Abstract
Background:
Patients with rectal cancer treated at specialized or high-volume hospitals have better outcomes, but a minority of these patients are treated there. Physician recommendations are important considerations for rectal cancer patients when making treatment decisions, yet little is known about the factors that affect these physician referral patterns.
Methods:
Semi-structured telephone interviews were conducted in 2018–2019 with Iowa gastroenterologists (GI) and general surgeons (GS) who performed colonoscopies in a community setting. A thematic approach was used to analyze and code qualitative data.
Results:
We interviewed 10 GIs and 6 GSs with self-reported averages of 15.5 years in practice, 1100 endoscopic procedures annually, and 6 rectal cancer diagnoses annually. Physicians believed surgeon experience and colorectal specialization were directly related to positive outcomes in rectal cancer resections. Most GSs performed resections on patients they diagnosed and typically only referred patients to colorectal surgeons (CRS) in complex cases. Conversely, GIs generally referred to CRS in all cases. Adhering to existing referral patterns due to the pressure of healthcare networks was a salient theme for both GIs and GSs.
Conclusions:
While respondents believe that high volume/specialization is related to improved surgical outcomes, referral recommendations are heavily influenced by existing referral networks. Referral practices also differ by diagnosing specialty and suggest rural patients may be less likely to be referred to a CRS since more GSs perform colonoscopies in rural areas and tend to keep patients for resection. System-level interventions that target referral networks may improve rectal cancer outcomes at the population level.
Keywords: rectal cancer, physician interview, referral patterns, qualitative research
Introduction
Rectal cancer is a relatively rare cancer, representing 2.4% of all estimated new cancer cases in the United States in 2020 (ACS Cancer Facts and Figures 2020). Staging and treatment of rectal cancer are complex and involve multimodal imaging and a multidisciplinary approach to include chemotherapy, radiation, and surgery. Post-operative morbidity (e.g. fecal incontinence, genitourinary dysfunction) of rectal cancer is higher compared to colon cancer due to increased anatomical challenges.1–3
Given the relative rarity of rectal cancer and the complexity of treatment regimens, studies have investigated whether there is a relationship between surgeon or hospital volume/specialization and optimal outcomes. Many of these studies have found that rectal cancer patients treated by high-volume, specialized surgeons or hospitals received higher rates of guideline recommended care4–6 and sphincter preservation7,8, decreased rates of postoperative mortality, morbidity and local recurrence9–13, and greater overall survival14–17 than patients treated by lower-volume surgeons/hospitals.
Research indicates that only 26% of patients with rectal cancer are treated at high or very high-volume hospitals18 and even fewer (4–10%) 4,19 are treated at National Cancer Institute Designated Cancer Centers. While centralization of other cancers requiring complex surgery, such as esophageal and pancreatic cancer, has increased over the years, there has been only modest, if any, increases in the amount of rectal cancer surgeries performed at high-volume centers.5,20 Efforts to improve rectal cancer care, including centralization, should take into account the drivers of decision making in patients and providers. A recent qualitative study found that rectal cancer patients relied heavily on the recommendations of their physicians when choosing a surgeon.21 Specifically, patients who chose low-volume hospitals did not have anyone advocate that they go to a high-volume hospital. On the provider side, little is known about physician attitudes and perspectives on rectal cancer management and referral. Given the influential role that providers play in patient decision making, we aimed to investigate the factors that guide provider management and referral of patients with rectal cancer.
Methods
Subject selection
Gastroenterologists (GIs) and general surgeons (GSs) from community practices who performed colonoscopies on patients residing in Iowa were eligible for the study. During the initial phase of the study, clinic addresses and phone numbers of GIs who met the study criteria were obtained from the Iowa Health Professions Inventory. GIs were categorized based on practice types (allopathic teaching/research, private practice, public/community health) and practice arrangements (independent practice, physician network, integrated health system) and stratified random sampling by practice type, arrangement, and rurality was used to create an initial recruitment sample of 22 GIs. Letters describing the study with an invitation to participate were mailed to the clinic addresses of the recruitment sample. One week after mailing the invitation letter, a member of the study team called the clinic of each GI to determine whether the provider would be interested in participating. A maximum of four phone calls were attempted and if interested, a time was set up for the interview. During this recruitment process, we were unable to speak to the vast majority of GIs, being directed instead by clinic managers and nurses to leave phone messages. Through this method, we were ultimately only able to recruit 2 GIs. Due to the low response rate, we amended our protocol and subsequently conducted purposive and snowball sampling through networking with providers at the authors’ institution. All potential subjects were mailed a letter describing the study and subsequently contacted via email, phone call, or text, and were asked whether they would agree to be interviewed for the study by phone. For those who agreed, verbal informed consent was obtained, and an interview was conducted immediately or scheduled for a time at the subject’s convenience. Efforts were made to include providers from different practice types, geographical areas, and both rural and urban communities.
Data collected
The interview guide for GIs was first drafted to address elements central to our study aim, including: specific considerations in referral decision making, perceived patient preferences in surgical referrals, and attitudes on the importance of surgeon experience and training. Questions regarding patient preferences were formulated based on results from research of patient perspectives on rectal cancer treatment. Pilot testing with GIs in a neighboring state was conducted to refine the questions. This interview guide was modified for GSs to ask questions specific to the surgical treatment of rectal cancer and was subsequently also pilot tested with a local surgeon and refined.
