Abstract
This study intended to discover the effect of education and muscle relaxation (EMR) program on anxiety, depression and care burden among caregivers of acute stroke survivors.
This randomized, controlled study enrolled a total of 110 caregivers of first-ever acute stroke patients, and randomly assigned to EMR (N = 55) and control (N = 55) groups. The caregivers in the EMR group received 12-month health education and progressive muscle relaxation, and those in control group were provided common rehabilitation advices. Hospital Anxiety and Depression Scale (HADS) and Zarit Caregiver Burden Scale in caregivers were evaluated at the time of patients’ discharge from hospital (M0), then at month(M) 3, M6 and M12 after the discharge.
HADS-anxiety score, anxiety rate and severity were similar at M0, M3, while were reduced at M6 and M12 in EMR group compared to control group. Furthermore, HADS-depression score was similar at M0 and M3 but was decreased at M6 and M12 in EMR group compared with control group, however, there was no difference of depression rate and severity between the 2 groups at each time point. Moreover, Zarit Caregiver Burden Scale score was similar at M0 and M3, but was decreased at M6 and M12; meanwhile, degree of care burden was similar at M0, M3 and M6, but was reduced at M12 in EMR group compared to control group.
EMR program decreases anxiety, depression and care burden in caregivers of acute stroke survivors, suggesting its potential in improving mental health and further promoting quality of lives in these caregivers.
Keywords: acute stroke, anxiety, care burden, caregiver, depression, education and muscle relaxation
1. Introduction
Stroke ranks as the second leading culprit of global mortality, which is responsible for over 1 million deaths annually.[1] Although the mortality of acute stroke has experienced a dramatic decline considering the recent advancements in acute stroke care interventions and rapid emergency response, the proportion of post-stroke survivors has been elevated, meanwhile, stroke survivors suffer from persistent and significant difficulty in daily tasks.[2] In the duration of post-stroke rehabilitation and recovery for acute stroke survivors, the effort of caregivers is important, while notably, caregivers often experience much stress for dealing with the patients’ social, biological and psychological needs.[3,4] Thus, it is common for caregivers to present psychological disorders (including anxiety and depression) with prevalence of anxiety and depression ranging from 20% to 40%, and with the increment of care burden, the severity of anxiety and depression becomes higher, which further negatively influences the quality of lives in caregivers.[5–8] Therefore, it is important to improve the mental health and alleviate the care burden, which could bring the welfare to the caregivers of acute stroke survivors.
Existing evidences indicate that caregivers feel under-skilled and lack inner strength to deal with complex and demanding caregiving situation, contributing to overwhelming stress and further unfavorable mental health, therefore, some programs on health education have been established targeting caregivers of stroke survivors.[9–11] For example, 1 program, which includes skill-developing education and focuses on social support in caregivers of stroke patients, reliefs depressive symptoms and improves quality of lives in these caregivers.[11] In addition, another study exhibits that a psychoeducational intervention, which enhances problem-solving coping and caregiving competence, presents improvement of family function and social support, decreases care burden in caregivers of stroke survivors.[9] Furthermore, progressive muscle relaxation is an easy approach to deal with anxiety and depression, and a number of researches demonstrate that progressive muscle relaxation exercises are effective in decreasing heart rate and blood pressure, severity of anxiety and depression in patients with various diseases.[10,12–14] According to these aforementioned evidences, we hypothesized that the complex of education and muscle relaxation (EMR) would efficiently improve mental health and decrease care burden in caregivers of acute stroke patients. Hence, in the present study, we designed an EMR program, and evaluated its effect on anxiety, depression and care burden among caregivers of acute stroke survivors.
2. Methods
2.1. Participants
Totally, 110 caregivers of first-ever acute stroke patients who treated in the 2nd Affiliated Hospital of Harbin Medical University from September 2016 to June 2018 were recruited in this randomized, controlled study. The inclusion criteria for caregivers were as follows:
-
(1)
caregiver was a family member of a first-ever acute stroke patient and was also mainly responsible for providing care for the patient.
-
(2)
age of the caregiver more than 18 years;
-
(3)
caregivers without severe psychiatric disease or cognition impairment;
-
(4)
caregivers was able to understand the study contents and finish the related assessments in the study.
The exclusion criteria for caregiver were:
-
(1)
caregivers complicated with malignancies or poorly controlled comorbidities (eg, uncontrolled diabetes, and hypertension);
-
(2)
caregivers with addiction (eg, drug abuse, alcohol abuse);
-
(3)
caregiver with physically disability;
-
(4)
caregivers without interest in participating in the present study.
This study was approved by Institutional Review Board of the 2nd Affiliated Hospital of Harbin Medical University, and all of the participants signed informed consents.
2.2. Basic data collection
Characteristics of acute stroke patients and caregivers were recorded after enrollment. Following information of acute stroke patients were collected: age, gender, smoke status, education duration, marry status, employment status before admission, common complications, disease features, National Institute of Health stroke scale score, mini-mental state examination score. As for caregivers, characteristics including age, gender, education duration, marry status as well as annual income were collected.
