19–5577_37 | Middle East | + (4441) | + (96%) | + | + |
| 19–5577_38 | Middle East | + (333) | + (47%) | + | - |
| 19–5577_39 | Middle East | ± (1) | - (29%) | - | - |
| Horse_1 (Océane) | D08/02 immunization triald | - | - | - | - |
| Horse_2 (Poupée) | D08/02 immunization triald | - | - | - | - |
| Horse_3 (Princese) | D08/02 immunization triald | - | - | - | - |
| Horse_4 (Quirina) | D08/02 immunization triald | - | - | - | - |
| Horse_1 (Océane) | D19/04 immunization triald | + (32) | + (47%) | - | - |
| Horse_2 (Poupée) | D19/04 immunization triald | + (444) | + (60%) | - | + |
| Horse_3 (Princese) | D26/04 immunization triald | + (443) | + (119%) | - | + |
| MRI#1 | Lyophilized serum from a naturally infected horse | - | + (111%) | - | - |
aNumbers in parenthesis indicate the magnitude of the CFT reported from the combination of two parameters: the last dilution giving a positive result combined with the intensity of hemolysis inhibition indicated as 0 = 0%, 1 = 25%, 2 = 50%, 3 = 75%, and 4 = 100%. Typically, sera were tested at dilutions 1/5, 1/10, 1/20, 1/40 and 1/80 and in some strong positives at 1/160.
bNumbers in parenthesis result from the following formula: (OD_Sample-OD_Negative control)/(OD_Positive control-OD_Negative control) × 100. Values above 40% are considered positive.
cBased on the cutoff OD value indicated in Figure 4.
dThese sera are from an immunization trial with a heat-inactivated B. mallei suspension performed in three horses; D, day/month) of sampling. 08/02: day 0; 19/04 and 26/04, days 63 and 70 post-immunization.
Figure 4.
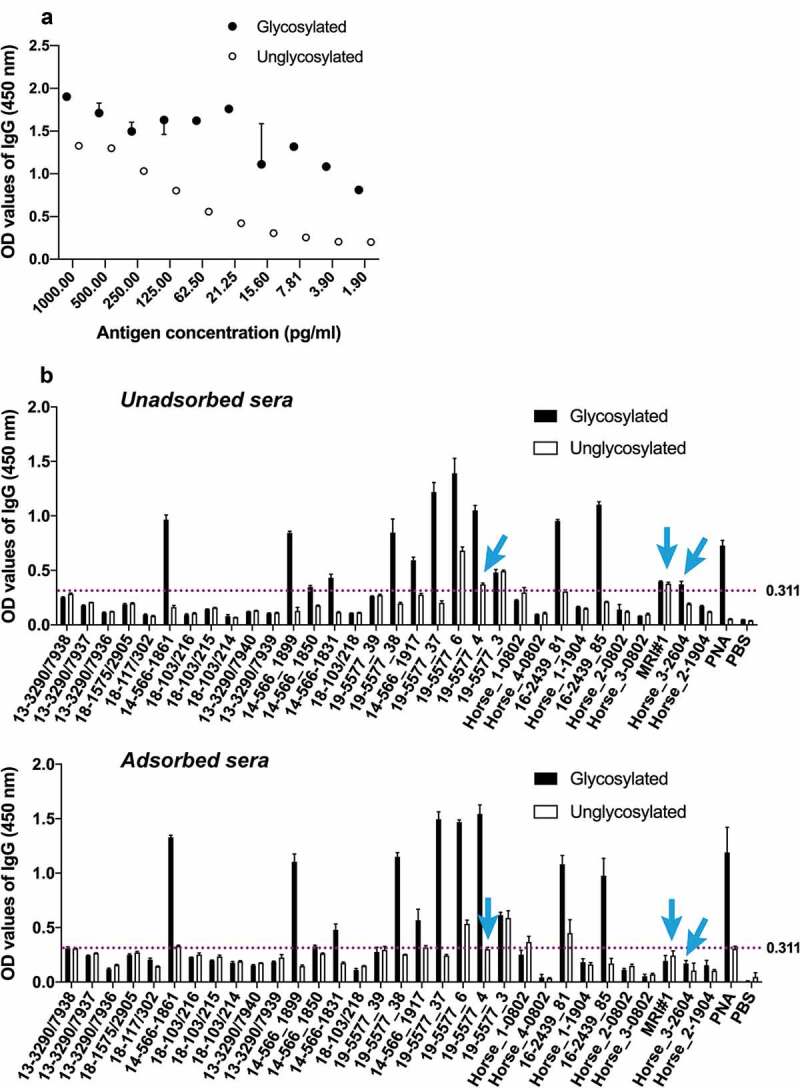
Detection of glycan-specific antibodies by indirect ELISA (see details in the “Materials and Methods” section). (a) Optimization of protein concentration (in pg/ml) and serum dilutions for ELISA using serum sample 19–5577_37 and purified CtxB-BCAL2737a produced in B. cenocepacia K56-2 (glycosylated protein) and ΔpglL (unglycosylated negative control) as a protein antigen. The results indicate the mean ± range of duplicate assays (b) ELISA results using a panel of glanders positive and