Abstract
The complexity of cirrhosis requires patients and their caregivers to be well educated to improve outcomes. Data are lacking regarding how to best educate patients and their caregivers in the setting of cirrhosis. Our aim is to understand (both through existing literature and by asking patients and their caregivers) how patients learn about their disease, barriers in their education and disease management, and self‐management strategies. We performed a structured search of published articles in PubMed (1973 to 2020) using keywords “cirrhosis” plus “barriers”, “education”, “self‐management”, or “self‐care”. Additionally, we conducted a focus group of a representative sample of patients and their caregivers to understand how knowledge about cirrhosis is found and incorporated into self‐management. Of 504 returned manuscripts, 11 pertained to barriers in cirrhosis, interventions, or educational management. Barriers are well documented and include disease complexity, medication challenges, comorbid conditions, and lack of effective education. However, data regarding addressing these barriers, especially effective educational interventions, are scarce. Current strategies include booklets and videos, patient empowerment, and in‐person lectures. Without widespread use of these interventions, patients are left with suboptimal knowledge about their disease, a sentiment unanimously echoed by our focus group. Despite linkage to subspecialty care and consistent follow‐up, patients remain uncertain about their disease origin, prognosis, and therapies to manage symptoms. It is clear that more data are needed to assess effective strategies to address unmet educational needs. Existing strategies need to be blended and improved, their effectiveness evaluated, and the results distributed widely.
Cirrhosis is increasingly common and morbid. Deaths due to cirrhosis have risen by at least 65% since 2009, and hospitalization rates for cirrhosis now exceed those for congestive heart failure.( 1 , 2 ) Complicating the increasing burden of cirrhosis is the complexity of the condition and its medical management.( 3 ) Ascites requires close monitoring, dietary modification, and adjunctive diuretic therapy that requires frequent dose adjustment; hepatic encephalopathy is often unpredictable, reduces one’s ability to effectively self‐care, yet depends on insight regarding one’s symptoms to guide frequent lactulose dose adjustment; pain is frequently comorbid, and concerns over medication safety increase anxiety while limiting the efficacy of pain‐control strategies. This complexity demands substantial support and rapid “on‐the‐job” training in cirrhosis management for patients and caregivers. Implementation of provider‐recommended screening, diet, and medication management is imperfect, likely in part due to failures in patient and caregiver education. We therefore sought to describe the barriers to optimal patient education for persons with cirrhosis and strategies for improvement. To this end, we reviewed the literature on patient education and also conducted a focus group with patients to identify their unmet needs and desired solutions. Our goal was to compile and synthesize these data from existing literature and to understand efforts being made to deconstruct these barriers to improve care for our patients.
Materials and Methods
Literature Review
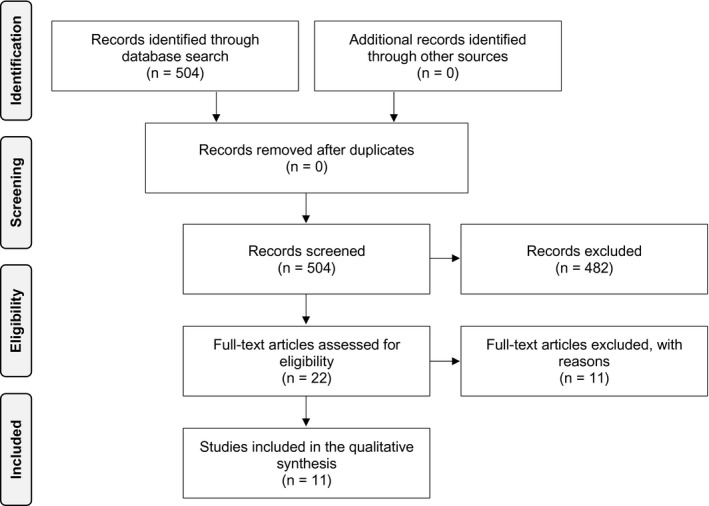
We first conducted a structured literature review. We searched PubMed by combining “cirrhosis” with keywords, including “barriers”, “education” (Medical Subject Headings term), “self‐management”, and “self‐care”, which returned 504 results from December 1973 to January 2020. All results were analyzed for mentions of 1) barriers to care, 2) interventions that have been investigated in improving care, and 3) models to educate patients with cirrhosis. Of those, 482 manuscripts matched but did not pertain to the barriers, interventions, or educational models in cirrhosis. Of the remaining manuscripts, four discussed barriers, four discussed interventions, and three discussed education in the context of cirrhosis. Additionally, each of the full‐text articles was scanned for references that matched the themes of this paper.