2.3. Random allocation
After obtaining written informed consents, 110 caregivers of acute stroke patients were randomly allocated into EMR group (N = 55) or control group (N = 55) as 1:1 ratio. A blocked randomization method with a block size of 4 was used for the random allocation, which could achieve an equal allocation. Intra-block assignment was designed as AABB, ABAB, ABBA, BBAA, BABA, BAAB; and the block was ranked by the random number created by SAS 9.4 software (SAS Institute, Inc., Cary, North Carolina). Caregivers were allocated by a researcher according to the caregivers’ enrolling numbers which were corresponded to the random grouping code.
2.4. Intervention
On the day of discharge from hospital, the caregivers of acute stroke patients in both EMR group and control group were offered a rehabilitation booklet written in an easy and practical language, which covered a range of contents, including basic knowledge about stroke, management of medicine after stroke, secondary stroke prevention, home-based exercise rehabilitation, matters needing attention, nutritional health, mental health, and family support.
In the control group, except for the rehabilitation booklet, investigators also provided common rehabilitation advices to the caregivers of acute stroke patients on the day of discharge from hospital. After discharge, the caregivers of acute stroke patients in control group were required to return to the rehabilitation center of our hospital to finish study assessments at the time specified in the study.
In the EMR group, caregivers of acute stroke patients were invited to rehabilitation center of our hospital twice a month to receive health education and muscle relaxation training for a total of 12 months, which started at the first month after patients were discharged from our hospital. The health education and muscle relaxation was carried out in a form of session, and totally 24 sessions were scheduled in a 12-month intervention duration. Each session lasted 90 minutes and included 3 procedures: a 30-minute health education, a 30-minute muscle relaxation demonstration by investigator, and a 30-minute muscle relaxation practice. The 30-minute health education was given to caregivers by investigators according to the rehabilitation booklet, during which, the caregivers were free to ask any nursing-related questions. The 30-minute muscle relaxation demonstration was conducted by investigators in an orderly way and step by step based on progressive muscle relaxation training method.[15] This technique involved systematically relaxing the major muscle groups of the body with the goal of physical and mental relaxation. The caregivers were instructed the way how to contract and relax the 16 muscle groups (including right hand and forearm, right biceps, left hand and forearm, left biceps, forearm, upper section of cheeks and nose, lower section of cheeks and nose, neck and throat, chest, shoulders and upper part of back, abdominal region and stomach, right thigh, right calf, right foot, left thigh, left calf and left foot). The 30-minute muscle relaxation practice was performed by caregivers with the guidance of the investigators, during which, if caregivers had any questions about muscle relaxation practice, the investigators would demonstrate the essential of exercise again. Besides the session, caregivers in the EMR group were required to do progressive muscle relaxation exercises twice a day at home and record the daily exercise times in a notebook which was provided after first session. In each session, investigators would check the records and supervise the caregivers to do progressive muscle relaxation exercises as required in the study.
2.5. Assessments for caregivers
Anxiety, depression and burden of care of caregivers were assessed at the time of patients’ discharge from hospital (M0), then at the 3rd month (M3), 6th month (M6) and 12th month (M12) after the discharge. Hospital Anxiety and Depression Scale (HADS) was applied for the assessment of anxiety and depression, and Zarit Caregiver Burden Scale (ZCBS) was used for the evaluation of burden of care. The HADS included 2 subscales: HADS for anxiety (HADS-A) and HADS for depression (HADS-D). Both HADS-A and HADS-D consisted of 7 items, and each item was scored ranging from 0 to 3, as a result, the possible scores ranged from 0 to 21 for anxiety and 0 to 21 for depression, respectively. The anxiety was defined as HADS-A score ≥8, and the anxiety severity was classified as follows: 0–7, no anxiety; 8–10, mild anxiety; 11–14, moderate anxiety; 15–21, severe anxiety; The depression was defined as HADS-D score ≥8, and the depression severity was classified as follows: 0–7, no depression; 8–10, mild depression; 11–14, moderate depression; 15–21, severe depression.[16] The ZCBS comprised of 22 statements that measure the effect of caregiving on caregiver life by using a Likert scale from 0 to 4, as follows: 0, “never;” 1, “rarely;” 2, “sometimes;” 3, “quite frequently;” and 4, “nearly always.” The total ZCBS score was ranging from 0 to 88.[17] A higher ZCBS score indicated a higher caregiver burden, and the degree of burden was classified as follows: ZCBS score 0–20 points, no to low maintenance; ZCBS score 21–40 points, low to moderate; ZCBS score 41–60, moderate to severe; ZCBS score 61–88, very high load.
2.6. Sample size estimation
According to a previous study,[10] we hypothesized the mean ZCBS score at M12 was 40 with standard deviation (SD) of 10 in the EMR group and 46 with SD of 10 in the control group. Using PASS 11.0 software (NCSS, Kaysville, Utah), the minimal required sample size was 44 in each group, with a 1:1 ratio, a power of 80% and a significance level of 0.05. Meanwhile, in order to ensure the statistical power, a 20% dropout rate had to take into consideration, as a result, final total sample size was increased to 110 with 55 participants in each group.
2.7. Statistical analysis
Statistical analysis was conducted by SPSS 24.0 software (IBM, Chicago, IL), and graph was plotted by GraphPad Prism 7.01 software (GraphPad Software Inc., San Diego, CA). All data of caregivers were included in the final analysis according to the intention-to-treat principle. The last observation carried forward method was used to deal with the missing data. Data were expressed as mean with SD or number and percentage. Comparison between 2 groups was determined by Student t test, Chi-Square test or Wilcoxon rank sum test. A 2-tailed P value less than .05 was considered as statistically significance.
