Abstract
Background
A 2006 Canadian survey showed a large variability in neonatal follow-up practices. In 2010, all 26 tertiary level Neonatal Follow-Up clinics joined the Canadian Neonatal Follow-Up Network (CNFUN) and agreed to implement a standardized assessment (including the Bayley Scales of Infant and Toddler Development-III (Bayley-III) at 18 months corrected age for children born < 29 weeks’ gestation. It is unknown whether the variability in follow-up practices lessened as a result.
Objectives
To describe the current status of neonatal follow-up services in Canada and changes over time.
Methods
A comprehensive online survey was sent to all tertiary level CNFUN Follow-up programs. Questions were based on previous survey results, current literature, and investigator expertise and consensus.
Results
Respondents included 23 of 26 (88%) CNFUN programs. All sites provide neurodevelopmental screening and referrals in a multidisciplinary setting with variations in staffing. CNFUN programs vary with most offering five to seven visits. Since 2006, assessments at 18 months CA increased from 84% to 91% of sites, Bayley-III use increased from 21% to 74% (P=0.001) and eligibility for follow-up was expanded for children with stroke, congenital diaphragmatic hernia and select anomalies detected in utero. Audit data is collected by > 80% of tertiary programs.
Conclusion
Care became more consistent after CNFUN; 18-month assessments and Bayley-III use increased significantly. However, marked variability in follow-up practices persists.
Keywords: Canada, Health services, Neonatal follow-up
The introduction of neonatal intensive care units (NICUs) and the subsequent increase in survival rates of very premature infants created a new population of survivors with unknown long-term outcomes. Neonatal Follow-Up programs (NFUPs) emerged to address this knowledge gap and to ensure that these children receive early diagnosis and intervention to optimize the potential of these new survivors. Most NFUPs have a multidisciplinary team that provides parents and infants with access to experts who can provide reassurance and support, timely diagnosis, referral to needed services and assistance with coordination of their care (1). NFUPs also conduct standardized assessments at specified ages which, in addition to providing clinical screening, can also provide infrastructure and data for audit and research (2).
A high-risk NFUP affiliated with tertiary level NICUs is the standard of care in most developed countries such as Canada and is mandated in others, such as the USA (2,3). In Canada, NFUPs emerged independently with different practices, infrastructure, and funding sources (research versus operational funding). Despite this variation, starting in the 1980s, program leaders recognized the benefits of standardization and initiated several collaborative efforts. Consensus guidelines, published in 1987 (4), provided Canadian recommendations for NFUP staffing, recruitment criteria, schedule of visits, and standardized assessments but surveys in 1996 and 2006 (5,6) showed little consistency in practices. These variations hinder collaboration in research and benchmarking to improve family and child outcomes.
The Canadian Neonatal Follow-Up Network (CNFUN), a voluntary collaboration of all 26 tertiary level NFUPs in Canada, developed a standardized set of assessments at 18 months corrected age (CA) for children born preterm at less than 29 weeks’ gestational age. CNFUN was implemented in 2010 as part of the research funded CIHR Team in Maternal Infant Care project for the birth cohort April 1, 2009 to September 30, 2011. Data entered into the CNFUN database with linkage to neonatal data collected by the Canadian Neonatal Network (7) provide data from pregnancy to infancy for benchmarking, quality improvement, and research. Voluntary unfunded CNFUN data collection has continued for children born after 2011.
Governments have also been interested in standardizing NFUP practices. In Ontario, a government initiative of the Provincial Council for Maternal and Child Health (PCMCH) launched a Neonatal Follow-Up Clinics Working Group in 2013 to improve the delivery and standardization of NFUP care in the province. Recommendations for both tertiary and secondary level neonatal follow-up clinics were finalized in November 2017 (8).
The effect of CNFUN on the provision of neonatal follow-up services in Canada has not been studied. It is unknown whether the practice variability in eligibility criteria, timing and developmental assessment measures used and the number, type and characteristics of health care professionals working in NFUPs noted in the 1987, 1997, and 2006 (4–6) studies have changed.
