Abstract
Background:
Lamaze breathing has been widely used as a breathing training method. Nursing intervention including postural nursing, delivery ball, doula nursing, massage and psychological nursing is usually provided by nurses during labor. A number of clinical studies have investigated the effect of Lamaze breathing training combined with nursing intervention on maternal pain relief and outcomes improvement. But there were some scholars who were against it.
Methods:
Randomized controlled trials from January 2000 to November 2019 in PubMed, Cochrance Library, Medline, Web of Science, Embase, Chinese Academic Journals, Chinese Biomedical Literature Database, VIP Database, Wanfang Database were searched. Two researchers independently screened the literature according to the criteria. After extracting the data, the researchers used Cochrane system to evaluate the literature quality. Statistical analyses were performed by using Comprehensive Meta Analysis V2 software.
Results:
Twenty-two randomized controlled trials conducted on 7035 primiparas were eligible. The results revealed that Lamaze breathing training combined with nursing intervention increased the rate of natural delivery (relative risk [RR] = 2.97, 95% confidence interval [CI] [2.48, 3.56]), shortened the length of labor (−2.604, 95% CI [−3.120, −2.087]), alleviated labor pain (RR = 0.194, 95% CI [0.115, 0.325]) and reduced postpartum bleeding (−2.966, 95% CI [−4.056, −1.877]).
Conclusions:
Lamaze breathing training combined with nursing intervention was effective for ameliorating the process and outcomes of childbirth in primiparae and deserves to be promoted and applied in clinical practice.
Keywords: delivery, Lamaze, meta-analysis, nursing intervention, primipara
1. Introduction
Delivery refers to the process in which the fetus and its appendages are delivered out of the maternal birth canal after 28 weeks of gestation. In the process of childbirth, due to severe labor pain, the puerperae usually experience anxiety and fear and thus lead to exerting forth inappropriately, further aggravating maternal pain, prolonging the duration of labor, increasing the amount of blood loss, which threatens the health of mothers and babies. Currently, Chinese total cesarean section rate ranks first in the world, more than three times above the world warning line.[1,2] Moreover, with the liberalization of the two-child policy in China, the second pregnancy would expose the cesarean women to various complications and high risks.[3] Therefore, the problem on how to improve natural delivery rate and reduce cesarean section rate demands prompt resolutions.
Pioneered by Dr Fernand Lamaze, Lamaze breathing has been widely used in many countries as a breathing training method.[4] The Lamaze breathing is based on the focused breathing, mainly involving muscle relaxation, structured breathing and focus shifting. Muscle relaxation is guarded by a specific relaxation procedure which assists woman to relax voluntary muscles to the greatest extent possible. Muscle relaxation and structured breathing help the woman in labor distract themselves from their negative emotions to the breathing movements, which is conductive for the mothers to stay calm during labor and increase their confidence of the ability to give birth. Generally speaking, Lamaze breathing has been found to effectively help expectant mothers understand how to cope with pain in ways that both facilitate delivery and promote comfort.[5] Nursing intervention is usually provided by nursing staff during labor; the contents of the intervention vary and mainly include postural nursing, delivery ball, doula nursing, massage, and psychological nursing. A number of clinical studies have investigated the effect of Lamaze breathing training combined with nursing intervention on maternal pain relief and outcomes improvement. Conversely, there is some controversy regarding its effectiveness due to the varying methodological qualities of present researches, especially lacking high-quality evidence-based studies. For example, Zhao et al ever questioned the effect of the non-pharmacological analgesia on labor analgesia.[6] Hotelling[7] reported that the content and teaching techniques in Lamaze childbirth education may have a negative impact on maternal confidence of their capacity to deliver. And the results of study implemented by Lonnberg et al[8] showed that the efficiency of mindful delivery method was superior to the Lamaze breathing training method. Therefore, through meta-analysis, this paper systematically evaluated the effect of Lamaze breathing training method combined with nursing intervention on the childbirth of primiparas, so as to provide high-quality evidence-based evidence for parturient pain relief and pregnant outcomes improvement.
2. Methods
2.1. Criteria for eligibility
2.1.1. Types of researches
The randomized controlled trials investigating the combined effects of Lamaze breathing training and nursing intervention on the delivery in primipara were included.
2.1.2. Types of participants
Participants were selected if the following criteria were met:
-
1.
Primipara with singleton childbirth;
-
2.
Prenatal examination: fetus without coiling of umbilical cord, malpresentation, overlarge head circumference, and other abnormalities.
The exclusion criteria were as follows:
-
1.
Premature or overdue pregnancy;
-
2.
Narrow pelvis;
-
3.
Maternal complications such as gestational diabetes, eclampsia.
