Abstract
Context
Coronavirus Disease 2019 (COVID-19) put a spotlight on focused cardiac ultrasound (FoCUS). However, the spectra of cardiac disease, and the resources available for investigation vary internationally. The applicability of FoCUS to internal medicine (IM) and critical care medicine (CCM) practice in Saudi Arabia and their current use of FoCUS are unknown.
Aims
To determine the applicability of FoCUS to IM and CCM practice in Saudi Arabia and quantify the residents’ current proficiency, accreditation and use of FoCUS.
Methods
A questionnaire was distributed to the residents in IM and CCM at our institution to determine their proficiency, use of FoCUS, and perceptions of its applicability.
Results
In total, 110 residents (IM 100/108; CCM 10/10) participated (Response rate 93.2%) and reported that FoCUS was very applicable to their practice, most specifically for pericardial effusion, right heart strain, and left ventricular function. Two IM residents had received postgraduate training, ten used FoCUS regularly, none were accredited and overall self-reported proficiency was poor. In contrast all CCM residents had received postgraduate training and reported regular use of FoCUS. Two were accredited.
Conclusions
Whilst FoCUS is applicable to IM practice in Saudi Arabia, significant skills gaps exist. The skills gap in CCM is lower but unaccredited practice is common. Our residents’ responses were similar to those from Canada. Thus, international standardization of FoCUS training could be considered.
Keywords: Cardiac ultrasound, Echocardiography, Education needs assessment, Curriculum development, Internal medicine, Critical care medicine
1. Introduction
Reducing the risk of Coronavirus Disease 2019 (COVID-19) to healthcare professionals is of utmost importance. So, consensus statements recommend the use of portable devices, to perform focused cardiac ultrasound (FoCUS), instead of departmental transthoracic echocardiography (TTE) [2].
To the uninitiated, FoCUS is indistinguishable from bedside TTE. However, whilst FoCUS is a powerful adjunct to bedside clinical assessment, several important limitations distinguish it from TTE [3,4].
Performed by cardiologists and specialist sonographers; TTE is a comprehensive, advanced diagnostic test with a standardized protocol and rigorous accreditation standards for image acquisition and reporting [3,4]. In contrast, FoCUS is fast, limited scanning, often performed with pocket-sized devices. Healthcare providers with basic training in ultrasound can use FoCUS to answer specific questions in ‘real-time’ [3–5], expediting the management of unwell patients [3–5].
Although substantial evidence supports the clinical utility of FoCUS [5]; like TTE, FoCUS is operator dependent [3–5], and practitioners must be competent [3,4,6,7]. So, training to close gaps in learners’ knowledge and skills is therefore required to ensure safe, and effective use of FoCUS [7–9]. Adopting FoCUS, therefore, requires significant initial investment to acquire portable ultrasound devices and train providers.
An international consensus document on FoCUS training and accreditation for intensivists is available [3]. However, uptake of these recommendations has been poor. There is no equivalent international consensus for training and accrediting internists in FoCUS.
Several countries have developed their own curricula for physicians and intensivists [6,10–12]. However, the Saudi Commission for Health Specialties (SCFHS) does not, as yet, have a syllabus for FoCUS. As the resources available, and the spectra of cardiac diseases in the Middle East differs from that in other regions [13–15], FoCUS may not be applicable in Saudi Arabia. To justify training in FoCUS, its relevance to internists and intensivists practising in Saudi Arabia must be confirmed. Thus, a needs assessment is required [8,16], and the current use of FoCUS must be quantified.
Furthermore, for a post-graduate training program to be successful, residents’ opinions must be acknowledged [8,16]. Nothing is known of Saudi residents’ opinions on FoCUS, in terms of its relevance to their practice.
The aim of this study was to determine IM and CCM residents’ perceptions on the applicability of FoCUS and define the skills gap in Saudi Arabia.
2. Methods
2.1. Ethical approval
The institutional review board approved this study.
2.2. Study design
This cross-sectional survey of IM and CCM residents was performed at a Medical City in Saudi Arabia.
