INTRODUCTION:
As the number of cancer survivors grows, new models of survivorship care are being implemented, but there is limited evaluation to date. This retrospective review assesses the concordance of care provided to adult-onset cancer survivors by advanced practice providers (nurse practitioners and physician assistants) with Institute of Medicine guidelines for survivorship care.
METHODS:
Records from three survivorship clinics at a single institution were reviewed for frequency of recurrence surveillance, screening for second cancers, symptom management (physical, psychological), health promotion education (alcohol, tobacco, cholesterol, and bone density screenings; diet/exercise discussion), care coordination, and provision of care plan. Data were characterized using descriptive statistics.
RESULTS:
Over 2 years, 9,052 unique survivorship visits occurred; 210 breast, 208 prostate, and 204 colorectal visits were randomly selected for review. All patients with breast cancer underwent surveillance for recurrence; 99% were screened for new cancers. Discussion of health promotion activities ranged from 83% to 100%; 91% of patients were reviewed for physical symptoms, and 93% were reviewed for psychological symptoms. All patients with prostate cancer underwent recurrence surveillance; 97% were screened for new primaries. Health promotion activities ranged from 70% to 97%, and symptoms were discussed in 89% of visits. All patients with colorectal cancer underwent a surveillance colonoscopy for recurrence; 97% had a carcinoembryonic antigen test. Among women, 97% had mammograms, and 96% had a Papanicolaou test; 83% of men had a prostate-specific antigen test. Health promotion activities ranged from 69% to 100%, and symptoms were discussed in 93% to 97% of visits.
CONCLUSIONS:
Findings suggest that advanced practice providers can provide survivorship care in accordance with Institute of Medicine standards, which provide a normative standard. This assessment is an important step in evaluating survivorship outcomes.
INTRODUCTION
It has been more than a decade since the publication of the seminal Institute of Medicine (IOM) report, From Cancer Patient to Cancer Survivor: Lost in Transition.1 During this time, the number of cancer survivors has increased, both in the United States and internationally, with an estimated 33 million survivors globally.2 Currently in the United States, there are more than 15.5 million cancer survivors, representing nearly 5% of the population.3 By 2026, the number of survivors will reach more than 20.3 million in the United States, and by 2040, it is estimated that 73% of survivors will be older than 65 years of age.4 In the United States and many European countries, 5-year survival rates have increased to 50% or greater for individuals diagnosed with adult-onset cancers and 83% for childhood cancers; in the United States, 5-year survival for all cancers combined was 67% in 2013.5
Concomitant with these positive results in survival rates, researchers have identified substantial risks for morbidity, reduced quality of life, and premature mortality for some survivors as a result of their cancer and/or cancer treatment.1 These late and long-term effects cross the physical (eg, cardiopulmonary, infertility, second malignancies),6-8 psychological (eg, fear of recurrence, anxiety, depression),9,10 and practical (eg, employment difficulties, insurance and financial issues)11,12 domains. As such, increasing attention is being paid to the post-treatment period of care and the subsequent challenges of developing new models of survivorship care to address these needs and implementing methods of evaluation to track health outcomes.1
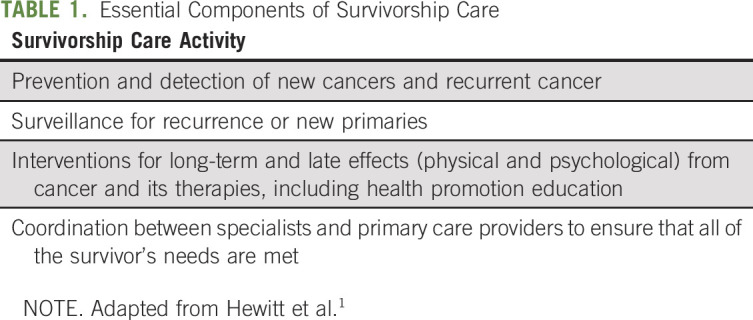
In recent years, national professional organizations have published position papers (American Society of Clinical Oncology [ASCO], IOM), clinical care guidelines (National Comprehensive Cancer Network [NCCN], ASCO, and American Cancer Society), and professional standards (American College of Surgeons) focused on cancer survivorship. Also, there is a growing body of literature establishing the key components of survivorship care, including the need for ongoing medical services, psychosocial support, and monitoring for late effects and cancer recurrence. Although some research has found an underuse of surveillance tests in cancer survivors,13 other studies have suggested there is variation between recommended age-appropriate screening for second primary cancers and observed cancer screening in cancer survivors.14-17 In addition to research addressing service utilization, a number of survivorship care delivery models have been proposed in the literature, including care led by varying providers: oncologists and other physician specialists, community-based primary care providers (PCPs), advanced practice providers (APPs; nurse practitioners [NPs] and physician assistants), or care shared within a multidisciplinary team.18-23 Although these reports outline the structure of the associated models, evaluation efforts, be they focused on the feasibility of implementation or the effectiveness of a particular model, have been limited.24 To address this growing need for evaluation, this article describes one aspect of effectiveness evaluation: the concordance of care provided in APP-led survivorship clinics (in this case, NPs) with IOM guidelines for comprehensive survivorship care, among a sample of adult survivors at a single institution, Memorial Sloan Kettering Cancer Center (MSK; Table 1).