2.1.3. Interventions
The participants in the experimental group were treated with Lamaze breathing training combined with nursing intervention including postural nursing, delivery ball, doula nursing, massage, and psychological nursing while the comparators in control group were treated with routine nursing such as health education and nursing operation.
2.1.4. Types of outcomes
Natural delivery rate, labor endurance, pain level, and the amount of postpartum hemorrhage were the outcomes in the studies. Each of the included studies in this meta-analysis had to have assessed at least one of the above outcomes.
2.2. Exclusion criteria
The studies would be excluded if any of the following criteria were not met:
-
1.
The full-text papers were not available;
-
2.
Detailed data could not be extracted from the articles for the meta-analysis.
2.3. Search strategy
Computer retrieval of randomized controlled trials published from January 2000 to November 2019 in PubMed, Cochrance Library, Medline, Web of Science, Embase, Chinese Academic Journals, Chinese Biomedical Literature Database, VIP Database, Wanfang Database were searched. The following combination of keywords and free terms was used for foreign language databases which was limited in English. The search strategy included the use of Title/Abstract related to Lamaze breath training (“Lamaze pain relieving delivery method” or “breath training” or “respiratory training”), to the nursing intervention (“nursing” or “nursing measures”), to the unipara (“primipara” or “the first time delivery” or “parturitions” or “birth” or “childbirth”), and to randomized controlled trial (“clinical test” or “clinic trial” or “clinical controlled trial”), and the same retrieval strategy was used in Chinese database.
2.4. Studies selections and data extraction
All the retrieved studies were imported into the ENDNOTE X9 software. Two researchers screened the literatures by reviewing titles and abstracts primarily and next the selected articles were read in full. The differences and discrepancies were resolved by discussion and, when necessary, by consulting a third reviewer. The following data were extracted from the included articles: title, the first author, year of publication, number of participants, and outcomes. In addition, the evaluation indexes of literature quality were also collected, including random, allocation concealment, blinding, integrity of outcome data, and selective reporting data.
2.5. Statistical analysis
All statistical analyses were performed using Comprehensive Meta Analysis V2 software. The percentage of variability attributable to the heterogeneity of the studies was estimated by I2 statistics, with a P-value of <.10, I2 ≥ 50% considered statistically significant. If there was no heterogeneity between studies, the fixed effect model was used for analyzing. Otherwise, sensitivity analysis was performed to identify the heterogeneity. And random effect model was performed for the studies with heterogeneity not being eliminated. The data of the numerical variables were expressed by weighted mean difference and confidence interval (CI) of 95% while the data of binomial variables were expressed by rate ratio (RR) and confidence interval (CI) of 95%. Besides, the safety loss factor was used to evaluate whether there was publication bias in the meta-analysis.
2.6. Ethical approval
Ethical approval was not necessary. Because we did not make any clinical research in this manuscript, we just collected the data from available publications.
3. Results
3.1. Study selection
A total of 816 eligible studies were identified, with 64 English literature and 752 Chinese literature articles. ENDNOTE X9 software removed 149 articles because of duplicates. From the remaining 603 studies, 547 were excluded after the initial reading stage. The other 56 were read in full, and 22 studies conducted on 7155 primiparas were eventually included in our meta-analysis (Fig. 1).
Figure 1.
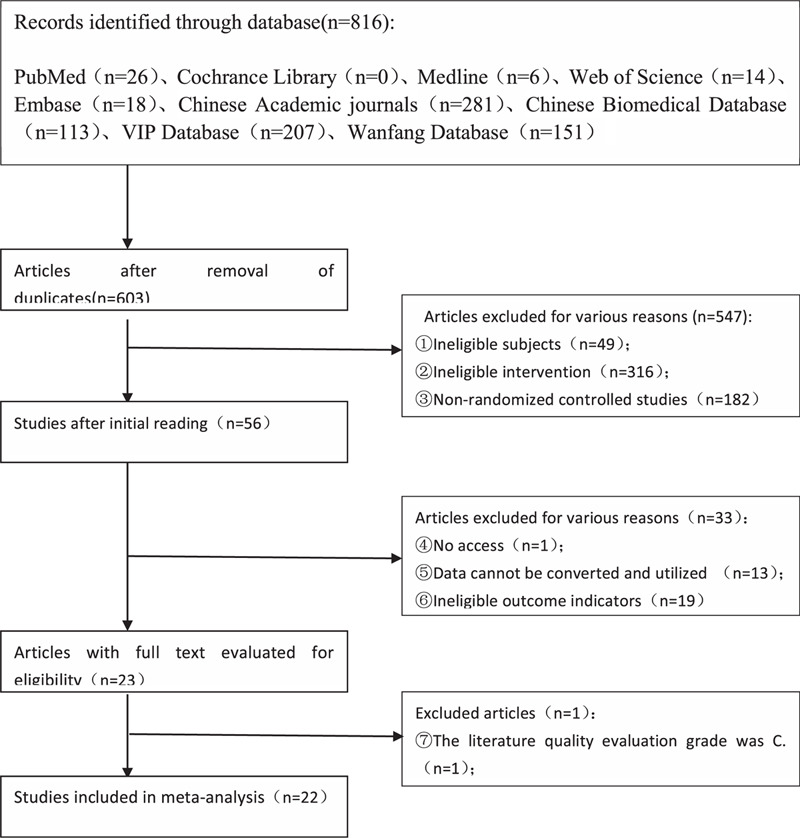
flow diagram showing the selection of studies for the meta-analysis.