PRISMA Diagram, Source: Moher et al.( 24 )
Focus Group
We next conducted a focus group. We contacted a random purposive selection of 38 patients with cirrhosis who had recent outpatient visits to the Hepatology (nontransplant) clinic at the University of Michigan to participate in a 2‐hour focus group for patients and caregivers in June 2019. A total of 11 patients and caregivers attended. Patients and their caregivers were offered dinner as thanks for participating. A semistructured interview guidebook was developed before the meeting that had input from hepatologists, nurses, social workers, and pharmacists (see Supporting Materials). Facilitation questions addressed patients’ experiences with cirrhosis education, current knowledge of cirrhosis management, and desired aspects of a future patient education model. Our current patient education practice is at the discretion of each clinician with verbal education and/or handouts. The proceedings were recorded by four independent reviewers who routinely conduct focus groups with patients as part of patient education program development and quality improvement. Their notes were combined and examined for consistent themes. Multiple coders (Z.S., E.T.) evaluated the notes to distill themes with differences reconciled by a third reviewer (K.G.). The review of this study for quality improvement was institutional review board exempt.
Results
Literature Review
Many of the barriers to self‐management faced by patients with cirrhosis are detailed in Table 1. Patients with cirrhosis have a high average number of medications (from seven to 10),( 4 , 5 ) many of which require monitoring and titration,( 3 ) which likely contributes to the low rates of medication adherence described in the literature.( 6 ) Long medication lists combined with frequent discrepancies between the patients’ listed prescriptions and their actual regimen( 4 ) lead to a cluster of barriers to self‐management. The incidence of medicine‐related problems can approach 40% in patients with cirrhosis.( 7 )
TABLE 1.
Patient Barriers to Self‐Management of Their Cirrhosis
| Barriers to Self‐Management | ||
|---|---|---|
| Barrier | Description | Intervention |
| Disease complexity | Cirrhosis and its management are complex even for hepatologists. | Education improvement |
| High number of medications | Average number of medications can approach seven to 10 in patients with cirrhosis.( 4 , 5 ) | Reduce PIMs; |
| primary care collaboration | ||
| High medication complexity | Many medications in this patient population have variable dosing frequencies and the need to be frequently titrated (diuretics, lactulose, beta blockers).( 3 ) | Education improvement; |
| primary care collaboration | ||
| Low medication adherence | Over half of patients with cirrhosis report missing one or more doses of their medications each month.( 6 ) | Education improvement |
| Faulty medication reconciliation | Patients often have multiple prescribing providers with discrepancies between the prescribed regimen and what the patient is actually taking in more than 50% of patients.( 3 ) | Primary care collaboration |
| Managing comorbid conditions | Therapies for common comorbid conditions put patients with cirrhosis at higher risk for adverse effects (analgesics for pain, PPIs for PUD, statins for cardiovascular disease).( 3 ) | Education improvement; |
| primary care collaboration | ||
| Lack of education | Over 50% of patients cannot provide a meaningful definition of cirrhosis, its long‐term complications, or warning signs of worsening disease.( 8 ) | Education improvement |
| Misconceptions | Patients commonly believe HCC screening is not indicated with a healthy diet (47%) or with a normal exam/without symptoms (34%). Misperceptions lead to lower screening adherence.( 16 ) Many misconceptions exist, but their impact on outcomes is to be determined.( 7 ) | Education improvement |
| Cognitive impairment | Concomitant hepatic encephalopathy is associated with a lower health‐related quality of life( 9 ) and affects patients’ and their caregivers’ abilities to manage their disease. | Optimized therapy |
| Ongoing alcohol use | Patients with cirrhosis and ongoing alcohol use are less likely to use available resources to learn about their disease and its management.( 8 ) | Education improvement; |
| Addiction counseling; | ||
| AUDIT‐C screening | ||
| Comorbid depression | 56%‐64% of patients with cirrhosis have comorbid depression,( 10 , 11 ) which has been linked to impaired self‐management and reduced adherence to treatment in other chronic diseases.( 11 , 12 ) | Psychiatry collaboration; |
| optimized therapy; | ||
| PHQ‐9 screening | ||
| Lack of chronic disease management programs | Standardized programs improve quality of care, adherence to screening and prevention guidelines, and clinic attendance rates.( 17 ) | Program creation |
| Socioeconomic status | Lower socioeconomic status has a clear negative impact on survival in patients with cirrhosis.( 14 ) | Social work collaboration |
Abbreviations: AUDIT‐C, Alcohol Use Disorders Identification Test‐Concise; HCC, hepatocellular carcinoma; PHQ‐9, Patient Health Questionnaire‐9; PIMs, potentially inappropriate medications; PPI, proton pump inhibitor; PUD, peptic ulcer disease.
