Abstract
The Payer Policy Review Committee of the American Academy of Sleep Medicine launched an initiative to assess the alignment between clinical practice guidelines and private payer medical policies. This article summarizes the importance of the initiative, details the scorecard development process, including an analysis of policy scores and subsequent revisions, and discusses the impact of the scorecards particularly as related to the scorecards on the clinical practice guideline for diagnosis of obstructive sleep apnea in adults. This initiative has increased communication and engagement among members of the Payer Policy Review Committee and private payers, creating opportunities to advocate on behalf of sleep medicine providers and patients with sleep disorders, encouraging payers to modify existing policies so that evidence-based care is provided to patients with sleep disorders.
Citation:
Kaplish N, D’Andrea L, Auger RR, Gay P, Jacobowitz O, Johnson K, Lance C, Licis A, Patil S, Summers M, Vohra KP, Abbasi-Feinberg F. Addressing gaps between payer policies and AASM clinical practice guidelines using scorecards. J Clin Sleep Med. 2020;16(5):811–815.
INTRODUCTION
The diagnosis of obstructive sleep apnea (OSA) requires objective testing by attended polysomnography (PSG) or a home sleep apnea test (HSAT), with the former recognized as the gold standard.1 In 2007, the American Academy of Sleep Medicine (AASM) published guidelines that recommended an HSAT only be used in conjunction with a comprehensive sleep evaluation in adult patients (≥ 18 years of age) at high risk for moderate to severe OSA.2 The same guidelines advised against an HSAT in children or adults > 65 years of age, due to a lack of sufficient supporting data. Additionally, because the determination of the apnea-hypopnea index is based upon recording time, rather than sleep time in an HSAT, and due to the fact that hypopneas are defined by desaturations, an HSAT was not recommended for the assessment of suspected mild OSA due to their propensity to underestimate OSA severity.1 Finally, given the risks of false negative results, PSG was recommended if a single HSAT failed to establish the suspected diagnosis.
Sleep medicine is affected by broad-scale changes in the health care climate of the United States. Insurers are creating cost containment measures that impact the delivery of patient care in all fields of medicine. HSAT usage has grown exponentially due to its lower health care utilization costs and increased accessibility in areas where PSG availability is limited.3,4 Concurrent with these trends, health care insurers established prior authorization processes and/or relationships with benefit management companies to facilitate implementation of HSAT coverage policies, which do not align with clinical practice guidelines. Resultant issues include insurers’ recommendations for an HSAT among patients at low OSA risk, requirements for multiple HSAT assessments prior to PSG approval, and/or requests for an HSAT prior to evaluations for primary disorders of hypersomnolence or among patients with comorbid medical conditions for whom PSG is considered mandatory, according to AASM guidelines. Persistent discrepancies between these guidelines and coverage policies have resulted in significant challenges for both clinicians and patients. Clinical care providers are tasked with the reconciliation of misaligned cost containment measures and clinical practice guidelines on an individual level, with potentially detrimental effects on health outcomes. The AASM recognizes these challenges and seeks to enact measures that preserve high quality medical care for sleep medicine patients.
The AASM has formed several committees to fulfill its mission of advancing sleep care and enhancing sleep health to improve lives. One such committee is the Payer Policy Review Committee (PPRC). The AASM commissioned the PPRC, composed of board-certified sleep medicine physicians, in 2015. The PPRC mandate was to develop and maintain resources that facilitate alignment of insurer’s sleep medicine policies with AASM guidelines. The PPRC addresses the challenges faced by the nearly 10,000 AASM accredited sleep centers and individual AASM members in providing medical care consistent with AASM clinical practice guidelines.
A significant area of focus of the PPRC is implementation of care for OSA. OSA is recognized as an important public health problem, affecting 14% of men and 5% of women.5 If left untreated, OSA increases the risk for hypertension, atrial fibrillation, heart failure, stroke, coronary artery disease, insulin resistance and all-cause mortality.6–9 Undiagnosed OSA is estimated to cost the United States health care system more than 100 billion dollars due to associations with comorbid diseases, lost productivity, and workplace and motor vehicle accidents.10 The importance of adequate assessment and treatment of OSA cannot be underestimated, but a challenge faced by clinical care providers pertains to prior authorization policies that limit implementation of best care practices as outlined in the clinical practice guidelines, negatively impacting the provision of high quality care.