TABLE 1.
Essential Components of Survivorship Care
MSK EXPERIENCE
In 2003, MSK established its Survivorship Initiative, an institution-wide approach to addressing post-treatment clinical care, research, and education. Recognizing that many factors determine what care model works best within an academic medical center, hospital, or private practice, a multidisciplinary planning committee considered MSK’s existing clinical care model, institutional culture, survivor population, and available resources.23,25 Needs assessments and focus groups with patients, providers, and administrators determined survivors’ unmet needs, gaps in care, and anticipated resources; this feedback shaped the approach to developing the survivorship care model. Other considerations in program development were projected increases in the number of patients with cancer, historically limited communication with PCPs, and an increased focus on efficient care delivery models.
All clinical components of care, including patient eligibility for referral to survivorship, timing for referral, and follow-up care guidelines (on the basis of evolving guidelines developed by the NCCN, ASCO, and the American Cancer Society),26-28 were established in partnership with disease- or modality-based physician specialists. Organizational details, such as clinic metrics, approval of incremental positions, staff support, and physical space for examination rooms, were established through collaboration with hospital administration. Survivorship program staff provided institution-wide education at staff meetings, in-services, and grand rounds to raise awareness and gain support for the initiative.
In 2006, three pilot clinics (lung, prostate, and lymphoma), led by three survivorship NPs, were opened, focusing on disease groups with physician champions in leadership positions. Since 2006, the program has expanded to include 17 disease site clinics and 23 survivorship NPs. Patients were eligible for transition from the oncologist to a survivorship NP if they were at low risk for recurrence and significant late or long-term effects, as determined by NCCN guidelines, published data, and clinical consensus. The NP provided focused, comprehensive care to patients and communicated with local PCPs through the provision of a follow-up note, treatment summary, and survivorship care plan (SCP). To allow the NPs to build their practices while working side by side their physician and nursing colleagues, the NPs were embedded in the treatment team, rather than having a standalone survivorship clinic. This approach provided continuity for patients as they transitioned from active treatment to long-term follow-up care. Neither group—survivors nor clinicians—had to relinquish access to the other, which is often cited as a barrier to the success of survivorship care models.29
To determine oncology provider acceptance of the survivorship APP model, physician referrals were tracked and ranged from 80% to 100% of physicians referring at least some of their eligible patients to the NP clinics. To determine patient satisfaction with the NP clinics, a surrogate end point was used: the number of individuals who had one NP visit, but returned to care by the oncologist in the absence of a recurrence; 95% to 98% of patients who were referred by their oncologist remained in the NP clinics.
METHODS
Patients
This study was approved as retrospective research by the MSK Institutional Review Board/Privacy Board. The cohort for evaluation consisted of cancer survivors who were being followed in one of three APP-led survivorship clinics at MSK—breast, prostate, or colorectal—the three disease types with the largest number of survivors nationally (50% of all cancer survivors in the United States). Eligible survivors were those with early-stage breast cancer, colon cancer, rectal cancer, or prostate cancer; under active routine follow-up; without recurrence or new primary cancer; and with at least two visits to the survivorship clinic from January 2011 to December 2013. Male patients with breast cancer were excluded, as were patients with prostate cancer who received radiation and patients with colorectal cancer who received chemotherapy, to ensure that patients with metastatic disease were not inadvertently included in the analysis. A random sample of 622 survivors was drawn from the eligible survivor population (N = 5,815): records were reviewed for 210 patients (of 4,298) with breast cancer, 208 patients (of 963) with prostate cancer, and 204 patients (of 498) with colorectal cancer.
