ABSTRACT
Human breast milk (HM) contains multiple bioactive substances determining its impact on children's health. Extracellular vesicles (EVs) are a heterogeneous group of secreted nanoparticles that are present in HM and may be partially responsible for its beneficial effects. The precise roles and content of EVs in HM remain largely unknown. To examine this, we performed a short narrative review on the literature focusing on HM EVs to contextualize the available data, followed by a scoping review of MEDLINE and Embase databases. We identified 424 nonduplicate citations with 19 original studies included. In this perspective, we summarize the evidence around HM EVs, highlight some theoretical considerations based on existing evidence, and provide an overview of some challenges associated with the complexity and heterogeneity of EV research. We consider how the existing data from HM studies conform to the minimal information for studies of EVs (MISEV) guidelines. Across the studies a variety of research methods were utilized involving both bench-based and translational methods, and a range of different EV contents were examined including RNA, proteins, and glycopeptides. We observed a variety of health outcomes in these studies, including allergy and atopy, necrotizing enterocolitis, and HIV. While some promising results have been demonstrated, the heterogeneity in outcomes of interest, methodological limitations, and relatively small number of studies in the field make comparison between studies or further translational work problematic. To date, no studies have examined normative values of HM EVs in a large, diverse population or with respect to potentially important influencing factors such as timing (hind- vs. foremilk), stage (colostrum vs. mature milk), and infant age (preterm vs. term), which makes extrapolation from bench or “basic” research impossible. Future research should focus on addressing the current inadequacies in the literature and utilize MISEV guidelines to inform study design.
Keywords: breast milk, extracellular vesicles, exosomes, human milk, microvesicles, nanovesicles
Introduction
Human breast milk (HM) is a unique body fluid containing a plethora of constituents with multiple functions (1). HM can be described as a combination of immunologically active factors, PUFAs, human milk oligosaccharides (HMOs), and a complex microbiome, which may potentially influence health outcomes in infancy and early childhood (1–4). Epidemiological studies of breastfeeding have shown apparent benefits for both the infant and mother (5–7). However, the exact HM constituents responsible for the protective effect remain unknown. Breastfeeding has not been consistently observed to be protective across the studies and some experts attribute this to the variation in the constituents of HM within and between individuals (1). Although PUFAs, HMOs, and the microbiome remain the main focus of HM research, recent studies suggest that HM extracellular vesicles (EVs) may also contribute to the short- and long-term benefits of breastfeeding (8–10).
EVs are a heterogeneous group of secreted nanoparticles, often referred to as distinct subsets, such as “exosomes,” “apoptosomes,” “oncosomes,” “microvesicles,” and “platelet dust,” with a wide range of roles in human health and disease (11, 12). Although originally believed to be derived from megakaryocytes and platelets, recent studies have demonstrated that they are produced by most cell types (12). EVs can be identified in various biological fluids, such as urine, blood, cerebrospinal fluid, and breast milk (13–15), and several studies have demonstrated that they play a role in both infectious and noncommunicable diseases (12, 16, 17).
Both human and animal milk have been examined for the presence and function of EVs (18–21). A number of these studies have had a strong focus on the possible impact of these particles on immune system and gastrointestinal tract development in infancy (8, 22–26), highlighting the role of mammalian breast-milk EVs in immunity, metabolism, and infant development (19, 27–32). Yet, methodological differences in approaches to EV analysis make it difficult to compare and combine the available data. Recently published minimal information for studies of EVs (MISEV) guidelines outlined a methodological framework for EV research to allow for reproducibility of results given the current technical limitations in examining EVs and their contents (11). The guidelines encourage the use of a standardized collection and processing method and utilizing multiple methods to describe the EVs of interest in both their structure and function.
A systematic evaluation of available data on EVs in HM is lacking. This Perspective aims to first evaluate the available evidence on the role of HM EVs on infant and child health defined by the authors as conditions or diseases that occur or first develop in the neonatal, infant, or childhood part of the human life cycle [e.g., necrotizing enterocolitis (NEC), bronchopulmonary dysplasia (BPD), and allergic diseases]. Second, we aimed to critically appraise the concordance of published data with the MISEV guidelines (11). Although approaches to EV assessment in HM are variable and existing evidence is very sparse, we reviewed available knowledge to highlight unmet needs for future research.
Methodological Approach
This Perspective is the result of a narrative review and subsequent systematically conducted scoping review. We followed the methods outlined in the PRISMA-ScR (Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews) (33). We conducted a comprehensive search in the bibliographic databases MEDLINE and Embase using both free-text and MeSH (medical subject heading) terms to identify bibliographic records involving HM and EVs. To reduce the potential for selection bias, titles, abstracts, and full-text articles were screened by 2 reviewers (DO and DD) independently for eligibility, and any disagreements were resolved through discussion involving additional reviewers (MRS and DM) until consensus was reached. A full description of the search strategy, study selection, and exclusion process may be found in Supplemental Figure 1. The search resulted in 598 titles, of which 19 studies were eligible for inclusion in the qualitative analysis. The heterogeneity of these studies, both in terms of their aims and methods, does not lend itself to any meta-analysis of their results. In the following sections we summarize and discuss the findings of these 19 studies into HM EVs, placing them within the broader context of EV research. Details of methodology used may be found in the Supplemental Methods.
Characteristics of the Studies Examining EVs in HM
A comparable number of studies used a translational approach (9/19) (8, 26, 34–40) and a descriptive or basic science approach (10/19) (22–25, 41–46). Most research was carried out in the United States (8 studies) or used US subjects (42%) (22, 23, 25, 26, 35, 36, 41, 45), 4 studied Swedish populations (21%) (8, 34, 42, 44), and the remaining studies took place in the Netherlands (43), China (24, 37), Israel (38), Japan (40), Poland (46), and Norway (39). While the number of participants and/or samples greatly varied between the studies, the sample size in most of the studies was relatively small, with between 1 and 61 subjects included (41, 44) and between 1 and 54 samples analyzed (41, 44). Eight studies did not provide details on the number of subjects or samples (25, 26, 34–36, 38, 42, 45).
Milk-collection time differed both within and between identified studies with timing of the “mature milk” varying from day 4 of life (8) to 11 months (40), and 4 studies had no description of the infant's age at the time of milk collection (27%) (26, 35, 36, 42). Colostrum was inconsistently defined, with 1 study collecting samples in the first 3 d of life (37), a second study describing milk collected during the first 4 d of life as colostrum (8), and a third describing HM collected at 1 to 3 mo as “early milk” (23) (Table 1).
TABLE 1.