negative horse serum samples (see Table 1 for additional details). Dotted line indicates the negative cutoff OD450 value for background color in the ELISA determined using 15 CFT negative serum samples. PNA (peanut agglutinin lectin) and PBS were also used as additional positive and negative controls, respectively. ELISA were done with unadsorbed and adsorbed sera (using unglycosylated CtxB-BCAL2737a, as described in Results. Arrows indicate serum samples that showed OD values higher than the cutoff value with unabsorbed sera and lower than the cutoff value with absorbed sera. Three technical replicates were performed for each sample
Table 2.
Results of ELISA and western blot analysis of 32 horse serum samples
| Assay (Results)a | Reference testb (+) | Reference testb (−) |
|---|---|---|
| ELISA (+) | 15 | 0 |
| ELISA (−) | 2 | 15 |
| Western blot (+) | 15 | 0 |
| Western blot (−) | 2 | 15 |
aTwo samples giving inconclusive results (±) in CFT were excluded from these comparisons.
bCFT was used as reference.
To further validate the ELISA results, we carried out western blots with unabsorbed horse sera using glycosylated CtxB-BCAL2737a and its unglycosylated form as a control. As expected, the results of western blot and ELISA agree, except for four samples (19–5577_3, 19–5577_38, Horse_2(Poupée) D19/04, and Horse_3(Princese) D26/04). The samples 19–5577_38 and 19–5577_3 were strongly positive in ELISA but negative in western blot, which could reflect differences in antibody titers related to the stage on disease at the time of serum extraction, since both sera correspond to infected animals in the same farm. In the other two samples, Horse_2(Poupée) D19/04 and Horse_3(Princese) D26/04, tested negative in ELISA but were positive in western blot (Figure 5). These samples were considered true positives because they were also positive in both CFT and B. mallei ELISA. Moreover, same sensitivity and specificity was observed in western blot as compared to ELISA (Table 2), indicating that both methods can be used to detect anti-O-glycan antibodies in sera from infected horses.
Figure 5.