To make medication adherence even more challenging, many patients with cirrhosis have cognitive impairment secondary to hepatic encephalopathy, ongoing alcohol use, or comorbid depression, all of which translates to reduced ability to manage their cirrhosis.( 8 , 9 , 10 , 11 ) It is also apparent that these patients lack the knowledge or resources to address some of these cognitive and mental health barriers, as evidenced by the misconceptions and perceived lack of benefit surrounding alcohol use‐disorder treatment( 12 ) and the small percentage of patients (19%‐56%) familiar with lactulose titration.( 13 , 14 ) Additionally, lower socioeconomic status is a barrier that negatively correlates with outcomes in cirrhosis.( 15 )
These barriers are compounded by our lack of effective disease education( 16 ) and disease management programs( 17 ) to help patients overcome these barriers. In an interview study of 50 patients admitted for a complication of cirrhosis, 79% were interested in using a digital health management tool that could provide information about cirrhosis and 75% were interested in more education on a low‐salt diet.( 18 )
Few cirrhosis education programs were described in our literature review (Table 2), and the ones that exist demonstrated improvement on a small scale. Volk et al.( 13 ) administered a knowledge assessment questionnaire to 115 patients before and after an educational intervention (concise educational booklet), with scores increasing from 53% to 67% before and after intervention, respectively. Goldworthy et al.( 19 ) demonstrated the utility of a video‐based educational intervention, improving knowledge assessment questionnaires from 25.0% to 66.7% before and after intervention, respectively. Zhang et al.( 20 ) showed that modifying patient education with a focus on patient empowerment yields statistically significant improvement in patient disease management knowledge and improvement in activities of daily living scores in a study of 60 patients. Zandi et al.( 21 ) found that educational sessions on the nature of cirrhosis, coping strategies for symptoms/comorbidities, and therapies for treatment side effects resulted in increased patient quality of life and decreased fatigue, anxiety, and abdominal symptoms.
TABLE 2.
Summary of Educational Interventions and Their Outcomes in the Literature for Patients With Cirrhosis
| Author | Aim | Population | Educational Intervention | Methods | Outcome |
|---|---|---|---|---|---|
| Beg et al.( 8 ) | To assess baseline knowledge in patients, and the impact of an informational leaflet on their cirrhosis knowledge base | n = 39 | Informational leaflet | Before and after intervention knowledge questionnaire | Baseline knowledge was poor (mean score 3.4 out of 9 points), improved to 7.5 after intervention (P = 0.0006) |
| Compensated and decompensated | |||||
| Goldworthy et al.( 19 ) | To assess baseline knowledge in patients, and the impact of an informational video on their cirrhosis knowledge base | n = 52 | Informational video | Before and after intervention knowledge questionnaire | Baseline knowledge was poor (median score 25.0%), improved to 66.7% after intervention (P < 0.001) |
| Compensated and decompensated | |||||
| Hayward et al.( 22 ) | To assess receptiveness and retention to an informational booklet | n = 50 | Informational booklet | After intervention cued‐recall questionnaire | Most patients found the booklet helpful (85%) and reported using it (78%), but retention was poor (mean score 8.1 out of 13) |
| Compensated and decompensated | |||||
| Volk et al.( 13 ) | To understand and improve patient knowledge about cirrhosis self‐management | n = 150 | Informational booklet | Before and after intervention knowledge questionnaire | Baseline knowledge was poor (median score 53%), improved to 67% after intervention (P < 0.001). All questions were answered correctly more frequently after intervention. |
| Compensated and decompensated | |||||
| Zandi et al.( 21 ) | To determine the effects of a self‐care educational program on QoL | n = 44 | In‐person educational sessions on the nature of disease, coping strategies, relaxation techniques, diet and nutrition, and of complexities of medical therapies. | Before and after intervention QoL (as measured by the CLDQ) | QoL significantly improved after intervention in multiple domains (abdominal symptoms, fatigue, systemic symptoms, and emotional symptoms; all P = 0.001) |
| Compensated and decompensated | |||||
| Zhang et al.( 20 ) | To evaluate the effect of education using health empowerment theory on ADL and patient knowledge in hospitalized patients | n = 30 | Incorporating health empowerment theory into patient education | Study group with intervention versus control group without; effect on ADL (Barthel Index score) and disease knowledge questionnaire | Understanding of major clinical symptoms, etiology, diet and nutrition, use of medication, treatment, and disease awareness were higher in the study group on discharge (P < 0.05) as were ADL scores at 2‐month follow‐up (81.5 vs. 68.5; P = 0.006) |
| Compensated and decompensated |
Abbreviations: ADL, activities of daily living; CLDQ, chronic liver disease questionnaire; QoL, quality of life.