Summary of characteristics of the studies and EVs1
| Study (reference) (year) | Location | Subjects, n | Number of samples | Collection procedure | Milk-collection times | Size of EVs, nm | Protein/RNA/glycosome content |
|---|---|---|---|---|---|---|---|
| Admyre et al. (8) (2007) | Sweden | 17 | 25 (8 samples colostrum, 17 samples mature milk) | Manual breast pump in sterile tubes | 4 d–6 mo | 50 | Protein: HLA-DR, CD63, CD81, HLA-ABC, CD40, CD54, CD80, lactadherin (MFG-E8). Unique: CD36, Butyrophilin and polymeric Ig receptor, MUC-1 |
| Batista et al. (41) (2011) | USA | 1 | 1 | Mechanical expression | 27 d | N.R. | Protein: CD63/CD81 used to determine "microvesicles"; glycome: no clear description of breast-milk glycome, focused on cell line glycomes |
| Golan-Gerstl et al. (38) (2017) | Israel | N.R. | N.R. | Manual breast pump in sterile tubes | 1 mo | N.R. | RNA: miR-148–3p,miR-6073,let-7a-5p,miR-30a-5p,miR-99a-5p,miR-146–5p,miR-200a,miR-21–5p,miR-30d |
| Kahn et al. (22) (2018) | USA | 20 | 10 term samples, 10 preterm samples (digested and undigested) | Manual breast pump in sterile tubes | 5 d–4 wk (pretermsamples collected 25–32 wk corrected gestational age) | N.R. | Protein: CD54/lactoferrin; RNA: 21 preterm specific miRNAs miR-22–3p most abundant, miR-148a-3p,miR-146a |
| Karlsson et al. (25) (2016) | USA/Sweden | 30 | 30 | Manual breast pump | 0–2 mo | 100 | Protein: CD63/CD9 used to determine EVs; RNA: lncRNAs: CRNDE,DANCR,GAS5,SRA1,ZFAS1 (90–100%) HOTAIRM1,NCBP2-AS2,OIP5-AS1,PRKCQ-AS1,SHNG8,TUG1 (50%) |
| Kosaka et al. (40) (2010) | Japan | 8 | 24 samples, different time points for each subject, 1 subject with no timings provided | N.R. | 4 d–11 mo | N.R. | Protein: CD63; RNA: miR-155,miR-181aandmiR-181b,miR-17,miR-92 cluster, miR-125b,miR-146b,miR-223,let-7I |
| Lässer et al. (42) (2011) | Sweden | N.R. | N.R. | N.R. | N.R. | 50–80 | Protein: CD9/CD63/CD81 used to determine EVs; RNA: mRNA qualitatively assessed but N.R., nil specific constructs |
| Leiferman et al. (45) (2019) | USA | 5 | N.R. | N.R. | 2–10 mo | 128.3–169.9 | Protein: CD63/CD9/Alix; RNA: miR-30d-5p,let-7b-5p,let-7a-5p,miR-125a-5p,miR-423–5p,miR-21–5p,miR-423–5p,let-7g-5p,let-7f-5p,miR-30a-5p,miR146b-5p |
| Liao et al. (23) (2017) | USA | 12 | 12 | Breast pump into sterile tubes with RNAse inhibitor | 1.5–8 mo | 30–120 | Protein: CD9/lactoferrin; RNA: 288 miRNA identified; noted immune active miRNA miR-22–3p,miR-181c-5p,miR-181a-5p,miR-16–5p,miR-148a-3p |
| Lukasik et al. (46) (2018) | Poland | 6 | 6 split into whole-milk and “exosome” fraction | Mechanical expression | 1.5–8 mo | N.R. | RNA: specifically examined 5 plant-based RNA constructs, 2 identified miR168a, miR156a |
| Martin et al. (26) (2018) | USA | N.R. | N.R. | Leftover samples of breast milk from NICU | N.R. | 74.6(26.6–122.6) | Protein: CD81/clathrin used to determine "exosomes" |
| Näslund et al. (34) (2014) | Sweden | N.R. | N.R. | Manual breast pump in sterile tubes | N.R. | N.R. | Protein: MUC-1, LFA-1 |
| Sims et al. (35) (2017) | USA | N.R. | N.R. | Leftover samples of breast milk from NICU | N.R. | 116.2 | Protein: CD9/CD63 |
| Sims et al. (36) (2018) | USA | N.R. | N.R. | Scavenged samples of breast milk from the NICU | N.R. | 94 ± 3.4 | Protein: CD81/clathrin |
| Simpson et al. (39) (2015) | Norway | 54 | 54 samples: 32 from probiotic arm; 22 from placebo arm | Collected into sterile tubes, method not reported | 3 mo | N.R. | RNA: miR-148a-3p,miR-22–3p,miR-30d-5p,let-7b-5p, and miR-200a-3p |
| Torregrosa Paredes et al. (44) (2014) | Sweden | 61 | 22 paired samples; 47 comparing impact of anthroposophic lifestyle (8 of which paired samples) | Manual breast pump in sterile tubes | Early: days 3–8; late: 2 mo | N.R. | Protein: early: high HLA-DR, low HLA-ABC, MUC-1 higher in sensitized vs. nonsensitized, MUC-1 lower in anthroposophic vs. nonanthroposophic, high CD63 anthroposophic |
| van Herwijnen et al. (43) (2016) | Netherlands | 7 | 7 (10–35 mL) | Breast pump mixed and 10–50 mL aliquoted | 3–9 mo | N.R. (sucrose density) | Protein: unique to this study: OLAH (oleal acp hydrolase), parathyroid hormone–related protein, MPZL1, ehd3, 3331 unique proteins total |
| Wang et al. (37) (2019) | China | N.R. | N.R. | N.R. | N.R. | 50–100 | Protein: CD9/CD63, different expression of 70 peptides between preterm and term EVs |
| Zhou et al. (24) (2012) | China | 4 | 4 (20–50 mL) | Manual breast pumps in sterile tubes | 60 d | N.R. | RNA: miR-148–3p (most common and with TGIF2, PXR, DNMT3B as known targets), miR-30b-5p (immunosuppression), miR-182–5p,miR-200a-3p, let-7 family(let-7f-1–5p, let-7f-2-5p,let-7a-2–5p, and let-7a-3–5p) |
1CD, cluster of differentiation; CRNDE, colorectal neoplasia differentially expressed; DANCR, differentiation antagonizing non-protein coding RNA; EV, extracellular vesicle; GAS5, growth arrest-specific 5; HLA, human leukocyte antigen; miR, microRNA; MUC-1, mucin 1 cell surface–associated; NICU, neonatal intensive care unit; N.R., not reported; SRA1, steroid receptor RNA activator 1; ZFAS1, ZNFX1 antisense RNA 1.
Mechanical expression or expression into sterile tubes using a breast pump were the most commonly described methods of sample collection (8, 22–25, 34, 38, 41, 44, 46). Details on type of breast pump used were not provided in any of the above studies. Other methods included utilizing remaining expressed milk following feeding from neonatal intensive care (26, 35–37) (Table 1). Substantial variation in the size of EVs in HM samples collected using the same methodology in the same clinical settings was reported in some studies (26, 35, 36) (Table 1). A single study described the timing of milk collection as “mid-stream” (46). No differentiation was made on any of the studies between foremilk or hindmilk.
Overall, we also observed a wide range of outcomes considered across these studies. Two studies examined digestion survival of EVs (22,23). A small number of studies examined atopy specifically (39, 44), with 3 studies examining HIV transmission with conflicting results (34–36). While many researchers examined predictive immune-regulatory RNAs in breast-milk–derived EVs (8, 22–25, 38, 42), only a single study on this topic demonstrated an effect of these EVs in a cell culture model (8).
Challenges in Characterizing and Studying EVs
Similar to other areas, the field of EV biology is subject to rapid change where evolving technologies and terminologies make comparison between studies difficult (11). Analysis of EVs and their contents is inherently difficult as their small size means their contents can become dilute relative to the surrounding fluid. While several studies included in this review were cognizant of this, many used only a single method of confirming that the contents they described were truly EV-derived [e.g., cluster of differentiation (CD) 63 fractions of HM] (40). As described, the MISEV guidelines provide us with useful advice about how to approach EV research. While many of the articles we identified were published before the most recent version of these guidelines, we considered the recommendation of the MISEV guidelines as we reviewed the studies characterizing HM EV contents, their capacity to survive digestion, as well as their potential role in allergic and other immunological outcomes, preterm infants, and NEC, and in the context of future therapeutics.
Studies Characterizing HM EV Content
We identified 10 papers that characterized the nucleomic, proteomic, or glycomic contents of HM EVs. However, there was heterogeneity in the techniques used to isolate EVs, as well as how they were characterized (Supplemental Table 1). The details of the studies’ methodologies are outlined in brief as we consider this information useful for any potential future EV research.
Ribonucleic Acids in EVs
EVs are enriched with microRNAs (miRNAs), which are short nucleic acids that are involved in post-transcriptional gene regulation (47). miRNAs have been shown to be very stable in HM despite the prevalence of ribonucleases (40, 48). The stability or concentration of miRNAs has been shown to persist even after HM was subjected to extreme temperature and pH changes, multiple freeze-thaw cycles, and extended storage (40, 49, 50). EVs confer protection by enclosing miRNAs and preventing ribonuclease degradation, thus enabling cell-to-cell communication (51, 52). Through our search, we found 5 studies that investigated the general RNA content of EVs (25, 38, 40, 42, 46). Another 5 papers considered the RNA content of HM EVs in association with digestion (22–24), allergic outcomes (39, 44), and preterm infants (22). These papers are described in more detail in later sections.
