Abstract
Background:
Intensive neuromuscular stabilization exercise on highly obese patients with low back pain results in positive effects of body fat decline and prevention of complications. The purpose of this study is to investigate the effects of progressive neuromuscular stabilization exercise on unstable surface on pain, motor function, psychosocial factors, balance, and abdominal contraction with highly obese patients with lumbar instability.
Methods:
This study is a double-blinded randomized controlled trial. A total of 46 highly obese patients (body mass index [BMI] ≥ 30 kg/m2) with lumbar instability were assigned randomly to experimental group (n = 23) and control group (n = 23). The control group performed the intensive progressive exercise on a stable surface and the experimental group on an unstable surface.
Result:
Significant differences were shown for BMI, QVAS, K-ODI, FABQ, and balance ability for both groups before and after the intervention (P < .05), and only the experimental group showed significant difference for transverse abdominis muscle thickness in contraction and contraction rate (P < .05). Compared to the control group, the experimental group showed significant difference (P < .05) in the amount of changes for QVAS, K-ODI, balance ability, transverse abdominis muscle thickness in contraction, and contraction rate.
Conclusion:
Progressive neuromuscular stabilization exercise program on unstable surfaces demonstrated to be an effective and clinically useful method to decrease pain level, increase motor function, balance, and transverse abdominis muscle thickness in contraction and contraction rate for highly obese patients with lumbar instability.
Keywords: back pain, exercise therapy, obesity, postural balance, progressive patient care
1. Introduction
Low back pain is a neuromuscular dysfunction and a chronic disease with high incidence. Development of information media such as the Internet increased the time spent sitting, and resulted in many health-related problems like office work type of environment, decline in physical activities due to automated systems, improper postures, and insufficient exercise.[1] Development of information media such as the Internet increased the time spent sitting, and resulted in many health-related problems like office work type of environment, decline in physical activities due to automated systems, improper postures, and insufficient exercise, Lumbar instability and decreased balance may occur due to deep lumbar muscle weakness and decreased proprioception from the lumbar dysfunction.[2] Additionally with low back pain, there are tendencies for psychological intimidation and anxiety. Therefore, it is considered an important factor within the psychosocial aspect.
The causes of low back pain are structural factors from spinal lesions, psychological factors from stress, and decreased dynamic dysfunction of the neuromuscular system. Among the causes, the main factor is reported to be lumbar instability due to weaknesses of the lumbar muscles and ligaments from insufficient exercise. In order to improve the deep muscles and stabilize lumbar instability, stabilization of the muscles and neuromuscular control must be enhanced.[3] In addition, maintaining proper posture in everyday life is also essential.
Obesity is a factor that decreases the quality of life more than smoking or alcohol consumption, and is also a social issue that yields high social expenditures. Modern people have increased body weight due to shifted lifestyle to over consumption of fast foods and insufficient exercise, and these lifestyles resulted in quick increase of obesity prevalence.[4] Abdominal obesity causes imbalances in the muscles around the pelvis. Compensation of the weakened abdominal muscles causes shortened hip flexors and pelvic anteversion, leading to low back pain from the lordosis.[5] Additionally, abnormal pressure is applied to the spine in obese patients, resulting in chronic low back pain along with cardiovascular, circulatory, and muscular complications. Therefore obesity must be prevented and treated along with maintaining proper eating habits, increased physical activities, and exercising regularly to promote positive effects in decreasing body fat and cardiovascular diseases.[6]
Obese patients with low back pain have higher levels of dysfunction, pain, and decreased functional status than nonobese low back pain patients. Thereby low back pain and obesity have positive correlation with economical, social, and clinical issues.[7] The effects of stabilization exercise program through muscle contractions have been reported to decrease low back pain and enhance functional recovery. Specifically, the muscles of each body segment yield more muscular mobilization to maintain balance on unstable surfaces. This affects joint stability by activating gamma motor neurons. In addition, exercises on unstable surfaces stimulate neuromuscular system to enhance muscle strength, balance, and optimize exercise effects.[8]
Excessive obesity in the abdominal area inhibits the role of the abdominal muscles resulting in severity of low back pain symptoms. Among the deep muscles that stabilized the trunk, transversus abdominis (TrA) increases the intra-abdominal pressure to stabilize the lumbar area. In order to obtain accurate contraction of TrA, abdominal drawing-in maneuver must be used, and it needs to be selectively contracted before other deep muscle contraction. Additionally, it is important to determine and compare muscle size, thickness, and fiber structures for assessment and analysis of TrA functions.[9]
Through many existing studies demonstrated the effectiveness of trunk stabilization exercise programs to improve low back pain.[10] However, there is a lack of evidence on positive effects of exercise interventions to obese low back pain patients in regards to decrease of body fat and prevention of complications. Therefore this study aims to investigate the effects of progressive neuromuscular stabilization exercise on unstable surface has on pain, motor function, psychosocial factors, balance, and TrA thickness and contraction rate of obese patients with low back pain.
