ABSTRACT
This study investigates the hypotheses that during passive heat stress, the change in perception of time and change in accuracy of a timed decision task relate to changes in thermophysiological variables gastrointestinal temperature and heart rate (HR), as well as subjective measures of cognitive load and thermal perception. Young adult males (N = 29) participated in two 60-min head-out water immersion conditions (36.5°C-neutral and 38.0°C-warm). Cognitive task measurements included accuracy (judgment task), response time (judgment ask), and time estimation (interval timing task). Physiological measurements included gastrointestinal temperature and heart rate. Subjective measurements included cognitive task load (NASA-TLX), rate of perceived exertion, thermal sensation, and thermal comfort. Gastrointestinal temperature and HR were significantly higher in warm versus neutral condition (gastrointestinal temperature: 38.4 ± 0.2°C vs. 37.2 ± 0.2°C, p < 0.01; HR: 105 ± 8 BPM vs. 83 ± 9 BPM, p < 0.01). The change in accuracy was significantly associated with the change in gastrointestinal temperature, and attenuated by change in thermal sensation and change in HR (r2=0.40, p< 0.01). Change in response time was significantly associated with the change in gastrointestinal temperature (r2=0.26, p< 0.002), and change in time estimation was best explained by a change in thermal discomfort (r2=0.18, p< 0.01). Changes in cognitive performance during passive thermal stress are significantly associated with changes in thermophysiological variables and thermal perception. Although explained variance is low (<50%), decreased accuracy is attributed to increased gastrointestinal temperature, yet is attenuated by increased arousal (expressed as increased HR and warmth thermal sensation).
KEYWORDS: Thermoregulation, passive heat stress, cognitive performance, heat, time perception
Introduction
Cognitive performance might be affected in people that work and live in hot and humid environments [1–6]. A recent review suggests that raised core temperature is associated with a reduction in vigilance, and more complex dual-task performance, even though the effects slightly differed between the independent studies [4]. In hot conditions, severe reductions in physical and cognitive performance become apparent with dehydration [25–27], and there is also increasing evidence that environmental changes and corresponding elevations in skin temperature and subjective experience of heat, without increase in core temperature, negatively influence cognitive performance [7–9]. In terms of decision-making Gaoua et al. (2012) [7], conclude that an increase in skin temperature and the subjective experience of being warm impair effective decision-making. For the case that both skin and core temperature increase, in concurrency with a warm thermal sensation, we reported earlier that an underproduction of a time interval is associated with lower accuracy [10]. An explanation for the underproduction of a time interval is in line with findings in the field of time perception which suggests that core body temperature itself mediates the subjective experience of time [28, 29] and research in the field of decision-making indicating the importance of a correct estimation of the passing of time for decision-making [11–13]. This has important practical implications for the operational efficiency of people with occupations that are associated with hyperthermia due to high activity, clothing insulation, or hot (humid) work environments (e.g. soldiers, police officers, firefighters, or steelworkers).
It is therefore valuable to be able to judge the confidence in a decision before making a decision. Tamm et al., 2014, showed that the perception of time is compressed when participants’ core temperature is elevated, however only with a certain amount of experienced physical fatigue. In addition, recent studies highlight the importance of the subjective experience of people to heat exposure on cognitive performance [6–8]. Therefore, the quality of decisions in hot circumstances may be assessed by either a subjective measure such as the rate of perceived exertion, or by how “hard” a cognitive task is (e.g. NASA Task Load Index, [30]), or by physiological measures such as core body temperature and heart rate.
However, it is not known how time estimation, reaction time, and the accuracy of decision-making (cognitive performance) are associated with subjective cognitive performance, subjective thermal perception, or thermophysiological responses. This study further investigates previous findings on the effect of passive heat stress on decision-making [10]. Specifically, the association between objective cognitive performance and subjective cognitive performance, and the association between objective cognitive performance and gastrointestinal temperature and heart rate is examined. The aim is to gain an understanding of the dynamic relationship between subjectively experienced load, physiological indicators, and objective task performance.
Concurrent with data reported by others stated above, it is hypothesized that with significantly increased gastrointestinal temperature participants’ change in time estimation, change in reaction time and change in accuracy in a timed decision task are associated with thermophysiological variables: change in gastrointestinal temperature and change in heart rate and subjective variables: change in subjective cognitive task load, change in subjective thermal assessment, and change in rate of perceived exertion.
Methods
Ethical approval
The ethical committee of The Netherlands Organization of Applied Scientific Research approved the study. Each subject gave written informed consent prior to participation in the study. All procedures conformed the standards of the Declaration of Helsinki.
Participants
Twenty-nine young adult males participated in this study (see Table 1 for characteristics).