Lässer et al. (42) examined EVs in saliva, plasma, and breast milk. This study concluded that breast-milk EVs contain RNA, while not defining which specific RNA constructs were involved. As per MISEV 2018 guidelines, authors assessed EVs using multiple methodologies, including electron microscopy, flow cytometry, and Western blot (11). They also investigated the ability of HM EVs to be taken up by recipient cells (cultured human macrophages) using fluorescent labels (42). RNA content of HM-derived EVs was examined further by Karlsson et al. (25) who assessed long noncoding RNAs and identified a range of long noncoding RNAs implicated in the immune system [e.g., growth arrest-specific 5 (GAS5), ZNFX1 antisense RNA 1 (ZFAS1), steroid receptor RNA activator 1 (SRA1), and differentiation antagonizing non-protein coding RNA (DANCR)] and metabolism [e.g., GAS5, SRA1, colorectal neoplasia differentially expressed (CRNDE)] (Table 1). This study demonstrated a robust characterization of EV content utilizing electron microscopy, with labeling using anti-CD63/CD9 and nanoparticle tracking analysis used in addition to a commercially available EV isolation kit (25). Kosaka et al. (40) used anti-CD63 antibody–coated magnetic beads to extract EVs. Although the study did not demonstrate similar rigor when defining EV population, high expression levels of immune-related miRNAs were observed in the CD63-positive fraction during first 6 mo of lactation. The authors reported HM miRNAs being stable even upon acidic (pH 1) solution treatment. The presence of microRNA (miR)-181a and miR-17 in a CD63-positive fraction of milk supported the presence of EVs as delivery vehicles (40). While the exact functions of these HM EVs are largely unknown, it appears that miRNA in HM EVs are reasonably conserved with overlapping miRNA profiles found across different human populations and mammalian species.
Looking to the animal world, existing data suggest that bovine-milk EVs are enriched in miRNAs that are involved in both the adaptive and innate immune responses (53). Porcine-milk EV–associated miRNAs are also thought to target genes within immune system, metabolism, and development, including through members of the let-7 family, miR-181a and miR-320 (19). HM EVs and HM-associated miRNAs may also play a role in the regulation of metabolism. Although this possibility is poorly understood in humans, evidence for the role of mammalian-milk EVs and metabolism in other mammals is better established (18, 23). For instance, porcine EVs contain miRNAs associated with regulation of key metabolic pathways including the citrate cycle and glycerophospholipid metabolism (19). Both rat and mouse models showed differences in muscle physiology in those that received an oral gavage of EVs that were RNA sufficient versus those treated with RNA-depleted EVs (30, 54). Some mechanistic evidence was also found to support a role of EV-associated miRNAs in the regulation of the mammalian target of rapamycin complex (mTORC) pathway, a key regulator of both growth and development (55). Additionally, bovine-milk EVs have been shown to survive in vitro digestion (56), suggesting they can survive the transit through the intestinal tract and deliver their various protein and nucleic acid contents.
It has also been speculated that exogenous dietary miRNAs could be transferred via breast milk in addition to the mother's endogenous miRNAs. Lukasik et al. (46) isolated EVs using an EV precipitation solution with no other specific methodology used to characterize EVs. Two of the plant food–derived miRNAs were present in both whole milk and the EV fraction of HM (miR-156a,miR-168a), although no significant difference in expression was found between vegetarian and nonvegetarian mothers in the EV fraction. Leiferman et al. (54) examined not only the stability of HM EVs in storage but also set out to identify miRNA profiles in both HM and infant formula. While successfully demonstrating the presence of miRNA in HM EVs, they could not replicate this with infant formula. They suggested that EV-like particles in formula milk represent casein micelles. It is also possible that miRNAs are depleted during the processing of cow milk to infant formula.
Proteins in HM EVs
Using proteomics analysis of HM EVs, van Herwijnen et al. (43) revealed >600 proteins not previously detected in HM. While non-EV milk proteins are involved in metabolism and the “immune response,” EV milk proteins were associated with signal transduction, controlling inflammatory signaling pathways, suggesting that EVs could support the newborn's gut and immune system (43). In particular, many HM EV proteins are associated with the “cytoskeleton” and “plasma membrane.” This is the only study to date that has used a high-throughput method to assess the protein content of HM EVs, with other studies analyzing specific proteins or surface markers in association with digestion or infant outcomes. This is also the case for animal studies where, for example, bovine-milk EVs have been found to contain transforming growth factor β (TGF-β), a cytokine known for its importance in both mucosal barrier formation and T-cell regulation promoting a T-helper 17 (Th17) phenotype (57).
HM EVs and Digestion Survival
Three studies provided evidence for gastric and pancreatic digestion survival of miRNA and protein cargos within EVs in vitro, supporting the hypothesis that intact EV cargos are delivered to intestinal cells where they may elicit their functions (22–24). Liao et al. (23) and Kahn et al. (22) demonstrated that EVs can survive gastric and pancreatic digestion while preserving their miRNA and protein cargos. Zhou et al. (24) provided evidence of miRNA cargo preservation after treatment with RNAse, multiple freeze-thaw cycles, and incubation at 100°C. The miRNA cargos identified in all 3 studies were predominantly immune-associated, with a good agreement between the authors (22–24). Liao et al. (23) also characterized cargo at different stages of lactation, providing exosomes and miRNA profile for “early,” “mid,” and “late” lactation, and showed significant variation in exosome concentrations and miRNA counts with the relative abundance of miRNAs changing according to timing, and further validating the importance of timing in breast-milk composition. These findings suggest the physiological relevance of miRNA and protein readings in undigested HM (22, 23). However, the physiological concentration of HM EVs remains largely unknown, with only 1 study identifying the concentration of EVs per milliliter in a range of HM (23). Further studies pertaining to EV concentrations would benefit future research and allow for design of better dose–response studies to examine whether an average infant ingests sufficient quantities of these particles to generate the responses demonstrated in experiments to date.
HM EVs’ Role in Allergic and Immunological Outcomes
HM has been shown to play a role in protection from upper respiratory tract, ear, and gastrointestinal infection, and is thought to have longer lasting effects on the development of the immune system. The role of EVs in these outcomes has been recently appreciated. For example, Admyre et al. (8) studied the role of HM EVs in immunomodulation. Differential ultracentrifugation was utilized to enrich a sample of HM EVs, described in the paper as “exosome-like particles.” The EVs were analyzed using electron microscopy and flow cytometry. Trypsinization of EVs followed by Western blots demonstrated EV markers human leukocyte antigen–DR isotype (HLA-DR), heat shock cognate (HSC) 70, and CD81. This was further confirmed by flow cytometry; interestingly, HLA-DR was higher in “colostrum derived” (0–4 d of life) EVs than in “mature milk.” Additionally, proteomics analysis identified additional proteins [e.g., lactadherin, mucin 1 cell surface–associated (MUC-1)] and confirmed EV markers such as CD81, HSC, and major histocompatibility complex II. Finally, the function of EVs was assessed by an in vitro assay using both autologous and allogeneic maternally derived peripheral blood mononuclear cells (PBMCs) by co-culturing with HM EVs for 4 d. This showed a reduction in IL-2, IFN-γ, and TNF-α and an increase in IL-5 expression in a concentration-dependent manner, with 500 μg/mL (0.5 g/L) of EVs producing significant changes in all 4 of these cytokines and 50 μg/mL (0.05 g/L) of EVs resulted in a statistically significant increase only in IL-5. In the case of the changes seen with 0.5 g EVs/L, it is unclear if this corresponds to physiologically relevant concentrations of EVs. In another study, Liao et al. (23) found that exosome concentrations in 8 breast-milk samples ranged from 0.06 g/L to 0.31 g/L of EVs. As such, the increased IL-5 production by PBMCs incubated with 0.05 g/L of EVs is probably physiologically relevant, but cytokine changes after incubation with 0.5 g/L of EVs are unlikely to occur physiologically. Additionally, regulatory T-cell (Treg) analysis with allogeneic adult PBMCs alone demonstrated an increase in forkhead box P3+ (FOXP3+) cells, a key transcription factor involved in the expression of the Treg and anti-inflammatory phenotype (8, 58) in the presence of EVs. Nevertheless, small sample size along with filtration technique using 0.45-μm pores that could allow cell debris passage into the supernatant could have yielded unrealistic EV concentrations, so the inferred physiological relevance remains questionable. Additionally, these findings represent the effects observed when PBMCs are incubated with EVs in concentrations found within breast milk. The HM EV concentration in an infant's circulation would be substantially lower and therefore it is uncertain whether there would be sufficient concentrations to exert similar effects on infant PBMCs.
