The emergence of coronavirus disease (COVID-19) has profoundly impacted many facets of clinical practice, including the need to adapt to rapidly changing hospital capacity and its impact on workflow processes. On this backdrop, the importance of point-of-care ultrasound (PoCUS) to patient care is increasingly recognized. Focused Cardiac Ultrasound (FoCUS), one of the most common applications of PoCUS, has been defined as goal-directed, problem-oriented, but time-sensitive and repeatable cardiac ultrasound examination that is simplified and limited in scope [1]. FoCUS is usually performed by clinicians at the point-of care, for early recognition and treatment of serious cardiac pathology [1]. The use of FoCUS allows for bedside identification and monitoring of changes in cardiac function; in addition, its performance by the treating clinician allows for the conservation of personal protective equipment [2]. Thus, in the era of COVID-19, for patients in whom cardiac ultrasound is indicated, a FoCUS-first strategy is recommended [2]. Despite these recommendations, many centers to date remain sub optimally poised to perform FoCUS.
Reflecting on the history of PoCUS may provide some insights for healthcare systems which have not, as yet, fully realized the benefits of this paradigm changing technology. First introduced in the 1950s, ultrasound was not used routinely until the 1970s [3]. And even then, early ultrasound machines were large and complex, requiring the patient to be immersed in water [3]. Over the years, technological advances allowing real-time scanning and miniaturization of the devices opened the door for widespread uptake. The first data on PoCUS use by emergency medicine physicians were published in 1988, and the use of PoCUS in the assessment of major trauma began shortly thereafter [3].
Whilst emergency medicine and obstetrics/gynecology were the first specialties to recognize and realize the benefits of PoCUS to frontline patient care, several other specialties rapidly followed suit. These include critical care, anesthesia, and to some extent, internal medicine and family medicine. However, in the case of internal medicine, the degree to which FoCUS has been integrated has been variable worldwide. In Europe, FoCUS is considered a core competency [4], while in Canada, FoCUS is recommended only as part of an expanded curriculum, not core [5]. Regardless of these curricular differences, what has emerged over time is the consistent recognition of the importance of PoCUS to the practice of clinical medicine by regulatory bodies and professional societies both on the national level (e.g. Society for Hospital Medicine, USA [6]) and the international level (e.g. WINFOCUS [7]). Reflecting on these variations in practices raises important questions about how effectively are these practice-changing bedside assessment tools currently being deployed in the Middle East?
To answer these questions, the current state of PoCUS training and skills amongst physicians and trainees in Saudi Arabia must be defined. In this issue, Mahmood and colleagues [8] provide unsettling answers by presenting the findings of an important study specifically addressing the current state of training and self-reported FoCUS skills amongst trainees in internal medicine and critical care medicine in Saudi Arabia (Fig. 1). ‘FoCUSing’ on residents at all stages of training. Mahmood and colleagues’ observations indicate that all critical care medicine trainees report regularly integrating FoCUS into their routine clinical practice, albeit often without formal accreditation [8]. In sharp contrast, internal medicine trainees, though interested in learning, by and large, are not actively engaged in either using or learning FoCUS. More alarming still is the finding that of the 10% of internal medicine trainees who are regularly using FoCUS, none received any formal training [8].
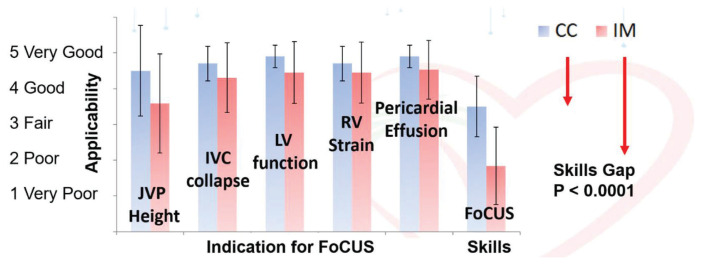
Fig. 1.