The primary objective of this study was to describe the status in 2017 of tertiary level Canadian NFUP services. A secondary objective was to evaluate changes in Canadian NFUP services over time by comparing the 2017 findings with the 2006 survey and the effect of a research-funded network, CNFUN, on NFUP services.
METHODS
Descriptive study using survey methods
An online survey with 68 questions was developed based on current literature, the previous 2006 survey (6) results, and investigators’ NFUP clinical expertise and knowledge about CNFUN and PCMCH. Themes included NFUP eligibility criteria, staffing models, services, communication methods, timing and frequency of visits, and the range of assessments conducted at each visit. The questions were piloted at two centres and modifications were carried out following their feedback.
Participants
An e-mail survey was sent to site investigators at all 26 CNFUN NFUPs. The voluntary and anonymous nature of the study was explained. Responses were captured using REDCap Software Version 6.10.19. The survey was conducted over a 14-week period from March to July 2017. The questionnaires were sent three times to all participants to maximize the response rate. Research ethics approval was obtained by the Children’s & Women’s Hospital of British Columbia.
Analyses
Data were analyzed descriptively. For CNFUN survey results, comparisons were made with the comparable 2006 survey items. Chi square analyses were used to test six a priori hypotheses. We hypothesized that in 2017, compared to 2006, use of the motor and cognitive domains of the Bayley Scales of Infant Development would increase as a result of the CNFUN standardized protocol and recruitment for prematurity < 29 weeks’ gestation, congenital diaphragmatic hernia, stroke, and antenatally diagnosed fetal conditions would be higher in 2017. To adjust for six multiple comparisons, a Bonferroni correction was made and a p value of < 0.008 was chosen to be significant.
RESULTS
There were 23 of 26 (88%) respondents.
2017 Tertiary Canadian Neonatal Follow-Up Network practices
Services offered by CNFUN sites are shown in Table 1. As expected, services included neurodevelopmental assessment, screening and referral for intervention at all sites. Patient advocacy (96%), parent education or support (87%), health care professional teaching (91%), and audit or research (87%) was provided by most of these NFUPs. Treatment interventions were provided by fewer sites: 52% provided some physiotherapy and occupational therapy and 30% psychology interventions. Collaboration with community and rehabilitation services were provided with brochures or written materials in 52%, 3 (13%) programs had joint intake meetings with community care providers and one site organized tours of community and rehabilitation facilities for families.
Table 1.
Canadian neonatal follow-up programs services
| Clinical services | 2017 n=23 |
|---|---|
| Medical evaluation | 16 (70%) |
| Neurodevelopmental evaluation | 23 (100%) |
| Referral to rehabilitation services | 23 (100%) |
| Caregiver support/education/coaching | 20 (87%) |
| Patient advocacy | 22 (96%) |
| Child interventions | |
| General medical care | 8 (35%) |
| Physio/Occupational therapy interventions | 12 (52%) |
| Psychology interventions | 7 (30%) |
| Education interventions | 4 (17%) |
| Research/Data collection: | |
| Data collection for quality improvement | 19 (83%) |
| Data collection for research | 20 (87%) |
| Health care professionals teaching/ training | 21 (91%) |
Canadian NFUPs reported a wide spectrum of eligibility criteria (Table 2). Prematurity and low birth weight criteria were frequently used but the gestational age and birth weight threshold criteria varied. Neurological conditions associated with neurodevelopmental impairment in both preterm and term born children, especially hypoxic ischemic encephalopathy, were eligibility criteria at 91% of sites.
Table 2.