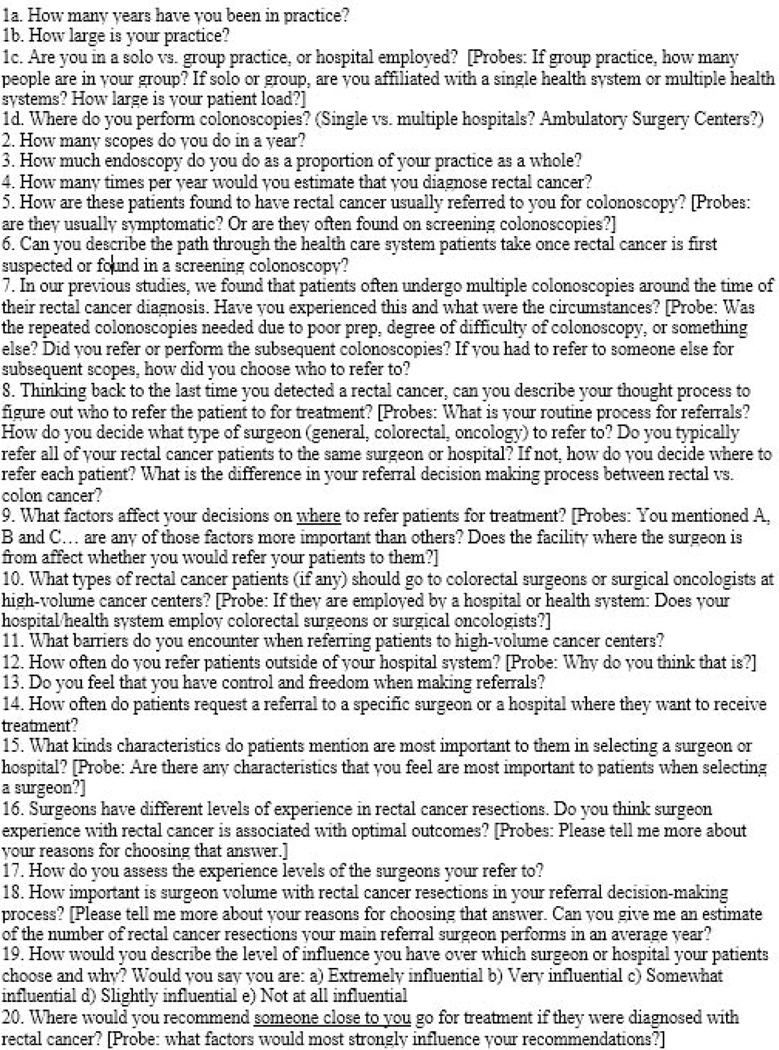
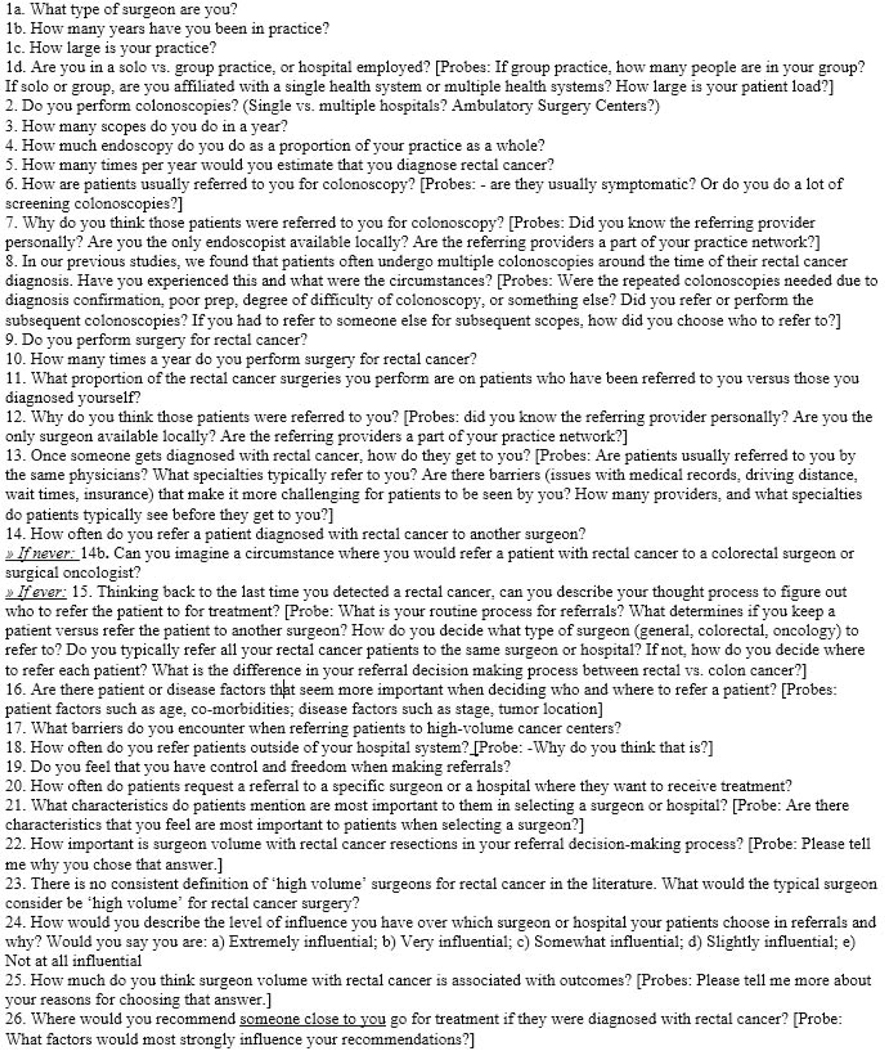
Both interview guides included open-ended questions (19 for GIs, 22 for GSs) with probes for clarification and one closed-ended question. Interview topics included: practice characteristics, referral decision making process, patient preferences in referrals, and attitudes and perspectives on the importance of surgeon experience and training. The GS interview guide included additional questions regarding surgical referral and practice patterns. The interview guides are provided in Figure 1 and Figure 2. All interviews were conducted by one of two team members. Participants were assured that their answers would be confidential. On average, interviews lasted 24 minutes and they were transcribed verbatim. Subjects were provided $50 in compensation for participation. Saturation was reached when no new themes emerged from the data. This study was approved by the University of Iowa Institutional Review Board.