Focus Group
Common patient knowledge gaps observed in our focus group, their experiences with cirrhosis education, and potential solutions for areas of concern are outlined in Table 3. Participants were uniformly distressed about not understanding which factors led to their development of cirrhosis and its complications. Patients felt unsure of their prognosis. Multiple patients reported being told they were “on a cliff,” but some had heard this phrase years before. Many wondered why they could not be told the percentage of their liver function and why they were not offered biopsies to stage their cirrhosis; 1 participant reported finding indocyanine green clearance testing online and requesting it from the hepatologist. Most participants voiced concern that they did not know how to safely treat musculoskeletal and neuropathic pain, reporting frustrations with conflicting opinions from multiple providers. Similarly, participants were frustrated by a lack of clarity regarding which foods and exercises were safe. Caregivers expressed the need to know anything the patient needed to know and reiterated the need for clear discussions regarding prognosis. Caregivers also specifically felt that they needed education about symptoms to watch for and how to administer medications.
TABLE 3.
Patient and Caregiver Concerns About Their Health and Their Experiences With Education About Their Disease During a Structured Focus Group
| Themes | Consensus Needs | Contrasting Opinions | Solutions | |
|---|---|---|---|---|
| Concerns about their heath | Difficulty understanding disease origin | Clear explanation of cirrhosis etiology. | None | Standard illustrations covering “Basics of Cirrhosis.” |
| “Why me? Why does cirrhosis develop?” | New “Expand your Knowledge” resources: available videos with patient testimonials or links to additional reading in patient portal. | |||
| Tools to explain cirrhosis to family and friends. | ||||
| Risk of disease in family members (transmission and genetic basis). | ||||
| Uncertainty regarding prognosis | Uncertainty about prognosis. | None | Illustrated document covering spectrum of chronic liver disease to decompensated cirrhosis, including often unpredictable course of disease. | |
| “How long until I become sicker?” | “Expand your Knowledge” resources. | |||
| “Do I have months or years to live?” | ||||
| How cirrhosis affects other medical problems. | ||||
| Why decompensation happens. | ||||
| When patients need a liver transplant. | ||||
| Uncertainty regarding diagnostics and therapeutics | Pain control in cirrhosis. | None | Pocket cards covering safe pain control strategies, diet and exercise recommendations, and recurring tests (e.g., ultrasound, upper endoscopy). | |
| “What can I use for pain control?” | Multidisciplinary clinic visits with nutritionist and pharmacist consultation. | |||
| Health and diet in cirrhosis. | ||||
| “Is exercise safe? Is there a liver diet?” | ||||
| Understanding cirrhosis health maintenance testing. | ||||
| Experiences with education | Written education | High‐quality color diagrams including stages of cirrhosis, physiology, and prognosis. | Some reported simply throwing away written resources. | Clear language in clinic notes available to patients online. |
| in the health care system | Centralized, searchable resources with hyperlinks for greater detail. | Standard illustrations covering “Basics of Cirrhosis.” | ||
| Insight into medical decision‐making process. | Create videos with patients sharing hopeful stories. | |||
| Patient “Quick Guides” | Simple list of “things to avoid” with cirrhosis. | Some patients would like explanations in addition to quick list. | Pocket cards covering safe pain control, diet, and exercise recommendations, and recurring tests (e.g., ultrasound, upper endoscopy). | |
| Mnemonics preferred. | ||||
| Verbal education | Highlights given verbally, and detailed information available in writing. | All pertinent information to be provided during visit discussion. | Query education preference: mostly verbal vs. written. | |
| Diagrams clinicians annotate during the clinic visit. | ||||
| “Expand your Knowledge” resources. | ||||
| Psychosocial support | Help locating patient support groups | Preference for online (“Facebook”) vs. in‐person support groups. | Create hospital support group including patient facilitators with stable disease. | |
| Connecting with patients who have “made it to the other side.” | Create videos with patients sharing how they managed their condition successfully. | |||