Eligibility criteria in Canadian neonatal follow-up programs
| Criteria | 2006 | 2017 | |
|---|---|---|---|
| Gestational Age Criteria: | 47% | 91% | |
| (upper threshold): | <29 to ≤33 weeks | 26%a | 65%a |
| <28 weeks | 16% | 22% | |
| <25 weeks | 5% | 4% | |
| Birth Weight Criteria | 84% | 91% | |
| (upper threshold): | <2,000 g | 0% | 0% |
| <1,500 g | 47% | 43% | |
| <1,250 g | 26% | 35% | |
| <800 g or <1,000 g | 10% | 13% | |
| Neurologic Criteria: | |||
| Intraventricular hemorrhage | 63% | 83% | |
| Periventricular leukomalacia | 42% | 83% | |
| Hypoxic ischemic encephalopathy | 63% | 91% | |
| Seizures | 32% | 56% | |
| Hyperbilirubinemia | 21% | 65% | |
| Stroke | 5%b | 87%b | |
| Cardio-Respiratory Criteria | |||
| Bronchopulmonary dysplasia | 32% | 56% | |
| Persistent pulmonary hypertension newborn | 16% | 30% | |
| Congenital diaphragmatic hernia | 21%c | 65%c | |
| Congenital heart disease | 5% | 39% | |
| Shock | 5% | 22% | |
| ECMO | 10% | 52% | |
| Other Criteria: | |||
| Small for Gestational Age | 32% | 39% | |
| Maternal Substance Use | 26% | 17% | |
| Antenatally Diagnosed Conditions & Therapies | 5%d | 52%d |
ECMO Extracorporeal membrane oxygenation.
aP=0.01, bP<0.00001, cP=0.004, dP=0.001.
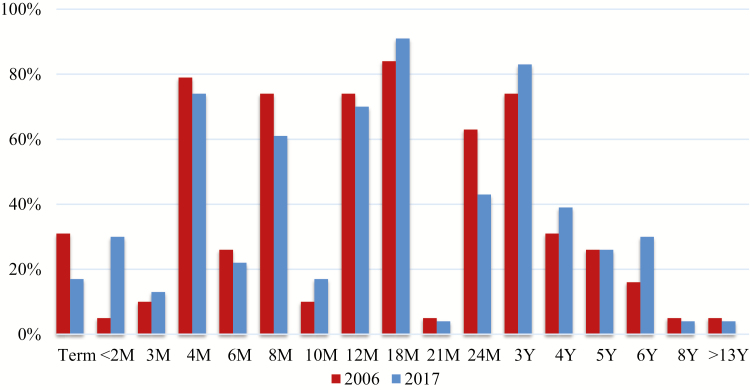
The schedule of follow-up visits is shown in Figure 1. Most NFUPs (>70%) provided between 5 and 7 follow-up visits (range 3 to 10). One-third of centres (35%) offered school age visits (≥6 years) whereas the remainder discharged patients between 18 months and 5 years of age. The timing of visits continued to vary except for the 18-month visit which was offered by 91% of CNFUN sites.
Figure 1.
Neonatal follow-up schedule of visits in Canada.
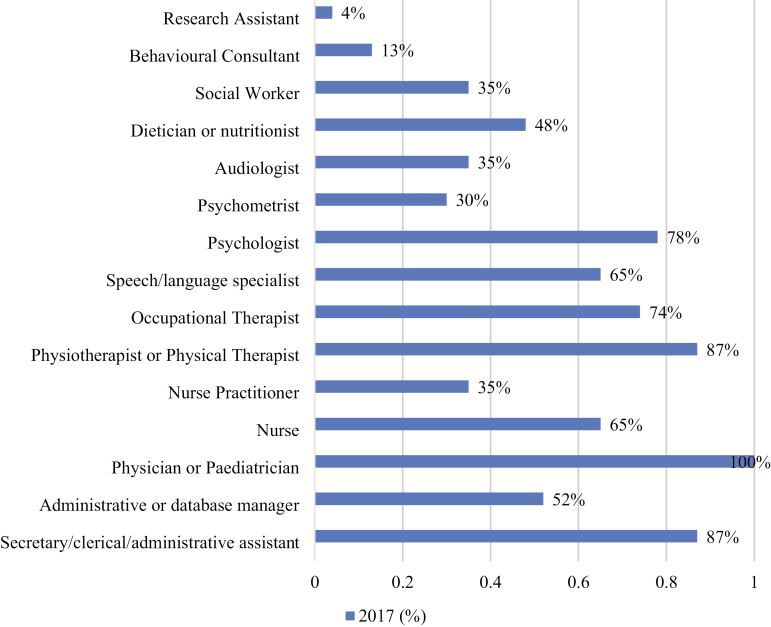
Tertiary level NFUPs were multidisciplinary as shown in Figure 2. The average number of professional services employed by a NFUP was 8 (range 3 to 13) with, on average, three additional professional services available on a consultant basis (range 0 to 10).