Figure 1.
Gastroenterologist interview guide
Figure 2.
General surgeon interview guide
Data analysis
A thematic approach was used to provide insight into respondents’ thought processes and meanings.22 Initial codes were generated inductively using multiple coding to compare and distinguish sections of text into specific categories.23 Multiple coding involves each team member bringing observations and descriptions about the data to team meetings to discuss experiences with the analytic process and describe their codes in detail. Discussions involved the similarities, differences, and patterns within and between codes. Overall, discussions revealed high levels of agreement across team members. In instances of differing opinions on how themes and ideas should be grouped together, members were able to reach a consensus through collective reflection and meshing of interpretations until a list and description of codes were developed that all agreed were reflective of the data. Through this process, codes were adapted, redefined, incorporated, or dropped until team members agreed they reached a list of codes that most reflected shared interpretations of participant experiences. The dataset was first analyzed as a whole to capture themes across all physicians. Then, the dataset was split into two groups as a function of specialty (GI versus GS) and analysis was undertaken to identify where themes were comparable or contrasting across groups. Demographic and closed-ended responses were described and summarized.
Results
Study population
Among the 22 initial GIs who were mailed study invitations and called at their clinics, 2 participated in the study. Subsequently, among 12 GIs and 9 GSs identified through purposive and snowball sampling, we interviewed 10 GIs and 6 GSs with self-reported averages of 15.5 years in practice (range 1–41 years), 1100 endoscopic procedures performed per year (range 450–2000), and 6 rectal cancer diagnoses per year (range 1–12). Two respondents identified as female and the remaining 14 identified as male. GSs performed an average of 9 rectal cancer resections per year (range 2–20). Among all respondents, 4 were locum tenens, 6 worked at private multi-disciplinary practices, 4 worked at private single specialty practices, and 2 were hospital employed. One GI and 5 GSs practiced in a nonmetropolitan county (population 2,500–20,000, Rural-urban Continuum Codes 4–9). The remaining respondents practiced in a metropolitan county (population 50,000–1,000,000, Rural-urban Continuum Codes 1–3)
Presentation for colonoscopy
Both GIs and GSs reported primary care providers as the major referral source for patients undergoing colonoscopy. Other sources included the emergency department, in-patient consults, and patient self-referral. Some respondents noted that the referring providers are frequently from within their health system.
“Nearly everyone I get referred comes from our health group.” -GS
Patients later identified as rectal cancer patients had typically presented with symptoms such as rectal bleeding.
“Usually have rectal bleeding, majority of them… occasionally they just come for a screening colonoscopy.” -GI
“It’s very hard to find a rectal cancer in those patients [who are asymptomatic] in my practice. Almost unheard of actually.” -GS
Being the only provider in the area or being well known in the community were salient themes when GSs were asked why they were the provider who was referred to for colonoscopy.
“My partner and I are the only ones that do them in…a three- or four-county area.” -GS
“…I was born and raised in the area, so [the primary care providers] all know me.” -GS
“I’ve been here for nine years, so established relationships with patients too. So, they say, ‘Oh.
Go -- send my cousin to see you as well…’ and that sort of thing.” -GS
GSs also noted that they may be preferred for referrals over GIs specifically when patients have rectal or potentially surgical complaints.
“As general surgeons, you know, we manage the anorectal complaints. And the gastroenterologists … I don’t think feel comfortable with, and… don’t want to deal with anorectal complaints.” -GS
“It’s easier for them to refer to us, and then we’re available…. because we do the surgery, a lot of people here tend to prefer surgeons over a GI doctor, honestly.” -GS
GSs reported that the majority of their surgical cases were diagnosed by themselves which may be due to the limited number of local endoscopists. GSs also stated that they were frequently consulted for rectal cancer because they are well established in the community or known to take care of a wide range of diseases.
“There aren’t any gastroenterologists that practice -- that treat -- in our local market, so there’s not really anybody else that would be diagnosing it to refer to me. I’m diagnosing it, and then I’m treating it.” -GS
“I’ve been doing this a long time, and so I do get a fair number of referrals that the patients request me just because I’ve taken care of their relatives in the past or friends of theirs in the past or family members, those kinds of things.” -GS
Gastroenterologists’ referral preferences related to surgeon characteristics
Several themes emerged when GIs were asked about the surgeon characteristics they considered when deciding on a referral for their patients with rectal cancer. The majority of GIs expressed preferences for referring these patients to colorectal surgeons.
“All rectal cancers get referred to colorectal surgeons.” -GI
“I would always opt for a colorectal surgeon, just because I would assume they see much more of that in volume than a general surgeon.” -GI
However, some GIs noted that they refer to GSs who they knew to be experienced or were comfortable with the surgery.