2. Study methods
2.1. Participants
This study recruited patients who are admitted or outpatients of P hospital in D city. Among the patients, 71 participants who voluntarily participated in the intervention were provided with comprehensive information about the study purpose. The inclusion criteria were persons who have experienced low back pain within 6 weeks, higher than 3 points in quadruple visual analogue scale (QVAS), over 30 in body mass index (BMI) (≥30 kg/m2),[11] over 30% of body fat percentage (≥30%), over 0.85 cm in waist hip ratio (≥0.85 cm), able to stand on one leg for 30 seconds, and who are positive in more than 3 items among the 5 item lumbar instability test.[12] The exclusion criteria were persons with low back pain due to compression fracture, who have systemic disease such as cancer, who have neural symptoms, and who have participation rate of less than 80%. All participants have fully understood the purpose and content of the study, and the participants have voluntarily participated after signing the written consent.
2.2. Study design
The design of this study was a double-blinded randomized-controlled clinical trial conducted. G-power version was used to set the number of participants.[13] Based on the pilot study result that the size of the main effect was (d): 0.91, significance level was set to α = 0.05 and power (1−β) = 0.8, thereby requiring at least 20 participants for each group. However, 15% of drop-out rate was considered, therefore minimum participants for each group were set to 23.
The recruited participants were screened for lumbar instability. Lumbar instability test consisted of lumbar instability in prone (positive if there is pain after manually pressure is applied anteriorly and posteriorly and pain is relieved after both lower extremities are extended), anterior and posterior test of lumbar segments (positive when spinous processes are pressured, and there is excessive movement or moves to abnormal direction), straight leg raising test (positive when mean angle of both hip joints exceed 90°), lumbar manual extension test (positive when there is pain with both legs raised in prone position and the pain is relieved when the legs are lowered), and age (below 40 is positive). If there are 3 or more items that resulted positive, the participant was categorized as participant with lumbar instability.[12] Through the screening test, 25 participants who had BMI below 29 (n = 16) and who did not satisfy the inclusion criteria (n = 9) were excluded from the study.
To compare the effects before and after the interventions, assessments were made before the intervention, and all 46 participants were assigned to experimental group (n = 23) and control group (n = 23) using the random number production program under the supervision of the lead researcher.[14] Both groups were measured for QVAS, Korean-Oswestry disability index (K-ODI), fear-avoidance beliefs questionnaire (FABQ), balance ability, muscle thickness, and contraction rate (Fig. 1). All participants performed the exercise program to be blinded to their own group. All data after the intervention were analyzed. All assessments were made with 3 skilled researchers excluding the lead researcher. This study is approved by the bioethical committee of Daejeon University and is registered in the WHO International Clinical Trials Registry Platform: KCT0004512.
Figure 1.
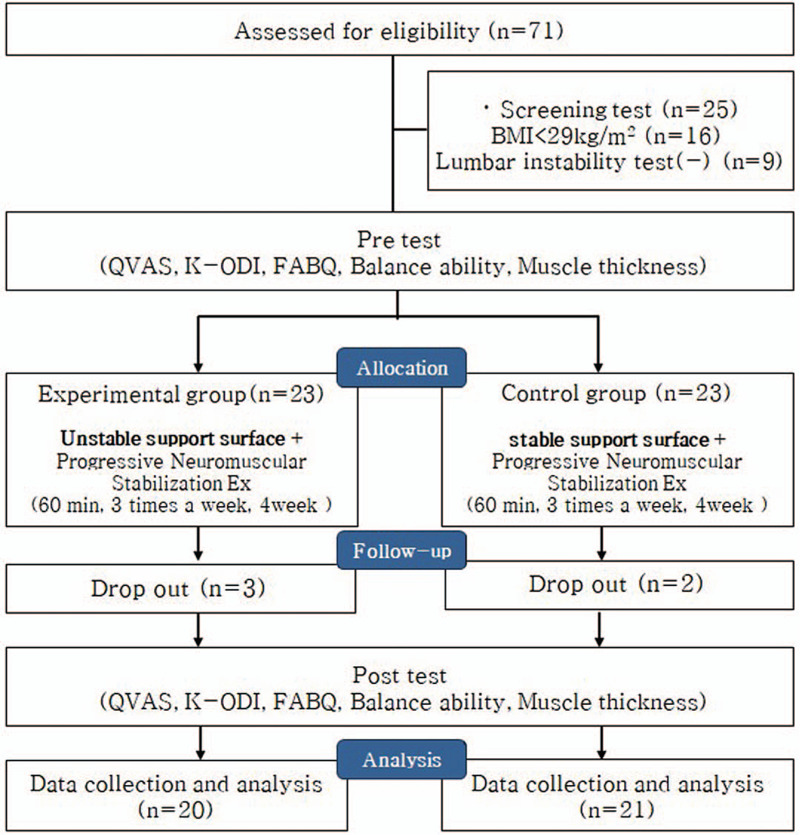
CONSORT flow chart.