Data Collection Procedures
All sampled patients were identified through a hospital-based registry. Medical records of the selected patients were reviewed to determine frequency of surveillance for recurrence, screening for second cancers, provision of symptom management (physical and psychological), health promotion education, care coordination, and provision of an SCP.
Study Outcomes
Outcomes were selected to measure the elements of comprehensive survivorship care and were assessed by reviewing each medical record for documentation of the following:
Adherence to the clinical guideline on follow-up care: the frequency and types of surveillance for recurrence screenings were recorded; frequency of and reason for additional testing were also assessed.
Screening for new primary cancers: discussion of age- and sex-appropriate screening for second primary cancers.
Symptom management: discussion of physical (eg, lymphedema, fatigue, sexual dysfunction, incontinence), and/or psychological symptoms (eg, depression, anxiety).
Health promotion education: counseling regarding physical activity, diet, alcohol abstinence, tobacco cessation, cholesterol screening, and bone density testing.
Care coordination: involvement of the PCP in survivorship care.
Delivery of SCP: receipt of a care plan at any time during follow-up.
Recommended surveillance tests (ie, magnetic resonance imaging of the breast, breast ultrasound, mammogram, prostate-specific antigen [PSA] blood test, carcinoembryonic antigen blood test, colonoscopy) were based on clinical practice guidelines. Screening tests for second cancers (Papanicolaou test, mammogram, PSA test, and colonoscopy) were based on guidelines from the US Preventive Services Task Force.30 The provision of symptom management (physical and psychological), health promotion education (alcohol, tobacco, cholesterol, bone density screenings, and discussions on diet and exercise), and care coordination and provision of SCP were evaluated based on the recommendations of the IOM. Of note, the correspondence with the PCP via SCP made clear which testing responsibilities were undertaken by the NP, and test results for recurrence and screenings were provided to the PCP along with a progress note. As such, we did not assess testing ordered by PCPs.
Statistical Methods
Data were characterized using descriptive statistics. Frequency reports were generated for each of the outcomes noted previously.
RESULTS
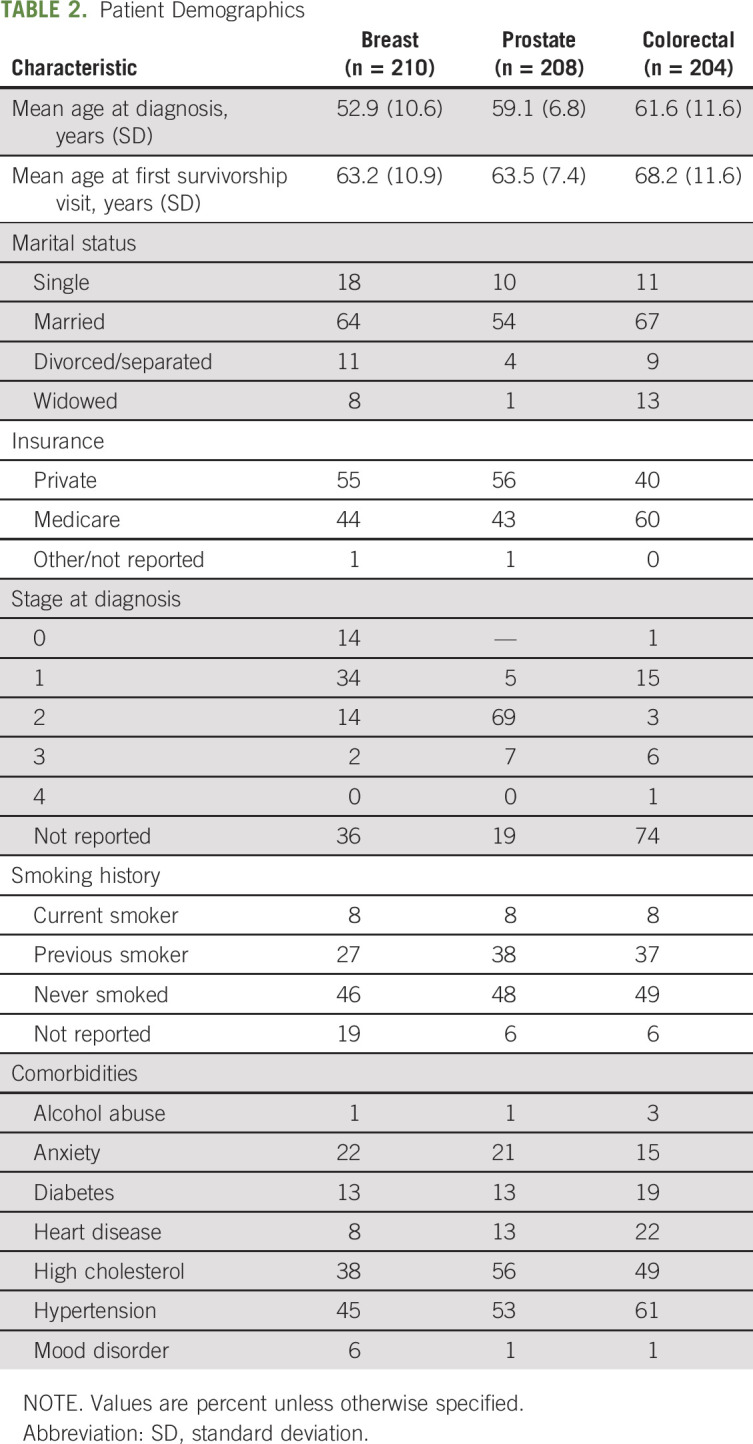
Table 2 lists the patient demographics. Patients with breast cancer in the sample were 53 years old, on average, at diagnosis and 63 years old at the time of their first survivorship visit. The most frequently occurring comorbid conditions among patients with breast cancer were hypertension (45%) and high cholesterol (38%). Patients with prostate cancer were, on average, 59 years old at their diagnosis and 64 years old at their first survivorship visit; 56% of patients with prostate cancer had high cholesterol, and 53% were hypertensive. Among patients with colorectal cancer, the mean age at diagnosis was 62 years, and the mean age at first survivorship visit was 68 years. The most frequently occurring comorbid conditions among patients with colorectal cancer were high cholesterol (61%) and hypertension (49%).