The PPRC is developing scorecards as a systematic measure of payer adherence to clinical practice guidelines, scoring individual components of the clinical practice guideline and totaling those for an overall score. The scorecards are a communication tool through which the PPRC can act on behalf of AASM members and patients to achieve better overall agreement between payer policies and clinical practice guidelines. In a coordinated effort, the PPRC used scorecards to review and provide feedback on payer policies from different states and ascertain consistency with the clinical practice guideline for diagnostic testing of OSA in adults. The first scorecard developed by the PPRC pertains to an AASM clinical practice guideline, updated in 2017, on diagnostic testing for OSA in adults.1 The 2017 guideline recommends an HSAT only be performed in conjunction with a comprehensive sleep evaluation in adult patients (≥ 18 years of age) at increased risk for moderate to severe OSA, among other recommendations.1,2
This article summarizes how these scorecards were developed and the impact of the scorecards on payer policies for diagnostic testing of OSA in adults. Assessing efficacy is imperative for several reasons, one being refinement of scorecard development and implementation to achieve the greatest effect. Also, additional scorecards may be created to encompass other aspects of sleep medicine care. In addition, these scorecards may serve as a model for medical societies in other fields to replicate, if the scorecards are found to be impactful.
INITIAL SCORECARD DEVELOPMENT PROCESS
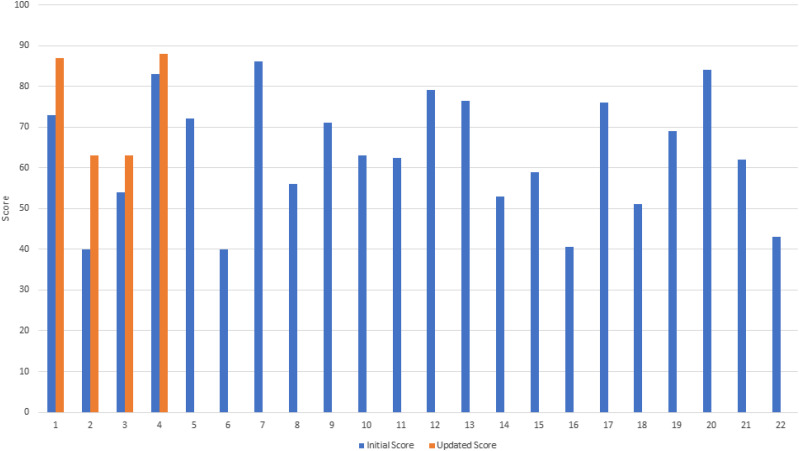
The committee developed a payer policy scorecard (Figure 1), to standardize scoring across insurance plans. The scorecard included 9 criteria based upon the recommendations in the AASM clinical practice guideline for diagnostic testing for OSA in adults,1 with specific emphasis on payers’ stipulations for HSAT and PSG. Various policies were subsequently reviewed and scored by the PPRC members, with monthly quorum discussions. Each criterion was assigned a value of either 10 or 15 points, based upon internal consensus, for a maximum total score of 100. A rationale section for each criterion within the scorecard was completed in order to provide justifications for point allocations. To standardize scoring, typical point subtractions were assigned to common omissions, such as not authorizing PSG to be used in patients with severe insomnia, and the requirement of performing 2 HSATs prior to approval of PSG. Many policies included referenced data sections in addition to the main policy section but, unless the latter specifically met scoring criteria, points were not given. Each committee member scored each policy. Once scores were finalized, an average score was generated and policies were given 1 to 5 stars (1 star [0–50 points], 2 stars [51–60 points], 3 stars [61–80 points], 4 stars [81–90 points], and 5 stars ([91–100 points]).
Figure 1. Diagnostic testing for obstructive sleep apnea payer policy scorecard.
AASM = American Academy of Sleep Medicine, HSAT = home sleep apnea test, OSA = obstructive sleep apnea, PSG = polysomnography.