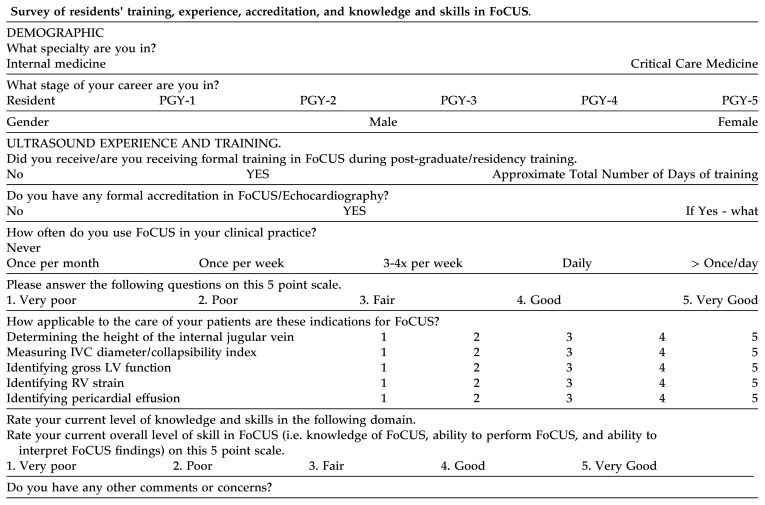
2.3. Survey development
A validated questionnaire to investigate FoCUS was derived from previous studies [8,17] describing applications of FoCUS [4,5] and the competencies required [6,10–12]. Three researchers with expertise in IM, CCM, TTE, FoCUS, and survey design (NM, MS, and RR) then developed the questionnaire in July 2019. The questionnaire had 4 sections:
Demographics (gender, specialty, postgraduate year of training)
Applicability of five diagnostic applications of FoCUS (i.e. a needs assessment). For each application, participants were asked: How applicable is the specified indication for FoCUS to your practice?
Proficiency in FoCUS. This section included a single self-reported question on knowledge of FoCUS and ability to interpret FoCUS findings.
Experience (postgraduate training, accreditation, and use of FoCUS). These questions were restricted to Y/N responses.
After ethical approval, the survey was piloted with four emergency medicine residents to obtain input on survey length, content, and clarity. No changes were required.
2.4. Participants
The setting of our study is a 1500 bed tertiary referral centre which hosts a new CCM residency in its third year and a large, well-established IM residency training program.
Based on the total number of IM residents (n = 108) and CCM residents (n = 10), assuming response distribution of 50%, it was estimated that the participation of 85 IM residents and 10 CCM residents would be required to obtain a 5% margin of error at a level of confidence of 95%.
All IM (postgraduate year [PGY] 1–4; n = 108) and CCM residents (postgraduate year [PGY] 1–3) at our institution during the academic year 10/2018–10/2019 were invited to participate. The final questionnaire was distributed in paper form to residents at various teaching activities in September 2019. Informed consent was obtained. No incentives were provided.
2.5. Study outcomes
The perceived applicability of indications for FoCUS in the practice of IM and CCM in Saudi Arabia was assessed using a 5-point Likert scale (1 very poor, 2 poor, 3 fair, 4 good, 5 very good). Self-reported proficiency in FoCUS was assessed on the same scale. Use of FoCUS was assessed using an incremental scale (never, once a month, once a week, daily, more than once daily). The skills gap in FoCUS was determined from the difference between residents’ perception of the applicability of FoCUS to their practice and their self-reported proficiency, and experience (i.e. training, accreditation and use of FoCUS).
2.6. Statistical analysis
Data were analysed using standard statistical techniques. All responses were included in the analysis. Responses of IM and CCM residents were analysed separately. The IM residents’ responses were stratified by PGY and gender. The number of CCM residents was too small to allow stratification of their responses.
To facilitate comparison of data, interval data, described as a 5 point Likert scale, were presented as both frequencies and mean ± SD, as described previously [8]. The data were compared using Student’s t-tests or analysis of variance (ANOVA) as appropriate. Categorical variables were compared using a Fisher exact test. All analyses were performed using Excel version 2016 (Microsoft, USA).