3.2. The characteristic and quality assessment of included researches
There were 22 randomized controlled trials conducted on 7155 primiparas, being eligible for the meta-analysis. The specific characteristics were shown in Table 1. As summarized in Table 2, the quality levels of the 22 RCTs were all appraised as grade B according to Cochrane 5.1.0 system evaluation standard. The differences of age and gestational weeks between experimental and control groups had no significance.
Table 1.
Characteristics of the included randomized controlled trials for the meta-analysis.
| Intervention | Sample size | Outcomes | ||||
| Study | Year of publication | Treatment group | Control group | T | C | |
| Bai J et al[9] | 2017 | Lamaze breath training + nursing care of delivery ball | Usual nursing care | 26 | 26 | ①③ |
| Ban CM et al[10] | 2019 | Lamaze breath training + nursing care of delivery ball | Usual nursing care | 160 | 148 | ①②④ |
| Cao HX et al[11] | 2014 | Lamaze breath training + body posture care | Usual nursing care | 100 | 100 | ①②④ |
| Deng JF et al[12] | 2015 | Lamaze breath training + nursing care of delivery ball | Usual nursing care | 36 | 30 | ② |
| Feng XX et al[13] | 2017 | Lamaze breath training + nursing care of delivery ball | Usual nursing care | 36 | 36 | ②③ |
| Feng ZJ et al[14] | 2014 | Lamaze breath training + nursing care of delivery ball | Usual nursing care | 80 | 80 | ①②③ |
| Guo JY et al[15] | 2013 | Lamaze breath training + nursing care of delivery ball | Usual nursing care | 132 | 140 | ①②③ |
| Guo L et al[16] | 2017 | Lamaze breath training + Doula nursing | Usual nursing care | 60 | 60 | ①② |
| He QN et al[17] | 2016 | Lamaze breath training + neuromuscular relaxation exercise, traditional Chinese medicine hot compress, perineum elastic nursing | Usual nursing care | 463 | 463 | ①②③④ |
| Huang JL et al[18] | 2017 | Lamaze breath training + Doula nursing | Usual nursing care | 60 | 60 | ①② |
| Huang QM et al[19] | 2018 | Lamaze breath training + nursing care of delivery ball | Usual nursing care | 56 | 55 | ①③ |
| Jiang LZ et al[20] | 2019 | Lamaze breath training + nursing care of delivery ball | Usual nursing care | 47 | 47 | ②③ |
| Jiang L et al[21] | 2019 | Lamaze breath training + knowledge, attitude and practice health education | Usual nursing care | 120 | 120 | ①② |
| Jiang X et al[22] | 2017 | Lamaze breath training + nursing care of delivery ball | Usual nursing care | 1350 | 1650 | ②③ |
| Kong QJ et al[23] | 2016 | Lamaze breath training + nursing care of delivery ball | Usual nursing care | 42 | 42 | ①②④ |
| Li MR et al[24] | 2016 | Lamaze breath training + nursing care of delivery ball | Usual nursing care | 60 | 60 | ② |
| Ling TT et al[25] | 2019 | Lamaze breath training + nursing care of delivery ball | Usual nursing care | 48 | 48 | ①② |
| Qu XQ et al[26] | 2018 | Lamaze breath training + nursing care of delivery ball | Usual nursing care | 46 | 46 | ①② |
| Zhang H et al[30] | 2014 | Lamaze breath training + nursing care of delivery ball, accompany the whole process, systematic health education | Usual nursing care | 180 | 180 | ①②③④ |
| Zhang P et al[27] | 2018 | Lamaze breath training + Doula nursing | Usual nursing care | 75 | 75 | ①② |
| Zhao Y et al[28] | 2017 | Lamaze breath training + Doula nursing, nursing care of delivery ball, | Usual nursing care | 111 | 111 | ①③ |
| Zhen LX et al[29] | 2014 | Lamaze breath training + nursing massage | Usual nursing care | 85 | 85 | ①②③ |
① the rate of natural delivery; ② delivery endurance; ③ pain level; ④ the amount of postpartum bleeding.