TABLE 2.
Patient Demographics
Among breast cancer survivors, all eligible patients underwent surveillance testing (mammogram; 21 had a bilateral mastectomy as part of treatment and were ineligible for mammography), and 99% received screenings for new primary cancers (colonoscopy, Papanicolaou test). Frequency of discussion of designated health promotion activities ranged from 83% to 100%. Physical symptoms were discussed in 91% of visits, and psychological symptoms were discussed in 93% of visits. Ninety-one percent of patients with breast cancer had a PCP involved in their care, and 70% received an SCP (Table 3).
TABLE 3.
Percentage of Sample Charts/NP Notes Containing Relevant Information
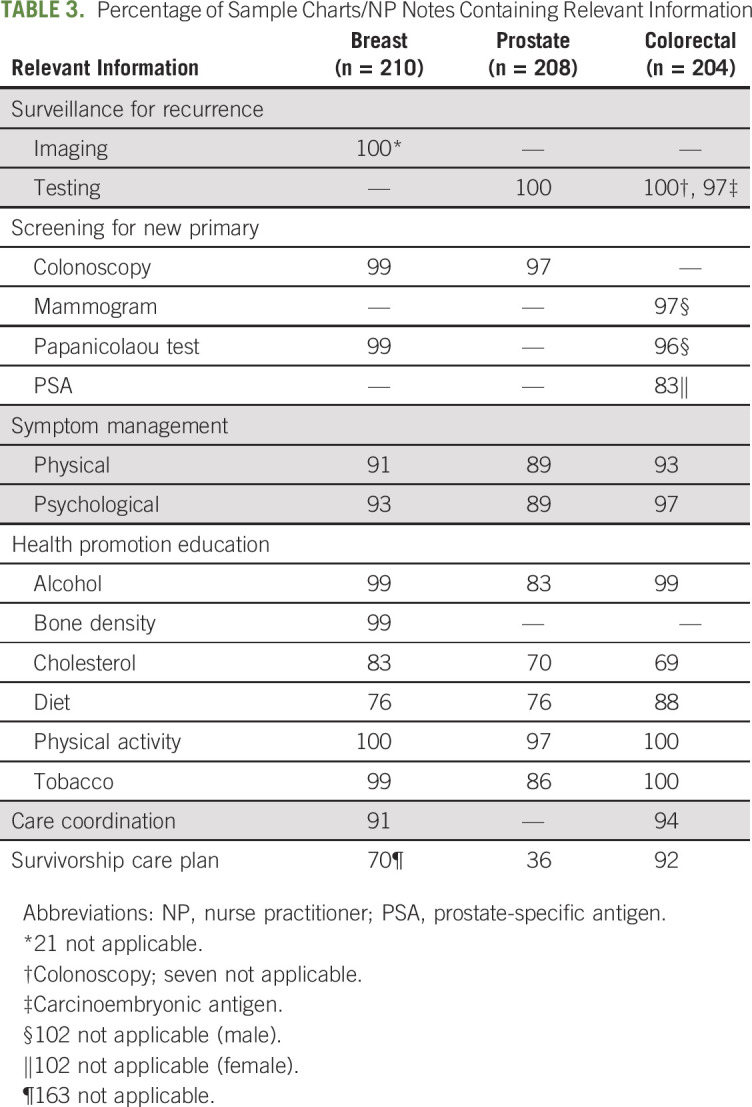
Among prostate cancer survivors, all patients underwent surveillance testing (PSA), and 97% had a colonoscopy for new cancer screening. Health promotion activities were discussed in 70% to 97% of visits, and physical and psychological symptom management was discussed in 89% of visits. Evidence of PCP involvement with this group of patients with prostate cancer could not be determined because of variation in medical record systems at the time of this evaluation, and 36% of prostate survivors received an SCP.
In colorectal cancer survivors, all eligible patients underwent a colonoscopy for surveillance testing (seven patients had total or subtotal colectomy), and 97% had a carcinoembryonic antigen test. Among female colorectal cancer survivors, 97% and 96% had a mammogram and Papanicolaou test, respectively, whereas 83% of male patients had a PSA test. Health promotion education activities were discussed in 69% to 100% of visits, and symptom management was discussed in 93% to 97% of visits. Ninety-four percent of patients with colorectal cancer had a PCP involved in their care, and 92% of patients with colorectal cancer received an SCP.
DISCUSSION
To date, evaluation of the care provided in survivorship care models is lacking, in particular, survivorship care provided by APPs. Thus, our retrospective evaluation is unique in that it takes a broad, practical look at the delivery of recommended services to adult survivors of three common cancers within the APP-led model of survivorship care. The findings from this evaluation demonstrated that the NPs were able to deliver care in adherence with established guidance and to function as independent providers.
The Role of the APP
Increasingly, as health care systems evolve to ensure quality and efficiency in care delivery, there is acknowledgment of the role for APPs in oncology care, with specific emphasis on the post-treatment period.24,31,32 Our choice of NPs as one set of APPs to care for adult cancer survivors was built on a number of reports calling for nurses to practice at the top of their licenses and follows an Agency for Healthcare Research and Quality report that identified NPs as having “the right training and skills to address survivorship issues with patients.”33(p23)