“A general surgeon -- any surgeon whoever feels comfortable.” -GI
“[General surgeons] do everything… you kind of get the nuances of their practice with time.” GI
In addition, some GIs noted that while they preferred colorectal surgeons, they referred to GSs if that was the only type of surgeon available in their health system.
“I would refer to a general surgeon if I did not have access to a colon and rectal surgeon or a surgeon oncologist…within the health care system that I was working in. If they only had general surgeons, then I would refer to the general surgeon.” -GI
While the prompts and discussion about referral providers largely focused on surgeons, GIs pointed out the role of other specialties, particularly medical oncology and primary care providers who may be the point person in determining where a patient receives care.
“…most of the time I will send them to the oncologist, and then the oncologist goes from there. So oftentimes, it’s the oncologist who’s making the decision, where to send the patient for surgery.” -GI
“I tend to call, already, the primary care doctor right away when I found something and then I discuss if they have any preferences in terms of where the patient is seen for a surgical evaluation and oncology evaluation.” -GI
GSs’ referral preferences
Most GSs indicated they typically provide surgery to the rectal cancer patients they diagnose, although one GS indicated a preference for referring all patients with rectal cancer to a colorectal surgeon.
“[my mentor] said that her recommendation would be that you refer rectal cancers and Crohn’s, ulcerative colitis patients to colorectal surgeons. So that’s kind of what my practice has been. So, I guess, probably it’s due to my training.” -GS
When GSs did refer these patients to another surgeon, they mentioned preference for surgeons who communicate and coordinate care well.
“I like referring to that person because they keep me in the loop, or they -- you know, they don’t duplicate everything that I’ve already done, or they don’t make the patient come back a million times.” -GS
Some GSs mentioned circumstances under which they prefer to refer patients to colorectal surgeons, which are described in the next section.
Patient and disease factors that influence GIs’ referral preferences
Tumor location emerged as an important factor when considering where to refer rectal cancer cases. Many GIs referred both colon and rectal cancer cases to colorectal surgeons as a standard referral pattern but some explicitly expressed preference of referring rectal cancer cases to colorectal surgeons due to the complexity of the disease.
“The low lesions, definitely the colorectal surgeon, who has more technical expertise and stuff like that.” -GI
“I definitely think that rectal is more complex as far as surgery, or it could be -- particularly lower rectal cancer. I always -- if it is up to me, I always will have a colorectal surgeon take care of those patients.” -GI
GIs also discussed that they tended to refer patients with more advanced disease to oncologists rather than surgeons.
“Usually when I’m [referring to a non-surgeon, like medical oncology], it’s someone who’s got, like, widely-metastatic disease. Or, you know, they’re probably not… a surgical candidate.” -GI “So when there are no lymph nodes or when it is localized [I refer to a surgeon]… If there’s any lymph nodes, I’ll refer to the oncologist.” -GI
Patient and disease factors that influence GSs’ referral preferences
GSs also discussed the importance of tumor location in their decisions whether or not to refer and reported they are more comfortable treating colon cancers than rectal cancers.
“If it’s very distal, I typically will give those to a colorectal surgery specialist. But, you know, if it’s like -- if it’s around the peritoneal reflection, I’ll deal with it. The rectal cancer that I would typically manage would be, like, rectal sigmoid junction region, you know, right where the peritoneal reflection is.…my argument for why I refer someone or what determines, it’s, like, if there’s a chance they can spare the patient a sphincter and hook them up, then that would be a benefit.” -GS
“[Most of] the colon cancer, technically, from a surgical standpoint, I’m comfortable doing most of those myself. So I don’t tend to refer those as often…” -GS
Patient comorbidities were also discussed as a potential reason to refer.
“Because we’re a small community hospital. It’s not like we’re a tertiary facility. So if there are a lot of comorbidities from a medical standpoint, then I would consider that in addition [as a reason to refer the patient out].” -GS
Moreover, age was mentioned by one GS:
“If it’s an older patient that has a very low rectal cancer, then most of those patients benefit from abdominoperineal resection because if you try to do a coloanal anastomosis, they’ll have problems with incontinence, and they’re not going to be happy. But if it’s a very young patient, that has a very low rectal cancer, then I refer them out sometimes to a colorectal surgeon …so that -- you know, if they have the opportunity to get a coloanal anastomosis or something like that.” -GS
Patient preferences for referral hospitals
Both GIs and GSs expressed that patients largely want to receive care locally. Respondents noted that patients prefer the convenience of local care, especially if there are multiple clinical appointments involved. Respondents also pointed out that local care was often preferred because patients were familiar with the hospital and were at times anxious about receiving care from large academic institutions because they are intimidating.
“So for patients it’s ‘Well, if I’m going to have to go multiple times and I have to have surgery, and I don’t have anybody that lives in [X] and I don’t know anybody there,’ then they often times don’t want to go there…. And I’m in a somewhat rural area…and so the [academic medical center] seems like a big, scary place to a lot of rural people, and it’s confusing.” -GS
“Well, selecting a hospital, it’s usually they want to go to a place that they’re familiar with, where they’ve been before or where family members have been before, and then it’s close to home.” -GI
“Especially in this town… -- they go to one hospital right from the day they were born, and they want to just go to that hospital because that’s where everyone in their family goes for many reasons… which may be nonmedical reasons.” -GI
GIs and GSs noted that when patients expressed preferences about surgeons, these preferences were largely based on subjective factors.
“It is based more on personality than any mention of technical skills or outcomes or whatnot, in my experience.” -GI
“It’s very rare that I have anybody that has any objective, clinical reason for preferentially selecting something over another. It’s more “I know that town” or “it’s closer, and I have a family member who lives there.” -GS
And generally, it was rare for patients to request specific surgeons or hospitals. For the patients who do, they often request renowned academic institutions or providers they or their family are familiar with.