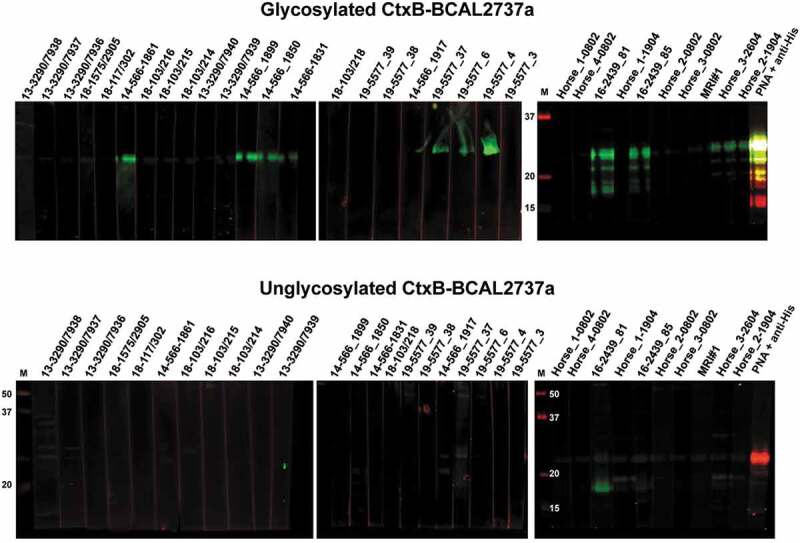
Western blot analysis of unadsorbed horse serum samples (see Table 1 for additional details) using glycosylated (top blots) and unglycosylated (bottom blots) CtxB-BCAL2737a. Blots were developed as described in the “Materials and Methods” section. As a control, glycosylated and unglycosylated CtxB-BCAL2737a were developed with PNA + anti-His (last lane in both series of blots). M, molecular mass markers; masses indicated in kilodaltons
Glycosylated CtxB-BCAL2737a can be used to detect anti-O-glycan antibodies in human serum samples from patients infected with various Burkholderia species
To examine whether glycosylated CtxB-BCAL2737a can also detect anti-O-glycan antibodies elicited from infections caused by other Burkholderia species, nine serum samples collected from patients infected with B. multivorans, B. cenocepacia, B. mallei, and B. pseudomallei were used for western blots analysis. These samples had been reported to recognize an O-glycosylated DsbA1 protein from Neisseria meningitidis when expressed in B. cenocepacia [18]. The results show that glycosylated CtxB-BCAL2737a but not the unglycosylated form can be recognized by antibodies present in these serum samples (Figure 6), further emphasizing that glycosylated CtxB-BCAL2737a can be used to detect anti-O-glycan antibodies resulting from not only from B. mallei but also from other Burkholderia-associated infections.
Figure 6.
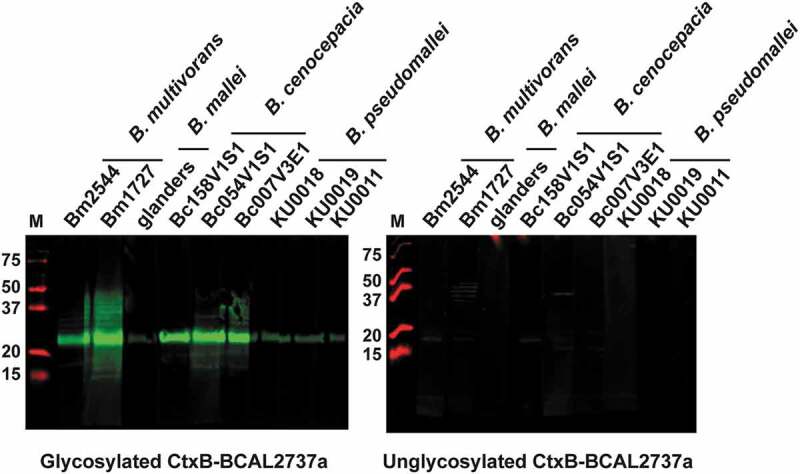
Western blot analysis of unadsorbed human serum samples from patients infected with the indicated Burkholderia species, as previously reported [20] using glycosylated and unglycosylated CtxB-BCAL2737a. Blots were developed as described in the “Materials and Methods” section. M, molecular mass markers; masses indicated in kilodaltons
Discussion
Glanders poses a significant threat to both the equine industry and human health. Successful control of glanders infection requires reliable diagnostic tools. Although numerous methods [9–11,13,16,18,35] have been described for diagnosis of glanders, some have limitations [9–11,18]. Protein glycosylation, a post-translational modification that covalently attaches a glycan to a protein, is prevalent in Archaea and bacteria [36,37]. As some glycans contain unusual carbohydrates that are highly immunogenic, glycan-specific antibodies are attractive targets for diagnosis of bacterial infections and vaccine design [38]. In this study, we exploited the conserved trisaccharide glycan synthesized by the Burkholderia O-glycosylation system to develop a glycoconjugate antigen for the diagnosis of glanders.