| Communication outside of clinic | Contact by phone important for urgent issues. | None | Ensure patients can contact clinic by phone or portal and that they understand when to use each. | |
| Patient portal also beneficial for less urgent issues. | Standardized phone call after hospital discharge. | |||
| Patients appreciate being called after hospital discharge to check‐in. |
The group agreed that current written educational materials are inadequate. Some participants said written material should be brief and direct, while others felt it should be more detailed. Most participants reported conducting their own research. By consensus, the Mayo Clinic website was felt to be the best source, followed by social media support groups, and open access journal articles searched for using keywords specific to their condition. Some voiced concern that it was their physician’s responsibility to educate them on their condition while in clinic. The group ultimately reached consensus that educational material should be succinct with optional links to more information. Many were interested in online videos of patients telling their story of diagnosis and survival or how they learned to manage their hepatic encephalopathy. All participants requested pocket reference cards for topics such as dietary instruction and pain control. Regarding verbal education, participants requested high‐level illustrated explanations given in person, using visual aids that were preprepared or even sketched on the exam table paper. Patients wanted multiple avenues of contact with the clinic (e.g., patient portal, phone) and appreciated posthospital discharge phone calls. They were interested in assistance locating support groups for patients with cirrhosis.
Discussion
Our study combines a literature review and focus group to define and outline solutions for the present needs for educational efforts in contemporary cirrhosis clinics. We have summarized our findings in a conceptual model for modernized educational efforts in cirrhosis care (Fig. 1).
FIG. 1.

What patients want. Abbreviation: NSAID, nonsteroidal anti‐inflammatory drug.
Focus Group
Education is a core clinical competency for delivering effective care. Patients with cirrhosis face large barriers to managing their disease, and our current patient education practice is not optimally helping patients overcome these barriers. Our qualitative study shows that contemporary patients and their caregivers are unsatisfied with available educational materials. Our participants shared multiple generalizable lessons. First, their key unmet needs were an understanding of the mechanisms of disease and prognosis as well as how to manage their pain and optimize their diet. Second, even where educational materials are lacking, patients are resourceful and turn to the Mayo Clinic website for information but also often read open‐access journal articles that may not apply to their cases. Third, our participants highlighted multiple ways in which they wish to receive information. Above all, patients appreciate expert clinicians who can explain their disease, particularly using charts and figures. In addition, patients prefer printed synopses with hyperlinks to more extensive online information and videos as well as clear‐cut upfront recommendations regarding pain control and diet. Fourth, patients and caregivers also want to connect with peers who can share their experiences and offer advice. They view online support groups as desirably as in‐person groups.
These findings must be interpreted in the context of the study design. Our data are derived from a small single‐center sample at risk for selection bias toward healthier patients able to attend. This was also a well‐informed group with self‐reported high confidence in managing their health problems. Notwithstanding this, clear knowledge gaps were identified.
Literature Review
Despite these gaps in our patient education practice, based on our literature review, few scientific data are available regarding existing educational interventions and their effectiveness. Most interventions documented in the literature are performed within small cohorts, and follow‐up studies assessing their impact on quality of life, clinical outcomes, and patient satisfaction are lacking. It is also unclear whether the studied interventions were implemented on a grander scale to benefit a larger number of patients. Hepatologists must address how patients and their caregivers want to learn and be supported outside of the traditional clinic model and formally evaluate clinical and patient satisfaction outcomes regarding these interventions to address our current system’s shortcomings.