3. Results
3.1. Study flow
A total of 147 caregivers of acute stroke patient were screened, and 37 of them were excluded, since 28 caregivers disobeyed inclusion criteria or met the exclusion criteria and 9 caregivers refused to participate (Fig. 1). The remaining 110 caregivers were recruited, and randomized at a 1:1 ratio into EMR group (N = 55) and control group (N = 55). During the intervention of 12 months, HADS-A/HADS-D was applied for the assessment of anxiety and depression, and ZCBS was used for the evaluation of care burden at M0, M3, M6 and M12, respectively. In EMR group, there were 10 dropouts (including 6 caregivers who lost follow-up (10.9%) and 4 caregivers who dropped out due to patients’ death (7.3%)). In control group, there were 7 dropouts (including 6 caregivers who lost follow-up (10.9%) and 1 caregiver who dropped out due to patients’ death (1.8%)). At last, all 55 subjects in EMR group and all 55 subjects in control group were included in the final analysis based on intention-to-treat principle.
Figure 1.
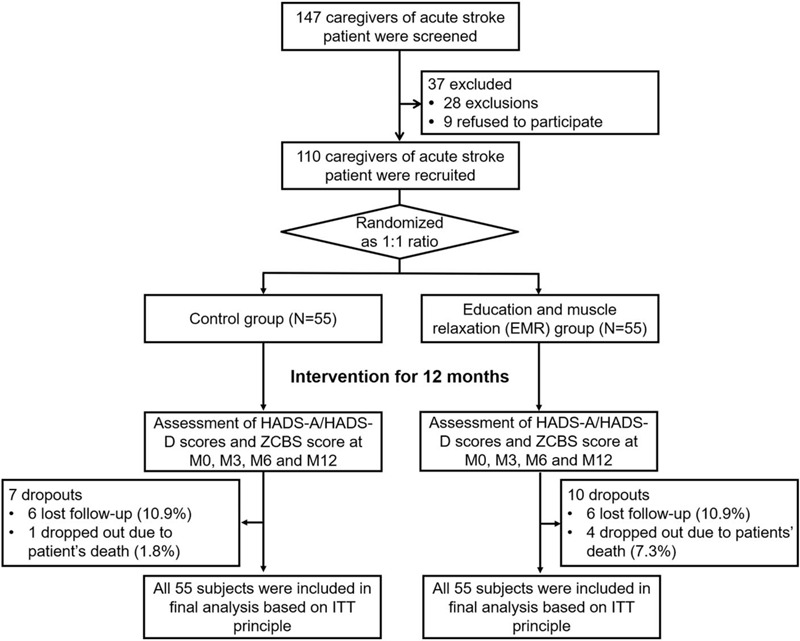
Study flow. HADS-A = Hospital Anxiety and Depression Scale for anxiety, HADS-D = Hospital Anxiety and Depression Scale for depression, ITT = intention-to-treat, ZCBS = Zarit Caregiver Burden Scale.
3.2. Clinical characteristics of acute stroke patients between 2 groups
The average age of acute stroke patients in EMR group and control group was 67.4 ± 9.5 years and 68.4 ± 9.7 years, respectively (Table 1). Among the acute stroke patients in EMR group, the number of female patients and male patients were 21 (38.2%) and 34 (61.8%), respectively; meanwhile, among the acute stroke patients in control group, the number of female patients and male patients were 16 (29.1%) and 39 (70.9%), respectively. Furthermore, the comparison of clinical characteristics between acute stroke patients in EMR group and those in control group revealed that there was no difference of age, gender, current smoker, education duration, marry status, employment status before admission, common complications, disease features (all P > .05). The detailed information of characteristics in acute stroke patients between 2 groups was exhibited in Table 1.
Table 1.
Characteristics of acute stroke patients.
| Items | Control group (N = 55) | EMR group (N = 55) | P value |
| Basic characteristics | |||
| Age (yr), mean ± SD | 68.4 ± 9.7 | 67.4 ± 9.5 | .584 |
| Sex, No. (%) | .313 | ||
| Female | 16 (29.1) | 21 (38.2) | |
| Male | 39 (70.9) | 34 (61.8) | |
| Current smoker, No. (%) | .654 | ||
| No | 41 (74.5) | 43 (78.2) | |
| Yes | 14 (25.5) | 12 (21.8) | |
| Education duration (years), mean ± SD | 7.0 ± 4.5 | 7.4 ± 3.4 | .600 |
| Marry status, No. (%) | .703 | ||
| Single/divorced/widowed | 26 (47.3) | 28 (50.9) | |
| Married | 29 (52.7) | 27 (49.1) | |
| Employment status before admission, No. (%) | .221 | ||
| Unemployed | 47 (85.5) | 51 (92.7) | |
| Employed | 8 (14.5) | 4 (7.3) | |
| Common complications | |||
| Hypertension, No. (%) | .606 | ||
| No | 10 (18.2) | 8 (14.5) | |
| Yes | 45 (81.8) | 47 (85.5) | |
| Hyperlipidemia, No. (%) | .550 | ||
| No | 21 (38.2) | 18 (32.7) | |
| Yes | 34 (61.8) | 37 (67.3) | |
| Diabetes, No. (%) | .539 | ||
| No | 39 (70.9) | 36 (65.5) | |
| Yes | 16 (29.1) | 19 (34.5) | |
| Disease features | |||
| Lesion location, No. (%) | .483 | ||
| Left | 19 (34.5) | 22 (40.0) | |
| Right | 22 (40.0) | 16 (29.1) | |
| Bilateral/brainstem/unknown | 14 (25.5) | 17 (30.9) | |
| NIHSS score, mean ± SD | 8.7 ± 4.1 | 8.1 ± 2.7 | .369 |
| MMSE score, mean ± SD | 26.7 ± 2.3 | 26.5 ± 2.0 | .182 |
Comparison was determined by Student t test or Chi-square test. EMR = education and muscle relaxation, MMSE = mini-mental state examination, NIHSS = National Institute of Health stroke scale, SD = standard deviation.