Table 2.
Quality assessment of all included studies.
| Study | Random sequence generation | Allocation concealment | Blinding | Incomplete outcome data | Selective outcome reporting | Other bias |
| Bai J et al[9] | Yes but method was unclear | Unclear | No | No | No | Unclear |
| Ban CM et al[10] | Sortition randomisation | Unclear | No | No | No | Unclear |
| Cao HX et al[11] | Both unclear | Unclear | No | No | No | Unclear |
| Deng JF et al[12] | Yes but method was unclear | Unclear | No | No | No | Unclear |
| Feng XX et al[13] | Yes but method was unclear | Unclear | No | No | No | Unclear |
| Feng ZJ et al[14] | Random and with number table | Unclear | no | no | no | Unclear |
| Guo JY et al[15] | Both unclear | Unclear | No | No | No | Unclear |
| Guo L et al[16] | Yes but method was unclear | Unclear | No | No | No | Unclear |
| He QN et al[17] | Yes but method was unclear | Unclear | No | No | No | Unclear |
| Huang JL et al[18] | Both unclear | Unclear | No | No | No | Unclear |
| Huang QM et al[19] | Yes but method was unclear | Unclear | No | No | No | Unclear |
| Jiang LZ et al[20] | Yes but method was unclear | Unclear | No | No | No | Unclear |
| Jiang L et al[21] | Yes but method was unclear | Unclear | No | No | No | Unclear |
| Jiang X et al[22] | Both unclear | Unclear | No | No | No | Unclear |
| Kong QJ et al[23] | Yes but method was unclear | Unclear | No | No | No | Unclear |
| Li MR et al[24] | Yes but method was unclear | Unclear | No | No | No | Unclear |
| Ling TT et al[25] | Both unclear | Unclear | No | No | No | Unclear |
| Qu XQ et al[26] | Both unclear | Unclear | No | No | No | Unclear |
| Zhang P et al[27] | Random and with number table | Yes | No | No | No | Yes |
| Zhao Y et al[28] | Random and with number table | Unclear | No | No | No | Unclear |
| Zhen LX et al[29] | Yes but method was unclear | Unclear | No | No | No | Unclear |
| Zhang H et al[30] | Both unclear | Unclear | No | No | No | Unclear |
3.3. Effects on the rate of natural delivery
There were 17 researches investigating the natural deliver rate (cesarean section rate was converted into the natural delivery rate) (Fig. 2).[9–11,13,14–19,21,23,25–29] Since no heterogeneity was shown among the studies (I2 = 0%, P = .85), fixed effect model was chosen for analysis. Ultimately, the findings revealed that compared to the routine nursing group, the natural delivery rate of primipara who were treated with Lamaze breathing training combined with nursing was significantly improved (RR = 2.97, 95% CI [2.48,3.56], P < .001). There was no publication bias (fail-safe number 592 > 5K+10).
Figure 2.
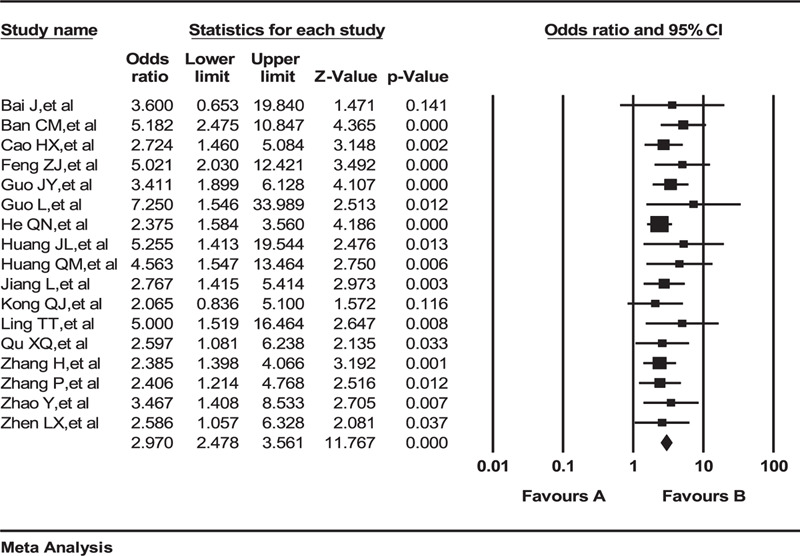
Effects on the rate of natural delivery. A = cesarean section, B = natural delivery.