Table 1.
Participant characteristics, values are mean ± SD
| N | 29 |
| Age (yr) | 23 ± 4 |
| Height (m) | 1.78 ± 0.33 |
| Mass (kg) | 76.8 ± 8.0 |
| BMI (kg/m2) | 22.9 ± 2.1 |
| Dubois body surface area (m2) | 1.98 ± 0.1 |
All participants were healthy, non-obese, not regularly taking medications and did not have any known motoric issues with the upper limbs. Participants were instructed to refrain from alcoholic beverages 24 h before the test, not to perform medium to heavy exercise on the day before the test and not to use medication up to 1 week before the test (with the exception of a single paracetamol 500 mg). Participants were asked to have consumed a meal and drink water before they arrived.
Design
Time perception and decision-making tasks were performed in two conditions, a neutral temperature condition and an elevated gastrointestinal temperature condition (~38.5°C). Body gastrointestinal temperature was clamped by head-out water immersion in a water temperature of 36°C in the neutral condition and in a water temperature of 38°C in the warm condition. The bath temperatures are based on immersion experiments reported by Craig & Dvorak [14]. Pilot testing confirmed that gastrointestinal temperature remains stable in the neutral bath condition and gastrointestinal temperature increases to and plateaus to ~38.5°C within 40 minutes. Participants are exposed to the two conditions at two different days, at the same time of day, with at least 24 h between testing days, and the order of the interventions is randomized.
Measurements
Cognitive measurements
Participants performed two cognitive tasks, an interval timing task frequently used in time perception research and an adapted version of the expanded judgment task [12,15,16].
Interval timing task
In this task, the participant presses a button when a fixation cross appears in the middle of the screen, and then the participant aims to press the button again exactly 1 s later. Before the start of the experiment, participants learn to estimate these 1 s and receive feedback about their performance.
Expanded judgment task
Two flickering white circles on a black background appear next to each other on the screen and the participant has to estimate which circle has the highest flicker rate. The answer is given by pressing a button in the left hand for the left circle and pressing a button in the right hand for the right circle. Participants are instructed to pay more attention to accuracy than to speed; however, they should answer within 1 s. After 1 s, feedback is given on the screen about their performance (“correct,” “incorrect,” “too slow”).
Physiological measurements
Body gastrointestinal temperature
Body gastrointestinal temperature is measured with an ingested capsule (e-Celsius Performance, BodyCap, Cain, France) which is ingested 1 h to 45 min before the onset of the measuring session (in one case a participant arriving late at the laboratory ingested the pill 30 min before the onset of measuring). This has the advantage that we reduce the variation in the pill location in the body (all around stomach). However, in some disciplines involved in thermal physiology, it is common to ingest the pill the night before the experiment up to 6 h before the experiment. The main arguments for this are to be (1) less susceptible for measurement artifacts due to eating or drinking, (2) as the pill location after that time is more close to the rectum, the recorded temperature is more in line with rectal temperature. Nevertheless for the purpose of measurement of abdominal gastrointestinal temperature, in absence of eating or drinking, there is no significant difference in pill temperature when ingested 24 h or 40 min before an exercise [17]. Therefore, participants are not allowed to drink or eat after ingestion of the pill for the duration of the experiment.
Heart rate
Heart rate is measured with an ECG monitor worn around the chest (Polar V800, Polar Electro, Kempele, Finland), and data were recorded with a corresponding watch around the wrist. Care was taken not to lose any signals, because of possible bluetooth transmission issues while submerged.
Body mass
Participant nude weight is measured using a scale (888, Seca, Hamburg, Germany). Because of possible issues with respect to nude exposure to experiment leaders, participants weighed themselves and reported their weight to the experiment leader.
Subjective measurements
Thermal perception and comfort
Thermal sensation is assessed on a 7-point paper scale ranging from very cold (−3) to very hot (+3) according to ISO10551 (1995), and associated thermal comfort is assessed using a 4-point paper scale ranging from comfortable (0) to uncomfortable (+3) according to ISO10551 (2001).
Perceived exertion
Rate of perceived exertion (RPE) from water immersion is assessed using a paper Borg scale (1982).
Cognitive Task load
Workload experienced during tasks is assessed using NASA Task Load Index (NASA-TLX, Hart & Staveland, 1988). The task load index consists of six dimensions that are combined in one index, the dimensions are mental demand, physical demand, temporal demand, performance, effort, and frustration.
Protocol
The protocol consists of a part outside the bath and a part inside the bath, see Figure 1.
Figure 1.