Previous studies on protein substrates for the Burkholderia O-glycosylation system revealed an abundant highly glycosylated glycopeptide in B. cenocepacia, which could not be ascribed to any annotated gene [21]. In this work, we identified and annotated this gene as BCAL2737a. The corresponding protein has three serine residues that can be O-glycosylated, as demonstrated by mass spectrometry analysis. An optimal O-glycosylation motif, WPAAASAP (the underlined serine is the glycosylation acceptor site), required for recognition by the Neisseria meningitidis PglL O-Tase has been suggested [39], which is very similar to the sequences where we detect glycosylated serine residues in Burkholderia glycoproteins [20,21,32]. The presence of three glycosylation sites in BCAL2737a, coupled to its small mass, make this protein an ideal carrier for presenting the trisaccharide. Our results demonstrated that Burkholderia O-glycosylation system can efficiently glycosylate the recombinant BCAL2737a protein with the correct trisaccharide structure. Moreover, fusion of this protein with the CtxB at N- and C-terminal locations did not affect the glycosylation of the BCAL2737a partner, suggesting that the glycosylation sites in BCAL2737a are accessible by the Burkholderia PglL O-Tase. This is consistent with the prediction that native glycosylation sites in bacterial proteins are located in flexible structures [40]. However, we noticed that the native BCAL2737a polypeptide, as well as the BCAL2737a-CtxB fusion was unstable in the O-glycosylation-deficient mutants of B. cenocepacia K56-2. In bacterial N-glycosylation systems such as Campylobacter jejuni, loss of glycosylation affects the stability of the glycoproteome, which in turns reduces bacterial fitness and virulence [41,42]. Similar observations were made with protein O-glycosylation in Burkholderia [20], although the analysis of the proteome indicates that only some glycoproteins are highly reduced in abundance while others do not change significantly in the absence of glycosylation [32]. Remarkably, BCAL2737a and BCAL2737a-CtxB were not detected in O-glycosylation defective mutants, indicating they are unstable in the absence of glycosylation. Our results demonstrated that unglycosylated BCAL2737a can only be stabilized when N-terminally fused with CtxB. The instability of BCAL2327a prevented us from using this protein in its unglycosylated form as a negative control in our serological assays, and to adsorb non-O-glycan potentially cross-reacting antibodies in tested sera. Together, our results suggest that O-glycosylation is required for the stability of BCAL2737a, possibly by assisting the folding of this polypeptide and preventing its degradation by periplasmic proteases. In this scenario, the N-terminally fused CtxB could help BCAL2737a to fold properly in the absence of glycosylation or at least adopt a proteolysis resistant conformation. Confirmation of this hypothesis awaits structural information of the chimeric protein.
Detection of anti-glycan antibodies using ELISA and western blot based on glycosylated CtxB-BCAL2737a suggests this antigen can be used for diagnosis of glanders, as high specificity (100%) and sensitivity (88.23%) were achieved by these two methods. Validation of this test in a larger cohort of serum samples will be required to establish its specificity and sensitive more accurately. The ELISA test was slightly improved concerning background by absorbing the horse serum with non-glycosylated CtxB-BCAL2737. However, this step was only necessary for 3 samples and can be avoided. Concerning the few false-negative results in both ELISA and western blot, several factors could affect the diagnostic reliability of ELISA and western blot, such as the purity and amount of the antigen, dilutions of test sample, and other interferences. We observed that the established protocol for ELISA worked well in detection of antibodies from samples of naturally infected horses and did not have false positives in sera from noninfected animals. However, the ELISA failed to detect anti-O-glycan antibodies in samples obtained from an immunization trial with a heat-inactivated B. mallei preparation, especially from samples taken at 63 and 70 days after the trial’s initiation. In contrast, western blots were positive in later samples (see Table 1). It is likely that poor detection may be due to very low antibody titers against the O-glycan upon immunization with heat-inactivated B. mallei due to protein denaturation resulting in levels below the ELISA detection limit. This notion agrees with the finding that anti-O-glycan antibodies could be detectable by western blot upon increasing the amount of serum in the assay, suggesting that the heat-inactivated B. mallei antigen is a less potent inducer of anti-O-glycan antibodies compared to a natural infection. It is also possible that the major antibody isotype against the O-glycan in these sera was IgM, not IgG, due to the nature of the antigen and the immunization protocol. Detection of both IgM and IgG antibody classes in future trials may help improve the sensitivity of detection of anti-glycan antibodies in early infection. Further, our results showed that some samples appeared to have nonspecific interactions with unglycosylated CtxB-BCAL2737a in ELISA. It is unlikely that these samples contain cross-reactive antibodies that can recognize the carrier protein, because they did not interact with unglycosylated CtxB-BCAL2737a by western blot. Therefore, this might be attributed to contaminating proteins in the CtxB-BCAL2737a antigen preparation. Nevertheless, the combined use of ELISA and western blot was important to confirm inconclusive results. Further optimization and standardization of these assays are currently underway in our laboratory.