3. Results
3.1. Demographic data and response rates
Participants’ demographic data and response rates are shown in Table 1. One hundred of 108 (M 74/77; F 26/31) IM residents and 10 (PGY1 6, PGY2 2, PGY3 2) of 10 (M7; F3) CCM residents participated. The response rates were excellent (93.2% overall; CCM 100%; IM 92.6%). Although, the response rate of male participants (96%) was significantly higher than that of females (84%; χ2 4.8, P = 0.03); male and female IM residents’ responses were not significantly different.
Table 1.
Sample demographic data and response rates.
| Grade | N (RR % PGY) | Internal Medicine Gender N (RR, % Gender) |
Critical Care Medicine Gender N (RR, % Gender) |
||
|---|---|---|---|---|---|
|
|
|
||||
| Male | Female | Male | Female | ||
| PGY 1 | 31 (93.9%) | 22 (100%) | 9 (81.8%) | 4 (100%) | 2 (100%) |
| PGY 2 | 25 (89.3%) | 17 (100%) | 8 (72.7%) | 1 (100%) | 1 (100%) |
| PGY 3 | 25 (89.3%) | 23 (92.0%) | 2 (66.7%) | 2 (100%) | 0 |
| PGY 4 | 19 (100%) | 12 (100%) | 7 (100%) | - | - |
| Total | 100 (92.6%) | 74 (96.1%) | 26 (83.9%) | 7 (100%) | 3 (100%) |
The table presents the sample demographics and response rates. Response rates (RR) are stratified by specialty, postgraduate year (PGY) of training and gender. Data are presented as frequency and percentage of strata totals. N, number of responses.
3.2. Applicability of FoCUS in Saudi Arabia
The applicability of FoCUS to IM and CCM practice in Saudi Arabia is shown in Tables 2 and 3. Combining IM residents’ perceptions of the five indications for FoCUS studied suggested that the applicability of FoCUS was good (mean 4.3 ± SD 1.1; 403 responses (80.6%) were good or very good). However, there was a statistically significant difference between groups’ means as determined with one-way ANOVA (F (4,495) 15.3, P < 0.0001). The applicability of FoCUS for assessment of left ventricular (LV) function and detection of right ventricular (RV) strain and pericardial effusion were very high. The participants considered the assessment of inferior vena cava (IVC) diameter to be slightly less relevant. Although, measurement of jugular venous pulsation (JVP) height was considered least relevant, 58 residents rated its applicability as good or very good (mean 3.6 ± SD 1.4).
Table 2.
Residents’ perceptions of the applicability of FoCUS and their proficiency.
| Grade/Sex | Application of diagnostic focused cardiac ultrasound (Mean ± SD) | Knowledge & Skills (Mean ± SD) | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| JVP height | IVC diameter | LV function | RV strain | Pericardial effusion | FoCUS | |
| Internal Medicine | ||||||
| PGY 1 | 3.7 ± 1.1 | 4.1 ± 1.1 | 4.4 ± 1.1 | 4.3 ± 1.1 | 4.4 ± 0.9 | 1.7 ± 1.0 |
| PGY 2 | 3.6 ± 1.6 | 4.5 ± 0.8 | 4.5 ± 0.8 | 4.6 ± 0.6 | 4.6 ± 0.7 | 1.9 ± 1.2 |
| PGY 3 | 3.6 ± 1.4 | 4.5 ± 1.0 | 4.5 ± 0.8 | 4.3 ± 0.9 | 4.4 ± 1.0 | 2.1 ± 1.0 |
| PGY 4 | 3.4 ± 1.5 | 4.2 ± 1.0 | 4.5 ± 0.7 | 4.6 ± 0.6 | 4.9 ± 0.3 | 1.6 ± 1.0 |
| Male | 3.6 ± 1.4 | 4.3 ± 1.0 | 4.4 ± 0.9 | 4.4 ± 0.9 | 4.5 ± 0.9 | 1.7 ± 1.1 |
| Female | 3.4 ± 1.3 | 4.3 ± 0.9 | 4.5 ± 0.7 | 4.7 ± 0.6 | 4.6 ± 0.6 | 2.2 ± 1.1 |
| Overall | 3.6 ± 1.4 | 4.3 ± 1.0 | 4.5 ± 0.9 | 4.5 ± 0.9 | 4.5 ± 0.8 | 1.9 ± 1.1 |
| Critical Care Medicine | ||||||
| Overall | 4.5 ± 1.2 | 4.7 ± 0.5 | 4.9 ± 0.3 | 4.7 ± 0.5 | 4.9 ± 0.3 | 3.5 ± 0.8 |
This table presents residents’ perceptions on applicability of FoCUS to their clinical practice and their self-reported proficiency in FoCUS. Applicability and proficiency are rated on a 5 point Likert Scale (1, Very Poor; 2, Poor; 3, Fair; 4, Good and 5, Very Good). Data are stratified by specialty, postgraduate year of training (PGY) and gender and are presented as mean ± standard deviation.