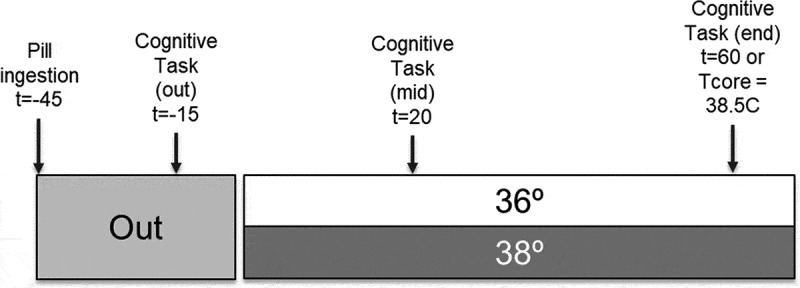
Timeline of the protocol, participants take the pill 45 min before start entering bath; thereafter, participants are prepared and practice the cognitive tests. At T = −15 the experiment starts outside the bath and continues at T = 0 inside the bath. Twenty minutes after entering the bath (T = 20) the second bout of the cognitive tests takes place. Then, either after 60 min in the bath, or when gastrointestinal temperature (Tcore) reaches 38.5°C participants start with the final bout of the cognitive tests. Thereafter, the experiment is finished and participants carefully leave the bath
Outside bath
After signing the consent form, participants ingest a capsule for measurement of gastrointestinal temperature and are equipped with a heart rate monitor. From now on the participant is not allowed to drink or eat anymore throughout the measurement session. Next, the participant practices the cognitive tasks. Participants perform fifty trials of the interval timing task and fifty trials of the expended judgment task to get familiarized with the task (this takes 10 minutes). During the interval timing task, participants receive feedback on the quality of their estimation every trial. Afterward, participants are given the opportunity to empty their bladder and are asked to change into swimming shorts and register their nude weight on a scale. At time −15 participants perform the first bout of the cognitive tasks.
Inside bath
Participants enter the bath and stay in head-out immersion for the remainder of the time. Immediately after immersion participants are asked to indicate thermal sensation, thermal comfort, and rating of perceived exertion (RPE), thereafter every 10 minutes. Furthermore, these values are asked directly before and after the cognitive tasks. The cognitive tasks are performed after 20 minutes of immersion and after 60 minutes of immersion or earlier if gastrointestinal temperature reaches 38.5°C before these 60 minutes (in the warm water condition). The participant performs 100 trials of the interval timing task followed by 100 trials of the expanded judgment task with a total duration of about 15 minutes. Directly after the tasks, participants complete the NASA TLX to assess the workload experienced during the task.
Exiting the bath
Prior experience obtained from pilot experiments has shown that head-out immersion in the warm condition yields a high risk for syncope due to the large peripheral blood flow. Therefore, upon exiting of the bath great care was taken that participants stand up slowly and sit a few minutes on the edge of the bath with only legs in the water. Only when the participant does not experience dizziness and heart rate starts to decline, he is allowed to exit and to report his nude body weight. Participants are dismissed when core body temperature has decreased below 38°C and there are no complaints.
Lab environment and planning
Three jacuzzi bathtubs (Viking Spas, Model Legend 1) were available for the experiments. All tubs were separated by a movable wall. All measurements took place within 3 weeks (November 2017, average ambient temperature 7.3°C), with two time slots per bath per day. During every measurement, one main experiment leader was present to oversee the entire experiment, furthermore, each bathtub was manned by a research assistant. The experiments in the different bathtubs start at the same time and all participants are instructed by the main experiment leader. In order to minimize the risk of heat-related incidents occurring at the same time every time slot has at least one neutral temperature bath.
Stop criteria
Stop criteria are determined by a medical doctor and are aimed at avoiding medical complications and define the endpoint of the experiment. The following stop criteria for individual participants are respected and continually monitored:
Core body temperature exceeding 39.0°C.
Heart rate lower than during rest outside of bath.
Complaints of the participant of dizziness, wooziness, feeling in a daze, headache, nausea, feeling to faint, hyperventilation seen as breathlessness or panic, tingling around the mouth and/or in the hands/arms.
Voluntarily exhaustion.
Data analysis
Data were analyzed for each bout of cognitive tasks. For the interval estimation task, the average of the estimated interval was calculated and for the expanded judgment task, the accuracy, as well as the average response time, was calculated. These variables are referred to as the objective outcome variables. As subjective outcome variables, the answers to the questionnaires immediately after the execution of the tasks were used (thermal perception, thermal comfort, RPE, and NASA-TLX). The ratings for the NASA-TLX were combined into one cognitive workload score by averaging over the six dimensions. For the physiological outcome variables (gastrointestinal temperature and heart rate) data was averaged over the duration of the bout.