On the other hand, the barriers to effective self‐care in cirrhosis are well documented. At present, data regarding addressing these barriers through education (or other interventions) are limited.
Future Directions
Our focus group suggests that patients and their caregivers crave more robust education regarding cirrhosis. This notion is echoed by Hayward et al.,( 22 ) where 64% of a 50‐patient cohort felt they needed to turn to external resources for their education. Half of these patients reported that they still were unable to locate the information they desired. What changes do we make to our current education practice to ensure patients are able to receive the knowledge they desire while simultaneously limiting the amount of externally sought (and unfiltered) information?
Our educational system must be revamped to address 1) knowledge gaps, 2) barriers to care, 3) varying patient preferences, 4) poor knowledge assessment tools, and 5) a desire for peer support and education. To address knowledge gaps, we must develop an easily understood curriculum that explains cirrhosis development, disease and comorbidity management, trajectory, and prognosis. To accommodate varying patient preferences, this curriculum should have concise information that can be quickly read but also accompanying expansive information to satisfy patient curiosity for more information. It must address the barriers to care detailed in Table 1 by providing descriptions and methods for overcoming them (whether by self‐interventions or collaborating with other physicians). To further accommodate varying patient preferences, the written information must be accompanied by optional in‐person or electronic educational sessions, as described by Goldsworthy et al.( 19 , 21 ) and Zandi et al.( 19 , 21 ) Caregivers should also receive copies of the educational materials. There must be a focus on patient empowerment rather than externally imposed interventions, given its demonstrated improvement both within cirrhosis and other chronic diseases.( 20 )
Additionally, to expand implementation, we must be able to assess improvement in patient knowledge after interventions, which could involve the use of a validated knowledge‐assessment questionnaire.( 23 ) Furthermore, the educational intervention must be studied both in terms of knowledge improvement as an outcome, in addition to effect on clinical outcomes, quality of life, and patient satisfaction. Lastly, the questionnaire, educational materials, and data on outcomes must be disseminated to address the widespread patient education deficit in cirrhosis.
Supporting information
Supplementary Material
Supported by the National Institutes of Health (DK117055 to E.T.).
Potential conflict of interest Dr. Bloom consults for Synlogic. Dr. Tapper consults for Mallickrodt, Axcella, Allergan, and Kaleido; he advises Novo Nordisk, Rebiotix, and Takeda and has received grants from Valeant and Gilead. The other authors have nothing to report.
References
- 1. Tapper EB, Parikh ND. Mortality due to cirrhosis and liver cancer in the United States, 1999‐2016: observational study. BMJ 2018; 10.1136/bmj.k2817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Asrani SK, Hall L, Hagan M, Sharma S, Yeramaneni S, Trotter J, et al. Trends in chronic liver disease‐related hospitalizations: a population‐based study. Am J Gastroenterol 2019;114:98‐106. [DOI] [PubMed] [Google Scholar]
- 3. Thomson MJ, Lok AS, Tapper EB. Optimizing medication management for patients with cirrhosis: evidence‐based strategies and their outcomes. Liver Int 2018;38:1882‐1890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hayward KL, Valery PC, Martin JH, Karmakar A, Patel PJ, Horsfall LU, et al. Medication beliefs predict medication adherence in ambulatory patients with decompensated cirrhosis. World J Gastroenterol 2017;23:7321‐7331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kuo SZ, Haftek M, Lai JC. Factors associated with medication non‐adherence in patients with end‐stage liver disease. Dig Dis Sci 2017;62:543‐549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Polis S, Zang L, Mainali B, Pons R, Pavendranathan G, Zekry A, et al. Factors associated with medication adherence in patients living with cirrhosis. J Clin Nurs 2016;25:204‐212. Erratum in: J Clin Nurs 2017;26:3751. [DOI] [PubMed] [Google Scholar]