Two large cohorts of patients were examined, 1 set from the Assessment of Lifestyle and Allergic Disease During INfancy (ALADDIN) study and the other from the Probiotics in the Prevention of Allergy among Children in Trondheim (ProPACT) trial, both of which examined atopy and allergic phenotypes in the context of breastfeeding and breast-milk–derived EVs (39, 44). This concept has good mechanistic basis given what has been described in other included literature of HM EVs inducing a Treg phenotype.
Torregrosa Paredes et al. (44) explored the following 2 questions using samples from the ALADDIN cohort: 1) does maternal lifestyle and sensitization affect HM EV expression profile and 2) does the HM EV profile change from “early” to “mature” milk? They found that EV phenotype changed in “early” (day 3–8) versus “mature” (2 mo) milk with high HLA-DR and low HLA-A,B,C expression in early samples versus mature samples. Maternal lifestyle was found to be associated with EV expression in mothers following a lifestyle characterized by the authors as “anthroposophic” (characterized by home deliveries, organic diet, and reduced use of medications). Women characterized by an anthroposophic lifestyle had significantly lower mucin (MUC-1) expression on their HLA-DR–enriched milk exosomes. The identification of MUC-1 associated with HM EVs (8, 44) is particularly interesting given these proteins were previously described to prevent certain strains of viral and bacterial gastroenteritis (59, 60). This also reflects epidemiological data that show lower rates of gastroenteritis in breastfed infants (7). Finally, Torregrosa Paredes et al. (44) also reported an association between the immunological composition of EVs in mature milk and allergic sensitization at 2 y of age, although these results should be interpreted with caution due to the small sample size (44). In the second study, Simpson et al. (39) used samples from ProPACT, a randomized controlled trial studying the effect of maternal probiotic use on HM miRNAs and their potential role in atopic dermatitis development prevention. Small RNA-seq of the EV-enriched HM samples did not demonstrate statistically significant differences between the probiotic-treated group and placebo group or those with atopic dermatitis versus no atopic dermatitis.
Although both studies demonstrated primarily negative results, failing to identify a strong effect of HM-derived EVs on atopy and allergy (39, 44), the outcomes are thought provoking. This may be due to the modest effect size of EVs in atopy and allergy given what is known of the multifactorial pathogenesis of these conditions to date (61). Currently available information does not conclusively determine if EVs are beneficial in protection from infections, allergic outcomes, or other immunological diseases. A large, multicenter prospective study would likely be required to achieve the desired power to show the individual role of breast-milk EVs on the outcome of an atopic phenotype.
HM EVs and HIV
Three papers assessing the role of HM EVs in HIV transmission were identified; however, they yielded contradictory conclusions (34–36). Näslund et al. (34) demonstrated that EVs derived from monocyte-derived dendritic cells (MDDCs) of healthy donors, but not EVs derived from their plasma, inhibited HIV-1 infection if they were preincubated with HM EVs. Furthermore, co-culture of preincubated MDDCs with HM exosomes and CD4− T cells showed prevention of HIV transfer from MDDCs to CD4+ T cells. The authors suggested that HM-derived EVs may provide protection against vertical transmission of HIV infection (34). However, Sims et al. (35) found an enhanced HIV infection when treated with HM-derived EVs and demonstrated that HIV utilized exosomes entering into human immune cells. In a follow-up study, Sims et al. (36) found that treating cells with a CD9 antibody prevented augmentation of HIV-1 entry into cells in the presence of HM EVs, indicating this process is tetraspanin dependent.
Possible reasons for the contradictory data could be differences in measurement of infection—that is, the use of virus-produced luciferase versus protein markers and the direct inoculation of T-cell–like culture in the study by the Sims group versus the use of MDDC co-culture in the paper by the Näslund group. Similarly, differences in the individual milk samples collected, with Näslund et al. (34) recruiting a set of volunteers versus samples collected from remnants after feeding in the neonatal intensive care unit by Sims et al.’s group. Additionally, Sims et al. (36) demonstrated that the increased infection of cells was abrogated when tetraspanins (namely CD9) were blocked using an antibody. While this gives a mechanistic basis for the role of EVs generally in HIV transmission, the role of HM EVs in vertical transmission of HIV has not yet been conclusively answered to date. Moreover, the aforementioned studies have all used HM from HIV-negative donors.
Extremely limited data on HM EV glycome, the collection of carbohydrates on the membrane surface, exist. They come from a study investigating a single sample and from only 1 individual (41). While establishing that the glycoprotein coating of biofluid and cell culture–derived EVs was a mixture of conserved moieties and parent cell–derived carbohydrates, they were unable to establish a role for these protein–carbohydrate complexes in human health, nor did they compare the HM EVs with a relevant “parent cell” (41).
Glycosylation patterns also aid in the recognition and uptake of EVs by target cells (62). Wolf et al. (63) used bovine-milk exosomes to demonstrate that, in human and rat intestinal cells, glycosylation of the EVs and the cells were responsible for recognition, endocytosis, and eventual accumulation of the cargo miRNA within cells. This highlights the role of the EV glycome in targeted delivery of bioactive components. Moreover, identifying HM EV glycosylation patterns might help clarify the contradictory data regarding the impact of EVs on HIV infectivity. Since HIV contains heavily glycosylated membrane proteins (e.g., gp120), EV glycome profile could elucidate their role in HIV particle penetration into target cells. Näslund et al. (34) also demonstrated that preincubation of MDDCs with plasma-derived exosomes did not have an effect on HIV transfer by MDDCs to CD4+ T cells, although the effect was observed with HM-derived EVs “in play.”
HM EVs, Preterm Infants, and NEC
Kahn et al. (22) examined the changes in HM EV miRNA in infants delivered preterm. They collected 20 milk samples that included 5 extremely preterm (<28 wk of gestation) and 5 preterm (28–32 wk of gestation) and 10 “early term” milk samples (>32 wk of gestation). They demonstrated that miRNA content in preterm milk and early term milk was mostly identical and was not altered after in vitro digestion in either group; however, they detected changes in preterm HM miRNA profile that were restricted to low abundance RNA reads. The most abundant RNA reads identified in both preterm and term populations are miRNA-22-3p, miRNA-148a-3p, and miRNA-146a, which are predominantly associated with immune function alongside cellular differentiation. Additionally, immunofluorescence demonstrated internalization of EVs by human intestinal epithelial crypt-like cells (22). Moreover, miRNAs in both preterm and term and digested and undigested milk were similar, which indicates a high degree of miRNA content preservation within EVs. The aforementioned findings suggest that both preterm and term milk may elicit immunomodulatory effects, either locally in the gut or systemically through circulation with the help of miRNA cargos within EVs in HM.
Martin et al. (26) utilized a different approach for isolated HM EVs, which were characterized by electron microscopy and nanoparticle tracking analysis. These EVs were assessed for their ability to prevent cell death of intestinal cell line 6 (IEC-6) cells treated with hydrogen peroxide, which constitutes a model of NEC. The researchers observed reduced IEC-6 cell death due to oxidative stress after subjecting them to 200 μM H2O2 in the presence of purified HM-derived EVs. This study provides initial mechanistic evidence for alleviation of oxidative stress by EVs in HM, which is a key pathophysiological mechanism of necrosis. However, the in vitro model cannot truly represent the wide variety of variables that contribute to the development of NEC. Wang et al. (37) extended the in vitro studies by treating an NEC rat model with term and preterm EVs and demonstrated greater proliferation of intestinal mucosa and reduced severity of NEC with preterm EVs. They described differences in the expression of peptides between HM EVs from mothers who delivered at term versus preterm with 47 peptides upregulated and 23 downregulated. Finally, the authors performed pathway analysis using Gene Ontology (GO) term enrichment to identify the putative protein domains responsible for this protective effect, suggesting that lactotransferrin and lactadherin proteins present in EVs are likely involved in gut barrier function (37).