“I can’t think of a particular incidence where they requested a specific [doctor or hospital].” -GS
“You do get that infrequent patient that immediately says, ‘I want to go to [X].’ Infrequently you’ll get that patient that says ‘[My sister] had such-and-such, and she used this oncologist; that’s who I want to see.’ But I would say that is probably less than five percent of the cases where the patient requests or dictates something other than the plan that has been set forward.” -GI
“One is you will have a highly educated and upper-income patient who, as soon as they hear the diagnosis, they kind of want to take control of everything. And they kind of say, ‘Oh. I want to pick -- get the best care in the world. And I want to have control of everything.’” -GI
Influence of physician referrals on patient decisions
Respondents stated that patients are generally willing to see whatever surgeon they recommend, and many pointed out that respecting patient autonomy was important. In cases where the patient preferred a GS while the respondent preferred a colorectal surgeon, respondents were able to educate and counsel the patient to go with the colorectal specialist.
“I’ve never really had a patient, like, who has refused to go where I recommended they go.” -GS
“Usually they will defer to me and ask me what my preference is.”-GS
“So with rectal cancers, I’m usually going to prefer the colon and rectal surgeon. But, again, if a patient has a preference to go to their general surgeon, they have the option to do that. It’s their choice after I explain to them what the situation is.” -GI
“Yes [there are instances where I push a patient to go to [X] even if they are hesitant]. And you can -- the conversation, then, is generally one where you -- they are able to be convinced that it’s the best thing to do. And they will recognize that.” -GI
When asked how much influence they had over where patients received rectal cancer surgery, 75% of respondents indicated they were very influential or extremely influential, and the remainder indicated they were somewhat influential or that it depended on the patient. The proportion of respondents reporting very or extremely influential were similar among GIs (70%) and GSs (83%, Fischer’s exact p value =1). Respondents discussed that patients often simply deferred to their judgement and some also mentioned that the shock of the diagnosis lead to patients relying on the provider.
“I’m the one diagnosing the patient, I’m kind of catching them at their worst moment. And most of their options when I’m telling them about what they’re dealing with, the majority of patients look to me, just say, ‘Well, what do I need? What do I do, Doc?’” -GS
“I believe most of the times they go with whatever -- they leave it to your choice. You know, whatever you want. The physician’s choice, they trust.” -GI
“They go wherever I tell them to go. I tell them, ‘This is your life’”. -GI
Barriers to referral
Respondents largely expressed that they do not encounter many barriers to referral, specifically noting that patient insurance is accommodating in cases of cancer diagnosis. However, some have encountered long wait times or duplication of work when referring to high-volume academic centers.
“I think there are some -- duplication of workup that sometimes happens when they’re referred to a high-volume center…” -GS
“High-volume cancer centers, as the name implies, means that there’s a lot of pressure and volume on the centers. And, as such, there may be wait time in terms of getting the patient in to see the person I want them to see.” -GI
Influence of resource limitations on referrals
Resources repeatedly listed by both GIs and GSs as limitations to their ability to care for patients locally were endoscopic ultrasound and ancillary specialists, both surgical and non-surgical.
“There’s certain levels of care that you never have in small hospitals. You don’t have the appropriate specialists to help you out. Even, like, urology can be an issue sometimes.” -GS
“Because this is a relatively rural hospital; we don’t have pulmonology or cardiology here, you know, nephrology.” -GS
“So the place where I work, we don’t have colorectal surgeon here.” -GI
“And a very good example of [resource limitation] would be endoscopic ultrasound… So I would refer if I thought a patient needed endoscopic ultrasound.” -GI
System level factors and existing referral networks
Both GIs and GSs overwhelmingly discussed the practice and value of keeping a patient within their existing healthcare system.
“There is a lot of benefit to having the patient stay -- when we have good options in both systems, then it is beneficial to have the patient stay where they have all their records, where their primary care doc will be able to follow them, especially if they have other medical issues.” -GI
“The networks are so integrated that there is this -- you know, there is a lot of pressure on the referral patterns, which, you know -- which are dictated by the system that you’re working for or working with.” -GI
“And a lot of times, insurance and networks determine that, like, what hospital patients can go to and what they can’t go to.” –GS
Respondents felt they had freedom to refer outside of their hospital system, but many stated that they felt like they did not need to or preferred to keep patients within the system.
“Since we’re independent, since we’re not hospital owned, we make a very concerted effort to make sure that that patient stays in the system that they came from.” -GI
“Very seldom do I recommend that [patients go outside of the healthcare system].” -GS
Respondents also discussed the routine use of existing referral networks. They favored these referral networks because of their familiarity and comfort with the providers whom they had worked with for a long period of time.
“It’s just where we’ve sent people before, we’re comfortable sending them.” -GS
“We end up with working relationships with the physicians and the surgeons and the oncologists and the radiation oncologists we work with. And then it becomes, after doing it for a few years, it becomes a routine process.” -GI
Attitude toward volume-outcome relationship
Respondents, especially GIs, believed that surgeon experience and procedure volume were directly related to optimal patient outcomes.
“My impression is yes, at least as far as comparing general surgeons and colorectal surgeons. I just think that, in general, it is a lot easier for them [colorectal surgeons] to be very up to date with what’s going on and to have the skills if things turned out to be more complicated.” -GI
“I want somebody who has done a lot of them, and they do that as a major part of their practice. So obviously, you know, outcomes will be better.” -GI
GIs did not know what specifically constituted high volume in rectal cancer and frequently stated they expected colorectal surgeons or surgeons at academic centers to have more experience with rectal cancer overall.