3.4. Effects on delivery endurance
Nineteen studies consisted of 6650 participants reported the effects on delivery endurance (Fig. 3). Random effect model was applied for analysis because the high heterogeneity (I2 = 98.16%, P < .001) was not altered visibly by sensitivity analysis. And the result pointed out that Lamaze breathing training combined with nursing shortened the length of labor in contrast to control group (−2.604, 95%CI [−3.120, −2.087], P < .001). There was no publication bias (fail-safe number 6055 > 5K+10).[10–18,20–27,29,30]
Figure 3.
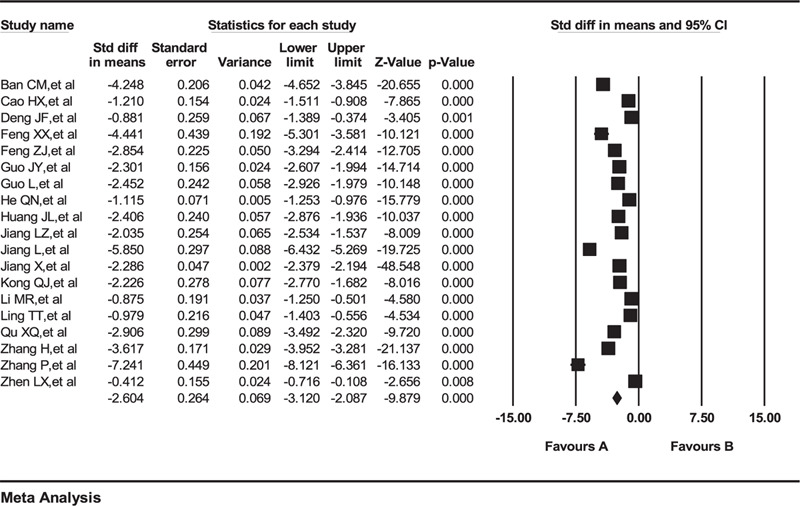
Effects on delivery endurance. A = shorten time, B = extend time.
3.5. Effects on pain level
Eleven studies including 5439 parturients investigated the pain level with WHO pain grading criteria as standard (Fig. 4).[9,13–15,17,19,20,22,28–30] There was high heterogeneity (I2 = 91.073%, P < .001) in the pain integrity factor. Therefore, the random effect model was chosen. The results showed that more participants in routine nursing group were rated as the moderate and severe pain levels than in the group with combined intervention, which illustrated that the experimental intervention had a positive effect on alleviating the pain integrity of childbirth (RR = 0.194, 95% CI [0.115, 0.325], P < .001). There was no publication bias (fail-safe number 1,285 > 5K+10).
Figure 4.
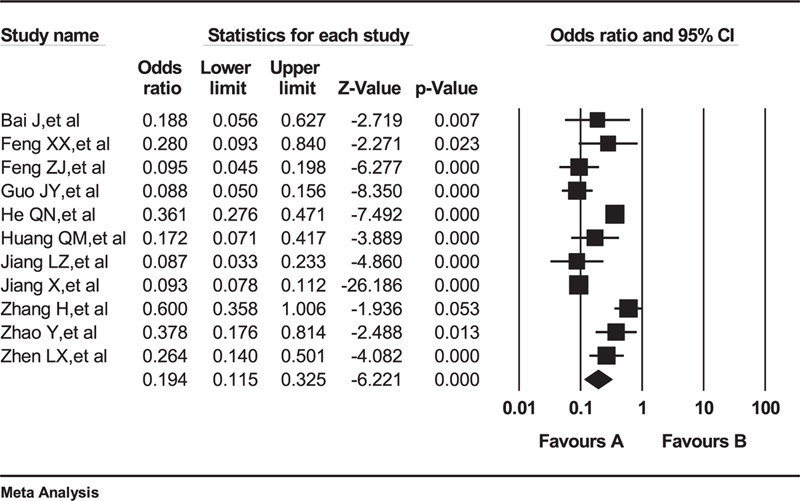
the effect on pain integrity. A = low pain level, B = high pain level.
3.6. Effects on the amount of postpartum hemorrhage
Five articles involving 1876 study participants demonstrated the amount of postpartum bleeding (Fig. 5). And the random effect model was used on account of the unchangeable high heterogeneity (I2 = 98.36%, P < .001).[10,11,13,17,23] The findings from the meta-analysis, without publication bias (fail-safe number 1421 > 5K+10), manifested that compared to routine nursing, the combination of Lamaze breathing training and nursing led to lower postpartum bleeding (−2.966, 95% CI [−4.056, −1.877], P < .001).
Figure 5.