In conclusion, we have developed a recombinant glycoprotein antigen, CtxB-BCAL2737a, and have shown that ELISA and western blot assays based on the glycosylated CtxB-BCAL2737a can be used for diagnosis of glanders. Particularly, our ELISA test gave identical results compared to the semi-purified B. mallei ELISA [18]. Combined with western blot, anti-O-glycan ELISA can add to the diagnostic tools for glanders. Diagnosing glanders, an OIE notifiable disease, have strong repercussions since it implies the slaughter of positive animals, and carries a negative impact on trade with other countries. Therefore, having access to a battery of different tests with robust specificity is important for a final decision. More broadly, our data support the notion that the conserved protein O-glycosylation system of Burkholderia can be used for diagnosis of other infections caused by these opportunistic bacteria.
Supplementary Material
Acknowledgments
We thank Dr Nora Madani for supplying equine sera from the experimental trial with B. mallei and Dr Keren Turton for a critical review of the manuscript. We also thank Dr Pat Lenihan (Ireland), Dr. Vania Lucia Santana (Brazil), and Prof. Mohammed Sami A (Kuwait) for providing field negative and positive horse sera. We thank the Melbourne Mass Spectrometry and Proteomics Facility of The Bio21 Molecular Science and Biotechnology Institute at The University of Melbourne for access to mass spectrometry infrastructure.
Funding Statement
This research was supported by a Medical Research Council (Confidence in Concept grant CD1617-CIC04) to M.A.V. and R.J.I., and by National Health and Medical Research Council of Australia (NHMRC) project grants APP1100164 awarded to N.E.S; National Health and Medical Research Council (Australia) [APP1100164]; Medical Research Council Canada (UK) [CD1617-CIC04]
Disclosure statement
No potential conflicts of interest were reported by the authors.
Supplementary material
Supplemental data for this article can be accessed here.
References
- [1].Van Zandt KE, Greer MT, Gelhaus HC.. Glanders: an overview of infection in humans. Orphanet J Rare Dis. 2013. September;3(8):131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Khan I, Wieler LH, Melzer F, et al. Glanders in animals: a review on epidemiology, clinical presentation, diagnosis and countermeasures. Transbound Emerg Dis. 2013. June;60(3):204–221. [DOI] [PubMed] [Google Scholar]
- [3].Scholz HC, Joseph M, Tomaso H, et al. Detection of the reemerging agent Burkholderia mallei in a recent outbreak of glanders in the United Arab Emirates by a newly developed fliP-based polymerase chain reaction assay. Diagn Microbiol Infect Dis. 2006. April;54(4):241–247. [DOI] [PubMed] [Google Scholar]
- [4].Ghori MT, Khan MS, Khan JA, et al. Seroprevalence and risk factors of glanders in working equines - Findings of a cross-sectional study in Punjab province of Pakistan. Acta Trop. 2017. December;176:134–139. [DOI] [PubMed] [Google Scholar]
- [5].Fonseca-Rodríguez O, Pinheiro Júnior JW, Mota RA.. Spatiotemporal analysis of glanders in Brazil. J Equine Vet Sci. 2019. July;78:14–19. [DOI] [PubMed] [Google Scholar]
- [6].Adhikari N, Acharya KP, Wilson RT. The potential for an outbreak of glanders in Nepal. Trop Med Health. 2019;47:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Singha H, Shanmugasundaram K, Tripathi BN, et al. Serological surveillance and clinical investigation of glanders among indigenous equines in India from 2015 to 2018. Transbound Emerg Dis. 2020. January 9;67:1336–1348. [DOI] [PubMed] [Google Scholar]
- [8].Rotz LD, Khan AS, Lillibridge SR, et al. Public health assessment of potential biological terrorism agents. Emerg Infect Dis. 2002. February;8(2):225–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Naureen A, Saqib M, Muhammad G, et al. Comparative evaluation of Rose Bengal plate agglutination test, mallein test, and some conventional serological tests for diagnosis of equine glanders. J Vet Diagn Invest. 2007;19:362–367. [DOI] [PubMed] [Google Scholar]