The identified studies established that intestinal cells in an in vitro model could internalize EVs. They also established that miRNA cargo is intact through this process (22–24). This suggests that EVs can effectively deliver miRNA cargo to infant gut allowing for maternal to infant transmission of regulatory signals including those involved in gut and immune system development during infancy. Additionally, both Martin et al. (26) and Wang et al. (37) demonstrated that breast-milk–derived EVs were effective either in an in vitro or animal model of NEC in preventing cell death and stimulating intestinal cell proliferation. The different methodologies utilized by both papers, as well as their focus on different cargos, suggests breast-milk EVs may be one of the components in breast milk leading to protection from NEC (26). The absence of functional EVs in infant formula may explain the epidemiological observation that children who receive donor breast milk instead of formula are less likely to develop NEC (45, 64). Future studies are needed to determine if other breast-milk components (i.e., HMOs, IgA) and EVs have synergistic roles in their protective effect on NEC (64, 65) and immune function during the infancy period.
EVs’ Role as Therapeutics
An additional rationale for examining HM EVs is for the possible therapeutic use of exogenously delivered EVs. This is already a fertile ground for research with multiple neonatal conditions targeted using mesenchymal stem cell (MSC)–derived EVs as “cell free” regenerative medicine. MSC-based therapies have also found application in BPD, a chronic lung disease that develops in preterm infants resulting from their immature lung development, as well as from environmental factors such as infection, invasive ventilation, and liberal supplemental oxygen. This has resulted in a number of phase I clinical trials (66–68). However, experimental animal models suggest that MSC cell-free media may ameliorate disease to a similar extent as the MSC-based treatment (69, 70). Numerous mechanisms have been postulated for the MSC-derived exosome effect, including TNF-stimulated gene 6 (TSG6) or through vascular endothelial growth factor (VEGF) signaling (71–73). The use of pluripotent stem cell lines in newborns comes with a risk of tumorigenesis, which would be avoided using MSC cell-free media or EVs, and there is some additional animal-derived evidence that EVs may provide other benefits over cell therapy in the treatment of BPD (70).
As mentioned above, EVs may be involved in the protective effect of HM against NEC. HM-derived EVs could be a therapeutic option for neonates whose mothers are unable to breastfeed and where receiving donor-expressed breast milk is difficult. MSCs derived from various sources (amniotic fluid, bone marrow) have been shown to enact protective effects in NEC in rat models and that these effects are at least partially driven by EV-related mechanisms (74–76). EVs have also been suggested as possible therapies for hypoxic-ischemic encephalopathy, retinopathy of prematurity, and spina bifida, which represent a substantial burden of disease in the neonatal population (77). It may be hypothesized that HM EVs may also be associated with the beneficial effects seen in the management of above mentioned conditions. Nonetheless, the mechanisms, efficacy, and feasibility of EVs in therapeutics need further investigation.
Conclusions
This Perspective identified a few studies addressing the role HM EVs play in child health and disease (Figure 1). While content characterization and in vitro studies have demonstrated biological plausibility for a role of EVs in immune tolerance, atopy, and the development of gastrointestinal barrier function, mechanistic details have not been elucidated in human subjects or in animal models. Other gaps in current knowledge include the changes in EV phenotype over time, with very little research on the impact of HM EVs on metabolism to date in contrast to animal data.
FIGURE 1.
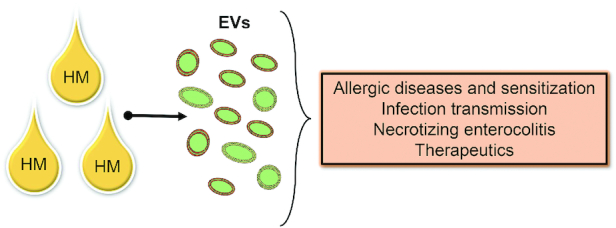
Summary of the role of EVs: HM EVs contain cargos (i.e., miRNA, proteins, metabolites, and glycopeptides). These EV cargos likely have a biological impact on neighboring cells and may impact health outcomes in children. EV, extracellular vesicle; HM, human milk.
While there are a number of very well-constructed studies, many of them predate current MISEV guidelines and would require validation with these in mind, with a significant minority only utilizing a single methodology for examining EVs specifically or assuming existence of EVs on the basis of CD9+/CD63+/CD81+ fractions (38–40). The available evidence is limited and outcomes of the studies cannot be extrapolated to the other cohorts due to a limited sample size. Large, rigorously harmonized, and standardized studies may help generate datasets that will allow for pooling the data from different cohorts and to each reliable conclusions of the impact HM EVs may have on infant health and disease.
Overall, the data on HM EVs at present do not support making definitive statements regarding the role of EVs in immune function during infancy and long-term health outcomes, such as cardiovascular, endocrine, and autoimmune disease development (78, 79). Studies determining the mechanistic role of EVs on health outcomes in infancy and childhood are needed, with a particular focus on elucidating the functions of breast-milk EVs, which suggest future directions in HM research.
Supplementary Material
ACKNOWLEDGEMENTS
The authors’ responsibilities were as follows—DO and DD: performed the literature search; DO, NVA, NAN, AAE, LP, MRS, LY, and DM: prepared the initial draft of the manuscript; JG: provided expertise with regard to the aspects of the reviewed topic; DO, MRS, and DM: developed the initial design; and all authors: read and approved the final manuscript.
Notes
AE and LY are supported by USDA-ARS project 6026–51000–010–06S. In addition, LY is supported by NIH P20GM121293 and NIH R21AI146521. DM acknowledges the receipt of funding from the “5–100” Russian Academic Excellence Project.
Author disclosures: DM received funding from the European Cooperation in Science and Technology (COST) and the “5-100” Russian Academic Excellence Project and is involved in expert activities within the ILSI Europe expert group. He also has given paid lectures for Merck, Sharp & Dohme (MSD) and Bayer. MRS receives funding from the Liaison Committee between the Central Norway Regional Health Authority (RHA) and the Norwegian University of Science and Technology (NTNU). All the other authors report no conflicts of interest.
Perspective articles allow authors to take a position on a topic of current major importance or controversy in the field of nutrition. As such, these articles could include statements based on author opinions or point of view. Opinions expressed in Perspective articles are those of the author and are not attributable to the funder(s) or the sponsor(s) or the publisher, Editor, or Editorial Board of Advances in Nutrition. Individuals with different positions on the topic of a Perspective are invited to submit their comments in the form of a Perspectives article or in a Letter to the Editor.
Supplemental Methods, Supplemental Figure 1, and Supplemental Table 1 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents on https://academic.oup.com/advances.
DO, MRS, LY, and DM contributed equally to this work.
Abbreviations used: ALADDIN, Allergic Disease During INfancy; BPD, bronchopulmonary dysplasia; CD, cluster of differentiation; DANCR, differentiation antagonizing non-protein coding RNA; EV, extracellular vesicle; GAS5, growth arrest-specific 5; HLA, human leukocyte antigen; HM, human breast milk; HMO, human milk oligosaccharide; HSC, heat shock cognate; IEC-6, intestinal cell line 6; MDDC, monocyte-derived dendritic cell; miR, microRNA; MISEV, Minimal Information for Studies of Extracellular Vesicles; MSC, mesenchymal stem cell; MUC-1, mucin 1 cell surface–associated; NEC, necrotizing enterocolitis; PBMC, peripheral blood mononuclear cell; ProPACT, Probiotics in the Prevention of Allergy among Children in Trondheim; SRA1, steroid receptor RNA activator 1; Treg, regulatory T cell.
Contributor Information
Daniel O'Reilly, Children's Health Ireland at Temple Street, Dublin, Ireland; SPHERE Research Group, Conway Institute, University College Dublin, Dublin, Ireland.
Denis Dorodnykh, Department of Pediatrics and Pediatric Infectious Diseases, Institute of Child's Health, Sechenov First Moscow State Medical University (Sechenov University), Moscow, Russia.
Nina V Avdeenko, Department of Pediatrics and Pediatric Infectious Diseases, Institute of Child's Health, Sechenov First Moscow State Medical University (Sechenov University), Moscow, Russia.