“Well, again, I don’t have any firsthand experience, and I make no assessments. I just accept the premise that if they’re performing surgeries at a tertiary center such as [X], they’ve been vetted and they’re able to do that, and they belong there.” -GI
“One, I make sure that they are board certified in colorectal surgery. And I also, kind of, see where they had their training. And then, the third, how long they’ve been practicing… I have no idea how many [rectal cancer surgeries the surgeons I refer to] do in a year.” -GI
“For me, it is really important that they’ve had specific training in colorectal surgery.” -GI
“I haven’t had that information [on surgeon volume] made ready to me, so I just assume that our group is able to handle it. But, yeah, I haven’t reviewed it specifically by numbers.” -GI
GSs considered anywhere from 1 resection per month to 5 resections per week to be high volume. There was not clear consensus among GSs in their attitudes toward the relationship between volume and outcomes.
“I think it’s important. Sometimes that’s my hesitancy to do more of it, is that I don’t see it that often in patients that I think would be appropriate for me to operate on.” -GS
“I mean, to me, I’ve seen people who do a high volume of really crappy work, and I’ve seen people who do a small volume of really good work. So, I think to equate volume with outcomes is a difficult and probably erroneous school -- train of thought.” -GS
“I wouldn’t even -- I don’t even know. It’s something -- really never considered it [what constitutes high volume].” -GS
“You know, I have my patients, and I think I’ve had very good outcomes. And the few complications I’ve seen from other surgeons, I think it was more the patients’ social habits that got them into trouble more than the surgery.” -GS
“But my volume of that kind of [sphincter preserving] surgery is low… And someone that does this every week has a better pathological specimen than I would probably. So, I would just refer that.” -GS
Where would respondents go for surgery?
When asked where they would refer a close friend or family member for rectal cancer surgery, many GIs responded that they would recommend treatment within their hospital system or practice, citing the availability of a trusted colorectal surgeon that they had worked with. Most GSs stated that they recommend a specific large hospital or academic institution, but one indicated that he would recommend local care if they didn’t have another specific preference.
Discussion
In this study, both GIs and GSs cited similar patient and health system factors that affect rectal cancer management and referral. Generally, respondents were more likely to refer rectal cancer cases with more comorbidities, advanced disease, and low tumor location to high-volume/specialized centers or surgeons. However, the baseline preference for most GIs was to refer all rectal cancer patients to a colorectal surgeon. On the other hand, most GSs referred to colorectal surgeons only for complex patients and diseases. These baseline referral preferences may have implications at the population level where GSs have much higher representation in rural areas than GIs (4.8 vs 0.39 physicians per 100,000 people, respectively).24 Consequently, rural patients, who are more likely to receive colonoscopies from GSs than their urban counterparts, may be less likely to receive care for rectal cancer from high-volume and specialized surgeons. This difference may be even more pronounced if other rural providers (e.g. emergency physicians, primary care providers) preferentially refer rectal cancer patients to GSs rather than GIs, as is perceived by some GSs in this study.
While respondents generally did not perceive any barriers to referrals, they did consistently reference the pressure of keeping patients within existing referral networks and healthcare systems. These referral networks can be informal, built from personal connections and a prior history of referrals, or they can be more formalized, where providers refer to others within their healthcare system. While these referral practices can facilitate continuity of care and communication of patient health information, there is some evidence that restricted provider networks systematically affect where patients receive treatment. In a survey-based study of 1539 breast cancer cases, patients who reported being referred to their surgeon by a provider or health plan were less likely to have been treated at a National Cancer Institute Designated Cancer Center than patients who chose their surgeon based on reputation.25
In an effort to improve rectal cancer care, the American College of Surgeons Commission on Cancer (COC) has begun implementation of a National Accreditation Program for Rectal Cancer (NAPRC) in which accredited healthcare programs will have demonstrated compliance with a set of evidence-based, multidisciplinary standards for rectal cancer care.26,27 A 2019 study of 1315 COC hospitals found that most rectal cancer cases are cared for at low-volume or low- NAPRC adherence hospitals and that high-volume academic hospitals were the most ready for NAPRC accreditation.26 Taken together with the results of this present study, it appears that patients diagnosed in community settings may be less likely to receive care at accredited hospitals unless referral patterns break from current norms. This may be especially important for treatment of complex diseases such as rectal cancer, where patients benefit from more specialized care. Efforts to educate providers and patients on the benefits of receiving care at accredited centers and to increase incentives for appropriate referrals outside of existing systems may be necessary for the success of programs such as the NAPRC.
Respondent observations that patients rarely expressed preferences for surgeons or hospitals and that these preferences were often based on subjective factors such as personality or familiarity is echoed in a 2018 interview-based study of 15 rectal cancer survivors who had undergone surgical resection.21 Results of this study found that physician recommendation was often the sole consideration for patients on where to go for rectal cancer surgery and that patients assessed experience by how well a surgeon explained the procedure or rectal cancer. In the study, patients who received surgery at a low-volume center valued the physician’s ability to make them feel comfortable and to explain rectal cancer and treatment procedures in an understandable way. Some low-volume center patients also reported that having a connection to the surgeon (either personally or through family members) was a factor in choosing a surgeon. These themes highlight the critical role that the diagnosing provider plays in where a patient with rectal cancer receives treatment. Interestingly, respondents in the present study reported that there is also a distinct subset of patients who voice very strong preferences for treatment at large academic centers. These patients may be more highly educated, have higher socioeconomic status, or have family/friends who advocate for treatment at large specialized treatment centers. In the 2018 study of patients with rectal cancer, the authors found that receiving recommendations from family and friends and doing online research about their surgeons was a more salient theme among patients who received surgery at high-volume centers than those at low-volume centers. Thus, increasing empowerment in patients with rectal cancer and bringing awareness to rectal cancer as a complex disease that benefits from specialized care may improve patient self-advocacy.