The applicability of FoCUS to internal medicine and critical care, the proficiency of internists and intensivists, and the skills gap in Saudi Arabia. This figure presents residents’ perceptions of the applicability of FoCUS to their clinical practice and their self-reported proficiency in FoCUS. The skills gap is calculated as the difference between the average applicability and the proficiency. Data stratified by specialty, are presented as mean ± standard deviation. Adapted from Mahmood et al., 2020 [8].
How shall educators act upon these results? Most importantly, medical educators need to be aware of the urgency to commit fully to FoCUS curriculum development efforts in the Middle East. Trained or not, learners are using FoCUS [8,9]. This phenomenon of using ultrasound without training is true not only of learners in Saudi Arabia. In a multi-center survey of practicing internists in North America, the number of practitioners who reported using ultrasound exceeded those who reported prior training [10].
Given the high operator-dependence of FoCUS skills, the dangers from untrained users cannot be ignored. Errors can range anywhere from clinical decisions made on uninterpretable images that are obtained by poor technique, to lack of appreciation of potential false positives and false negatives of any given finding, and lastly from inappropriate generalizations from existing literature. For example, learners may erroneously conclude that studies reporting high diagnostic accuracy in a trained population may imply that untrained learners can attain similar diagnostic accuracies. Thus, appropriate training, with oversight from qualified educators, is urgently needed.
It is noteworthy that FoCUS training gaps are not unique to Saudi Arabia, but exist elsewhere. In Canada, for example, despite a deliberate effort to develop a PoCUS curriculum and train their internal medicine residents in the relevant competencies [5], significant skill gaps persist [9]. The Canadian experience illustrates a key point: in building an ultrasound program ‘from the ground up,’ the importance of early engagement with the regulatory bodies overseeing postgraduate training cannot be underestimated. How could PoCUS curriculum design efforts be best executed in Saudi Arabia? First, for the curriculum to be successful, it is crucial that all the relevant stakeholders and regulatory bodies are fully engaged from the outset. Thus, an executive decision from the Saudi Commission for Health Specialties to incorporate ultrasound-related topics into individual specialty’s curriculum would be an important early step. In so doing, this would signal unambiguously the central role and competencies for FoCUS to the educational community. Second, each specialty should appoint a panel of experts with the competencies in PoCUS relevant to that specialty. This expert panel can then be tasked to develop a curriculum with clearly defined competencies and objectives applicable to their specialty. Third, three basic principles should be followed:
The curriculum content must be readily teachable and reliably learnable with sufficient practice. To ensure competency, trainee skills must also be assessed.
A clear scope of practice must be defined. Its use must follow clear indications (e.g. to answer focused questions or achieve a defined set of goals, such as assessing severe left and right ventricular systolic dysfunction, volume status, signs of cardiac tamponade, etc.).
Internists must be made fully aware of the limitations of FoCUS and appropriately recognize, where indicated, the need to seek expert opinion from cardiologists and/or obtain consultative echocardiograms. Limitations of FoCUS are many and stem from multiple sources, including technique, patient-related factors, equipment, false positives/false negatives, and clinical contextual factors. Recognizing these limitations of FoCUS, a low threshold to seek additional consultations is advised.
After curriculum development, the next challenge facing educators is curriculum implementation. At the hospital level, where all training is delivered, PoCUS and FoCUS champions should be appointed. These individuals must rise to the challenge of ensuring that proper equipment is readily available, regular didactic sessions are offered to the trainees, and most importantly, supervised hands-on training is provided.
It is imperative that faculty with sufficient theoretical, clinical, and practical knowledge and skills are engaged to deliver the requisite training. These fully trained, ideally accredited and institutionally credentialed in FoCUS individuals must be committed to training and assessing the competency of the learners. In the case of FoCUS, support of these individuals by cardiologists and specialist sonographers who are fully certified in formal echocardiography would be helpful. In addition, to provide quality control and maintain standards, infrastructure support with a secure imaging archiving system is also needed. One key barrier encountered in many programs is the lack of trained faculty [10]. Thus, providing institutional support for faculty to be trained and infrastructure for ongoing quality assurance processes should be a priority [10].
With the above in mind, it is important to recognize that the requisite components involved in curriculum implementation, while substantial, is not insurmountable. To facilitate curriculum implementation, Canadians have developed a set of education indicators and quality metrics to guide these efforts such that important aspects of a quality curriculum would not be neglected [11].