2.3. Intervention
Progressive neuromuscular stabilization exercise program provided to both groups was modified from the original method suggested by Saliba et al.[15] Considering the pain and motor function levels of the participants, exercise routines were graded each week from easier levels to more difficult. Progressive neuromuscular exercise program that supports anterior, posterior, and lateral sides of the trunk muscles consisted curl up, dead bug, bird dog, flank, and side flank with knee flexion. All participants ran on the treadmill for 5 minutes each for warm-up and cool-down. Each exercise for every week was performed for 10 seconds each repetition, 10 repetitions per set, and 5 sets total. 20 seconds of rest were given between each set. Each session lasted approximately 55 minutes, and it was given 3 times a week for 4 weeks. When the participant was able to perform 80% of the exercise successfully, that participant was able to move on to the next level.
The control group received progressive neuromuscular stabilization exercise program on stable surface, and the experimental group received progressive neuromuscular stabilization exercise program on the unstable support surface to activate the deep muscles for trunk stabilization (Fig. 2).
Figure 2.

Progressive neuromuscular stabilization exercise on the unstable support.
2.4. Assessment tools
In order to assess pain of the participants depending on the intervention methods, 4 items QVAS was used to measure pain before and after the intervention. This test has 4 items and each item has subitems that measure current pain level, average pain level, pain level when it is at the mildest level, and pain level when it is most severe. Every item is scored from 0 to 10 where 0 is no pain at all and 10 when it is at the worst level. The scores of the items are summed and mean was calculated. Reliability was high resulting in r = 0.76–0.84.[16]
In order to quantify physical dysfunction due to low back pain in everyday life, K-ODI was used. Total score was calculated for percentage. Test–retest reliability of K-ODI was (r = 0.92).[17]
Correlation between low back pain and dysfunction was found using FABQ, a self reporting tool. This questionnaire has 5 items related to physical activities (FABQ-PA) and 11 items related to work (FABQ-W). The participants score on a 7-point scale (0 = totally disagree, 6 = totally agree). The score ranges from 0 to 66 where higher score means greater avoidance. Questionnaire suggested by Joo and Kim[17] was used and the reliability of this test is (r = 0.95).
Wii balance board (WBB) (Nintendo, Kyoto, Japan) was used to measure balance ability of the groups with different intervention methods. Participants stand on the platform of Wii balance and center of pressure (CoP) sway was traced to calculate velocity, path length, and area 95%. The participants stand on WBB, and with the instruction from the therapist, they performed one leg standing on their dominant side for measurements. The measurement started when the participant found the stable position, and it was measured for 30 seconds. The measurements for 3 trials were recorded and the mean data was used for analysis. Measurement reliability of WBB was ICC = 0.92–0.98[18] and balancia program has intrarater reliability of (r = 0.79–0.96) and validity of (r = 0.85–0.96), making it useful assessment tools.[19]
For measuring TrA thickness of the participants, Mysono U6 (Samsung, Suwon, Korea) was used to make the measurement at the end of expiration. In order to find the thickness of TrA thickness, the most appropriate location for 3.5 MHz convex transducer was at 2.5 cm laterally after drawing a parallel line from the navel (Fig. 3).[20] The measurement was made in each relaxed and contracted position, and with the relaxed position as a reference, contracted TrA thickness was converted to contraction rate = (thickness in contraction − thickness in relaxation/thickness in relaxation) × 100. This assessment has a high test–retest reliability (ICC = 1.00–1.00), and intrarater reliability is also high (ICC = 0.91–0.96).[21]
Figure 3.