It is important to highlight that neither access to care nor insurance limitations were significant themes discussed by respondents as barriers to referrals. According to respondents, patients preferred local care for its familiarity and convenience, not necessarily because they lacked the resources to travel to high-volume hospitals or surgeons. This was also observed in the previous qualitative study of patients with rectal cancer.21 In that study, patients who described valuing a treatment center closer to home often did so in the context of being told by the surgeon that the same procedure done at a high-volume center could be done locally or the personal belief that a surgeon would tell the patient if the surgery was too complicated to complete at a low-volume center. Efforts to centralize rectal cancer surgery may need to focus on developing treatment networks that foster efficient communication between referring hospitals and providers and allow patients to receive other components of their treatment, such as chemotherapy, close to home.
Results of our study also demonstrate that there a potential role for physician education in improving treatment for rectal cancer cases. One GS indicated that his/her practice of referring all rectal cancer cases to a colorectal surgeon stems from advice he/she received during residency training. Additionally, GIs and GSs were unclear about surgical volume levels that reflect sufficient experience with rectal cancer resection and few GSs discussed the volume-outcome relationship within their own practice. It may be beneficial to present GSs with volume and outcome data of their own practice as well as that of specialists at high volume centers.
Our study was limited to GIs and GSs in Iowa and therefore our findings may not be generalizable to other states or regions. Although we were able to recruit participants from various community settings and practice types, there is low representation of urban GSs in this study. Specifically, understanding the referral decision making among urban providers may provide insight into the observation that many patients travel past a higher-volume center to undergo surgery at a low-volume hospital for surgically complex diseases.28 Additionally, GSs reported an average of 9 rectal cancer resections per year. As a comparison, the Leapfrog Group has established a minimum surgeon volume standard of 6 annual rectal cancer resections.29 While this volume is self-reported, it is possible that our GS population have a relatively high case-volume compared to community GSs in general which may explain their tendency to keep rectal cancer cases as opposed to referring out. Some respondents indicated that their first referral is to an oncologist, who then makes subsequent treatment referrals. While our previous studies have found that the bulk of rectal cancer diagnoses (94%) were made by GIs and GS,19 including oncologists in our study population would have increased the richness of our observations. The authors of this study are employed by an academic institution and the clinicians are colorectal surgeons so it is possible that our interpretation of the data lead to results which placed cancer treatments by specialists or at high-volume centers in a more positive light. However, these baseline attitudes pertain more to our a priori assumptions than the goal of the study which was to understand how providers in the community refer patients with rectal cancer.
Conclusions
Community-based GSs in Iowa typically referred more complex patients and rectal cancer cases, especially those with low tumors, to colorectal surgeons for surgical resection. However, GIs expressed a preference to refer all rectal cancer patients to colorectal surgeons. These differences in referral patterns may lead to urban-rural disparities in the treatment of rectal cancer. Both GIs and GSs discussed the pressure of maintaining existing referral pathways and keeping patients within their healthcare system when making referrals for rectal cancer. Efforts to increase guideline recommended surgical care for rectal cancer may need to break these practice patterns in order to be successful.
Disclosure and acknowledgement:
The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article. This work was supported by the National Institutes of Health (NIH)/National Cancer Institute (NCI) contract number HHSN261201300020I (M.E.C., A.R.K.), NIH grant T32 CA 148062 (PI: R.J.W.), and NIH/NCI P30 CA086862.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Rajput A, Bullard Dunn K. Surgical management of rectal cancer. Semin Oncol. 2007;34(3):241–249. [DOI] [PubMed] [Google Scholar]
- 2.Weiser MR, Landmann RG, Wong WD, et al. Surgical salvage of recurrent rectal cancer after transanal excision. Dis Colon Rectum. 2005;48(6):1169–1175. [DOI] [PubMed] [Google Scholar]
- 3.Wiig JN, Larsen SG, Giercksky KE. Operative treatment of locally recurrent rectal cancer. Recent Results Cancer Res. 2005;165:136–147. [DOI] [PubMed] [Google Scholar]