Table 3.
Residents’ responses to questions on the applicability of FoCUS and their proficiency.
| Response (Likert scale) | Applicability of Indication for Focused Cardiac Ultrasound | Knowledge & Skills | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||
| JVP height | IVC diameter | LV function | RV strain | Pericardial effusion | FoCUS | |||||||
|
|
|
|
|
|
|
|||||||
| Specialty | IM | CCM | IM | CCM | IM | CCM | IM | CCM | IM | CCM | IM | CCM |
| Very Poor | 13 | 1 | 2 | 0 | 2 | 0 | 2 | 0 | 2 | 0 | 55 | 0 |
| Poor | 9 | 0 | 4 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 17 | 1 |
| Fair | 20 | 0 | 13 | 0 | 10 | 0 | 9 | 0 | 9 | 0 | 19 | 4 |
| Good | 22 | 1 | 23 | 3 | 24 | 1 | 26 | 3 | 21 | 1 | 7 | 4 |
| Very Good | 36 | 8 | 58 | 7 | 63 | 9 | 62 | 7 | 68 | 9 | 2 | 1 |
| Total | 100 | 10 | 100 | 10 | 100 | 10 | 100 | 10 | 100 | 10 | 100 | 10 |
This table presents residents’ responses to questions on the applicability of five indications for FoCUS and their self-reported proficiency in FoCUS. Applicability and proficiency are rated on a 5 point Likert Scale (1, Very Poor; 2, Poor; 3, Fair; 4, Good and 5, Very Good). IVC, inferior vena cava; JVP, jugular venous pulsation; LV, left ventricular; RV, right ventricular. Data are stratified by specialty and presented as frequencies.
There were no significant differences between IM residents’ and CCM residents’ perceptions. One CCM resident reported that the applicability of FoCUS for measuring JVP was very poor. Combining CCM residents’ perceptions of the five indications for FoCUS studied suggested that the applicability of FoCUS was very good (mean 4.7 ± SD 0.7; 49 responses (98%) were good or very good. There was no significant difference between groups.
3.3. Postgraduate training, accreditation, and use of FoCUS
Residents’ postgraduate training, accreditation and self-reported use of FoCUS in clinical practice are shown in Table 4. Whilst only two IM residents (2%; M 2) received postgraduate training, all ten CCM residents received postgraduate training in FoCUS (P < 0.00001).
Table 4.