Repeated measure ANOVAs were used to test the change in outcome measures for main effect of condition (neutral vs. warm), main effect of time (t = 20, t = 60), and interaction between time and condition. Post-hoc analysis was performed with pairwise t-tests.
Furthermore, the proportion of explained variance (r2-value) of objective cognitive performance vs. subjective measures as well as objective cognitive performance vs. physiological measures was quantified by manual stepwise linear regression. The entry criterion for the stepwise linear regression was that a variable was significantly related to the model residuals (p < 0.05), vice versa for the exit criterion. In case multiple variables satisfied the entry criterion the variables were ranked on expected contribution to explained variance and the highest contributor was entered first. For the second highest contributor a new model was initiated and so on for remaining significantly contributing variables. For all analyses, p < 0.05 was used as a criterion for statistical significance of the effect or relation.
Results
Twenty-nine (n = 29) participants were recruited and performed the tests, however, n = 2 persons did not complete the complete test trials. Furthermore, due to technical and registration failure, the achieved full recordings were reduced to n = 27 for response time, accuracy, and estimation of time, n = 19 for gastrointestinal temperature, n = 23 for heart rate, n = 26 for NASA-TLX, n = 19 for thermal sensation and n = 17 for thermal comfort. Noteworthy, n = 3 participants did complete the study yet they experienced orthostatic hypotension while exiting the warm bath condition. Data from these three participants were included in the analysis as there were no complications during measurements.
Table 2 shows the absolute descriptives of the objective, subjective, and physiological outcome measures for both the neutral and warm conditions. Figure 2 shows the changes compared to baseline in objective, subjective, and physiological outcome measures, and Table 3 produces the tests performed to answer the hypotheses of this study, namely the association between change in objective vs. change in subjective and physiological outcome variables.
Table 2.
Descriptives (mean and standard deviation) of objective, subjective, and physiological outcome variables. Asterisks indicate a significant difference with the first bout (out of bath baseline) in the same condition (p < 0.05 = *, p < 0.01 = **, p < 0.001 = ***). Diamonds indicate a significant difference with the corresponding neutral condition (p < 0.05 = ◊, p < 0.01 = ◊◊, p < 0.001 = ◊◊◊). Objective cognitive measures are reported in [10], yet repeated in this table for completeness
| Neutral condition |
Warm condition |
|||||
|---|---|---|---|---|---|---|
| Outcome variables | Baseline | Mid | End | Baseline | Mid | End |
| Objective | ||||||
| Mean response time (ms) | 0.54 ± 0.09 | 0.52 ± 0.08 * |
0.52 ± 0.09 * |
0.55 ± 0.07 | 0.51 ± 0.08 *** ◊ |
0.48 ± 0.08 *** ◊ |
| Accuracy | 0.81 ± 0.04 | 0.79 ± 0.04 * |
0.79 ± 0.05 | 0.80 ± 0.05 | 0.79 ± 0.04 * |
0.77 ± 0.04 ** |
| Time estimation (ms) | 1.20 ± 0.28 | 1.24 ± 0.36 | 1.27 ± 0.45 | 1.28 ± 0.41 | 1.25 ± 0.42 | 1.17 ± 0.45 ** ◊◊ |
| Subjective | ||||||
| Thermal sensation | −0.4 ± 0.7 | 0.6 ± 0.9 *** |
0.7 ± 0.8 *** |
0.1 ± 0.7 | 2.5 ± 0.6 *** ◊◊◊ |
2.6 ± 0.6 *** ◊◊◊ |
| Thermal discomfort | 0.3 ± 0.8 | 0.2 ± 0.5 | 0.4 ± 0.5 | 0.4 ± 0.5 | 1.4 ± 0.7 *** ◊◊◊ |
1.8 ± 0.9 *** ◊◊◊ |
| RPE | 8.0 ± 1.8 | 8.3 ± 1.9 | 8.3 ± 1.8 | 8.8 ± 2.2 | 11.6 ± 2.6 *** ◊◊ |
12.6 ± 3.0 *** ◊◊◊ |
| NASA-TLX | 10.2 ± 2.3 | 10.9 ± 2.6 | 11.0 ± 2.6 | 10.8 ± 2.5 | 12.7 ± 2.6 | 13.5 ± 2.8 |
| Physiological | ||||||
| gastrointestinal temperature (° C) | 37.1 ± 0.2 | 37.0 ± 0.1 *** |
37.2 ± 0.2 | 37.2 ± 0.3 | 37.7 ± 0.2 *** ◊◊◊ |
38.4 ± 0.2 *** ◊◊◊ |
| Heart rate (BPM) | 74 ± 11 | 80 ± 9 *** |
83 ± 9 *** |
74 ± 9 | 99 ± 9 *** ◊◊◊ |
105 ± 8 *** ◊◊◊ |
Figure 2.