- [10].Khan I, Wieler LH, Melzer F, et al. Comparative evaluation of three commercially available complement fixation test antigens for the diagnosis of glanders. Vet Rec. 2011. November 5;169(19):495. [DOI] [PubMed] [Google Scholar]
- [11].Laroucau K, Colaneri C, Jay M, et al. Interlaboratory ring trial to evaluate CFT proficiency of European laboratories for diagnosis of glanders in equids. Vet Rec. 2016. June 18;178(25):632. [DOI] [PubMed] [Google Scholar]
- [12].Sprague LD, Zachariah R, Neubauer H, et al. Prevalence-dependent use of serological tests for diagnosing glanders in horses. BMC Vet Res. 2009. September;1(5):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Karimi A, Mosavari N. Development of Rose Bengal test against mallein test for rapid diagnosis of equine glanders. Trop Anim Health Prod. 2019. September;51(7):1969–1974. [DOI] [PubMed] [Google Scholar]
- [14].Elschner MC, Scholz HC, Melzer F, et al. Use of a Western blot technique for the serodiagnosis of glanders. BMC Vet Res. 2011. January;19(7):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kumar S, Malik P, Verma SK, et al. Use of a recombinant Burkholderia intracellular motility a protein for immunodiagnosis of glanders. Clin Vaccine Immunol. 2011. September;18(9):1456–1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Singh S, Dohre SK, Kamthan A, et al. Improvement of recombinant-truncated Burkholderia motility protein A (BimA)-based indirect ELISA for equine glanders. J Immunoassay Immunochem. 2018;39(5):565–575. [DOI] [PubMed] [Google Scholar]
- [17].Singha H, Malik P, Goyal SK, et al. Optimization and validation of indirect ELISA using truncated TssB protein for the serodiagnosis of glanders amongst equines. ScientificWorldJournal. 2014;2014:469407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Elschner MC, Laroucau K, Singha H, et al. Evaluation of the comparative accuracy of the complement fixation test, Western blot and five enzyme-linked immunosorbent assays for serodiagnosis of glanders. PLoS One. 2019;14(4):e0214963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Dohre SK, Kamthan A, Singh S, et al. Identification of a new diagnostic antigen for glanders using immunoproteome analysis. Comp Immunol Microbiol Infect Dis. 2017. August;53:26–32. [DOI] [PubMed] [Google Scholar]
- [20].Fathy Mohamed Y, Scott NE, Molinaro A, et al. A general protein O-glycosylation machinery conserved in Burkholderia species improves bacterial fitness and elicits glycan immunogenicity in humans. J Biol Chem. 2019. September 6;294(36):13248–13268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Lithgow KV, Scott NE, Iwashkiw JA, et al. A general protein O-glycosylation system within the Burkholderia cepacia complex is involved in motility and virulence. Mol Microbiol. 2014. April;92(1):116–137. [DOI] [PubMed] [Google Scholar]
- [22].Aubert DF, Flannagan RS, Valvano MA. A novel sensor kinase-response regulator hybrid controls biofilm formation and virulence in Burkholderia cenocepacia. Infect Immun. 2008;76:1979–1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Figurski DH, Helinski DR. Replication of an origin-containing derivative of plasmid RK2 dependent on a plasmid function provided in trans. Proc Natl Acad Sci USA. 1979;76(4):1648–1652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Swamy MJ, Gupta D, Mahanta SK, et al. Further characterization of the saccharide specificity of peanut (Arachis hypogaea) agglutinin. Carbohydr Res. 1991. June;25(213):59–67. [DOI] [PubMed] [Google Scholar]
- [25].Rappsilber J, Mann M, Ishihama Y. Protocol for micro-purification, enrichment, pre-fractionation and storage of peptides for proteomics using StageTips. Nat Protoc. 2007;2(8):1896–1906. [DOI] [PubMed] [Google Scholar]