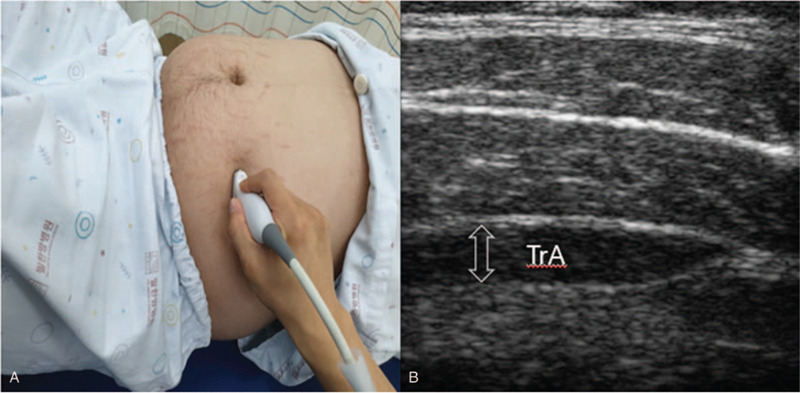
Muscle thickness measurement (A) and TrA ultrasound (B).
2.5. Analysis
SPSS version 25.0 (IBM, Chicago, IL) was used for data analysis. General characteristics of the participants were provided using mean and standard deviation values through descriptive statistics. Shapiro–Wilk test was used for normality testing. Normal distribution of all variables from the results was identified. General characteristics between groups and homogeneity test of preintervention values were analyzed through χ2 test and t test. The independent t test and χ2 test were used to compare the intervention results between the groups, and the paired t test was used to compare the dependent variables within the groups. Repeated measure analysis of variance was used to identify the change following time and the effects of interactions between time and group. Statistical significance was set to P < .05.
3. Results
Due to deconditioning and aggravated pain, 3 participants in the experimental group and 2 participants from the control group were excluded, where 20 data from the experimental group and 21 data from the control group were collected. General characteristics of both groups before the intervention were all homogeneous (Table 1).
Table 1.
General characteristics.
| Experimental group (n = 20) | Control group (n = 21) | t/χ2 | P | |
| Sex (male/female) | 13/7 | 13/8 | 0.107 | .744 |
| Age (year) | 36.55 ± 7.32∗ | 36.40 ± 7.74 | 0.063 | .950 |
| Height (cm) | 169.10 ± 10.35 | 169.25 ± 8.62 | −0.050 | .961 |
| Weight (kg) | 87.66 ± 10.88 | 87.88 ± 10.01 | −0.063 | .950 |
| Onset (month) | 7.45 ± 5.10 | 6.70 ± 4.96 | 0.471 | .640 |
Mean ± standard deviation.
BMI, QVAS, K-ODI, and FABQ before and after the intervention are shown in Table 2. Both groups showed no significant difference in all dependent variables in the measurements before the intervention. However, there was a significant difference in both groups after the intervention (P < .05). Differences between the groups showed significant difference (P < .05) in the experimental group for QVAS and K-ODI. All dependent variables showed change depending on the measurement time (P < .05) and only in QVAS there was interaction of time × group for measurement times (P < .05).
Table 2.
Comparison of dependent variables according to the intervention between groups.
| Experimental group (n = 20) | Control group (n = 21) | t (p) | Time F (p) | Time×group F (p) | ||
| BMI (score) | Pre | 30.55 ± 0.87∗ | 30.60 ± 1.58 | −0.125 (0.901) | 12.766 (0.001) | 0.001 (0.978) |
| Post | 29.93 ± 0.84 | 29.97 ± 1.29 | ||||
| Post–pre | −0.62 ± 1.02 | −0.63 ± 1.18 | −0.026 (0.979) | |||
| t (p) | −2.711 (0.014) | −2.380 (0.028) | ||||
| QVAS (cm) | Pre | 6.59 ± 0.50 | 6.48 ± .51 | 0.702 (0.487) | 420.731 (0.000) | 14.563 (0.000) |
| Post | 4.68 ± 0.49 | 5.16 ± 0.45 | ||||
| Post–pre | −1.91 ± 0.36 | −1.31 ± 0.61 | 5.022 (0.000) | |||
| t (p) | −24.018 (0.000) | −9.681 (0.000) | ||||
| K-ODI (score) | Pre | 16.90 ± 6.26 | 15.85 ± 3.90 | 0.637 (0.529) | 138.195 (0.000) | 3.874 (0.056) |
| Post | 10.45 ± 5.13 | 11.25 ± 3.04 | ||||
| Post–pre | −6.45 ± 3.28 | −4.60 ± 2.62 | 2.959 (0.008) | |||
| t (p) | −8.783 (0.000) | −7.841 (0.000) | ||||
| FABQ-PA (score) | Pre | 21.65 ± 2.78 | 21.90 ± 2.38 | −0.306 (0.762) | 63.420 (0.000) | 0.052 (0.821) |
| Post | 17.15 ± 2.62 | 17.65 ± 3.79 | ||||
| Post–pre | −4.50 ± 2.89 | −4.25 ± 3.97 | 0.201 (0.843) | |||
| t (p) | −6.957 (0.000) | −4.785 (0.000) | ||||
| FABQ-W (score) | Pre | 38.00 ± 4.28 | 38.70 ± 3.25 | −0.583 (0.563) | 163.454 (0.000) | 1.008 (0.322) |
| Post | 24.95 ± 4.68 | 27.55 ± 5.63 | ||||
| Post–pre | −13.05 ± 5.56 | −11.15 ± 6.38 | 1.075 (0.296) | |||
| t (p) | −10.500 (0.000) | −7.810 (0.000) | ||||
| FABQ-total (score) | Pre | 59.60 ± 6.20 | 60.60 ± 4.76 | −0.572 (0.571) | 171.329 (0.000) | 3.542 (0.067) |
| Post | 42.10 ± 5.00 | 47.50 ± 8.96 | ||||
| Post–pre | −17.50 ± 6.46 | −13.10 ± 8.22 | 1.789 (0.090) | |||
| t (p) | −12.114 (0.000) | −7.127 (0.000) |
Mean ± standard deviation, BMI = body mass index, FABQ = fear-avoidance beliefs questionnaire, K-ODI = Oswestry disability index-Korean, PA = physical activity, QVAS = quadruple visual analogue scale, W = work.