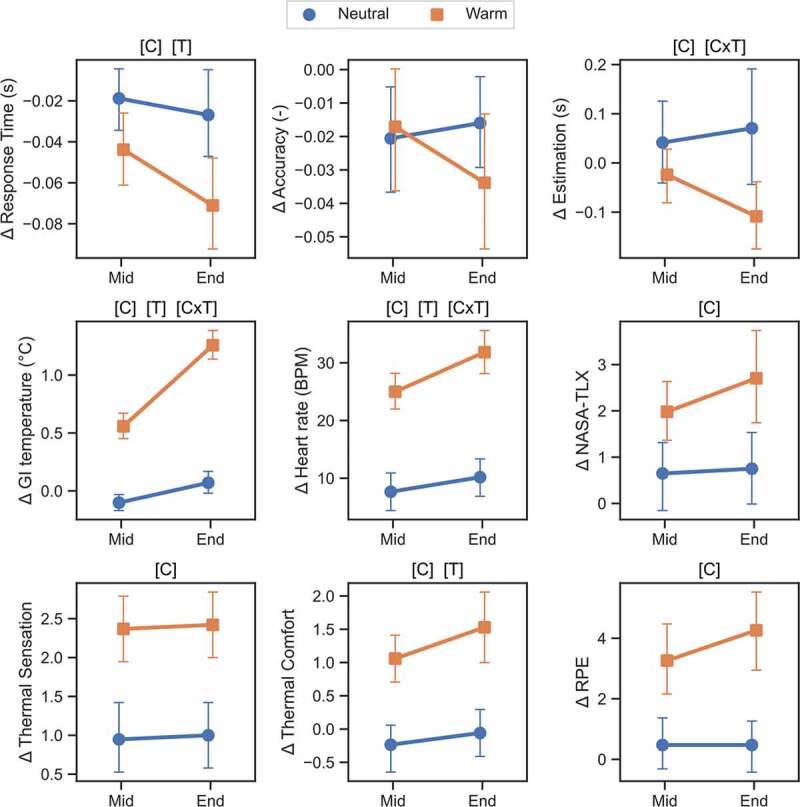
Mean±SD change of objective, subjective, and physiological outcome variables in neutral (blue) and warm condition (red) normalized vs. baseline. [C]: significant effect of condition (p < 0.05), [T]: significant effect of time (p < 0.05), [CxT]: significant interaction effect (p < 0.05). N = 27 for response time, accuracy, and estimation of time, n = 19 for gastrointestinal temperature (GI), n = 23 for heart rate, n = 26 for NASA-TLX, n = 19 for thermal sensation and n = 17 for thermal comfort
Table 3.
Stepwise linear regression models on objective cognitive performance. Number between brackets indicates the order of entry
| ΔThermal Sensation | ΔThermal discomfort | ΔTLX | ΔGI | ΔHR | p-value | r2 | |
|---|---|---|---|---|---|---|---|
| ΔTime estimation | - | −0.102 (1) | - | - | - | <0.01 | 0.18 |
| ΔTime estimation | - | - | - | −0.156 (1) | - | <0.03 | 0.11 |
| ΔResponse time | - | - | - | −0.048 (1) | - | <0.002 | 0.26 |
| ΔAccuracy | 0.013 (3) | - | - | −0.078 (1) | 0.003 (2) | <0.001 | 0.40 |
Results on objective cognitive performance reveal a main effect of higher response times in the neutral condition compared to the warm condition (F(1,26) = 7.21, p = 0.01) as well as an effect of time (F(1,26) = 11.54, p < 0.01) where the end time shows shorter response times than the mid condition. For accuracy no significant main effect of time and condition, nor interaction between time and condition was found; albeit that the interaction effect was not significant (p = 0.08), accuracy was significantly decreased relative to its own baseline in the warm condition (Table 2, p < 0.01). Furthermore, estimation of time is compressed in warm vs. neutral conditions (F(1,26) = 6.48, p < 0.02) including an interaction effect with time (F(1,26) = 11.7, p < 0.001). Post-hoc tests show that only at the end of the experiment, the estimation of time was significantly shorter in the warm condition than in the neutral condition.
Subjective performance measures show a main condition effect for the NASA-TLX indicating that a higher cognitive load was perceived in the warm bath (F(1,25) = 11.85, p = 0.002). Likewise, thermal sensation shows a main effect of the warm vs. neutral condition, where perhaps trivially, subjects perceived their temperature as warmer in the warm bath (F(1,18) = 27.48, p < 0.001). Thermal comfort shows a main (F(1,16) = 29.83, p < 0.001) and time effect (F(1,16) = 5.2, p = 0.04).