Internal medicine residents’ training, accreditation, and use of FoCUS.
| Grade/Sex | Training (N, %; Male N) (N, %) |
Accreditation | Use of Focused Cardiac Ultrasound (N, %PGY; Male N) (N, %Sex) |
|||
|---|---|---|---|---|---|---|
|
|
|
|
|
|||
| Specialty | IM | CCM | IM | CCM | IM | CCM |
| PGY 1 | 3 (9.7%; M 2) | 6 (100%; M 4) | 0 | 2 | 0 (0%) | 6 (100%; M 4) |
| PGY 2 | 1 (4%; M 1) | 2 (100%; M 1) | 0 | 0 | 7 (28%; M 5) | 2 (100%; M 1) |
| PGY 3 | 2 (8%; M 2) | 2 (100%; M 2) | 0 | 0 | 2 (8%; M 2) | 2 (100%; M 2) |
| PGY 4 | 0 (0%) | - | 0 | - | 1 (5.3%; M 1) | - |
| Male | 5 (6.8%) | 7 (100%) | 0 | 1 | 8 (11%) | 7 (100%) |
| Female | 1 (3.8%) | 3 (100%) | 0 | 1 | 2 (7.7%) | 3 (100%) |
| Total | 6 (6%) | 10 (100%) | 0 | 2 | 10 (10%; M 8) | 10 (100%) |
This table presents residents’ training, accreditation and use of focused cardiac ultrasound. Data are presented as frequencies and percentages of strata totals. Responses are stratified by specialty, postgraduate year of training (PGY) and gender. M, male, N, number of respondents.
All CCM residents reported regular use of FoCUS. However only two had accreditation. The vast majority of IM residents (90; 90%) never use FoCUS. Although none had accreditation; ten (10%; F 2; M8) reported regular use of FoCUS in clinical practice. There was no statistically significant difference between males and females (χ2 0.37, P = 0.54) in their reported use of FoCUS. Of the IM residents who reported regular use of FoCUS, none had any postgraduate training. Neither of IM residents who had received postgraduate training used FoCUS in clinical practice.
3.4. Proficiency in FoCUS, and the skills gap
Self-reported proficiency in FoCUS is displayed in Tables 2 and 3. The IM residents generally reported that their proficiency in FoCUS was poor (mean 1.9 ± SD 1.1). Self-reported proficiency in FoCUS was significantly lower than the internists’ overall perception of its applicability (mean 4.3 ± SD 1.1; P < 0.0001), suggesting the presence of a skills gap.
The CCM residents reported that their proficiency in FoCUS was fair (mean 3.5 ± SD 0.8). This was significantly greater than that of the IM residents (P < 0.0001). However, a skills gap was still present. Self-reported proficiency in FoCUS was significantly lower than the intensivists’ overall perception of its applicability (mean 4.7 ± SD 0.7; P < 0.0001).
4. Discussion
Focused cardiac ultrasound is an accurate tool for defining causes of acute breathlessness (e.g., pericardial effusion, systolic heart failure, valve dysfunction) and can be used to tailor cardiovascular support with fluids, inotropes and vasopressors [4,5]. However, the spectra of cardiac diseases and facilities available within the Middle East varies significantly from that in other regions [13–15].
Justification for the high costs of developing a FoCUS training program requires confirmation that this skill is required by physicians in Saudi Arabia. The current study therefore describes IM and CCM residents’ perception of the applicability of five indications for FoCUS to their practice at a medical city in Saudi Arabia.
4.1. Residents’ perceptions of the applicability of FoCUS and their self-reported proficiency
The IM and CCM residents reported that FoCUS is very applicable to their practice (Tables 2 and 3). Assessment of LV function and detection of RV strain and pericardial effusion were thought to be highly applicable to IM and CCM practice.
Whilst CCM residents’ self-reported proficiency in FoCUS was fair, IM residents reported that their proficiency was poor.
4.2. Residents’ current level of training, accreditation and use of FoCUS
The current study describes the residents’ training, accreditation and experience in FoCUS (Table 4). As the survey was conducted toward the end of the academic year, PGY1 residents had almost completed one year of training. Our observations and recommendations are, therefore, also likely to be relevant to cardiology fellows, as the participating PGY4 IM residents were at the end of their residency.
A similar study in the UK, collated IM residents’ accreditation and experience in FoCUS. Use of FoCUS by internists in the UK is high. Smallwood et al. 2015 [17] reported that 81.1% of UK IM trainees use FoCUS, and 14.4% had accreditation in FoCUS or TTE. In comparison, a small proportion of the IM residents in Saudi Arabia use FoCUS (10%) and none are accredited. The assessment of the skills gap can guide educational interventions to resolve this discrepancy.