3.3. Basic characteristics of caregivers between 2 groups
The average age of caregivers was 47.3 ± 10.4 years in EMR group and 47.6 ± 10.2 years in control group (Table 2). As for gender, there were 40 (72.7%) female caregivers and 15 (27.3%) male caregivers in EMR group; 44 (80.0%) females and 11 (20.0%) males in control group. No difference of age, gender, education duration, marry status, annual income was observed between 2 groups (all P > .05). The detailed information of basic characteristics in caregivers was exhibited in Table 2.
Table 2.
Basic characteristics of caregivers.
| Items | Control group (N = 55) | EMR group (N = 55) | P value |
| Age (yr), mean ± SD | 47.6 ± 10.2 | 47.3 ± 10.4 | .875 |
| Sex, No. (%) | .369 | ||
| Female | 44 (80.0) | 40 (72.7) | |
| Male | 11 (20.0) | 15 (27.3) | |
| Education duration (yr), mean ± SD | 10.9 ± 3.7 | 11.6 ± 4.7 | .422 |
| Marry status, No. (%) | .279 | ||
| Single/divorced/widowed | 6 (10.9) | 10 (18.2) | |
| Married | 49 (89.1) | 45 (81.8) | |
| Annual income (∗), No. (%) | .972 | ||
| < 10000 | 5 (9.1) | 2 (3.6) | |
| 10000-30000 | 12 (21.8) | 16 (29.1) | |
| 30000-50000 | 28 (50.9) | 27 (49.1) | |
| > 50000 | 10 (18.2) | 10 (18.2) |
Comparison was determined by Student t test, Chi-square test or Wilcoxon rank sum test. EMR = education and muscle relaxation, SD = standard deviation.
RMB.
3.4. Comparison of HADS-A score and anxiety rate between 2 groups
Anxiety of caregivers was evaluated at M0, M3, M6 and M12, which observed that HADS-A score was decreased at M6 (5.7 ± 2.3 vs. 6.9 ± 3.4, P = .040) and M12 (5.4 ± 2.3 vs 7.1 ± 3.9, P = .006), while was similar at M0 (5.7 ± 2.6 vs 6.2 ± 2.7, P = .335) and M3 (5.8 ± 2.7 vs 6.4 ± 3.0, P = .261) in EMR group compared with control group (Fig. 2A). Meanwhile, anxiety rate was also decreased at M6 (18.2% vs 38.2%, P = .020) and M12 (16.4% vs 38.2%, P = .010) but was similar at M0 (20.0% vs. 23.6%, P = .644) and M3 (20.0% vs 30.9%, P = .189) in EMR group compared with control group (Fig. 2B).
Figure 2.
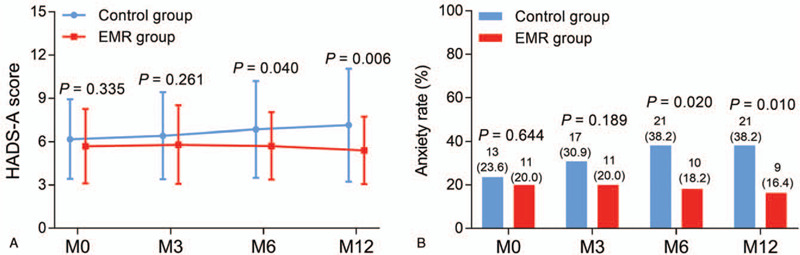
Anxiety condition in EMR group and control group. Comparison of HADS-A score between EMR group and control group at M0, M3, M6 and M12 (A). Comparison of anxiety rate between EMR group and control group at M0, M3, M6 and M12 (B). EMR = education and muscle relaxation, HADS-A = Hospital Anxiety and Depression Scale for anxiety, M0 = time of patients’ discharge from hospital, M12 = at the 12th month after discharge, M3 = at the 3rd month after discharge, M6 = at the 6th month after discharge.
3.5. Comparison of anxiety severity between 2 groups
Anxiety severity was classified to be no anxiety (HADS-A score: 0–7), mild anxiety (HADS-A score: 8–10), moderate anxiety (HADS-A score: 11–14) and severe anxiety (HADS-A score: 15–21). EMR group presented less anxiety severity at M6 (P = .019) and M12 (P = .006), but showed no difference of anxiety severity at M0 (P = .616) and M3 (P = .209) compared to control group (Table 3). The detailed information of anxiety severity between 2 groups was shown in Table 3.