Nikita A Nekliudov, Department of Pediatrics and Pediatric Infectious Diseases, Institute of Child's Health, Sechenov First Moscow State Medical University (Sechenov University), Moscow, Russia.
Johan Garssen, Division of Pharmacology, Utrecht Institute for Pharmaceutical Sciences, Faculty of Science, Utrecht University, Utrecht, Netherlands.
Ahmed A Elolimy, Department of Pediatrics, University of Arkansas for Medical Sciences, Little Rock, AR, USA; Arkansas Children's Nutrition Center, Little Rock, AR, USA.
Loukia Petrou, Department of Bioengineering, Imperial College London, London, United Kingdom.
Melanie Rae Simpson, Department of Public Health and Nursing, Norwegian University of Science and Technology, Trondheim, Norway; Clinic of Laboratory Medicine, St. Olavs Hospital, Trondheim, Norway.
Laxmi Yeruva, Department of Pediatrics, University of Arkansas for Medical Sciences, Little Rock, AR, USA; Arkansas Children's Nutrition Center, Little Rock, AR, USA; Arkansas Children's Research Institute, Little Rock, AR, USA.
Daniel Munblit, Department of Pediatrics and Pediatric Infectious Diseases, Institute of Child's Health, Sechenov First Moscow State Medical University (Sechenov University), Moscow, Russia; Inflammation, Repair, and Development Section, National Heart and Lung Institute, Faculty of Medicine, Imperial College London, London, United Kingdom; inVIVO Planetary Health, Group of the Worldwide Universities Network, West New York, NJ, USA; Research and Clinical Center for Neuropsychiatry, Moscow, Russia.
References
- 1. Ballard O, Morrow AL. Human milk composition: nutrients and bioactive factors. Pediatr Clin North Am. 2013;60:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Jantscher-Krenn E, Zherebtsov M, Nissan C, Goth K, Guner YS, Naidu N, Choudhury B, Grishin AV, Ford HR, Bode L. The human milk oligosaccharide disialyllacto-N-tetraose prevents necrotising enterocolitis in neonatal rats. Gut [Internet]. 2012;61:1417–25.. doi: 10.1136/gutjnl-2011-301404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Autran CA, Kellman BP, Kim JH, Asztalos E, Blood AB, Spence ECHH, Patel AL, Hou J, Lewis NE, Bode L. Human milk oligosaccharide composition predicts risk of necrotising enterocolitis in preterm infants. Gut. [Internet]2018;67:1064–70.. [Accessed 2017 Apr 5]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/28381523. [DOI] [PubMed] [Google Scholar]
- 4. Pannaraj PS, Li F, Cerini C, Bender JM, Yang S, Rollie A, Adisetiyo H, Zabih S, Lincez PJ, Bittinger Ket al. . Association between breast milk bacterial communities and establishment and development of the infant gut microbiome. JAMA Pediatr. 2017;171:647–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yang S, Martin RM, Oken E, Hameza M, Doniger G, Amit S, Patel R, Thompson J, Rifas-Shiman SL, Vilchuck Ket al. . Breastfeeding during infancy and neurocognitive function in adolescence: 16-year follow-up of the PROBIT cluster-randomized trial. PLoS Med. 2018;15:e1002554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kramer MS, Chalmers B, Hodnett ED, Sevkovskaya Z, Dzikovich I, Shapiro S, Collet J, Vanilovich I, Mezen I, Ducret Tet al. . Promotion of Breastfeeding Intervention Trial (PROBIT): a randomized trial in the Republic of Belarus. JAMA. 2001;285:413. [DOI] [PubMed] [Google Scholar]
- 7. Kramer MS, Kakuma R. Optimal duration of exclusive breastfeeding. Cochrane Database Syst Rev. 2012;CD003517. doi: 10.1002/14651858.CD003517.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Admyre C, Johansson SM, Qazi KR, Filén J-J, Lahesmaa R, Norman M, Neve EPA, Scheynius A, Gabrielsson S. Exosomes with immune modulatory features are present in human breast milk. J Immunol. 2007;179:1969–78. [DOI] [PubMed] [Google Scholar]
- 9. Zempleni J, Sukreet S, Zhou F, Wu D, Mutai E. Milk-derived exosomes and metabolic regulation. Annu Rev Anim Biosci. 2019;7:245–62. [DOI] [PubMed] [Google Scholar]
- 10. Zonneveld MI, Brisson AR, van Herwijnen MJC, Tan S, van de Lest CHA, Redegeld FA, Garssen J, Wauben MHM, Nolte-'t Hoen EN. Recovery of extracellular vesicles from human breast milk is influenced by sample collection and vesicle isolation procedures. J Extracell Vesicles. 2014;3:24215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Théry C, Witwer KW, Aikawa E, Alcaraz MJ, Anderson JD, Andriantsitohaina R, Antoniou A, Arab T, Archer F, Atkin-Smith GKet al. . Minimal Information for Studies of Extracellular Vesicles 2018 (MISEV2018): a position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J Extracell Vesicles. 2018;7:1535750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shah R, Patel T, Freedman JE. Circulating extracellular vesicles in human disease. N Engl J Med. 2018;379:958–66. [DOI] [PubMed] [Google Scholar]
- 13. Qin W, Tsukasaki Y, Dasgupta S, Mukhopadhyay N, Ikebe M, Sauter ER. Exosomes in human breast milk promote EMT. Clin Cancer Res. 2016;22:4517–24. [DOI] [PubMed] [Google Scholar]
- 14. Gheinani AH, Vögeli M, Baumgartner U, Vassella E, Draeger A, Burkhard FC, Monastyrskaya K. Improved isolation strategies to increase the yield and purity of human urinary exosomes for biomarker discovery. Sci Rep. 2018;8:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Welton JL, Loveless S, Stone T, von Ruhland C, Robertson NP, Clayton A. Cerebrospinal fluid extracellular vesicle enrichment for protein biomarker discovery in neurological disease; multiple sclerosis. J Extracell Vesicles. 2017;6:1369805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Iba T, Ogura H. Role of extracellular vesicles in the development of sepsis-induced coagulopathy. J Intens Care. 2018;6:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. König L, Kasimir-Bauer S, Bittner A-K, Hoffmann O, Wagner B, Santos Manvailer LF, Kimmig R, Horn PA, Rebmann V. Elevated levels of extracellular vesicles are associated with therapy failure and disease progression in breast cancer patients undergoing neoadjuvant chemotherapy. Oncoimmunology. [Internet]2017;7:e1376153. Available from: https://www.ncbi.nlm.nih.gov/pubmed/29296534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zempleni J. Milk exosomes: beyond dietary microRNAs. Genes Nutr. 2017;12:10–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Xi Q-Y, Zhang Y-L, Shu G, Wang S-B, Jiang Q-Y, Zhu X-T, Ye R-S, Qi Q-E, Chen T, Cheng Xet al. . Exploration of microRNAs in porcine milk exosomes. BMC Genomics. 2014;15:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ma J, Wang C, Long K, Zhang H, Zhang J, Jin L, Tang Q, Jiang A, Wang X, Tian Set al. . Exosomal microRNAs in giant panda (Ailuropoda melanoleuca) breast milk: potential maternal regulators for the development of newborn cubs. Sci Rep. 2017;7:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Modepalli V, Kumar A, Hinds LA, Sharp JA, Nicholas KR, Lefevre C. Differential temporal expression of milk miRNA during the lactation cycle of the marsupial Tammar wallaby (Macropus eugenii). BMC Genomics. 2014;15:1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kahn S, Liao Y, Du X, Xu W, Li J, Lönnerdal B. Exosomal microRNAs in milk from mothers delivering preterm infants survive in vitro digestion and are taken up by human intestinal cells. Mol Nutr Food Res. 2018;62:1–10. [DOI] [PubMed] [Google Scholar]
- 23. Liao Y, Du X, Li J, Lönnerdal B. Human milk exosomes and their microRNAs survive digestion in vitro and are taken up by human intestinal cells. Mol Nutr Food Res. 2017;61:1–11. [DOI] [PubMed] [Google Scholar]