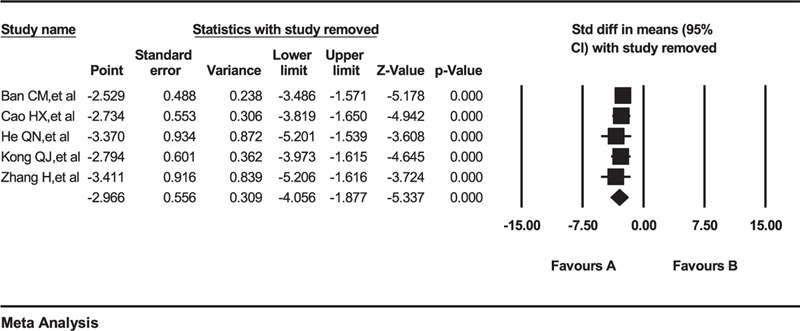
Effects on postpartum hemorrhage. A = reduce the amount of bleeding, B = increase the amount of bleeding.
4. Discussions
4.1. Assessment of methodological quality
Abiding strictly by the inclusion and exclusion standards, 22 randomized controlled trials with sample size of 7155 were included in the meta-analysis. And quality level of the 22 trials was all graded as B. Moreover, the data extracted from the studies were all lossless and comparable (P > .05). In consequence, the findings from the meta-analysis were reliable.
4.2. Improvement of the natural delivery rate
Lamaze breathing training is internationally recognized as an effective method for pain relieving in childbirth. Several studies reported that due to lacking labor experience, primiparas were prone to overstrain and thus led to shortness of breath, which would cause intrauterine hypoxia, uterine inertia and slowing down the dilation pace of the cervix, more seriously, the stagnancy may account for fetal anoxia.[31,32] The regular and specialized breathing techniques training starting from the seventh month of pregnancy guides lying-in women to relax muscle, breathe normatively, and distract themselves to the respiratory movement, which further reduce overstress and strengthen confidence during delivery.[33] Besides, the relaxed muscles enable sufficient oxygen entering uterus and ensure the childbirth goes smoothly.[34] What's more, some researches prove that those expectant mothers trained with Lamaze breathing techniques could act more confidently and less stressfully during delivery and they preferred spontaneous labor, which may contribute to the reduction of the high cesarean section rate in China.[35] Furthermore, the nursing intervention, like postural nursing, delivery ball, doula nursing, massage and psychological nursing, was also beneficial for the parturient to conquer fear and tension and contract coordinately, which facilitated the process of natural childbirth.[36,37] Generally, Lamaze breathing training combined with nursing intervention could increase the natural delivery rate via physiological breathing training and relaxation.
4.3. Reduction of pain level, delivery endurance, and postpartum bleeding
The pain of delivery principally originates from the parturient's endocrine hormones change and sympathetic excitation caused by the following three factors: uterine contraction, the fetus squeezing the birth canal, and psychological stress.[38] As mentioned above, the breathing techniques training combined with nursing could assist parturient to relax both physically and psychologically. Thus, when labor pains come, the training led parturient to relieve muscular tension and relax muscle initially, which decreased levels of 5-hydroxytryptamine, and finally alleviated the pain.[39,40] Besides, the effective breathing motions also guaranteed the sufficient intrauterine fetal oxygen supply and avoided uterine inertia, which accelerated the process of labor.[41] In addition, the psychological relief provided by nursing measures could ulteriorly reduce heart rate, blood pressure and breathing rate, which brought down the release of norepinephrine and shorten the delivery stages. Uterine inertia and soft birth canal injury are the two major causes of postpartum bleeding. The muscle relaxation and sufficient intrauterine fetal oxygen supply benefiting from the Lamaze breathing enabled the participants to avoid inappropriately contraction, intrauterine hypoxia and overlong delivery endurance, which reduced the risks of soft birth canal injury and uterine inertia.[42] And some nursing measures like uterine massage and postpartum education were also helpful for the involution of uterus and thus reduce postpartum bleeding.[38]
4.4. Limitations
Limitations of this meta-analysis were as follows:
-
1.
There existed language bias because this meta-analysis reviewed studies merely published in the Chinese language which can find Lamaze breathing training combining with nursing intervention;
-
2.
Due to different sample sizes, there existed differences in experimental design and breathing training length and frequency. Furthermore, the evaluation index of pain level was subjective and it lead to heterogeneity among findings;
-
3.
The quality of the 22 included literatures were all grade B because it was infeasible to apply blind method under the condition that the content and objective of experimental intervention had to be informed;
-
4.
Several studies verified that the Lamaze breath training combined with nursing intervention was able to ease the psychological tension and anxiety of unipara. But since those trials design did not meet the inclusion criteria and the data was unable to be converted, the psychological evaluation indexes, such as tension and anxiety level, failed to be incorporated into the outcomes.