Balance abilities, muscle thickness, and contraction rate before and after the intervention are shown in Table 3. Both groups showed no significant difference for all dependent variables in the assessment before the intervention. However both groups showed significant difference (P < .05) in balance abilities after the intervention. In addition, only the experimental group showed significant difference (P < .05) in muscle thickness in contraction and contraction rate before and after the intervention. When the 2 groups were compared, the experimental group showed significant difference (P < .05) in balance abilities, muscle thickness in contraction, and contraction rate. Time by different measurement times has changed (P < .05) and interaction of time×group for measurement times (P < .05) was shown for balance abilities, muscle thickness in contraction, and contraction rate.
Table 3.
Comparison of dependent variables according to the intervention between groups.
| Experimental group (n = 20) | Control group (n = 21) | t (p) | Time F (p) | Time×group F (p) | ||
| CoP velocity (cm/s) | Pre | 4.59 ± 0.66∗ | 4.57 ± 0.71 | 0.127 (0.900) | 57.769 (0.000) | 7.742 (0.008) |
| Post | 3.68 ± 0.66 | 4.14 ± 0.78 | ||||
| Post–pre | −0.91 ± .66 | −0.42 ± 0.43 | 3.271 (0.004) | |||
| t (p) | −6.191 (0.000) | −4.422 (0.000) | ||||
| CoP length (cm) | Pre | 137.90 ± 19.71 | 139.61 ± 15.69 | −0.303 (0.763) | 37.977 (0.000) | 5.088 (0.030) |
| Post | 114.91 ± 22.40 | 128.94 ± 19.63 | ||||
| Post-pre | −22.99 ± 21.02 | −10.67 ± 12.45 | 2.772 (0.012) | |||
| t (p) | −4.892 (0.000) | −3.834 (0.001) | ||||
| CoP area (cm2) | Pre | 9.11 ± 3.37 | 8.50 ± 2.78 | 0.626 (0.535) | 23.993 (0.000) | 6.026 (0.019) |
| Post | 5.99 ± 2.51 | 7.46 ± 2.41 | ||||
| Post–pre | −3.11 ± 3.11 | −1.03 ± 2.15 | 2.225 (0.038) | |||
| t (p) | −4.466 (0.000) | −2.152 (0.044) | ||||
| Muscle thickness in contraction (mm) | Pre | 0.39 ± 0.05 | 0.38 ± 0.06 | 0.258 (0.798) | 3.691 (0.062) | 11.618 (0.002) |
| Post | 0.41 ± 0.05 | 0.38 ± 0.05 | ||||
| Post–pre | 0.02 ± 0.03 | −0.00 ± 0.02 | −3.568 (0.002) | |||
| t (p) | 3.287 (0.004) | −1.270 (0.219) | ||||
| Muscle thickness in resting (mm) | Pre | 0.27 ± 0.035 | 0.27 ± 0.06 | 0.197 (0.845) | 0.343 (0.562) | 0.007 (0.934) |
| Post | 0.27 ± 0.04 | 0.27 ± 0.05 | ||||
| Post–pre | 0.00 ± 0.01 | 0.00 ± 0.02 | −0.111 (0.913) | |||
| t (p) | 0.607 (0.551) | 0.301 (0.767) | ||||
| Contraction rate (%) | Pre | 1.45 ± 0.21 | 1.46 ± 0.21 | −0.246 (0.807) | 1.035 (0.315) | 4.942 (0.032) |
| Post | 1.53 ± 0.26 | 1.43 ± 0.24 | ||||
| Post–pre | 0.08 ± 0.12 | −0.02 ± 0.16 | −2.230 (0.039) | |||
| t (p) | 2.856 (0.010) | −0.732 (0.473) |
CoP = center of pressure.