- 24. Zhou Q, Li M, Wang X, Li Q, Wang T, Zhu Q, Zhou X, Wang X, Gao X, Li X. Sample collection enrichment of exosomal RNA in breast milk. Int J Biol Sci. [Internet]2012;8:118–23.. Available from: http://www.biolsci.org. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Karlsson O, Rodosthenous RS, Jara C, Brennan KJ, Wright RO, Baccarelli AA, Wright RJ. Detection of long non-coding RNAs in human breastmilk extracellular vesicles: implications for early child development. Epigenetics. [Internet]2016;11:721–9.. Available from: 10.1080/15592294.2016.1216285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Martin C, Patel M, Williams S, Arora H, Sims B. Human breast milk-derived exosomes attenuate cell death in intestinal epithelial cells. Innate Immun. 2018;24:278–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. van Herwijnen MJC, Driedonks TAP, Snoek BL, Kroon AMT, Kleinjan M, Jorritsma R, Pieterse CMJ, Hoen ENMN-’t, Wauben MHM. Abundantly present miRNAs in milk-derived extracellular vesicles are conserved between mammals. Front Nutr. 2018;5:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chen T, Xie MY, Sun JJ, Ye RS, Cheng X, Sun RP, Wei LM, Li M, Lin DL, Jiang QYet al. . Porcine milk-derived exosomes promote proliferation of intestinal epithelial cells. Sci Rep. [Internet]2016;6:1–12.. Available from: 10.1038/srep33862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gu Y, Li M, Wang T, Liang Y, Zhong Z, Wang X, Zhou Q, Chen L, Lang Q, He Zet al. . Lactation-related microRNA expression profiles of porcine breast milk exosomes. PLoS One. 2012;7:e43691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Parry HA, Brooks Mobley C, Mumford PW, Romero MA, Haun CT, Zhang Y, Roberson PA, Zempleni J, Ferrando AA, Vechetti IJet al. . Bovine milk extracellular vesicles (EVs) modification elicits skeletal muscle growth in rats. Front Physiol. 2019;10:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Manca S, Upadhyaya B, Mutai E, Desaulniers AT, Cederberg RA, White BR, Zempleni J. Milk exosomes are bioavailable and distinct microRNA cargos have unique tissue distribution patterns. Sci Rep. [Internet]2018;8:1–11.. Available from: 10.1038/s41598-018-29780-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Zempleni J, Aguilar-Lozano A, Sadri M, Sukreet S, Manca S, Wu D, Zhou F, Mutai E. Biological activities of extracellular vesicles and their cargos from bovine and human milk in humans and implications for infants. J Nutr. 2017;147:3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks Let al. . PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. [Internet]2018;169:467. Available from: http://annals.org/article.aspx?doi=10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 34. Näslund TI, Paquin-Proulx D, Paredes PT, Vallhov H, Sandberg JK, Gabrielsson S. Exosomes from breast milk inhibit HIV-1 infection of dendritic cells and subsequent viral transfer to CD4+ T cells. AIDS. 2014;28:171–80. [DOI] [PubMed] [Google Scholar]
- 35. Sims B, Williams SD, Krendelchtchikov A, Matthews QL, Farrow AL, Bansal A, Gu L. Role of TIM-4 in exosome-dependent entry of HIV-1 into human immune cells. Int J Nanomedicine. 2017;12:4823–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sims B, Farrow AL, Williams SD, Bansal A, Krendelchtchikov A, Matthews QL. Tetraspanin blockage reduces exosome-mediated HIV-1 entry. Arch Virol. [Internet]2018;163:1683–9.. Available from: 10.1007/s00705-018-3737-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wang X, Yan X, Zhang L, Cai J, Zhou Y, Liu H, Hu Y, Chen W, Xu S, Liu Pet al. . Identification and peptidomic profiling of exosomes in preterm human milk: insights into necrotizing enterocolitis prevention. Mol Nutr Food Res. 2019;63::1801247. [DOI] [PubMed] [Google Scholar]
- 38. Golan-Gerstl R, Elbaum Shiff Y, Moshayoff V, Schecter D, Leshkowitz D, Reif S. Characterization and biological function of milk-derived miRNAs. Mol Nutr Food Res. 2017;61:1700009. [DOI] [PubMed] [Google Scholar]
- 39. Simpson MR, Brede G, Johansen J, Johnsen R, Storrø O, Sætrom P, Øien T. Human breast milk miRNA, maternal probiotic supplementation and atopic dermatitis in offspring. PLoS One. 2015;10:e0143496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kosaka N, Izumi H, Sekine K, Ochiya T. MicroRNA as a new immune-regulatory agent in breast milk. Silence. 2010;1:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Batista BS, Eng WS, Pilobello KT, Hendricks-Muñoz KD, Mahal LK. Identification of a conserved glycan signature for microvesicles. J Proteome Res. 2011;10:4624–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lässer C, Seyed Alikhani V, Ekström K, Eldh M, Torregrosa Paredes P, Bossios A, Sjöstrand M, Gabrielsson S, Lötvall J, Valadi H. Human saliva, plasma and breast milk exosomes contain RNA: uptake by macrophages. J Transl Med. [Internet]2011;9:9. Available from: http://www.translational-medicine.com/content/9/1/9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. van Herwijnen MJC, Zonneveld MI, Goerdayal S, Nolte-’t Hoen ENM, Garssen J, Stahl B, Maarten Altelaar AF, Redegeld FA, Wauben MHM. Comprehensive proteomic analysis of human milk-derived extracellular vesicles unveils a novel functional proteome distinct from other milk components. Mol Cell Proteomics. 2016;15:3412–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Torregrosa Paredes P, Gutzeit C, Johansson S, Admyre C, Stenius F, Alm J, Scheynius A, Gabrielsson S. Differences in exosome populations in human breast milk in relation to allergic sensitization and lifestyle. Allergy. 2014;69:463–71. [DOI] [PubMed] [Google Scholar]
- 45. Leiferman A, Shu J, Upadhyaya ÃB, Cui J, Zempleni ÃJ, Leferman A, Shu J, Upadhaya B, Cui J, Zempleni J. Storage of extracellular vesicles in human milk, and microRNA profiles in human milk exosomes and infant formulas. J Pediatr Gastroenterol Nutr. 2019;69:235–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Lukasik A, Brzozowska I, Zielenkiewicz U, Zielenkiewicz P. Detection of plant miRNAs abundance in human breast milk. Int J Mol Sci. 2018;19:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. He L, Hannon GJ. MicroRNAs: small RNAs with a big role in gene regulation. Nat Rev Genet. 2004;5:522–31. [DOI] [PubMed] [Google Scholar]
- 48. Ramaswamy H, Swamy CVB, Das MR. Purification and characterization of a high molecular weight ribonuclease from human milk. J Biol Chem. 1993;268:4181–7. [PubMed] [Google Scholar]
- 49. Mitchell PS, Parkin RK, Kroh EM, Fritz BR, Wyman SK, Pogosova-Agadjanyan EL, Peterson A, Noteboom J, O'Briant KC, Allen Aet al. . Circulating microRNAs as stable blood-based markers for cancer detection. Proc Natl Acad Sci U S A. [Internet]. 2008;105:10513–8.. Available from: https://www.ncbi.nlm.nih.gov/pubmed/18663219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Chen X, Ba Y, Ma L, Cai X, Yin Y, Wang K, Guo J, Zhang Y, Chen J, Guo Xet al. . Characterization of microRNAs in serum: a novel class of biomarkers for diagnosis of cancer and other diseases. Cell Res. [Internet]2008;18:997–1006.. Available from: 10.1038/cr.2008.282. [DOI] [PubMed] [Google Scholar]
- 51. Xu L, Yang B-F, Ai J. MicroRNA transport: a new way in cell communication. J Cell Physiol. [Internet]2013;228:1713–9.. Available from: https://www.ncbi.nlm.nih.gov/pubmed/23460497. [DOI] [PubMed] [Google Scholar]
- 52. Vickers KC, Remaley AT. Lipid-based carriers of microRNAs and intercellular communication. Curr Opin Lipidol. [Internet]2012;23:91–7.. Available from: https://www.ncbi.nlm.nih.gov/pubmed/22418571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Hata T, Murakami K, Nakatani H, Yamamoto Y, Matsuda T, Aoki N. Isolation of bovine milk-derived microvesicles carrying mRNAs and microRNAs. Biochem Biophys Res Commun. [Internet]2010;396:528–33.. Available from: 10.1016/j.bbrc.2010.04.135. [DOI] [PubMed] [Google Scholar]