5. Conclusions
In conclusion, we found that the Lamaze breathing training combined with nursing intervention indeed showed positive influence on the process and outcomes of delivery by increasing the natural delivery rate, shortening labor endurance, relieving pain, and reducing postpartum hemorrhage. Challenged by the high cesarean section rate, it is worth to popularize Lamaze breathing training during pregnancy and offer nursing during delivery. Besides, it also requires specialized staff to implement the prenatal education and antepartum nursing. To propel the practice of this, we were sincerely looking forward to more authentic relevant randomized controlled trials to be publicated.
Author contributions
Conceptualization: Chao Wu, Zhaohua Ji.
Data curation: Chao Wu, Yiling Ge.
Formal analysis: Shizhe He.
Investigation: Yiling Ge.
Methodology: Hongjuan Lang.
Resources: Chao Wu, Yanling Du.
Software: Zhaohua Ji.
Supervision: Chao Wu.
Visualization: Yanling Du.
Writing – original draft: Chao Wu, Zhaohua Ji.
Writing – review & editing: Xinyan Zhang, Zhaohua Ji, Hongjuan Lang.
Glossary
Abbreviations: CI = confidence interval, RR = relative risk.
References
- [1].Lumbiganon P, Laopaiboon M, Gulmezoglu AM, et al. Method of delivery and pregnancy outcomes in Asia: the WHO global survey on maternal and perinatal health 2007-08. Lancet 2010;375:490–9. [DOI] [PubMed] [Google Scholar]
- [2].Wang E, Hesketh T. Large reductions in cesarean delivery rates in China: a qualitative study on delivery decision-making in the era of the two-child policy. BMC Pregnancy Childbirth 2017;17:405–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Gu C, Zhu X, Ding Y, et al. A qualitative study of nulliparous women's decision making on mode of delivery under China's two-child policy. Midwifery 2018;62:6–13. [DOI] [PubMed] [Google Scholar]
- [4].Podgurski MJ. Theorists and techniques: connecting education theories to Lamaze teaching techniques. J Perinat Educ 2016;25:9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Amis D. A childbirth educator's commentary on hormonal physiology of childbearing: evidence and implications for women, babies, and maternity care. J Perinat Educ 2015;24:154–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Zhao Z, Jiang W. Research progress of non drug labor analgesia. Contemp Nurses (next ten issues) 2012;3:15–7. [Google Scholar]
- [7].Hotelling BA. The nocebo effect in childbirth classes. J Perinat Educ 2013;22:120–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Lonnberg G, Jonas W, Unternaehrer E, et al. Effects of a mindfulness based childbirth and parenting program on pregnant women's perceived stress and risk of perinatal depression-results from a randomized controlled trial. J Affect Disord 2019;262:133–42. [DOI] [PubMed] [Google Scholar]
- [9].Bai J, Wang H, Cai S. Effect of Lamaze pain reducing delivery method combined with delivery ball nursing on delivery outcome. Health Care Today 2017;23:271–8. [Google Scholar]
- [10].Ban C. Evaluation of the effect of labor ball training combined with Lamaze's respiratory pain reduction method in midwifery. J Practical Gynecol Endocrinol 2019;6:46–7. [Google Scholar]
- [11].Cao H. Effect of Lamaze delivery method combined with body position nursing on delivery. Nursing Pract Res 2014;21:50–1. [Google Scholar]
- [12].Deng J. Application of Lamaze breathing method combined with delivery ball in primipara delivery. J Nurs 2015;2:50–2. [Google Scholar]
- [13].Feng X, Duan P. Effect analysis of delivery ball nursing combined with Lamaze breathing method in primipara delivery. Chin Baby 2017;12:196–9. [Google Scholar]
- [14].Feng Z. Effect of labor ball combined with Lamaze respiration on labor pain, delivery control and pregnancy outcome of primipara. Chin Clin Nursing 2014;6:461–3. [Google Scholar]
- [15].Guo J, Yi C. Observation on the effect of Lamaze pain reducing delivery combined with delivery ball in primipara. Nursing Pract Res 2013;10:48–9. [Google Scholar]
- [16].Guo L. Clinical study of Lamaze respiration combined with music guide instrument in labor analgesia. Chin Med Sci 2017;7:90–2. [Google Scholar]
- [17].He Q, Yan C, Zhong Y, et al. Intensive nursing and midwifery experience of labor analgesia in the first and second stages of labor for primipara. Med Innov China 2016;13:86–90. [Google Scholar]
- [18].Huang J, Sheng S, Guo L. Clinical study of Lamaze respiration combined with music guide instrument in labor analgesia. Chin Practical Med 2017;12:181–3. [Google Scholar]