Mean ± standard deviation.
4. Discussion
This study compared progressive neuromuscular stabilization exercise programs on different surfaces with highly obese patients with lumbar instability. The results showed that the experimental group who received progressive neuromuscular stabilization exercise on unstable surface showed decreased pain, increased motor function, and balance (P < .05).
Highly obese low back pain patients have the tendency to maintain the CoP by excessively increasing the lodosis due to abdominal expansion. Additionally, lumbar lordosis due to obesity applies much pressure to body joints; therefore, it increases the risk of musculoskeletal diseases. Greve et al[22] reported that mechanical structural changes due to obesity induce musculoskeletal diseases such as degenerative arthritis, and weight loss of obese low back pain patients decreases pain and enhances quality of life.
Mirtz and Greene[23] reported that the risk for low back pain increases when BMI is over 30 kg/m2, and Shiri et al[24] reported that abdominal obesity applies abnormal pressure to the spine, thereby increasing low back pain. This suggests that obesity is highly correlated to low back pain, and this study also showed BMI changes before and after the interventions in both groups (P < .05). Regular physical activities affected endurance and BMI of highly obese patients, and it may also decrease obesity. Although there was no difference between the 2 groups, there was a difference in the effect size between the experimental group who received exercise program on unstable surface (SMD = .73, 95% CI = 0.09–1.36) and the control group who receive the exercise on a stable surface (SMD = 0.44, 95% CI = −0.18–1.05). The unstable surface in the exercise program for highly obese patients contributed to the BMI by deep muscle contraction, which maintains trunk posture. Therefore weight loss needs to be achieved before any interventions to highly obese patients with low back pain.
Progressive neuromuscular stabilization exercise on low back pain patients is proven to be an effective intervention method through many studies. Park and Lee[25] administered progressive stabilization exercise program with respiratory resistance for 4 weeks to chronic low back pain patients, and showed significant difference in pain level (P < .05, SMD = 2.74, 95% CI = 1.88–3.60). The results of this study showed decreased pain levels for both groups and it supports the results of prior studies (P < .05). QVAS was used to measure pain where the experimental group showed a change of mean 6.59 to 4.66 (P < .05, SMD = 3.86, 95% CI = 2.81–4.91) and the control group showed a change of mean 6.47 to 5.16 (P < .05, SMD = 2.74, 95% CI = 1.88–3.61). This proves that pain level has significantly decreased in both groups (P < .05).
Progressive neuromuscular stabilization exercise not only decreases pain, but it contributes to improvement of motor function in physical activities. Roffey et al[26] reported that weight loss of obese patients improved lumbar pain and dysfunction. This study also used K-ODI to measure the sensitivity of spinal diseases in general state, and to determine the level of lumbar dysfunction. Considering Korean culture, percentage was found for 45 points excluding the item for sexual activities. The experimental group showed a change from 37.56% to 23.22% and the control group from 35.22% to 25%, illustrating the decrease of dysfunction level.
Fear-avoidance response during injury or disease affects normal sensation for balance and may lead to sever dysfunction.[27] The result of FABQ for both groups showed decreased psychological anxiety (P < .05) for physical activities and occupational performance before and after the intervention, but there was no difference between the groups. This may be due to having all the participants performing exercise programs, and they were not knowledgeable to which group they were assigned. In addition, the differences in the effects of FABQ-PA of the experimental group (SMD = 1.67, 95% CI = 0.95–2.39), control group (SMD = 1.34, 95% CI = 0.67–2.01), FABQ-W of the experimental group (SMD = 2.91, 95% CI = 2.02–3.79), and the control group (SMD = 2.43, 95% CI = 1.63–3.22) showed a more significant result.
Ogon et al[28] suggested that stability required in low back pain patients is more than maintaining balance in a static position, but rather it is a stability in continuous dynamic state. In order to assess motor performance abilities, variables regarding velocity, distance, and area of CoP were measured and compared and all variables showed significant increases (P < .05). Additionally, the experimental group showed a more significant difference (P < .05) than the control group. This may imply that exercise on unstable surface increased co-contraction of the deep core muscles, which stabilizes the trunk, and contributed to trunk stabilization. Thereby the index for balance ability was enhanced.
Nabavi et al[29] reported that ultrasonography not only selectively measures deep muscles noninvasively, but also allows observation of changes of activation order during muscle contraction. Akuthota and Nadler[30] demonstrated that chronic low back pain patients have instability due to weak trunk muscles, which act as lumbar stabilizers. If lumbar instability is existent, TrA and multifidis muscles cocontract to support the spine and produce trunk stability. Because TrA is the deepest muscle in the abdominals, it controls each vertebral segment and increases stability.