- 7. Cheema E, Al‐Aryan A, Al‐Hamid A. Medicine use and medicine‐related problems in patients with liver cirrhosis: a systematic review of quantitative and qualitative studies. Eur J Clin Pharmacol 2019;75:1047‐1058. [DOI] [PubMed] [Google Scholar]
- 8. Beg S, Curtis S, Shariff M. Patient education and its effect on self‐management in cirrhosis: a pilot study. Eur J Gastro Hepatol 2016;28:582‐587. [DOI] [PubMed] [Google Scholar]
- 9. Montagnese S, Bajaj JS. Impact of hepatic encephalopathy in cirrhosis on quality‐of‐life issues. Drugs 2019;79(Suppl.1):11‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bianchi G, Marchesini G, Nicolino F, Graziani R, Sgarbi D, Loguercio C, et al. Psychological status and depression in patients with liver cirrhosis. Dig Liver Dis 2005;37:593‐600. [DOI] [PubMed] [Google Scholar]
- 11. Singh N, Gayowski T, Wagener M, Marino I. Depression in patients with cirrhosis. Impact on outcome. Dig Dis Sci 1997;42:1421‐1427. [DOI] [PubMed] [Google Scholar]
- 12. Mellinger JL, Scott Winder G, DeJonckheere M, Fontana RJ, Volk ML, Lok ASF, et al. Misconceptions, preferences and barriers to alcohol use disorder treatment in alcohol‐related cirrhosis. J Subst Abuse Treat 2018;91:20‐27. [DOI] [PubMed] [Google Scholar]
- 13. Volk ML, Fisher N, Fontana RJ. Patient knowledge about disease self‐management in cirrhosis. Am J Gastroenterol 2013;108:302‐305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dong N, Chen W‐T, Bao M, Lu Y, Qian Y, Lu H. Self‐management behaviors among patients with liver cirrhosis in Shanghai, China: a cross‐sectional study. Clin Nurs Res 2020;29:448‐459. [DOI] [PubMed] [Google Scholar]
- 15. Jepsen P, Vilstrup H, Andersen PK, Sørensen HT. Socioeconomic status and survival of cirrhosis patients: a Danish nationwide cohort study. BMC Gastroenterol 2009;9:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Farvardin S, Patel J, Khambaty M, Yerokun OA, Mok H, Tiro JA, et al. Patient‐reported barriers are associated with lower hepatocellular carcinoma surveillance rates in patients with cirrhosis. Hepatology 2017;65:875‐884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wigg AJ, McCormick R, Wundke R, Woodman RJ. Efficacy of a chronic disease management model for patients with chronic liver failure. Clin Gastroenterol Hepatol 2013;11:850‐858.e1‐e4. [DOI] [PubMed] [Google Scholar]
- 18. Bloom PP, Marx M, Wang TJ, Green B, Ha J, Bay C, Chung RT, Richter JM. Attitudes towards digital health tools for outpatient cirrhosis management in patients with decompensated cirrhosis. BMJ Innov 2020:6 10.1136/bmjinnov-2019-000369. [DOI] [Google Scholar]
- 19. Goldsworthy MA, Fateen W, Thygesen H, Aldersley MA, Rowe IA, Jones RL. Patient understanding of liver cirrhosis and improvement using multimedia education. Frontline Gastroenterol 2017;8:214‐219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zhang X, Xi W, Liu L, Wang L. Improvement in quality of life and activities of daily living in patients with liver cirrhosis with the use of health education and patient health empowerment. Med Sci Monit 2019;25:4602‐4608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zandi M, Adib‐Hajbagheri M, Memarian R, Nejhad A, Alavian S. Effects of a self‐care program on quality of life of cirrhotic patients referring to Tehran Hepatitis Center. Health Qual Life Outcomes 2005;3:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hayward KL, Horsfall LU, Ruffin BJ, Cottrell WN, Chachay VS, Irvine KM, et al. Optimising care of patients with chronic disease: patient‐oriented education may improve disease knowledge and self‐management. Intern Med J 2017;47:952‐955. [DOI] [PubMed] [Google Scholar]
- 23. Ramachandran J, Woodman R, Muller K, Wundke R, McCormick R, Kaambwa B, Wigg A. Validation of knowledge questionnaire for patients with liver cirrhosis. Clin Gastroenterol Hepatol 2020;18:1867‐1873.e1. [DOI] [PubMed] [Google Scholar]
- 24. Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group . Preferred Reporting Items for Systematic Reviews and Meta‐Analyses: The PRISMA Statement. PLoS Med 2009;6:e1000097 10.1371/journal.pmed1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