- [19].Huang Q, Qin A, Li Y, et al. Analysis of the effect of Lamaze's respiratory pain reducing delivery method combined with delivery ball intervention on the pain and delivery outcome of primipara. Clin J Tradit Chin Med 2018;30:1742–4. [Google Scholar]
- [20].Jiang L. To explore the effect of Lamaze pain reducing delivery combined with peanut ball nursing. J Pract Gynecol Endocrinol 2019;6:160–72. [Google Scholar]
- [21].Jiang L, Cai Q, Chen X. The application of knowledge, faith and practice health education combined with Lamaze's pain reducing delivery method in primipara. Nursing Pract Res 2019;16:83–5. [Google Scholar]
- [22].Jiang X. Clinical effect of combined application of labor ball nursing and Lamaze respiration in reducing pain delivery of primipara. Psychol Doctor 2017;23:329–30. [Google Scholar]
- [23].Kong Q. Effect of labor ball combined with Lamaze respiration on labor pain, delivery control and pregnancy outcome of primipara. J Clin Nurs 2016;15:2–4. [Google Scholar]
- [24].Li M, Xiang Y, Tang S. Application of Lamaze breathing method combined with delivery ball in primipara delivery. Nurs Pract Res 2016;13:64–5. [Google Scholar]
- [25].Lin T. Effect of labor ball nursing combined with Lamaze's breathing method to reduce pain and delivery on cesarean section rate and delivery time of primipara. Mod Med Imagel 2019;28:1182–3. [Google Scholar]
- [26].Qu X. Effect of labor ball nursing combined with Lamaze's breathing method to reduce pain and labor on cesarean section rate and labor process of primipara. Henan Med Res 2018;27:2648–9. [Google Scholar]
- [27].Zhang P. The effect of Doula delivery combined with Lamaze respiration on birth control and labor process of primipara. Chin Gen Pract Nurs 2018;16:4264–6. [Google Scholar]
- [28].Zhao Y, Tan J, Zhu L. Effect of whole course nursing intervention in natural delivery of primipara. Chin Gen Pract Nurs 2017;15:931–3. [Google Scholar]
- [29].Zhen L. Study on the effect of Lamaze pain reducing delivery method combined with head massage on the delivery mode of primipara. Int J Med Health 2014;20:234–40. [Google Scholar]
- [30].Zhang H, Feng X, Zhang L, et al. Application of systematic nursing intervention in natural delivery of primipara. Chin J Mod Nurs 2014;20:3588–90. [Google Scholar]
- [31].Enzelsberger H, Langer M, Reinold E, et al. Personality-dependent anxiety reactions in primiparous patients. Z Geburtshilfe Perinatol 1990;194:29–35. [PubMed] [Google Scholar]
- [32].Laursen M, Johansen C, Hedegaard M. Fear of childbirth and risk for birth complications in nulliparous women in the Danish National Birth Cohort. BJOG 2009;116:1350–5. [DOI] [PubMed] [Google Scholar]
- [33].Lothian JA, Hotelling BA. Continuing education module top 10: tips on teaching Lamaze classes. J Perinat Educ 2012;21:248–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Bernard MR, Eymard C. Trends and current issues in childbirth and parenting education. Sante Publique 2012;24:283–9. [PubMed] [Google Scholar]
- [35].McGrath K. Continuing education module the courage to birth. J Perinat Educ 2012;21:72–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].DiFranco JT, Curl M. Healthy birth practice #5: avoid giving birth on your back and follow your body's urge to push. J Perinat Educ 2014;23:207–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Difranco JT, Romano AM, Keen R. Care practice #5: spontaneous pushing in upright or gravity-neutral positions. J Perinat Educ 2007;16:35–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Budin WC. Making a difference with evidence. J Perinat Educ 2010;19:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Bause GS. Before the Lamaze method: Bonwill “Rapid Breathing”. Anesthesiology 2016;124:258. [DOI] [PubMed] [Google Scholar]
- [40].Florido J, Oltras CM, Fajardo MC, et al. Plasma concentrations of beta-endorphin and adrenocorticotropic hormone in women with and without childbirth preparation. Eur J Obstet Gynecol 1997;73:121–5. [DOI] [PubMed] [Google Scholar]
- [41].Shih HC, Lee TY, Chen WH, et al. The effectiveness of the video-based Lamaze method on prenatal mothers’ knowledge, attitudes, and practice. J Nurs 2005;52:27–38. [PubMed] [Google Scholar]
- [42].Zwelling E. Down memory lane: recollections of Lamaze international's first 50 years. J Perinat Educ 2010;19:11–6. [DOI] [PMC free article] [PubMed] [Google Scholar]