In this study, only the experimental group who performed exercise program on unstable surface showed significant difference (P < .05) in muscle thickness and contraction rate of TrA contraction. The exercise effect was maximized by distributing the internal forces of the muscles that act on the spine and each spinal joint to maintain balance on unstable surfaces. In addition, cocontraction of TrA and deep muscles for trunk stabilization may be suggested as an index for decreased low back pain and improved motor function and balance ability. Consequently, this study is methodologically meaningful since TrA thickness was measured using the ultrasound after lumbar neuromuscular stabilization exercise on low back pain patients.
This study has limitations. First of all, the age range of the participants was limited, thereby the results of this study are hard to generalize to low back pain patients of all ages. Secondly, obese patients with the body mass index mean of 31 participated in the exercise program, and this raises uncertainty whether super obese patients are able to follow the intervention. Thirdly, there may be some error range due to fat thickness during ultrasonic measurement. In order to supplement this issue, physical therapist with 6 years of ultrasonic measurement experience made the measurement alone to minimize the error. In future studies, modifications to progressive stabilization exercise program on different surfaces and the effects may be needed for discussion with these limitations in consideration of these limitations.
5. Conclusion
This study investigates the effects of progressive neuromuscular stabilization exercise program on unstable surface for highly obese low back pain patients. The exercise resulted statistically significant changes in decreased pain level, increased motor function and balance, transverse abdominis muscle thickness in contraction and contraction rate. Based on these results progressive neuromuscular stabilization exercise on unstable surface for highly obese low back pain patients has positive effects on deep stabilization muscles and is helpful in maintaining postural stability.
Author contributions
Conceptualization: Sam-Ho Park.
Data curation: Sam-Ho Park.
Formal analysis: Sam-Ho Park.
Methodology: Sam-Ho Park, Myung-Mo Lee.
Supervision: Myung-Mo Lee.
Visualization: Sam-Ho Park, Myung-Mo Lee.
Writing – original draft: Sam-Ho Park.
Writing – review & editing: Myung-Mo Lee.
Glossary
Abbreviations: BMI = body mass index, CoP = center of pressure, FABQ = fear-avoidance beliefs questionnaire, FABQ-PA = fear-avoidance beliefs questionnaire physical activities, FABQ-W = fear-avoidance beliefs questionnaire work, K-ODI = Korean-Oswestry disability index, QVAS = quadruple visual analogue scale, TrA = transversus abdominis, WBB = Wii balance board.
References
- [1].Shiri R, Falah-Hassani K, Heliövaara M, et al. Risk factors for low back pain: a population-based longitudinal study. Arthritis Care Res 2019;71:290–9. [DOI] [PubMed] [Google Scholar]
- [2].O'Sullivan PB, Burnett A, Floyd AN, et al. Lumbar repositioning deficit in a specific low back pain population. Spine (Phila Pa 1976) 2003;28:1074–9. [DOI] [PubMed] [Google Scholar]
- [3].Slade SC, Keating JL. Trunk-strengthening exercises for chronic low back pain: a systematic review. J Manipulative Physiol Ther 2006;29:163–73. [DOI] [PubMed] [Google Scholar]
- [4].Caban AJ, Lee DJ, Fleming LE, et al. Obesity in US workers: the national health interview survey, 1986 to 2002. Am J Public Health 2005;95:1614–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Shiri R, Karppinen J, Leino-Arjas P, et al. The association between obesity and low back pain: a meta-analysis. Am J Epidemiol 2010;171:135–54. [DOI] [PubMed] [Google Scholar]
- [6].Ma J, King AC, Wilson SR, et al. Evaluation of lifestyle interventions to treat elevated cardiometabolic risk in primary care (E-LITE): a randomized controlled trial. BMC Fam Pract 2009;10:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Melissas J, Kontakis G, Volakakis E, et al. The effect of surgical weight reduction on functional status in morbidly obese patients with low back pain. Obes Surg 2005;15:378–81. [DOI] [PubMed] [Google Scholar]
- [8].Verhagen E, Van der Beek A, Twisk J, et al. The effect of a proprioceptive balance board training program for the prevention of ankle sprains: a prospective controlled trial. Am J Sports Med 2004;32:1385–93. [DOI] [PubMed] [Google Scholar]
- [9].Bilodeau M, Schindler-Ivens S, Williams D, et al. EMG frequency content changes with increasing force and during fatigue in the quadriceps femoris muscle of men and women. J Electromyogr Kinesiol 2003;13:83–92. [DOI] [PubMed] [Google Scholar]