Although the CCM residency program is new, its trainers and trainees have embraced FoCUS. However, whilst all CCM residents at our institution received postgraduate training in FoCUS, and self-report regular use with fair proficiency, only two (20%) have accreditation.
4.3. Evaluation of the skills gap
A pragmatic measure of a skill gap is the difference between the self-reported ability to perform a skill and the perceived usefulness of that skill [8]. The IM residents’ self-reported proficiency in FoCUS (mean 1.9 ± SD 1.1; Table 2) was significantly lower than their overall perception of its applicability (mean 4.3 ± SD 1.1; P < 0.0001).
Furthermore, 90 IM residents reported that the applicability of FoCUS for identification of pericardial effusion and assessment of LV function was either good, or very good; but only ten (10%) use FoCUS. Of the ten IM residents who reported regular use of FoCUS, none had received postgraduate training. These observations suggest the presence of significant skills gaps in FoCUS in IM.
In contrast, the CCM residents’ self-reported proficiency in FoCUS was fair (mean 3.5 ± SD 0.8). This was significantly lower than their overall perception of its applicability (mean 4.7 ± SD 0.7; P < 0.0001). This suggests a small skills gap in FoCUS in CCM.
However, the unsupervised performance of FoCUS by partially trained residents raises governance issues and patient safety concerns. These must be addressed by a training program with formal processes for supervision, governance and accreditation.
4.4. Ability to provide FoCUS service
In the context of recent recommendations advocating the use of FoCUS rather than TTE [2], it is important to consider the feasibility of internists and intensivists providing this service.
In the UK, a pre-existing pool of skilled operators enabled effective use of FoCUS during the COVID-19 pandemic [1]. Whilst our data demonstrate that intensivists in Saudi Arabia do use FoCUS, the number of CCM residents is currently too small to deliver a sustainable service. It is therefore perturbing that the ability of IM residents to perform FoCUS is virtually non-existent. The COVID-19 pandemic heightened the urgency to develop FoCUS at our institution. The development of a FoCUS curriculum and training program is an integral component of the Department of Medicine’s preparation plan for a second wave of COVID-19.
4.5. Relevance of existing FoCUS training programs to Saudi Arabia
Our residents’ perceptions of the applicability of FoCUS and their skills gap (Table 2) are similar to those reported by Canadian IM residency programs [8]. This may be because, despite the regional differences in the epidemiology of pericardial effusion [14], for example; use of FoCUS to detect pericardial effusions is applicable worldwide. This observation suggests that international standardization of FoCUS training may be possible and that other countries’ curricula may be relevant in Saudi Arabia. However, to provide nationally recognised accreditation, any syllabus for FoCUS training must comply with SCFHS regulations.
4.6. Strengths and Limitations
The study has some limitations. Some of our data are self-reported. The accuracy of those data can be questioned [18]. However, the IM residents generally self-reported poor proficiency in FoCUS, whilst CCM residents generally self-reported fair proficiency. These data are consistent with our personal observations, and so are probably valid.
Our survey was administered to IM and CCM residents at only one institution in Riyadh, Saudi Arabia. So, it is possible that generalizability of the findings may be limited. The CCM residency training program, which began in 2016 at our institution, is relatively new. There are currently very few residents on the program, but their response rate was excellent.
Our institution hosts one of the largest IM residency programs in Saudi Arabia and the response rate was very high. Our program accepts interns trained at medical schools though out Saudi Arabia. Residency programs also include elective rotations during which our residents can choose placements in other hospitals throughout Saudi Arabia. Furthermore, residents have transferred into our program from other centers within Saudi Arabia. Thus, our participants’ views are therefore likely to represent IM residents throughout Saudi Arabia and indeed other countries with well-developed healthcare systems. Our observations and the sample’s views on FoCUS should therefore be taken into account when developing training programs to safely and effectively integrate FoCUS into the practice of IM.