In addition, from a practical perspective, the choice of NPs as sole providers came from the institutional realization that it was important to free up the oncologists to see new patients and was part of the institutional plan to increase APPs in clinical care generally, especially in the outpatient setting. The NPs in our survivorship program all had extensive oncology experience before being hired and gained their survivorship experience through a formal orientation, with sign off by the collaborating physician and an NP nurse leader. The APP training and orientation focused on disease(s), treatment exposures, and associated long-term and late effects, as well as health promotion and cancer screening. Mentorship was essential in reviewing didactic tools and coordinating clinical experiences. Competencies were used to evaluate practice throughout training and at the completion of orientation. After orientation, ongoing mechanisms are used to regularly monitor practice, including clinical case reviews, peer-to-peer evaluation, and documentation audits.
New York State allows NPs to bill health plans; therefore, our survivorship NPs could receive payment from both private payers and Medicare for their independent visits. This allowed for a business plan to support the APP model of survivorship care. We acknowledge that not all states allow for such billing and may prevent independent visits as a financially viable option or limit the role of APPs.
Communication With the PCP
Expanding the focus of the survivorship visit beyond an assessment for recurrence required attention to the incorporation of national standards/guidelines for cancer screening, visit frequency, symptom management, and health promotion in an efficient and consistent manner. It is important to note that it was possible to focus on psychosocial as well as medical issues during the visit, because survivors identify psychosocial concerns as being critical factors in their post-treatment quality of life.34,35 At the same time, these clinics required that the NPs focus specifically on the cancer-related issues, acknowledging that they are sharing care of their survivors with the community PCP. That is, the survivorship APP and the generalist PCP were both involved in the care of the patient at the same time, each with their own set of responsibilities. That the majority of survivors in this sample had a PCP involved in their care is significant, because we know many patients give up their PCP during cancer treatment.36,37 This result is likely due to two reasons: the majority of the sample in this review has insurance—private or public—and the NPs actively sought out PCPs for their patients who did not have one, a responsibility required of the NPs and discussed during their survivorship training and evaluation.