Payer policies were identified by committee members and AASM staff through an environmental scan of publicly available plans related to diagnostic testing for OSA. The committee selected policies from different regions of the country to identify any regional or national coverage variations. Completed scorecards were sent to the insurer for feedback. If necessary, a teleconference was held between the chair/vice chair of the committee and the medical director of the affiliated insurance company to discuss the rationale for policy scoring. Some insurers subsequently made changes and returned revisions for rescoring by the PPRC. Once scores were finalized, they were submitted to the AASM Executive Committee or Board of Directors for approval before posting to the AASM website. In addition, a sample 5-star policy was developed by the committee to be used as both a template for insurers and as a resource for AASM members during their discussions with payers.
SCORECARD ANALYSIS
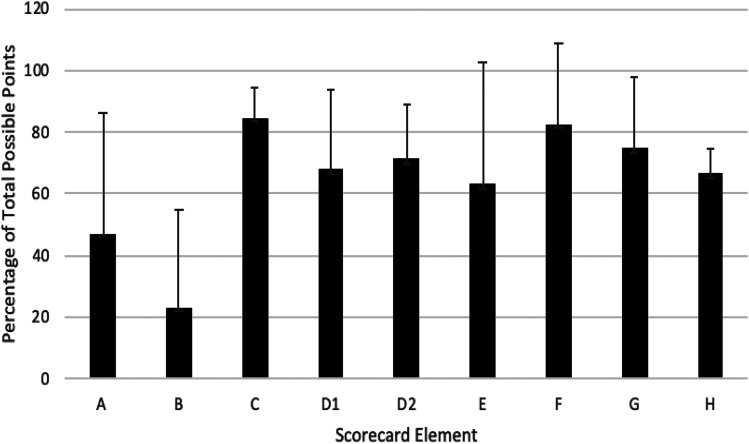
Policies for 22 payers were scored, 4 of which subsequently updated their policies and were then rescored. The average score of the 22 initial policies was 63.3 ± 14.8 points out of a total 100 points. Four received a 1-star rating, 5 a 2-star rating, 10 a 3-star rating, and 3 a 4-star rating. Following changes based upon the committee’s feedback, 4 revised policies increased on average by 12.8 ± 7.8 points with 1 policy moving from a 1-star to a 3-star rating, 1 from a 2-star to a 3-star rating, another from a 3-star to a 4-star rating and 1 remained at a 4-star rating (Figure 2).
Figure 2. Initial and updated overall policy scores.
Twenty-two insurance company’s sleep diagnostic testing policies were scored. Initial scores are indicated by the blue bars and the 4 companies with updated policies are indicated by the orange bars.
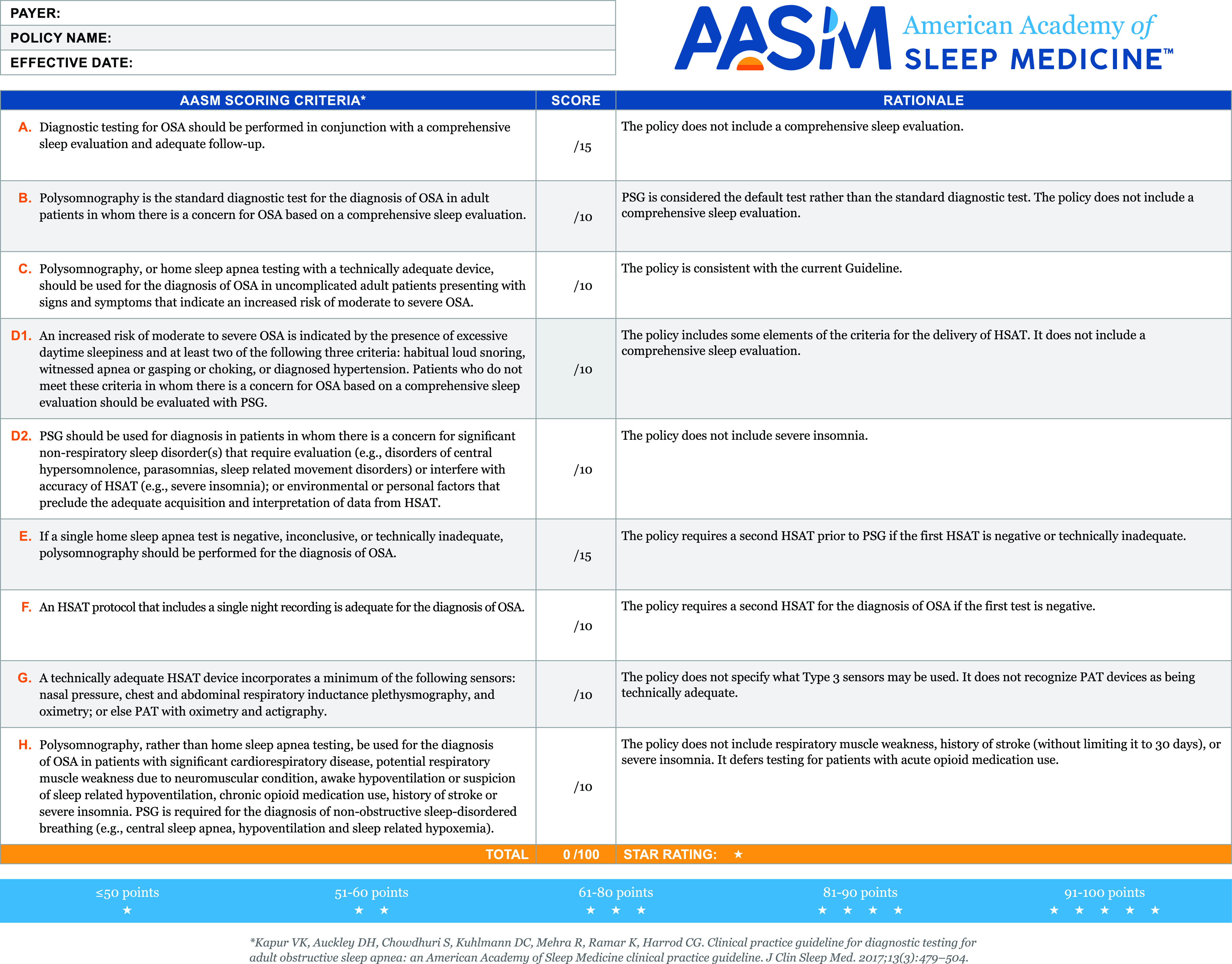
From the 22 initial policies scored, the average percent of total possible points for each of the 9 scorecard criteria ranged from 22.9–84.3%. The lowest scoring criteria were A, B and E, which focused on the need for a comprehensive sleep evaluation and follow-up, listing PSG as the standard diagnostic test for OSA and the need for a single HSAT prior to PSG, respectively (Figure 3).