4.7. Contribution to the pre-existing literature
These data provide evidence of the applicability of FoCUS to internists and intensivists practising in Saudi Arabia. It revealed that the IM residents in Saudi Arabia have significant a skills gap in FoCUS. A smaller skills gap is present in CCM. Training programs for FoCUS must aim to close the greatest skills gaps and provide instruction on the most relevant knowledge, and applications. Our observations can guide the development of a FoCUS curriculum. However, to ensure national recognition of credentialing, a FoCUS curriculum must comply with the regulations of the SCFHS.
Our survey demonstrated that the IM residency program at our institution currently cannot use FoCUS effectively. Whilst CCM residents do use FoCUS, their numbers are too small to provide a sustainable service. This is unfortunately likely to be true throughout the Kingdom.
5. Conclusion
Our data, suggest that FoCUS is highly applicable to the practice of IM and CCM in Saudi Arabia. However, significant skills gaps currently preclude the provision of a FoCUS service to IM patients at our institution. Despite regional differences in cardiac diseases, our residents’ responses on the applicability of FoCUS were similar to those of Canadian internists. So, international standardization of FoCUS training programs may be possible.
Abbreviations
- COVID-19
Coronavirus Disease 2019
- CCM
Critical Care Medicine
- FoCUS
Focused cardiac ultrasound
- IVC
Inferior vena cava
- IM
Internal Medicine
- JVP
Jugular venous pulsation
- LV
Left ventricular
- PGY
Postgraduate year
- RR
Response rate
- RV
Right ventricular
- SCFHS
Saudi Commission for Health Specialties
- SD
Standard deviation
- TTE
Transthoracic echocardiography
APPENDIX
Questionnaire used for the study of focused cardiac ultrasound (FoCUS) to medical practice in Saudi Arabia
Footnotes
Author contributions
Conception and design of Study: Naveed Mahmood, Mamdouh Souleymane, Rajkumar Rajendram. Literature review: Naveed Mahmood, Mamdouh Souleymane, Rajkumar Rajendram, Amro MT Ghazi, Mubashar Kharal, Mohammad AlQahtani. Acquisition of data: Mamdouh Souleymane, Rajkumar Rajendram, Amro MT Ghazi. Analysis and interpretation of data: Mamdouh Souleymane, Rajkumar Rajendram. Research investigation and analysis: Mamdouh Souleymane, Rajkumar Rajendram, Amro MT Ghazi. Data collection: Mamdouh Souleymane, Rajkumar Rajendram, Amro MT Ghazi. Data preparation and presentation: Mamdouh Souleymane, Rajkumar Rajendram. Supervision of the research: Rajkumar Rajendram, Mubashar Kharal, Mohammad AlQahtani. Research coordination and management: Rajkumar Rajendram.
Sources of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
None declared.
References
- 1.Smith MJ, Hayward SA, Innes SM, Miller ASC. Point-of-care lung ultrasound in patients with COVID-19 – a narrative review. Anaesthesia. 2020;75:1096–104. doi: 10.1111/anae.15082.anae.15082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ghazal S, Qaddoura F, Kinsara AK, Omran A, Atiyah M, Al Refae M, et al. Saudi Arabian Society Of Echocardiography Recommendations For Echocardiography Service During Corona Virus Disease 2019 (COVID-19) Outbreak. J Saudi Hear Assoc. 2020;32:1–5. doi: 10.37616/2212-5043.1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Price S, Via G, Sloth E, Guarracino F, Breitkreutz R, Catena E, et al. Echocardiography practice, training and accreditation in the intensive care: document for the World Interactive Network Focused on Critical Ultrasound (WINFOCUS) Cardiovasc Ultrasound. 