- 54. Leiferman A, Shu J, Grove R, Cui J, Adamec J, Zempleni J. A diet defined by its content of bovine milk exosomes and their RNA cargos has moderate effects on gene expression, amino acid profiles and grip strength in skeletal muscle in C57BL/6 mice. J Nutr Biochem. [Internet]2018;59:123–8.. Available from: 10.1016/j.jnutbio.2018.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Melnik BC, John SM, Schmitz G. Milk is not just food but most likely a genetic transfection system activating mTORC1 signaling for postnatal growth. Nutr J. 2013;12:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Conditions T, Benmoussa A, Lee CHC, Laffont B, Savard P, Laugier J, Boilard E, Gilbert C, Fliss I, Provost P. Commercial dairy cow milk microRNAs resist digestion under simulated gastrointestinal tract conditions. J Nutr. 2016;146:2206–15. [DOI] [PubMed] [Google Scholar]
- 57. Pieters BCH, Arntz OJ, Bennink MB, Broeren MGA, Van Caam APM, Koenders MI, Van Lent PLEM, Van Den Berg WB, De Vries M, Van Der Kraan PMet al. . Commercial cow milk contains physically stable extracellular vesicles expressing immunoregulatory TGF-β. PLoS One. 2015;10:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lu L, Barbi J, Pan F. The regulation of immune tolerance by FOXP3. Nat Rev Immunol 2017;17:703–17. [Internet]. Available from: 10.1038/nri.2017.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Peterson JA, Newburg DS, Yolken RH, Vonderfecht SL, Midthun K, Fouts ET. Human milk mucin inhibits rotavirus replication and prevents experimental gastroenteritis. J Clin Invest. 1992;90:1984–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Liu B, Yu Z, Chen C, Kling DE, Newburg DS. Human milk mucin 1 and mucin 4 inhibit Salmonella enterica Serovar Typhimurium invasion of human intestinal epithelial cells in vitro. J Nutr. 2012;142:1504–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Zellweger F, Eggel A. IgE-associated allergic disorders: recent advances in etiology, diagnosis, and treatment. Allergy. 2016;71:1652–61. [DOI] [PubMed] [Google Scholar]
- 62. Escrevente C, Keller S, Altevogt P, Costa J. Interaction and uptake of exosomes by ovarian cancer cells. BMC Cancer. [Internet]2011;11:108. Available from: https://www.ncbi.nlm.nih.gov/pubmed/21439085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Wolf T, Baier SR, Zempleni J. The intestinal transport of bovine milk exosomes is mediated by endocytosis in human colon carcinoma Caco-2 cells and rat small intestinal IEC-6 cells. J Nutr. [Internet]2015;145:2201–6.. Available from: 10.3945/jn.115.218586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. McGuire W, Anthony M. Donor human milk versus formula for preventing necrotising enterocolitis in preterm infants: systematic review. Arch Dis Child Fetal Neonatal Ed. 2003;88:11F–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Gopalakrishna KP, Macadangdang BR, Rogers MB, Tometich JT, Firek BA, Baker R, Ji J, Burr AHP, Ma C, Good Met al. . Maternal IgA protects against the development of necrotizing enterocolitis in preterm infants. Nat Med. [Internet]2019;25:1110–15.. Available from: 10.1038/s41591-019-0480-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Ahn SY, Chang YS, Kim JH, Sung SI, Park WS. Two-year follow-up outcomes of premature infants enrolled in the phase I trial of mesenchymal stem cells transplantation for bronchopulmonary dysplasia. J Pediatr. [Internet]2017;185:49–54., e2. Available from: 10.1016/j.jpeds.2017.02.061. [DOI] [PubMed] [Google Scholar]
- 67. Powell SB, Silvestri JM. Safety of intratracheal administration of human umbilical cord blood derived mesenchymal stromal cells in extremely low birth weight preterm infants. J Pediatr. [Internet]2019;210:209–13, e2.. Available from: 10.1016/j.jpeds.2019.02.029. [DOI] [PubMed] [Google Scholar]
- 68. Chang YS, Ahn SY, Yoo HS, Sung SI, Choi SJ, Oh W II, Park WS. Mesenchymal stem cells for bronchopulmonary dysplasia: phase 1 dose-escalation clinical trial. J Pediatr. [Internet]2014;164:966–72, e6.. Available from: 10.1016/j.jpeds.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 69. Pierro M, Ionescu L, Montemurro T, Vadivel A, Weissmann G, Oudit G, Emery D, Bodiga S, Eaton F, Péault Bet al. . Short-term, long-term and paracrine effect of human umbilical cord-derived stem cells in lung injury prevention and repair in experimental bronchopulmonary dysplasia. Thorax. 2013;68:475–84. [DOI] [PubMed] [Google Scholar]
- 70. Porzionato A, Zaramella P, Dedja A, Guidolin D, Van Wemmel K, Macchi V, Jurga M, Perilongo G, De Caro R, Baraldi Eet al. . Intratracheal administration of clinical-grade mesenchymal stem cell-derived extracellular vesicles reduces lung injury in a rat model of bronchopulmonary dysplasia. Am J Physiol Lung Cell Mol Physiol. 2019;316:L6–19. [DOI] [PubMed] [Google Scholar]
- 71. Chaubey S, Thueson S, Ponnalagu D, Alam MA, Gheorghe CP, Aghai Z, Singh H, Bhandari V. Early gestational mesenchymal stem cell secretome attenuates experimental bronchopulmonary dysplasia in part via exosome-associated factor TSG-6. Stem Cell Res Ther. 2018;9(1):173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Ahn SY, Park WS, Kim YE, Sung DK, Sung SI, Ahn JY, Chang YS. Vascular endothelial growth factor mediates the therapeutic efficacy of mesenchymal stem cell-derived extracellular vesicles against neonatal hyperoxic lung injury. Exp Mol Med. 2018;50(4):26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Braun RK, Chetty C, Balasubramaniam V, Centanni R, Haraldsdottir K, Hematti P, Eldridge MW. Intraperitoneal injection of MSC-derived exosomes prevent experimental bronchopulmonary dysplasia. Biochem Biophys Res Commun. 2018;503:2653–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Zani A, Cananzi M, Fascetti-Leon F, Lauriti G, Smith VV, Bollini S, Ghionzoli M, D'Arrigo A, Pozzobon M, Piccoli Met al. . Amniotic fluid stem cells improve survival and enhance repair of damaged intestine in necrotising enterocolitis via a COX-2 dependent mechanism. Gut. 2014;63:300–9. [DOI] [PubMed] [Google Scholar]
- 75. Rager TM, Olson JK, Zhou Y, Wang Y, Besner GE. Exosomes secreted from bone marrow-derived mesenchymal stem cells protect the intestines from experimental necrotizing enterocolitis. J Pediatr Surg. 2016;51:942–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Drucker NA, McCulloh CJ, Li B, Pierro A, Besner GE, Markel TA. Stem cell therapy in necrotizing enterocolitis: current state and future directions. Semin Pediatr Surg. 2018;27:57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Matei AC, Antounians L, Zani A. Extracellular vesicles as a potential therapy for neonatal conditions: state of the art and challenges in clinical translation. Pharmaceutics. 2019;11:404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Horta BL, Loret De Mola C, Victora CG. Long-term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: a systematic review and meta-analysis. Acta Paediatr. 2015;104:30–7. [DOI] [PubMed] [Google Scholar]
- 79. Garcia-Larsen V, Ierodiakonou D, Jarrold K, Cunha S, Chivinge J, Robinson Z, Geoghegan N, Ruparelia A, Devani P, Trivella Met al. . Diet during pregnancy and infancy and risk of allergic or autoimmune disease: a systematic review and meta-analysis. PLoS Med. 2018;15:e1002507. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