Mahmood and Colleagues provide clear evidence that the uptake of PoCUS and/or FoCUS by internal medicine trainees in the Middle East has been variable but that they are highly interested in learning [8]. Moving forward to improve patient outcomes, a firm commitment to curriculum development and implementation and a systematic approach to these educational efforts can readily rectify the situation. Learners in the Middle East are ready for it.
Footnotes
Authors’ contribution agreement
Dr Arif Hussain and Dr Irene W.Y. Ma conceived, wrote and edited the manuscript as invited authors for the Editorial and contributed equally.
Conflict of interest
A.H. is the serving president of WINFOCUS.
References
- 1.Via G, Hussain A, Wells M, Reardon R, ElBarbary M, Noble VE, et al. International evidence-based recommendations for focused cardiac ultrasound. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr. 2014;27:683.e1–683.e33. doi: 10.1016/j.echo.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 2.Johri AM, Galen B, Kirkpatrick JN, Lanspa M, Mulvagh S, Thamman R. ASE statement on point-of-care ultrasound during the 2019 novel coronavirus pandemic. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr. 2020;33:670–3. doi: 10.1016/j.echo.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kendall JL, Hoffenberg SR, Smith RS. History of emergency and critical care ultrasound: the evolution of a new imaging paradigm. Crit Care Med. 2007;35:S126–30. doi: 10.1097/01.CCM.0000260623.38982.83. [DOI] [PubMed] [Google Scholar]
- 4.Torres-Macho J, Aro T, Bruckner I, Cogliati C, Gilja OH, Gurghean A, et al. Point-of-care ultrasound in internal medicine: a position paper by the ultrasound working group of the European federation of internal medicine. Eur J Intern Med. 2020;73:67–71. doi: 10.1016/j.ejim.2019.11.016. [DOI] [PubMed] [Google Scholar]
- 5.Ma IWY, Arishenkoff S, Wiseman J, Desy J, Ailon J, Martin L, et al. Internal medicine point-of-care ultrasound curriculum: consensus recommendations from the Canadian internal medicine ultrasound (CIMUS) group. J Gen Intern Med. 2017;32:1052–7. doi: 10.1007/s11606-017-4071-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Soni NJ, Schnobrich D, Mathews BK, Tierney DM, Jensen TP, Dancel R, et al. Point-of-Care ultrasound for hospitalists: a position statement of the society of hospital medicine. J Hosp Med. 2019;14:E1–6. doi: 10.12788/jhm.3079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Neri L, Storti E, Lichtenstein D. Toward an ultrasound curriculum for critical care medicine. Crit Care Med. 2007;35:S290–304. doi: 10.1097/01.CCM.0000260680.16213.26. [DOI] [PubMed] [Google Scholar]
- 8.Mahmood N, Souleymane M, Rajendram R, Ghazi AMT, Kharal M, AlQahtani M. Focused cardiac ultrasound is applicable to internal medicine and critical care but skill gaps currently limit use. J Saudi Hear Assoc. 2020 doi: 10.37616/2212-5043.1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Watson K, Lam A, Arishenkoff S, Halman S, Gibson NE, Yu J, et al. Point of care ultrasound training for internal medicine: a Canadian multi-centre learner needs assessment study. BMC Med Educ. 2018;18:1–8. doi: 10.1186/s12909-018-1326-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wong J, Montague S, Wallace P, Negishi K, Liteplo A, Ringrose J, et al. Barriers to learning and using point-of-care ultrasound: a survey of practicing internists in six North American institutions. Ultrasound J. 2020;12:19. doi: 10.1186/s13089-020-00167-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ambasta A, Balan M, Mayette M, Goffi A, Mulvagh S, Buchanan B, et al. Education indicators for internal medicine point-of-care ultrasound: a consensus report from the Canadian internal medicine ultrasound (CIMUS) group. J Gen Intern Med. 2019;34:2123–9. doi: 10.1007/s11606-019-05124-1. [DOI] [PMC free article] [PubMed] [Google Scholar]