The physiological measure, gastrointestinal temperature, shows a significant main effect of condition (F(1,18) = 515.9, p < 0.001), main effect of time (F(1,18) = 99.4, p < 0.001) and interaction effect (F(1,18) = 82.0, p < 0.001). Indicating that gastrointestinal temperature was significantly higher in the warm vs. neutral bath condition, gastrointestinal temperature increased over time in both warm and neutral conditions and there was a greater increase in gastrointestinal temperature in the warm vs. neutral condition. During the mid timepoint in the neutral condition, gastrointestinal temperature was slightly lower than baseline (37.2 ± 0.2°C at baseline vs. 37.1 ± 0.1°C, p < 0.001 at the mid timepoint), yet at the end of the experiment gastrointestinal temperature did not significantly differ from baseline anymore. Finally, heart rate also shows a significant condition effect (F(1,23) = 139.3, p < 0.001), time effect (F(1,23) = 53.0, p < 0.001) and interaction between time and condition (F(1,23) = 17.0, p < 0.01). In all conditions and timepoints, heart rate was significantly greater than baseline.
Relation of change in cognitive task performance to change in subjective and physiological variables
Changes in cognitive performance measures (estimation of time, response time, and accuracy on an expanded judgment task) are all significantly related to the change in gastrointestinal temperature (see Table 3). Change of time estimation is best explained by change in thermal discomfort (r2 = 0.18), i.e. individuals who experienced higher levels of thermal discomfort estimated shorter time intervals. Changes in gastrointestinal temperature also significantly explained change in time estimation albeit to a lesser extent than change in thermal discomfort (r2 = 0.11). With respect to change in response times, only a change in gastrointestinal temperature is significantly related, where a greater increase in gastrointestinal temperature is associated with faster responses on the expanded judgment task. The accuracy is explained by a change in gastrointestinal temperature, heart rate, and thermal sensation (r2 = 0.40). A greater increase in gastrointestinal temperature is associated with a greater decrease in accuracy, yet the accuracy decrement is attenuated by increased heart rate and a warmer rating on the thermal sensation scale.
Discussion
This study aimed to investigate whether it is possible to estimate cognitive task performance from subjective and physiological measures. Results show that
Change in accuracy of an expanded judgment task was significantly associated with a change in gastrointestinal temperature, change in thermal sensation, and change in heart rate.
Change in response times to the same task was significantly associated with change in gastrointestinal temperature.
Change in time estimation was associated with a change in thermal discomfort or with a change in gastrointestinal temperature, but not to any of the other measured physiological or subjective variables.
However, explained variance is not high (all below 50%); hence, the associations may not be viable to use as an operationally relevant decision support on confidence in judgment; nevertheless, the relations provide insight in the interplay between subjective and physiological measures on cognitive performance which is discussed below.
Change in time estimation
Table 2 shows that participants pressed the button earlier when asked to estimate a certain time interval when gastrointestinal temperature was increased. However, the interaction between time and condition showed that this effect was only significantly different from the neutral condition toward the end of the experiment (Figure 2), which is in line with Tamm et al. (2014). Their results indicated that gastrointestinal temperature explains the compressions of time only when a participant has experienced a certain level of fatigue. This result is further supported by our findings from the linear regression analysis, showing that two indicators, thermal discomfort and gastrointestinal temperature explain the change in time estimation. In addition, thermal discomfort explained more variance than gastrointestinal temperature. These results show that an elevation in gastrointestinal temperature alone does not result in a compressed time perception but that the combination of gastrointestinal temperature and fatigue is responsible for the compressed time perception.
Change in response time
In terms of response times, results showed that response times are shortened in the warm condition compared to the neutral condition which is in line with [6,10,18,19]. In part, faster response times can be explained by increased synaptic activity and faster muscle cross-bridge cycling which are associated with increased tissue temperature (Arrhenius law or Q10 effect) [19,20]; nevertheless, a main effect of time showed that the duration of the experiment and time in the water further decreased the response times in both neutral and warm condition – hence also indicating an independent effect on response time. The stepwise linear regression showed that from changes in subjective and physiological measures only change in gastrointestinal temperature explained the change in reaction times. This is in line with Heuvel et al. showing more liberal and quick responses when gastrointestinal temperature is elevated [18]. In addition, Van Maanen et al., 2019, showed that the shorter response times are explained by the effect of lowering the information decision threshold (for more information on decision thresholds see [10,21,22]). The absence of a significant association between change in thermal sensation and change in response time could be a power issue, yet it does indicate that the association of gastrointestinal temperature to change in response time is the stronger of the two. Combined the results suggest that the faster response times can be explained by both neurophysiological (Q10-effect) and cognitive effects (decision threshold) of change in gastrointestinal temperature.