Figure 2.
Canadian NFU programs team members and health disciplines.
The scope of assessments provided by the multidisciplinary teams encompassed the general health and neurodevelopment of the child and caregiver mental health and well-being. Child motor (gross and fine) and cognitive abilities were the most common neurodevelopmental domains assessed. Speech and language, psychology, adaptive behaviour, quality of life, vision, and hearing were part of the standard assessment in less than half of CNFUN sites. Screening for caregiver mental health was routine in 61% of NFUPs. The variety of standardized assessment tools used by Canadian NFUPs in 2017 is shown in Table 3. The Bayley Scales of Infant and Toddler Development 3rd edition is the CNFUN standardized developmental assessment tool. The Bayley Scales, used by 74%, and the Alberta Infant Motor Scales (70%) were the only assessment tools used by more than half of sites in 2017.
Table 3.
Assessments undertaken by neonatal follow-up programs
| Assessment | 2006 | 2017 | Age range* |
|---|---|---|---|
| Motor Standardized Assessment | 22/23 (96%) | ||
| Bayley Scales of Infant Development | 4/19 (21%)a | 17/23 (74%)a | 1–42 months |
| Alberta Infant Motor Scales | 8/19 (42%) | 16/23 (70%) | 0–18 months |
| Peabody Developmental Motor Scales | 8/19 (42%) | 5/23 (22%) | 0–5 years |
| Gross Motor Function Classification System | 0/19 (0%) | 6/23 (26%) | 18 months – 8 years |
| Cognitive Standardized Assessment | 20/23 (87%) | ||
| Bayley Scales of Infant Development | 4/19 (21%)b | 19/23 (83%)b | 1–42 months |
| Wechsler Preschool & Primary Scales of Intelligence | 4/19 (21%) | 8/23 (35%) | 2 years 6 months – 7 years 7 months |
| Behavior Rating Inventory of Executive Function- Preschool | 0/23 (0%) | 5/23 (22%) | 2.0–5 years 11 months |
| Stanford-Binet | 5/19 (26%) | 0/23 (0%) | 2 years–adult |
| Speech and Language Standardized Assessment | 11/23 (48%) | ||
| Rossetti Infant Toddler Language Scale | 2/19 (11%) | 4/23 (17%) | 0–3 years |
| Preschool Language Scale | 0/19 (0%) | 3/23 (13%) | 0–7 years 11 months |
| Expressive One-Word Picture Vocabulary Test | 1/19 (5%) | 2/23 (9%) | 2-year adult |
| Communication and Symbolic Behavior Scales | 0/19 (0%) | 1/23 (4%) | 6–24 months |
| Adaptive Behavior Standardized Assessment | 11/23 (48%) | ||
| Ages and Stages Questionnaire | 0/19 (0%) | 8/23 (35%) | 2–60 months |
| Vineland Adaptive Behavior Scales | 2/19 (11%) | 3/23 (13%) | 0-adult |
| Adaptive Behavior Assessment System | 0/19 (0%) | 2/23 (9%) | 0-adult |
| Psychological Well-being Standardized Assessment | 11/23 (48%) | ||
| Child Behavior Checklist-preschool | 3/19 (16%) | 7/23 (30%) | 1.5–5 years |
| Modified Checklist for Autism in Toddlers | 0/19 (0%) | 3/23 (13%) | 16–30 months |
| Connors Rating Scale/Parent Rating Scale | 3/19 (16%) | 3/23 (13%) | 6–18 years |
| Others | |||
| History/Physical Exam/Growth | 23/23(100%) | All ages | |
| Hearing | 11/23 (48%) | All ages | |
| Visual | 9/23 (39%) | All ages | |
| Screening for caregiver’s mental health | 14/23 (61%) | All ages | |
| Child quality of life | 2/23 (9%) | 8–18 years |
*Age range for which the most current edition is valid aP=0.001, bP=0.0001.