- [26].Ishihama Y, Rappsilber J, Mann M. Modular stop and go extraction tips with stacked disks for parallel and multidimensional Peptide fractionation in proteomics. J Proteome Res. 2006. April;5(4):988–994. [DOI] [PubMed] [Google Scholar]
- [27].Cox J, Mann M. MaxQuant enables high peptide identification rates, individualized p.p.b.-range mass accuracies and proteome-wide protein quantification. Nat Biotechnol. 2008. December;26(12):1367–1372. [DOI] [PubMed] [Google Scholar]
- [28].Tyanova S, Temu T, Sinitcyn P, et al. The Perseus computational platform for comprehensive analysis of (prote)omics data. Nat Methods. 2016. September;13(9):731–740. [DOI] [PubMed] [Google Scholar]
- [29].Chen Y, Zhang J, Xing G, et al. Mascot-derived false positive peptide identifications revealed by manual analysis of tandem mass spectra. J Proteome Res. 2009. June;8(6):3141–3147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Vizcaíno JA, Csordas A, del-Toro N, et al. 2016 update of the PRIDE database and its related tools. Nucleic Acids Res. 2016. January 4;44(D1):D447–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Perez-Riverol Y, Csordas A, Bai J, et al. The PRIDE database and related tools and resources in 2019: improving support for quantification data. Nucleic Acids Res. 2019. January 8;47(D1):D442–D450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Oppy CC, Jebeli L, Kuba M, et al. Loss of O-Linked Protein Glycosylation in Burkholderia cenocepacia Impairs Biofilm Formation and Siderophore Activity and Alters Transcriptional Regulators. mSphere. 2019. November 13;4(6). DOI: 10.1128/mSphere.00660-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Carver T, Berriman M, Tivey A, et al. Artemis and ACT: viewing, annotating and comparing sequences stored in a relational database. Bioinformatics. 2008. December 1;24(23):2672–2676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Almagro Armenteros JJ, Tsirigos KD, Sonderby CK, et al. SignalP 5.0 improves signal peptide predictions using deep neural networks. Nat Biotechnol. 2019. April;37(4):420–423. [DOI] [PubMed] [Google Scholar]
- [35].de Carvalho Filho MB, Ramos RM, Fonseca AA Jr., et al. Development and validation of a method for purification of mallein for the diagnosis of glanders in equines. BMC Vet Res. 2012. September;2(8):154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Nothaft H, Szymanski CM. Protein glycosylation in bacteria: sweeter than ever. Nat Rev Microbiol. 2010. November;8(11):765–778. [DOI] [PubMed] [Google Scholar]
- [37].Koomey M. O-linked protein glycosylation in bacteria: snapshots and current perspectives. Curr Opin Struct Biol. 2019. June;56:198–203. [DOI] [PubMed] [Google Scholar]
- [38].Harding CM, Feldman MF. Glycoengineering bioconjugate vaccines, therapeutics, and diagnostics in E. coli. Glycobiology. 2019. July 1;29(7):519–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Pan C, Sun P, Liu B, et al. Biosynthesis of conjugate vaccines using an O-linked glycosylation system. MBio. 2016. April 26;7(2):e00443–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Kowarik M, Numao S, Feldman MF, et al. N-linked glycosylation of folded proteins by the bacterial oligosaccharyltransferase. Science. 2006. November 17;314(5802):1148–1150. [DOI] [PubMed] [Google Scholar]
- [41].Cain JA, Dale AL, Niewold P, et al. Proteomics reveals multiple phenotypes associated with N-linked glycosylation in Campylobacter jejuni. Mol Cell Proteomics. 2019. January 7;18:715–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Abouelhadid S, North SJ, Hitchen P, et al. Quantitative analyses reveal novel roles for N-glycosylation in a major enteric bacterial pathogen. MBio. 2019. April 23;10(2). DOI: 10.1128/mBio.00297-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