Change in accuracy
With respect to change in accuracy no main effect of time and condition was observed, meaning that there is no significant difference in change in accuracy between the warm and neutral bath and time in the bath. However, as shown in Table 2, and Figure 2, a significant interaction effect emerged. This effect is best described by the significant decrease in accuracy over time for the warm bath conditions whereas for the neutral condition, no differences emerged. Previous studies show that the likelihood of making errors increases with an increase in gastrointestinal temperature and errors are more likely when tasks become more complex [4,20]. Interestingly, a greater increase in gastrointestinal temperature is associated with a greater decrease in accuracy, yet the decrement is attenuated by increased heart rate and a greater sensation of warmth. Both the greater increase in heart rate and a greater sensation of warmth may be indicative of relatively increased arousal, and therefore, compensate the negative effect of increased gastrointestinal temperature.
General discussion, practical translations, and limitations
In addition to the above, participants reported more thermal discomfort, a higher level of perceived physical exertion, and a higher level of thermal sensation in the warm vs. neutral water immersion. The conditions chosen in this experiment thus resulted in both physiological and subjectively experienced load. In line with Martin et al. this study also showed that independent of exercise (i.e. passive heating) subjectively experienced workload (both RPE and TLX) are higher when gastrointestinal temperature is increased [4].
The cognitive tasks used in this experiment were a time estimation task and a timed decision-making task. The findings are in line with other studies showing that attentional and perceptual type of tasks as well as mathematical processing tasks are affected the most by an increase in rectal or gastrointestinal temperature [23]. However, many laboratory tests, including the ones used in this study, have low ecological validity and may it be difficult to interpret what the outcomes mean in practice. As the explained variance remains rather low (<50%) it is possible that the negative effects of increased gastrointestinal temperature on cognitive performance are either compensated (e.g. by arousal) or exacerbated (e.g. by dehydration or solar load) by contextual influences [18,20,24]. It may not be justified to interpret that an increased gastrointestinal temperature in practice yields a lower accuracy on a timed decision task per se. However, for a series of timed decision tasks, decreased accuracy accumulates and potentially leads to decreased performance. Therefore, for occupational settings where fast decision-making (e.g. perceived timed decision tasks) is relevant, cooling strategies may be relevant to maintain performance in the long run.
Conclusion
Changes in cognitive performance during passive thermal stress are significantly associated with changes in thermophysiological variables (gastrointestinal temperature and heart rate) and thermal perception (thermal discomfort and thermal sensation). During decision-making, negative accuracy effects are attributed to increased gastrointestinal temperature, yet this is attenuated by increased arousal (expressed as increased heart rate and warmth thermal sensation). For both cognitive tasks, the associations however are not strong (less than 50% explained variance) and may be of limited use as a measure of confidence in decision accuracy.
Funding Statement
This work was supported by the Dutch Ministry of Defense under Grant V1605 SOLAR; Ministerie van Defensie (NL) [V1605-Solar] and HeatShield under the EU Horizon 2020 programme grant (nr. 668786).
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Hancock PA, Vasmatzidis I.. Effects of heat stress on cognitive performance: the current state of knowledge. Int J Hyperth. 2003;19:355–372. [DOI] [PubMed] [Google Scholar]
- [2].Hancock PA, Ross JM, Szalma JL. A meta-analysis of performance response under thermal stressors. Hum Factors J Hum Factors Ergon Soc. 2007;49:851–877. [DOI] [PubMed] [Google Scholar]
- [3].Johnson RF, Kobrick JL. Psychological aspects of military performance in hot environments. In: Pandolf KB, Burr RE, Wenger CB, et al., editors. Medical aspects of harsh environments. Vol. 1. Houston TX: Department of the Army, Office of The Surgeon General, Borden Institute; 2002. p. 135–159. [Google Scholar]
- [4].Martin K, McLeod E, Périard J, et al. The impact of environmental stress on cognitive performance: a systematic review. Hum Factors. 2019;61:1205–1246. [DOI] [PubMed] [Google Scholar]