Figure 3. Average percentage of total possible points achieved for each scorecard criteria element.
The average percentage of total possible points is represented since criteria A and E have 15 possible points and the other criteria have 10 possible points. Error bars represent the standard deviation of the average score.
The most common identified deficiencies were: (1) the lack of a requirement for a comprehensive sleep evaluation prior to diagnostic testing, (2) a failure to mention PSG as the standard diagnostic test for OSA, (3) the requirement of 2 failed HSATs before authorization for PSG, (4) the lack of inclusion of peripheral arterial tonometry with integrated actigraphy as a diagnostic option and (5) the failure to specify conditions best suited to an in-laboratory study rather than an HSAT (eg, severe insomnia, opioid use).
IMPACT OF SCORECARD DEVELOPMENT AND COMMUNICATION TO PAYERS
Guideline scorecards were created to evaluate the effectiveness of payer policies with respect to the provision of appropriate care for diagnostic sleep testing services. The intent was to encourage payers to adopt evidence-based policies that support patient safety and delivery of high quality care. Payers were notified of scores prior to their placement on the AASM website.
Publication of the scorecards has resulted in an important and ongoing dialogue between the AASM and payers. Of the 22 initial scorecards published, there has been a response from 7 affiliated payers, and 4 have revised their policies in a manner that improved scores upon rereview. Examples include 1 payer changing its policy so 2 HSATs are no longer required prior to PSG authorization. Another payer made substantial changes in their policy to include insomnia and opioid use as indications for PSG, rather than HSAT for diagnosis of OSA. Other changes by payers included changing language which referenced the need to rule out OSA by HSAT (versus PSG) prior to a narcolepsy evaluation and revising recommendations regarding the appropriateness of a PSG or HSAT that aligned more closely with the AASM guidelines. Those payers that enacted policy modifications that resulted in increased scores are large entities, and the committee believes the changes will have a widespread impact on patient care.