- [10].Lee HS, Kim DJ, Oh Y, et al. The effect of individualized gradable stabilization exercises in patients with chronic low back pain: case-control study. J Back Musculoskelet Rehabil 2016;29:603–10. [DOI] [PubMed] [Google Scholar]
- [11].Koyanagi A, Stickley A, Garin N, et al. The association between obesity and back pain in nine countries: a cross-sectional study. BMC Public Health 2015;15:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Hicks GE, Fritz JM, Delitto A, et al. Interrater reliability of clinical examination measures for identification of lumbar segmental instability. Arch Phys Med Rehabil 2003;84:1858–64. [DOI] [PubMed] [Google Scholar]
- [13].Faul F, Erdfelder E, Lang A-G, et al. G∗ Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Res Methods 2007;39:175–91. [DOI] [PubMed] [Google Scholar]
- [14].Saghaei M. Random allocation software for parallel group randomized trials. BMC Med Res Methodol 2004;4:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Saliba SA, Croy T, Guthrie R, et al. Differences in transverse abdominis activation with stable and unstable bridging exercises in individuals with low back pain. N Am J Sports Phys Ther 2010;5:63–73. [PMC free article] [PubMed] [Google Scholar]
- [16].Boonstra M, Malefijt MDW, Verdonschot N. How to quantify knee function after total knee arthroplasty? Knee 2008;15:390–5. [DOI] [PubMed] [Google Scholar]
- [17].Joo M-K, Kim T-Y, Kim J-T, et al. Reliability and validity of the Korean version of the fear-avoidance beliefs questionnaire. Physical Therapy Korea 2009;16:24–30. [Google Scholar]
- [18].Holmes JD, Jenkins ME, Johnson AM, et al. Validity of the Nintendo Wii balance board for the assessment of standing balance in Parkinson's disease. Clin Rehabil 2013;27:361–6. [DOI] [PubMed] [Google Scholar]
- [19].Park D-S, Lee D-Y, Choi S-J, et al. Reliability and validity of the balancia using Wii balance board for assessment of balance with stroke patients. J Korea Academia-Industrial Cooperation Society 2013;14:2767–72. [Google Scholar]
- [20].Mannion AF, Pulkovski N, Gubler D, et al. Muscle thickness changes during abdominal hollowing: an assessment of between-day measurement error in controls and patients with chronic low back pain. Eur Spine J 2008;17:494–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Teyhen DS, Miltenberger CE, Deiters HM, et al. The use of ultrasound imaging of the abdominal drawing-in maneuver in subjects with low back pain. J Orthop Sports Phys Ther 2005;35:346–55. [DOI] [PubMed] [Google Scholar]
- [22].Greve J, Alonso A, Bordini ACP, et al. Correlation between body mass index and postural balance. Clinics (Sao Paulo) 2007;62:717–20. [DOI] [PubMed] [Google Scholar]
- [23].Mirtz TA, Greene L. Is obesity a risk factor for low back pain? An example of using the evidence to answer a clinical question. Chiropr Osteopat 2005;13:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Shiri R, Solovieva S, Husgafvel-Pursiainen K, et al. The association between obesity and the prevalence of low back pain in young adults: the Cardiovascular Risk in Young Finns Study. Am J Epidemiol 2008;167:1110–9. [DOI] [PubMed] [Google Scholar]
- [25].Park S-H, Lee M-M. Effects of a progressive stabilization exercise program using respiratory resistance for patients with lumbar instability: a randomized controlled trial. Med Sci Monit 2019;25:1740–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Roffey DM, Ashdown LC, Dornan HD, et al. Pilot evaluation of a multidisciplinary, medically supervised, nonsurgical weight loss program on the severity of low back pain in obese adults. Spine J 2011;11:197–204. [DOI] [PubMed] [Google Scholar]
- [27].Staerkle R, Mannion AF, Elfering A, et al. Longitudinal validation of the fear-avoidance beliefs questionnaire (FABQ) in a Swiss-German sample of low back pain patients. Eur Spine J 2004;13:332–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Ogon M, Bender BR, Hooper DM, et al. A dynamic approach to spinal instability: Part I: sensitization of intersegmental motion profiles to motion direction and load condition by instability. Spine (Phila Pa 1976) 1997;22:2841–58. [DOI] [PubMed] [Google Scholar]
- [29].Nabavi N, Mosallanezhad Z, Haghighatkhah HR, et al. Reliability of rehabilitative ultrasonography to measure transverse abdominis and multifidus muscle dimensions. Iran J Radiol 2014;11:e21008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Akuthota V, Nadler SF. Core strengthening. Arch Phys Med Rehabil 2004;85:86–92. [DOI] [PubMed] [Google Scholar]