- [5].Gaoua N, Racinais S, Grantham J, et al. Alterations in cognitive performance during passive hyperthermia are task dependent. Int J Hyperth. 2011;27:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Malcolm RA, Cooper S, Folland JP, et al. Passive heat exposure alters perception and executive function. Front Physiol. 2018;9:585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Gaoua N, Grantham J, Racinais S, et al. Sensory displeasure reduces complex cognitive performance in the heat. J Environ Psychol. 2012;32:158–163. [Google Scholar]
- [8].Racinais S, Gaoua N, Grantham J. Hyperthermia impairs short-term memory and peripheral motor drive transmission. J Physiol. 2008;586:4751–4762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Ramsey JD, Kwon YG. Recommended alert limits for perceptual motor loss in hot environments. Int J Ind Ergon. 1992;9:245–257. [Google Scholar]
- [10].van Maanen L, van der Mijn R, van Beurden MHPH, et al. Core body temperature speeds up temporal processing and choice behavior under deadlines. Sci Rep. 2019;9:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Boehm U, Hawkins GE, Brown S, et al. Of monkeys and men: impatience in perceptual decision-making. Psychonomic Bull Rev. 2016;23(3):738–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].van Maanen L, Fontanesi L, Hawkins GE, et al. Striatal activation reflects urgency in perceptual decision making. Neuroimage. 2016;139:294–303. [DOI] [PubMed] [Google Scholar]
- [13].Miletić S, van Maanen L. Caution in decision-making under time pressure is mediated by timing ability. Cogn Psychol. 2019;110:16–29. [DOI] [PubMed] [Google Scholar]
- [14].Craig AB Jr., Dvorak M. Thermal regulation during water immersion. J Appl Physiol. 1966;21:1577–1585. [DOI] [PubMed] [Google Scholar]
- [15].Kononowicz TW, van Rijn H. Slow potentials in time estimation: the role of temporal accumulation and habituation. Front Integr Neurosci. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Macar F, Vidal F, Casini L. The supplementary motor area in motor and sensory timing: evidence from slow brain potential changes. Exp Brain Res. 1999;125:271–280. [DOI] [PubMed] [Google Scholar]
- [17].Domitrovich JW, Cuddy JS, Ruby BC. Core-temperature sensor ingestion timing and measurement variability. J Athl Train. 2010;45:594–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].van den Heuvel AMJ, Haberley BJ, Hoyle DJR, et al. The independent influences of heat strain and dehydration upon cognition. Eur J Appl Physiol. 2017;117:1025–1037. [DOI] [PubMed] [Google Scholar]
- [19].Nybo L, Rasmussen P, Sawka MN. Performance in the heat-physiological factors of importance for hyperthermia-induced fatigue. Compr Physiol. 2014. [DOI] [PubMed] [Google Scholar]
- [20].Piil JF, Lundbye-Jensen J, Trangmar SJ, et al. Performance in complex motor tasks deteriorates in hyperthermic humans. Temperature. 2017;4(4):420–428. doi: 10.1080/23328940.2017.1368877 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Bogacz R, Wagenmakers EJ, Forstmann BU, et al. The neural basis of the speed-accuracy tradeoff. Trends Neurosci. 2010;33:10–16. [DOI] [PubMed] [Google Scholar]
- [22].van Maanen L, Brown SD, Eichele T, et al. Neural correlates of trial-to-trial fluctuations in response caution. J Neurosci. 2011;31:17488–17495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Pilcher JJ. Nadler E, Busch C. Effects of hot and cold temperature exposure on performance: a meta-analytic review. Ergonomics, Taylor & Francis; 2010. [DOI] [PubMed] [Google Scholar]
- [24].Kissling LS, Akerman AP, Cotter JD. Heat-induced hypervolemia: does the mode of acclimation matter and what are the implications for performance at Tokyo 2020? Temperature. 2019;1–20. doi: 10.1080/23328940.2019.1653736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Gonzalez-Alonso J, Crandall CG, Johnson JM. The cardiovascular challenge of exercising in the heat J Physiol. 2008;586:45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Grandjean AC, Grandjean NR. Dehydration and Cognitive Performance J Am Coll Nutr. 2007;26:549S–554S. [DOI] [PubMed] [Google Scholar]
- [27].Piil JF, Lundbye-Jensen J, Christiansen L, et al. High prevalence of hypohydration in occupations with heat stress – Perspectives for performance in combined cognitive and motor tasks. PLoS One. 2018;13(10):e0205321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Tamm M, Jakobson A, Havik M, et al. The compression of perceived time in a hot environment depends on physiological and psychological factors. Q J Exp Psychol. 2014;67(1):197–208. [DOI] [PubMed] [Google Scholar]
- [29].Wearden JH, Penton-Voak IS. Feeling the Heat: Body Temperature and the Rate of Subjective Time, Revisited. Q J Exp Psychol Sect B. 1995;48(2):129–141. [DOI] [PubMed] [Google Scholar]
- [30].Hart SG, Staveland LE. Development of NASA-TLX (Task Load Index): Results of empirical and theoretical research. In Hancock PA, Meshkati N, editor.. Human Mental Workload. Elsevier Science Publishers B.V; 1988. p. 139–183. [Google Scholar]