- 4.Charlton ME, Hrabe JE, Wright KB, et al. Hospital Characteristics Associated with Stage II/III Rectal Cancer Guideline Concordant Care: Analysis of Surveillance, Epidemiology and End Results-Medicare Data. J Gastrointest Surg. 2016;20(5):1002–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Del Vecchio NJ, Schlichting JA, Chioreso C, et al. Guideline-Recommended Chemoradiation for Patients With Rectal Cancer at Large Hospitals: A Trend in the Right Direction. Dis Colon Rectum. 2019;62(10):1186–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Etzioni DA, Young-Fadok TM, Cima RR, et al. Patient survival after surgical treatment of rectal cancer: impact of surgeon and hospital characteristics. Cancer. 2014;120(16):2472–2481. [DOI] [PubMed] [Google Scholar]
- 7.Gietelink L, Henneman D, van Leersum NJ, et al. The Influence of Hospital Volume on Circumferential Resection Margin Involvement: Results of the Dutch Surgical Colorectal Audit. Ann Surg. 2016;263(4):745–750. [DOI] [PubMed] [Google Scholar]
- 8.Lorimer PD, Motz BM, Kirks RC, et al. Pathologic Complete Response Rates After Neoadjuvant Treatment in Rectal Cancer: An Analysis of the National Cancer Database. Ann Surg Oncol. 2017;24(8):2095–2103. [DOI] [PubMed] [Google Scholar]
- 9.Baek JH, Alrubaie A, Guzman EA, et al. The association of hospital volume with rectal cancer surgery outcomes. Int J Colorectal Dis. 2013;28(2):191–196. [DOI] [PubMed] [Google Scholar]
- 10.Ortiz H, Biondo S, Codina A, et al. [Hospital variation in anastomotic leakage after rectal cancer surgery in the Spanish Association of Surgeons project: The contribution of hospital volume]. Cir Esp. 2016;94(4):213–220. [DOI] [PubMed] [Google Scholar]
- 11.Ptok H, Marusch F, Kuhn R, Gastinger I, Lippert H. Influence of hospital volume on the frequency of abdominoperineal resection and long-term oncological outcomes in low rectal cancer. Eur J Surg Oncol. 2007;33(7):854–861. [DOI] [PubMed] [Google Scholar]
- 12.Yasunaga H, Matsuyama Y, Ohe K. Volume-outcome relationship in rectal cancer surgery: a new perspective. Surg Today. 2009;39(8):663–668. [DOI] [PubMed] [Google Scholar]
- 13.Yeo HL, Abelson JS, Mao J, O’Mahoney PR, Milsom JW, Sedrakyan A. Surgeon Annual and Cumulative Volumes Predict Early Postoperative Outcomes after Rectal Cancer Resection. Ann Surg. 2017;265(1):151–157. [DOI] [PubMed] [Google Scholar]
- 14.Archampong D, Borowski D, Wille-Jorgensen P, Iversen LH. Workload and surgeon’s specialty for outcome after colorectal cancer surgery. Cochrane Database Syst Rev. 2012(3):Cd005391. [DOI] [PubMed] [Google Scholar]
- 15.Huo YR, Phan K, Morris DL, Liauw W. Systematic review and a meta-analysis of hospital and surgeon volume/outcome relationships in colorectal cancer surgery. J Gastrointest Oncol. 2017;8(3):534–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ortiz H, Codina A, Ciga MA, et al. Effect of hospital caseload on long-term outcome after standardization of rectal cancer surgery in the Spanish Rectal Cancer Project. Cir Esp. 2016;94(8):442–452. [DOI] [PubMed] [Google Scholar]
- 17.Yun YH, Kim YA, Min YH, et al. The influence of hospital volume and surgical treatment delay on long-term survival after cancer surgery. Ann Oncol. 2012;23(10):2731–2737. [DOI] [PubMed] [Google Scholar]
- 18.Billingsley KG, Morris AM, Green P, et al. Does surgeon case volume influence nonfatal adverse outcomes after rectal cancer resection? J Am Coll Surg. 2008;206(6):1167–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chioreso C, Gao X, Gribovskaja-Rupp I, et al. Hospital and Surgeon Selection for Medicare Beneficiaries With Stage II/III Rectal Cancer: The Role of Rurality, Distance to Care, and Colonoscopy Provider. Ann Surg. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stitzenberg KB, Meropol NJ. Trends in centralization of cancer surgery. Ann Surg Oncol. 2010;17(11):2824–2831. [DOI] [PubMed] [Google Scholar]
- 21.Charlton ME, Shahnazi AF, Gribovskaja-Rupp I, et al. Determinants of Rectal Cancer Patients’ Decisions on Where to Receive Surgery: a Qualitative Analysis. J Gastrointest Surg. 2019;23(7):1461–1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3(2):77–101. [Google Scholar]
- 23.Sweeney A, Greenwood KE, Williams S, Wykes T, Rose DS. Hearing the voices of service user researchers in collaborative qualitative data analysis: the case for multiple coding. Health Expect. 2013;16(4):e89–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aboagye JK, Kaiser HE, Hayanga AJ. Rural-Urban Differences in Access to Specialist Providers of Colorectal Cancer Care in the United States: A Physician Workforce Issue. JAMA Surg. 2014;149(6):537–543. [DOI] [PubMed] [Google Scholar]
- 25.Katz SJ, Hofer TP, Hawley S, et al. Patterns and correlates of patient referral to surgeons for treatment of breast cancer. J Clin Oncol. 2007;25(3):271–276. [DOI] [PubMed] [Google Scholar]
- 26.Antunez AG, Kanters AE, Regenbogen SE. Evaluation of Access to Hospitals Most Ready to Achieve National Accreditation for Rectal Cancer Treatment. JAMA Surg. 2019;154(6):516–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brady JT, Xu Z, Scarberry KB, et al. Evaluating the Current Status of Rectal Cancer Care in the US: Where We Stand at the Start of the Commission on Cancer’s National Accreditation Program for Rectal Cancer. J Am Coll Surg. 2018;226(5):881–890. [DOI] [PubMed] [Google Scholar]
- 28.Birkmeyer JD, Siewers AE, Marth NJ, Goodman DC. Regionalization of high-risk surgery and implications for patient travel times. Jama. 2003;290(20):2703–2708. [DOI] [PubMed] [Google Scholar]
- 29.The Leapfrog Group. Surgical Volume. https://www.leapfroggroup.org/ratings-reports/surgical-volume. Accessed June 10, 2020.