Communication with the PCP in our APP-led clinics included an SCP along with a copy of the most recent progress note; we chose to evaluate the provision of the SCP in this review because it is a standard required by the American College of Surgeons. Staffing difficulties resulted in the low/variable rate of SCP use in the time period studied; in both our prostate and breast cancer clinics, staffing changes and temporary shortages while new NPs were trained necessitated the decision to prioritize the clinic visit over the SCP. Because a progress note was readily available to be sent to the PCP and a process was in place for it to be faxed, the priorities were adapted to focus on the clinical care and suspend the provision of the SCP during the period of change. Since the period under study, our electronic medical record has improved, and SCP templates have been proposed that require a limited data set such that they can be completed in a brief amount of time.38-40
To determine PCP satisfaction with the SCP, we conducted a brief survey of PCPs whose patients were being followed by the survivorship NP. Twenty percent of PCPs responded to the survey, and, of these, 88% stated that they would discuss the SCP with the patient, 70% stated that they received new information, and 33% stated that they would change their plan of care on the basis of the information provided by the NP in the SCP.
Our study is limited because it is the evaluation of the IOM recommendations within the APP model of care at a single academic medical center. Thus, it is important to assess the ability to provide this comprehensive set of services delivered by APPs in other settings, especially in community practices and public hospitals. Finally, the fact that NPs can bill in New York allowed for a business model that included income to be generated by the NPs for their services. In states where this is not possible, other business models would need to be developed to offset the APP services.
In conclusion, this study provides a straightforward evaluation of an APP model of survivorship care demonstrating success in providing IOM-recommended services. Moving forward, it will be important for researchers to continue to evaluate not only the quality of survivorship services, but also the efficiency of the various models of care delivery. In addition, it is essential to move beyond the process measures used in this study—compliance with screening and delivery of medical and psychosocial services—to evaluate health outcomes and determine whether these services accomplish their intended goals. As we move forward with a rigorous evaluation effort in survivorship care, a key component of this research agenda will be the inclusion of patient-reported outcomes to ensure that we have the needed perspective on the outcomes of concern to various survivor populations. Only then will we be able to build a delivery system that ensures the highest quality of care for this growing population.
AUTHOR CONTRIBUTIONS
Conception and design: Bridgette Thom, Annelies H. Boekhout, Stacie Corcoran, Kevin C. Oeffinger, Mary S. McCabe
Financial support: Mary S. McCabe, Kevin C. Oeffinger
Administrative support: Kevin C. Oeffinger, Mary S. McCabe
Provision of study materials or patients: Stacie Corcoran, Mary S. McCabe
Collection and assembly of data: Annelies H. Boekhout, Roberto Adsuar, Kevin C. Oeffinger, Mary S. McCabe
Data analysis and interpretation: Bridgette Thom, Annelies H. Boekhout, Stacie Corcoran, Kevin C. Oeffinger, Mary S. McCabe
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Advanced Practice Providers and Survivorship Care: They Can Deliver
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jop/site/ifc/journal-policies.html.
Bridgette Thom
Stock and Other Ownership Interests: Alder Biopharmaceuticals (I), Inotek Pharmaceuticals (I), OncoSec (I), Caladrius Biosciences (I), Stemline Therapeutics (I), Mediwound (I), Sierra Oncology (I), Affimed Therapeutics (I), Polarity TE (I), Lipocine (I), Amphastar (I), Adverum (I), Rogers Sciences (I), Immunomedics (I), Bellicum Pharmaceuticals (I), Catalyst Pharmaceuticals (I), Ophthotech (I), Krystal Bio (I), Rocket Pharma (I), Adma Pharma (I), Sesen Bio (I), Aerie (I), Alimera Sciences (I), Connecture (I), Sunesis Pharmaceuticals (I), Tesaro (I)
No other potential conflicts of interest were reported.
ACKNOWLEDGMENT
Supported in part through the National Institutes of Health/National Cancer Institute Cancer Center Support Grant No. P30 CA008748. Presented at the 2016 ASCO Annual Meeting, Chicago, IL, June 3 to 7, 2016.