Table 3.
Anxiety severity of caregivers.
| Items | Control group (N = 55) | EMR group (N = 55) | P value |
| M0 anxiety severity, No. (%) | .616 | ||
| No | 42 (76.4) | 44 (80.0) | |
| Mild | 8 (14.5) | 7 (12.7) | |
| Moderate | 3 (5.5) | 4 (7.3) | |
| Severe | 2 (3.6) | 0 (0.0) | |
| M3 anxiety severity, No. (%) | .209 | ||
| No | 38 (69.1) | 44 (80.0) | |
| Mild | 12 (21.8) | 7 (12.7) | |
| Moderate | 3 (5.5) | 3 (5.5) | |
| Severe | 2 (3.6) | 1 (1.8) | |
| M6 anxiety severity, No. (%) | .019 | ||
| No | 34 (61.8) | 45 (81.8) | |
| Mild | 14 (25.4) | 7 (12.7) | |
| Moderate | 4 (7.3) | 3 (5.5) | |
| Severe | 3 (5.5) | 0 (0.0) | |
| M12 anxiety severity, No. (%) | .006 | ||
| No | 34 (61.8) | 46 (83.7) | |
| Mild | 11 (20.0) | 7 (12.7) | |
| Moderate | 5 (9.1) | 2 (3.6) | |
| Severe | 5 (9.1) | 0 (0.0) |
Comparison was determined by Wilcoxon rank sum test. EMR = education and muscle relaxation, M0 = time of patients’ discharge from hospital, M12 = at the 12th month after discharge, M3 = at the 3rd month after discharge, M6 = at the 6th month after discharge.
3.6. Comparison of HADS-D score and depression rate between 2 groups
Depression of caregivers was assessed at M0, M3, M6 and M12, which observed that HADS-D score was reduced at M6 (6.1 ± 1.7 vs 7.0 ± 2.5, P = .036) and M12 (6.3 ± 1.7 vs 7.2 ± 2.4, P = .018) but similar at M0 (5.7 ± 2.2 vs 5.9 ± 2.5, P = .537) and M3 (6.1 ± 2.2 vs 6.4 ± 2.5, P = .445) in EMR group compared with control group (Fig. 3A). Furthermore, depression rate was of no difference at M0 (20.0% vs 21.8%), M3 (20.0% vs 27.3%), M6 (21.8% vs 32.7%) and M12 (23.6% vs. 38.2%) between EMR group and control group (all P > .05) (Fig. 3B).
Figure 3.
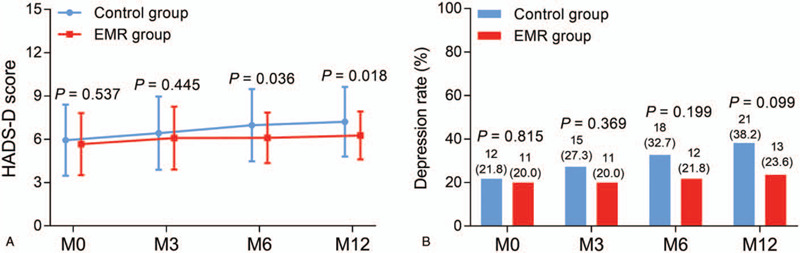
Depression condition in EMR group and control group. Comparison of HADS-D score between EMR group and control group at M0, M3, M6 and M12 (A). Comparison of depression rate between EMR group and control group at M0, M3, M6 and M12 (B). EMR = education and muscle relaxation, HADS-D = Hospital Anxiety and Depression Scale for depression, M0 = time of patients’ discharge from hospital, M12 = at the 12th month after discharge, M3 = at the 3rd month after discharge, M6 = at the 6th month after discharge.
3.7. Comparison of depression severity between 2 groups
Depression severity was defined to be no depression (HADS-D score: 0–7), mild depression (HADS-D score: 8–10), moderate depression (HADS-D score: 11–14), and severe depression (HADS-A score: 15–21). EMR group exhibited no difference of depression severity at M0, M3, M6 and M12 compared with control group (all P > .05) (Table 4). The detailed information of depression severity between 2 groups was displayed in Table 4.
Table 4.
Depression severity of caregivers.
| Items | Control group (N = 55) | EMR group (N = 55) | P value |
| M0 depression severity, No. (%) | .745 | ||
| No | 43 (78.2) | 44 (80.0) | |
| Mild | 8 (14.5) | 9 (16.4) | |
| Moderate | 3 (5.5) | 2 (3.6) | |
| Severe | 1 (1.8) | 0 (0.0) | |
| M3 depression severity, No. (%) | .449 | ||
| No | 41 (74.6) | 44 (80.0) | |
| Mild | 10 (18.2) | 9 (16.4) | |
| Moderate | 2 (3.6) | 2 (3.6) | |
| Severe | 2 (3.6) | 0 (0.0) | |
| M6 depression severity, No. (%) | .152 | ||
| No | 37 (67.3) | 43 (78.2) | |
| Mild | 13 (23.6) | 11 (20.0) | |
| Moderate | 4 (7.3) | 1 (1.8) | |
| Severe | 1 (1.8) | 0 (0.0) | .080 |
| M12 depression severity, No. (%) | |||
| No | 34 (61.8) | 42 (76.4) | |
| Mild | 17 (31.0) | 12 (21.8) | |
| Moderate | 2 (3.6) | 1 (1.8) | |
| Severe | 2 (3.6) | 0 (0.0) |
Comparison was determined by Wilcoxon rank sum test. EMR = education and muscle relaxation, M0 = time of patients’ discharge from hospital, M12 = at the 12th month after discharge, M3 = at the 3rd month after discharge, M6 = at the 6th month after discharge.