There were several limitations to the creation and review of scorecards. The scorecard was based on the OSA diagnostic testing clinical practice guideline and thus did not include criteria for diagnostic testing for other sleep disorders including, but not limited to, narcolepsy, periodic limb movement disorder, obesity hypoventilation and central sleep apnea. Moreover, the rating was based only on the written policy without knowledge of the insurance company’s compliance with their own stated policies. Additionally, the committee was unable to assess the ease of payers’ systems for obtaining authorization or peer review.
While the AASM continues to advocate for policy revisions that harmonize with clinical practice guidelines, the hope is that state sleep societies and individual sleep specialists will use the scorecards to advocate for necessary policy changes within their own states. To date, the published scorecards (https://aasm.org/advocacy/guideline-scorecards/) have been viewed by > 4,000 individuals with > 5,000 clicks on the webpage.
It has been educational to see how policies vary from state to state for the same payer. Ideally, as payers revise their policies to align with the clinical practice guideline, there will be more uniformity and all patients will be eligible to receive standardized, evidence-based care.
CONCLUSIONS
While clinicians aim to provide high quality care, payer policies do not always provide coverage for evidence-based diagnostic testing and treatment options. This presents challenges to providers as they try to implement clinical practice guidelines. The use of scorecards to evaluate the correspondence between clinical practice guidelines and payer policies is a promising tool to improve quality of care for patients with sleep disorders. The AASM PPRC encourages other medical specialties to adopt similar payer policy scorecard initiatives in order to highlight and communicate discrepancies between medical policies and evidence-based clinical practice guidelines to payers and encourage closer alignment between the two so that patients receive the highest quality of care.
DISCLOSURE STATEMENT
The authors constitute the 2017–2019 Payer Policy Review Committee of the AASM.
ACKNOWLEDGMENTS
The Payer Policy Review Committee thanks the AASM staff members who assisted with the development of this article.
REFERENCES
- 1.Kapur VK, Auckley DH, Chowdhuri S, et al. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med.. 2017;13(3):479–504. 10.5664/jcsm.6506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Collop NA, Anderson WM, Boehlecke B, et al. Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. Portable Monitoring Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med.. 2007;3(7):737–747. 10.5664/jcsm.27032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kakkar RK, Berry RB. Positive airway pressure treatment for obstructive sleep apnea. Chest.. 2007;132(3):1057–1072. 10.1378/chest.06-2432 [DOI] [PubMed] [Google Scholar]
- 4.Kapur V, Blough DK, Sandblom RE, et al. The medical cost of undiagnosed sleep apnea. Sleep.. 1999;22(6):749–755. 10.1093/sleep/22.6.749 [DOI] [PubMed] [Google Scholar]
- 5.Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol.. 2013;177(9):1006–1014. 10.1093/aje/kws342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc.. 2008;5(2):136–143. 10.1513/pats.200709-155MG [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fu Y, Xia Y, Yi H, Xu H, Guan J, Yin S. Meta-analysis of all-cause and cardiovascular mortality in obstructive sleep apnea with or without continuous positive airway pressure treatment. Sleep Breath.. 2017;21(1):181–189. 10.1007/s11325-016-1393-1 [DOI] [PubMed] [Google Scholar]
- 8.Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep.. 2008;31(8):1071–1078. [PMC free article] [PubMed] [Google Scholar]
- 9.Budhiraja R, Budhiraja P, Quan SF. Sleep-disordered breathing and cardiovascular disorders. Respir Care.. 2010;55(10):1322–1332, discussion 30-32. [PMC free article] [PubMed] [Google Scholar]
- 10.Frost & Sullivan, American Academy of Sleep Medicine . Hidden health crisis costing America billions. Underdiagnosing and undertreating obstructive sleep apnea draining healthcare system. https://www.aasm.org/sleep-apnea-economic-impact.aspx. Published 2016. Accessed February 28, 2020.