REFERENCES
- 1. Hewitt M, Greenfield S, Stoval E, (eds): From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC, National Academies Press, 2006. [Google Scholar]
- 2. World Health Organization: Estimated cancer incidence, mortality, and prevalence worldwide in 2012. http://GLOBOCAN.iarc.fr/Pages/Summary_table_site_prev_sel.aspx.
- 3.Miller KD, Siegel RL, Lin CC, et al. : Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin 66:271-289, 2016 [DOI] [PubMed] [Google Scholar]
- 4.Bluethmann SM, Mariotto AB, Rowland JH: Anticipating the “silver tsunami”: Prevalence trajectories and comorbidity burden among older cancer survivors in the United States. Cancer Epidemiol Biomarkers Prev 25:1029-1036, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Howlander N, Noone AM, Krapcho M, et al (eds): SEER cancer statistics review, 1975-2010. http://seer.cancer.gov/csr/1975_2010/
- 6.Goldfarb S, Mulhall J, Nelson C, et al. : Sexual and reproductive health in cancer survivors. Semin Oncol 40:726-744, 2013 [DOI] [PubMed] [Google Scholar]
- 7.Koppelmans V, Breteler MM, Boogerd W, et al. : Neuropsychological performance in survivors of breast cancer more than 20 years after adjuvant chemotherapy. J Clin Oncol 30:1080-1086, 2012 [DOI] [PubMed] [Google Scholar]
- 8.Oeffinger KC, Baxi SS, Novetsky Friedman D, et al. : Solid tumor second primary neoplasms: Who is at risk, what can we do? Semin Oncol 40:676-689, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Duijts SF, van Egmond MP, Spelten E, et al. : Physical and psychosocial problems in cancer survivors beyond return to work: A systematic review. Psychooncology 23:481-492, 2014 [DOI] [PubMed] [Google Scholar]
- 10.Skaali T, Fosså SD, Bremnes R, et al. : Fear of recurrence in long-term testicular cancer survivors. Psychooncology 18:580-588, 2009 [DOI] [PubMed] [Google Scholar]
- 11.Landwehr MS, Watson SE, Macpherson CF, et al. : The cost of cancer: A retrospective analysis of the financial impact of cancer on young adults. Cancer Med 5:863-870, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moskowitz MC, Todd BL, Chen R, et al. : Function and friction at work: A multidimensional analysis of work outcomes in cancer survivors. J Cancer Surviv 8:173-182, 2014 [DOI] [PubMed] [Google Scholar]
- 13.Grunfeld E, Hodgson DC, Del Giudice ME, et al. : Population-based longitudinal study of follow-up care for breast cancer survivors. J Oncol Pract 6:174-181, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Earle CC, Burstein HJ, Winer EP, et al. : Quality of non-breast cancer health maintenance among elderly breast cancer survivors. J Clin Oncol 21:1447-1451, 2003 [DOI] [PubMed] [Google Scholar]
- 15.Grunfeld E, Moineddin R, Gunraj N, et al. : Cancer screening practices of cancer survivors: Population-based, longitudinal study. Can Fam Physician 58:980-986, 2012 [PMC free article] [PubMed] [Google Scholar]
- 16.Snyder CF, Frick KD, Peairs KS, et al. : Comparing care for breast cancer survivors to non-cancer controls: A five-year longitudinal study. J Gen Intern Med 24:469-474, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Snyder CF, Frick KD, Kantsiper ME, et al. : Prevention, screening, and surveillance care for breast cancer survivors compared with controls: Changes from 1998 to 2002. J Clin Oncol 27:1054-1061, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blaauwbroek R, Tuinier W, Meyboom-de Jong B, et al. : Shared care by paediatric oncologists and family doctors for long-term follow-up of adult childhood cancer survivors: A pilot study. Lancet Oncol 9:232-238, 2008 [DOI] [PubMed] [Google Scholar]
- 19.Grunfeld E, Levine MN, Julian JA, et al. : Randomized trial of long-term follow-up for early-stage breast cancer: A comparison of family physician versus specialist care. J Clin Oncol 24:848-855, 2006 [DOI] [PubMed] [Google Scholar]
- 20.Helgesen F, Andersson SO, Gustafsson O, et al. : Follow-up of prostate cancer patients by on-demand contacts with a specialist nurse: A randomized study. Scand J Urol Nephrol 34:55-61, 2000 [DOI] [PubMed] [Google Scholar]