2008;6:49. doi: 10.1186/1476-7120-6-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hall DP, Jordan H, Alam S, Gillies MA. The impact of focused echocardiography using the Focused Intensive Care Echo protocol on the management of critically ill patients, and comparison with full echocardiographic studies by BSE-accredited sonographers. J Intensive Care Soc. 2017;18:206–11. doi: 10.1177/1751143717700911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andersen GN, Haugen BO, Graven T, Salvesen O, Mjølstad OC, Dalen H. Feasibility and reliability of point-of-care pocket-sized echocardiography. Eur J Echocardiogr J Work Gr Echocardiogr Eur Soc Cardiol. 2011;12:665–70. doi: 10.1093/ejechocard/jer108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ma IWY, Arishenkoff S, Wiseman J, Desy J, Ailon J, Martin L, et al. Internal Medicine Point-of-Care Ultrasound Curriculum: Consensus Recommendations from the Canadian Internal Medicine Ultrasound (CIMUS) Group. J Gen Intern Med. 2017;32:1052–7. doi: 10.1007/s11606-017-4071-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pinto A, Pinto F, Faggian A, Rubini G, Caranci F, Macarini L, et al. Sources of error in emergency ultrasonography. Crit Ultrasound J. 2013;5:1–5. doi: 10.1186/2036-7902-5-S1-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Watson K, Lam A, Arishenkoff S, Halman S, Gibson NE, Yu J, et al. Point of care ultrasound training for internal medicine: A Canadian multi-centre learner needs assessment study. BMC Med Educ. 2018;18:1–8. doi: 10.1186/s12909-018-1326-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beaulieu Y, Laprise R, Drolet P, Thivierge RL, Serri K, Albert M, et al. Bedside ultrasound training using web-based e-learning and simulation early in the curriculum of residents. Crit Ultrasound J. 2015;7:1. doi: 10.1186/s13089-014-0018-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alber KF, Dachsel M, Gilmore A, Lawrenson P, Matsa R, Smallwood N, et al. Focused acute medicine ultrasound (FAMUs) Acute Med. 2018;17:164–7. [PubMed] [Google Scholar]
- 11.Brown GM, Otremba M, Devine LA, Gray C, Millington SJ, Ma IWY. Defining Competencies for Ultrasound-Guided Bedside Procedures: Consensus Opinions from Canadian Physicians. J Ultrasound Med. 2016;35:129–41. doi: 10.7863/ultra.15.01063. [DOI] [PubMed] [Google Scholar]
- 12.Smallwood N, Dachsel M, Matsa R, Tabiowo E, Walden A. Focused Acute Medicine Ultrasound (FAMUS) - point of care ultrasound for the Acute Medical Unit. Acute Med. 2016;15:193–6. [PubMed] [Google Scholar]
- 13.Waness A, El-Sameed YA, Mahboub B, Noshi M, Al-Jahdali H, Vats M, et al. Respiratory disorders in the Middle East: A review. Respirology. 2011;16:755–66. doi: 10.1111/j.1440-1843.2011.01988.x. [DOI] [PubMed] [Google Scholar]
- 14.Albugami S, Al-Husayni F, AlMalki A, Dumyati M, Zakri Y, AlRahimi J. Etiology of Pericardial Effusion and Outcomes Post Pericardiocentesis in the Western Region of Saudi Arabia: A Single-center Experience. Cureus. 2020;12:e6627. doi: 10.7759/cureus.6627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.GBD 2017 Saudi Arabia Collaborators. The burden of disease in Saudi Arabia 1990-2017: results from the Global Burden of Disease Study 2017. Lancet Planet Heal. 2020;4:e195–208. doi: 10.1016/S2542-5196(20)30075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kern D, Thomas P, Hughes M. Curriculum Development for Medical Education A Six-Step Approach. The Johns Hopkins University Press; 2009. [Google Scholar]
- 17.Smallwood N, Matsa R, Lawrenson P, Messenger J, Walden A. A UK wide survey on attitudes to point of care ultrasound training amongst clinicians working on the Acute Medical Unit. Acute Med. 2015;14:159–64. [PubMed] [Google Scholar]
- 18.Davis DA, Mazmanian PE, Fordis M, Van Harrison R, Thorpe KE, Perrier L. Accuracy of physician self-assessment compared with observed measures of competence: A systematic review. J Am Med Assoc. 2006;296:1094–102. doi: 10.1001/jama.296.9.1094. [DOI] [PubMed] [Google Scholar]