3.8. Comparison of care burden between 2 groups
Care burden of caregivers was evaluated at M0, M3, M6, and M12, which revealed that ZCBS score was lower at M6 (43.5 ± 11.6 vs. 48.5 ± 14.3, P = .046) and M12 (42.9 ± 10.9 vs 49.5 ± 14.9, P = .009), but was of no difference at M0 (40.3 ± 13.7 vs 41.4 ± 12.9, P = .652) and M3 (42.6 ± 13.9 vs 44.6 ± 12.7, P = .438) in EMR group compared to control group (Fig. 4).
Figure 4.
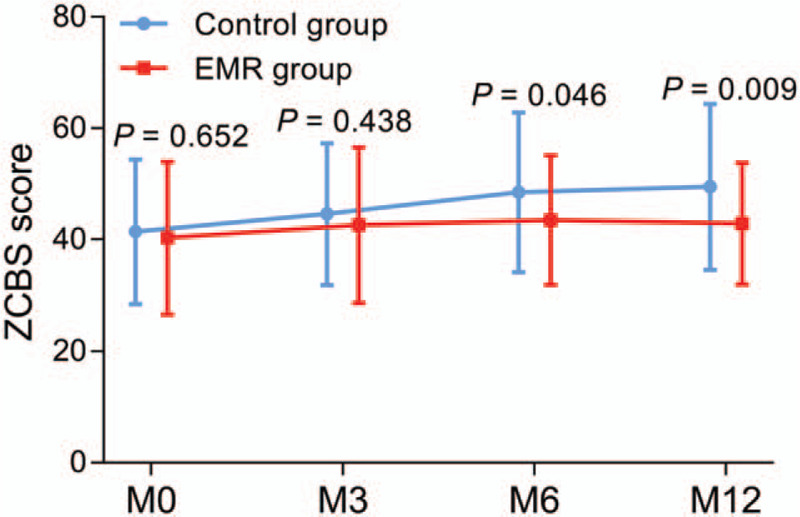
Care burden in EMR group and control group. Comparison of ZCBS score between EMR group and control group at M0, M3, M6 and M12. EMR = education and muscle relaxation, M0 = time of patients’ discharge from hospital, M12 = at the 12th month after discharge, M3 = at the 3rd month after discharge, M6 = at the 6th month after discharge, ZCBS = Zarit Caregiver Burden Scale.
3.9. Comparison of care burden degree between 2 groups
The degrees of care burden in caregivers was classified according to ZCBS score, which were as follows: no to low maintenance (ZCBS score: 0–20 points), low to moderate (ZCBS score: 21–40 points), moderate to severe (ZCBS score: 41–60 points), very high load (ZCBS score: 61–88 points). EMR group showed decreased degree of care burden at M12 (P = .031), but similar degree of care burden at M0 (P = .817), M3 (P = .710) and M6 (P = .098) compared with control group (Table 5). The detailed information of care burden degree between 2 groups was displayed in Table 5.
Table 5.
The degree of burden of caregivers.
| Items | Control group (N = 55) | EMR group (N = 55) | P value |
| M0 degree of burden, No. (%) | .817 | ||
| No to low maintenance | 1 (1.8) | 0 (0.0) | |
| Low to moderate | 30 (54.5) | 34 (61.8) | |
| Moderate to severe | 19 (34.6) | 14 (25.5) | |
| Very high load | 5 (9.1) | 7 (12.7) | |
| M3 degree of burden, No. (%) | .710 | ||
| No to low maintenance | 0 (0.0) | 0 (0.0) | |
| Low to moderate | 27 (49.1) | 31 (56.4) | |
| Moderate to severe | 22 (40.0) | 15 (27.2) | |
| Very high load | 6 (10.9) | 9 (16.4) | |
| M6 degree of burden, No. (%) | .098 | ||
| No to low maintenance | 0 (0.0) | 0 (0.0) | |
| Low to moderate | 23 (41.8) | 29 (52.7) | |
| Moderate to severe | 19 (34.6) | 21 (38.2) | |
| Very high load | 13 (23.6) | 5 (9.1) | |
| M12 degree of burden, No. (%) | .031 | ||
| No to low maintenance | 0 (0.0) | 0 (0.0) | |
| Low to moderate | 20 (36.4) | 28 (50.9) | |
| Moderate to severe | 23 (41.8) | 24 (43.6) | |
| Very high load | 12 (21.8) | 3 (5.5) |
Comparison was determined by Wilcoxon rank sum test. EMR = education and muscle relaxation, M0 = time of patients’ discharge from hospital, M12 = at the 12th month after discharge, M3 = at the 3rd month after discharge, M6 = at the 6th month after discharge.