- 21.Verschuur EM, Steyerberg EW, Tilanus HW, et al. : Nurse-led follow-up of patients after oesophageal or gastric cardia cancer surgery: A randomised trial. Br J Cancer 100:70-76, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wattchow DA, Weller DP, Esterman A, et al. : General practice vs surgical-based follow-up for patients with colon cancer: Randomised controlled trial. Br J Cancer 94:1116-1121, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oeffinger KC, McCabe MS: Models for delivering survivorship care. J Clin Oncol 24:5117-5124, 2006 [DOI] [PubMed] [Google Scholar]
- 24.Spears JA, Craft M, White S: Outcomes of cancer survivorship care provided by advanced practice RNs compared to other models of care: A systematic review. Oncol Nurs Forum 44:E34-E41, 2017 [DOI] [PubMed] [Google Scholar]
- 25.McCabe MS, Jacobs LA: Clinical update: Survivorship care--Models and programs. Semin Oncol Nurs 28:e1-e8, 2012 [DOI] [PubMed] [Google Scholar]
- 26.Denlinger CS Sanft T Baker KS et al. :. Survivorship, version 2.2017: Clinical practice guidelines in oncology. J Natl Compr Canc Netw 15:1140-1163, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.American Society of Clinical Oncology: Patient and survivor care , 2017. https://www.asco.org/practice-guidelines/quality-guidelines/guidelines/patient-and-survivor-care
- 28.American Cancer Society: American Cancer Society survivorship care guidelines , 2017. https://www.cancer.org/health-care-professionals/american-cancer-society-survivorship-guidelines.html
- 29.Chubak J, Aiello Bowles EJ, Tuzzio L, et al. : Perspectives of cancer survivors on the role of different healthcare providers in an integrated delivery system. J Cancer Surviv 8:229-238, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.United States Preventative Services Task Force: USPSTF recommendations a and b , 2017. https://www.uspreventiveservicestaskforce.org/Page/Name/uspstf-a-and-b-recommendations/
- 31.Post KE, Moy B, Furlani C, et al. : Survivorship model of care: Development and implementation of a nurse practitioner-led intervention for patients with breast cancer. Clin J Oncol Nurs 21:E99-E105, 2017 [DOI] [PubMed] [Google Scholar]
- 32. Institute of Medicine: The Future of Nursing: Leading Change, Advancing Health. Washington, DC, National Academies Press, 2011. [PubMed] [Google Scholar]
- 33.Viswanathan M, Halpern M, Swinson Evans T, et al. : Models of Cancer Survivorship Care. Rockville, MD, Agency for Healthcare Research, and Quality, 2014 [PubMed] [Google Scholar]
- 34.Palmer SC, Stricker CT, DeMichele AM, et al. : The use of a patient-reported outcome questionnaire to assess cancer survivorship concerns and psychosocial outcomes among recent survivors. Support Care Cancer 25:2405-2412, 2017 [DOI] [PubMed] [Google Scholar]
- 35.Stanton AL: What happens now? Psychosocial care for cancer survivors after medical treatment completion. J Clin Oncol 30:1215-1220, 2012 [DOI] [PubMed] [Google Scholar]
- 36.Hauer KE, Durning SJ, Kernan WN, et al. : Factors associated with medical students’ career choices regarding internal medicine. JAMA 300:1154-1164, 2008 [DOI] [PubMed] [Google Scholar]
- 37.Lipner RS, Bylsma WH, Arnold GK, et al. : Who is maintaining certification in internal medicine--and why? A national survey 10 years after initial certification. Ann Intern Med 144:29-36, 2006 [DOI] [PubMed] [Google Scholar]
- 38.Bulloch KJ, Irwin ML, Chagpar AB, et al. : Systematic approach to providing breast cancer survivors with survivorship care plans: A feasibility study. J Oncol Pract 11:e170-e176, 2015 [DOI] [PubMed] [Google Scholar]
- 39.American Society of Clinical Oncology: Survivorship care planning tools , 2017. https://www.asco.org/practice-guidelines/cancer-care-initiatives/prevention-survivorship/survivorship-compendium
- 40. Mayer DK, Taylor K, Gerstel A, et al: Implementing survivorship care plans within an electronic health record. Oncology (Williston Park) 29:980-982, 989, 2015. [PubMed]