Most NFUPS were funded publicly by divisions of neonatology, hospital operational funding, or regional health programs. One quarter of sites received additional funding from research studies in 2017.
Comparisons between 2006 and 2017 tertiary NFUP practices
Compared to 2006, in 2017, more CNFUN sites (65% versus 26%, P=0.01) identified a gestational age threshold of < 29 weeks’ or greater as a recruitment criteria (Table 2). Neurologic, cardio-respiratory and other miscellaneous eligibility criteria were used more frequently in 2017. Newborns with stroke (P<0.00001), congenital diaphragmatic hernia (P=0.004), or antenatally diagnosed conditions (P=0.001) were recruited at more sites. Since 2006, the proportion of CNFUN sites offering an 18-month visit increased from 84% to 91% in 2017 (Figure 1) with a decrease in the number of 2-year-old visits (63% versus 43%). Slightly more centres were assessing children at 3 years (74% versus 83%) and the number of centres with a school age assessment increased twofold, from 16% to 30%. The use of the Bayley Scales increased significantly from 21% to 83% (P=0.001) and the use of the Alberta Infant Motor Scales increased from 42% to 70% (Table 3).
Discussion
This survey captured 88% of tertiary level Canadian NFUPs which provided a comprehensive picture of current practices and changes that occurred in the last decade. Significant increases in the proportion of NFUPs administering the Bayley-III and recruitment for a gestational age less than 29 weeks’ occurred after CNFUN initiated data collection. Increased recruitment for children with congenital diaphragmatic hernia is supported by published recommendations (9).
Though this study was prompted by, and is of great interest to staff and administrators of NFUPs, the results are also useful to paediatricians interested in health care services delivery. A multidisciplinary model of care which provides clinical care, audit, research and education in a unified setting can be applied to other settings. Standardized follow-up has many potential benefits. In the spirit of the 1984 Canada Health Act, health services should be comprehensive, universal, portable, and accessible to all Canadians (10). NFUP clinical services should therefore be similar across Canada. Audit with benchmarking, a key component of quality improvement initiatives, requires standardized data collection and reporting. Large obstetric and neonatal multicentre trials with long-term infant outcomes have been possible because of the NFUP infrastructure.
The NFUP community of health care providers recognized the benefits of collaboration and standardization but were unable to reduce variability between 1987 and 2006. After CNFUN introduced a national 18-month visit, with some research funding, improvement was noted with 91% of CNFUN site respondents offering an 18-month CA visit and 74% using the Bayley-III in 2017. CNFUN has demonstrated risk adjusted site variation in neurodevelopmental rates (7). The Canadian Neonatal NetworkTM has used site variations in short term morbidities to successfully improve neonatal outcomes (11) and CNFUN is now striving to do the same with longer term outcomes.
In Ontario, the PCMCH Neonatal Follow-Up Clinics Work Group developed guidelines for a cohesive system of tertiary and secondary neonatal follow-up in 2017 (8). The effectiveness of collaborative provincial ministry of health initiatives on standardizing care will be of interest. Little is known about secondary level NFUPs that are responsible for lower-risk infants.
Though an 88% response rate is excellent for a survey, information was not obtained from three NFUPs who may have found the comprehensive nature of the survey too lengthy. The small number of sites and exploratory nature of the study limited the number of statistical comparisons. Statistical analyses were therefore limited to a few targeted questions and a correction for multiple comparisons was made.
The lack of evidence to support which outcomes should be measured at which age has hampered standardization of NFUPs. Some, but not all, NFUPs have been able to change in response to existing evidence. For example, less than one half of sites assess behaviour and psychological well-being despite the increased risk of conditions such as attention deficit disorders (12) and autism (13) in the very preterm population. There is a need to identify the role of various health care providers in screening for these conditions. Future evidence based research to identify the paediatric outcomes that key stakeholders identify as most important, the best assessment tools to measure those outcomes and collaborative provincially led working groups, such as the Ontario PCMCH, are likely to improve standardized follow-up care.