4. Discussion
Stroke often contributes to chronic disability and difficulties of daily lives among stroke survivors, and it is common for the majority of stroke survivors to be dependent on others (such as caregivers) to continue their normal daily lives.[4] Therefore, caregivers play important roles in supporting stroke survivors during the post-stroke process, and offer care services including personal care (feeding, toileting, bathing, etc), health care (stroke monitoring, functional rehabilitation, management of stroke complication, etc), social support, which might disrupt the normal life and work of caregivers, thus leading to heavy burden and poor mental status to a certain extent.[18] According to the previous data, about 68.4% of the caregivers display moderate and severe care burden, and it is indicated that care burden burnout is correlated with several factors, including caregiving hours, the stroke severity at discharge, health-related quality of life in patients, the presence of atrial fibrillation in patients, and the degree of dependence.[18,19] In addition, the undesirable mental states exert a negative influence on the social function, physical health state, and quality of lives in caregivers, further leading to worse caregiving for stroke survivors.[18] A number of programs are designed to improve psychosocial outcomes and mental health in caregivers of stroke survivors.[9,10] For instance, a strength-oriented psychoeducational program improves greatly caregiving competence, problem-solving coping abilities and social support satisfaction, thus reducing care burden in caregivers of stroke survivors.[9] However, the interventions for the improvement of mental health and relief of care burden in caregivers are still limited. Hence, in the present study, we aimed to design an EMR program involving education and muscle relaxation, and explored the effect of EMR on the anxiety, depression and care burden in caregivers for acute stroke survivors.
For the effect of EMR program on anxiety in caregivers of acute stroke patients, we observed that the prevalence of anxiety and its severity were of no difference at M0 and M3, but were decreased at M6 and M12 in caregivers receiving EMR program compared to caregivers who received common rehabilitation advices, suggesting that EMR program presented capability in decreasing anxiety in caregivers of acute stroke survivors. The possible reasons might include that
According to prior evidence, progressive muscle relaxation training method reduced heart rate, respiratory rate, blood pressure and physiological tension to some extent, further achieving a deep state of relaxation, which has been applied among different patient groups with anxiety.[12–14] As EMR program comprises progressive muscle relaxation training, therefore, we speculated that EMR presented anti-anxiety effect in caregivers of acute stroke survivor.
Apart from progressive muscle relaxation training method, EMR group also included the health education, which offered opportunities to improve the problem-solving abilities and establish the self-confidence to cope with stressful condition in caregivers.[9] Considering that mental status was largely influenced by stress from the complex and demanding tasks of caregiving, support to deal with stressful caregiving situations was speculated to improve the psychological status and relieve anxiety.[9]
Furthermore, routine health education and muscle relaxation provided caregivers chances to receive social support, thus helping them recover the social function and further decreasing anxiety in caregivers of acute stroke survivors.[20]
Regarding the effect of EMR program on depression in caregivers of acute stroke survivors, we found that depression rate and severity exhibited decreased trends in caregivers who received EMR program compared to those who received common rehabilitation advices, implying the positive effect of EMR on the decrease of depression to some extent. The possible reasons might include that
EMR program included health education, which was reported to improve the caregiving competence, and help caregivers to have muscle relaxation, which both decreased the depression status.[9,21]
A 12-month intervention duration was not sufficient to observe the significant change in depression score, therefore, depression rate and severity was of no difference between caregivers who received EMR and caregivers who received common rehabilitation advices.
Furthermore, with the increment of caregiving duration, depression would continually aggravate, which weakened the effect of EMR program.
Additionally, the lack of the significant difference in depression status between 2 groups might attribute to the relatively small sample size.[13,21]
Furthermore, we observed that care burden as well as the degree of care burden was decreased in caregivers receiving EMR program compared to those who received common rehabilitation advices, suggesting the effect of EMR on the relief of care burden in caregivers of acute stroke survivors. The possible reasons might include that
Muscle relaxation directly released body burden and further reduced emotional stress, therefore, caregiver receiving EMR program presented lower level of care burden compared with those who received common rehabilitation advices.
Considering that there existed a close correlation of care burden with anxiety and depression in caregivers of stroke survivors, and given the prior results that EMR decreased anxiety and depression status, caregivers therefore presented reduced care burden indirectly via decreasing anxiety and depression.[8,18]
Furthermore, previous papers indicated that the health education about functional rehabilitation improved caregiving competence of caregivers, which might accelerate functional recovery of acute stroke survivors.[9]
Meanwhile, considering that 1 determinant of increased caregiver burden was functional independent of stroke survivors, caregivers therefore presented decreased care burden after receiving EMR.[10,18,19]
However, the present study existed some limitations as follows:
The present study was a single-center study with relatively small sample size, and more patients from multiple centers were needed for validation.
The current study involved a 12-month EMR program, which was relatively short, therefore, the long-term effect of EMR on anxiety, depression and care burden needed further exploration.
Considering that numerous data would make our results too complicated and unreadable, we did not include the disease progression of stroke survivors during the follow-up in our analysis, which might have direct influence on the status of anxiety, depression and care burden in caregivers.
In conclusion, EMR program decreases anxiety, depression and care burden in caregivers of acute stroke survivors, suggesting its potential in improving mental health and further promoting quality of lives in these caregivers.
Author contributions
Conceptualization: Shihong Yue, Zhaojun Liu.
Data curation: Jinhong Wang, Jie Liu.
Formal analysis: Jinhong Wang, Jing Man.
Funding acquisition: Shihong Yue, Zhaojun Liu.
Investigation: Jie Liu, Ling Li, Jing Man.
Methodology: Jinhong Wang, Jie Liu.
Resources: Jie Liu, Ling Li, Jing Man, Shihong Yue, Zhaojun Liu.
Supervision: Shihong Yue, Zhaojun Liu.
Validation: Ling Li.
Writing – original draft: Ling Li, Jing Man.
Writing – review and editing: Shihong Yue, Zhaojun Liu.
Glossary
Abbreviations: EMR = education and muscle relaxation, HADS = Hospital Anxiety and Depression Scale, HADS-A = HADS for anxiety, HADS-D = HADS for depression, SD = standard deviation, ZCBS = Zarit Caregiver Burden Scale.
References
- [1].Peisker T, Koznar B, Stetkarova I, et al. Acute stroke therapy: a review. Trends Cardiovasc Med 2017;27:59–66. [DOI] [PubMed] [Google Scholar]
- [2].Teasell R, Salbach NM, Foley N, et al. Canadian stroke best practice recommendations: rehabilitation, recovery, and community participation following stroke. part one: rehabilitation and recovery following stroke; 6th Edition Update 2019. Int J Stroke 2020;15:763–88. [DOI] [PubMed] [Google Scholar]
- [3].Winstein CJ, Stein J, Arena R, et al. Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2016;47:e98–169. [DOI] [PubMed] [Google Scholar]
- [4].Tyagi S, Koh GC, Nan L, et al. Healthcare utilization and cost trajectories post-stroke: role of caregiver and stroke factors. BMC Health Serv Res 2018;18:881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Akosile CO, Banjo TO, Okoye EC, et al. Informal caregiving burden and perceived social support in an acute stroke care facility. Health Qual Life Outcomes 2018;16:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Denno MS, Gillard PJ, Graham GD, et al. Anxiety and depression associated with caregiver burden in caregivers of stroke survivors with spasticity. Arch Phys Med Rehabil 2013;94:1731–6. [DOI] [PubMed] [Google Scholar]
- [7].Efi P, Fani K, Eleni T, et al. Quality of life and psychological distress of caregivers’ of stroke people. Acta Neurol Taiwan 2017;26:154–66. [PubMed] [Google Scholar]
- [8].Loh AZ, Tan JS, Zhang MW, et al. The global prevalence of anxiety and depressive symptoms among caregivers of stroke survivors. J Am Med Dir Assoc 2017;18:111–6. [DOI] [PubMed] [Google Scholar]
- [9].Cheng HY, Chair SY, Chau JPC. Effectiveness of a strength-oriented psychoeducation on caregiving competence, problem-solving abilities, psychosocial outcomes and physical health among family caregiver of stroke survivors: a randomised controlled trial. Int J Nurs Stud 2018;87:84–93. [DOI] [PubMed] [Google Scholar]
- [10].Yilmaz CK, Asiret GD, Cetinkaya F, et al. Effect of progressive muscle relaxation on the caregiver burden and level of depression among caregivers of older patients with a stroke: a randomized controlled trial. Jpn J Nurs Sci 2019;16:202–11. [DOI] [PubMed] [Google Scholar]
- [11].Bakas T, Austin JK, Habermann B, et al. Telephone assessment and skill-building kit for stroke caregivers: a randomized controlled clinical trial. Stroke 2015;46:3478–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Liu K, Chen Y, Wu D, et al. Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID-19. Complement Ther Clin Pract 2020;39:101132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Ramasamy S, Panneerselvam S, Govindharaj P, et al. Progressive muscle relaxation technique on anxiety and depression among persons affected by leprosy. J Exerc Rehabil 2018;14:375–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Hasanpour-Dehkordi A, Solati K, Tali SS, et al. Effect of progressive muscle relaxation with analgesic on anxiety status and pain in surgical patients. Br J Nurs 2019;28:174–8. [DOI] [PubMed] [Google Scholar]
- [15].Kieffer M. Progressive relaxation. Dr. E. Jacobson's method. Bull Soc Sci Med Grand Duche Luxemb 1978;115:83–7. [PubMed] [Google Scholar]
- [16].Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. [DOI] [PubMed] [Google Scholar]
- [17].Zarit SH, Zarit JM. The Memory and Behavior Problems Checklist and the Burden Interview. University Park, PA: Pennsylvania State University Gerontology. [Google Scholar]
- [18].Hu P, Yang Q, Kong L, et al. Relationship between the anxiety/depression and care burden of the major caregiver of stroke patients. Medicine (Baltimore) 2018;97:e12638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Oliva-Moreno J, Pena-Longobardo LM, Mar J, et al. Determinants of informal care, burden, and risk of burnout in caregivers of stroke survivors: the CONOCES study. Stroke 2018;49:140–6. [DOI] [PubMed] [Google Scholar]
- [20].Tough H, Siegrist J, Fekete C. Social relationships, mental health and wellbeing in physical disability: a systematic review. BMC Public Health 2017;17:414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Klainin-Yobas P, Oo WN, Suzanne Yew PY, et al. Effects of relaxation interventions on depression and anxiety among older adults: a systematic review. Aging Ment Health 2015;19:1043–55. [DOI] [PubMed] [Google Scholar]