CONCLUSION
This comprehensive survey of Canadian NFUPs demonstrates the considerable variations in infrastructure and practices between sites. Introduction of a national standard assessment for children born very preterm likely increased use of the Bayley-III as a standard measure of development at 18 months CA. New recommendations for neonatal follow-up by an Ontario provincial council may further reduce the variation in Canadian NFUPs but this will need to be evaluated.
Contributors’ statements: FA implemented the study, wrote the initial manuscript, and approved the final manuscript as submitted. PC was a CNFUN steering committee member while the study was conducted and approved the final manuscript as submitted. MB was a CNFUN steering committee member while the study was conducted and approved the final manuscript as submitted. AG developed the first draft of the survey and approved the final manuscript as submitted. AS is the founding Director of the CNFUN, conceptualized and supervised the study, edited the initial manuscript, and approved the final manuscript as submitted.
Funding: There are no funders to report for this submission.
Potential Conflicts of Interest: AG performed part of the work for this study while funded by the CIHR team grant in Maternal Infant Care that supported the Canadian Neonatal Follow-up Network. There are no other reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Ballantyne M, Stevens B, Guttmann A, Willan AR, Rosenbaum P. Transition to neonatal follow-up programs: Is attendance a problem? J Perinat Neonatal Nurs 2012;26(1):90–8. [DOI] [PubMed] [Google Scholar]
- 2. Kuppala VS, Tabangin M, Haberman B, Steichen J, Yolton K. Current state of high-risk infant follow-up care in the United States: Results of a national survey of academic follow-up programs. J Perinatol 2012;32(4):293–8. [DOI] [PubMed] [Google Scholar]
- 3. Bockli K, Andrews B, Pellerite M, Meadow W. Trends and challenges in United States neonatal intensive care units follow-up clinics. J Perinatol 2014;34(1):71–4. [DOI] [PubMed] [Google Scholar]
- 4. Hanvey L Neonatal follow-up in Canada: Report of a survey, 1987. In: Feldman W, Paré C, eds. Neonatal Follow-up Programs in Canada. Proceedings of Ross Conference in Paediatrics. Montreal: Ross Laboratories, Division of Abbott Laboratories Ltd, 1987. [Google Scholar]
- 5. Cake HA, Jangaard K, Pelausa E, Sampson D, Vincer M. A survey of Canadian perinatal follow-up programs. Paediatr Child Health. 1997;2Suppl 1:51A. [Google Scholar]
- 6. Synnes AR, Lefebvre F, Cake HA. Current status of neonatal follow-up in Canada. Paediatr Child Health 2006;11(5):271–4. [PMC free article] [PubMed] [Google Scholar]
- 7. Synnes A, Luu TM, Moddemann D, et al. Determinants of developmental outcomes in a very preterm Canadian cohort. Arch Dis Child Fetal Neonatal Ed. 2017;102:F235. [DOI] [PubMed] [Google Scholar]
- 8. Final Report of the Neonatal Follow-Up Clinics Work Group [Internet]. Provincial Council for Maternal and Child Health; 2015. May. http://www.pcmch.on.ca/wp-content/uploads/2015/09/NFUC-Final-Report_15-06-02.pdf (Accessed November 13, 2019). [Google Scholar]
- 9. The Canadian Congenital Diaphragmatic Hernia Collaborative. Diagnosis and management of congenital diaphragmatic hernia: A clinical practice guideline. CMAJ. 2018;190: E103–E112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Canada Health Act-Annual Report 2017–2018. https://www.canada.ca/en/health-canada/services/publications/health-system-services/canada-health-act-annual-report-2017-2018.html (Accessed November 13, 2019).
- 11. Lee SK, Aziz K, Singhal N, et al. Improving the quality of care for neonates: A cluster randomized controlled trial. CMAJ 2009; 181:469–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Aylward GP Neurodevelopmental outcomes of infants born prematurely. J Dev Behav Pediatr 2005;26(6):427–40. [DOI] [PubMed] [Google Scholar]
- 13. Pritchard MA, Dassel T, Beller E, et al. Autism in toddlers born very preterm. Pediatrics. 2016;137:e20151949. [DOI] [PubMed] [Google Scholar]