Abstract
Background
This study aimed to investigate the recent prevalence, management, and comorbidities of diabetes among Korean adults aged ≥30 years by analyzing nationally representative data.
Methods
This study used data from the Korea National Health and Nutrition Examination Survey from 2016 to 2018, and the percentage and total number of people ≥30 years of age with diabetes and impaired fasting glucose (IFG) were estimated.
Results
In 2018, 13.8% of Korean adults aged ≥30 years had diabetes, and adults aged ≥65 years showed a prevalence rate of 28%. The prevalence of IFG was 26.9% in adults aged ≥30 years. From 2016 to 2018, 35% of the subjects with diabetes were not aware of their condition. Regarding comorbidities, 53.2% and 61.3% were obese and hypertensive, respectively, and 72% had hypercholesterolemia as defined by low-density lipoprotein cholesterol (LDL-C) ≥100 mg/dL in people with diabetes. Of the subjects with diabetes, 43.7% had both hypertension and hypercholesterolemia. With regard to glycemic control, only 28.3% reached the target level of <6.5%. Moreover, only 11.5% of subjects with diabetes met all three targets of glycosylated hemoglobin, blood pressure, and LDL-C. The percentage of energy intake from carbohydrates was higher in diabetes patients than in those without diabetes, while that from protein and fat was lower in subjects with diabetes.
Conclusion
The high prevalence and low control rate of diabetes and its comorbidities in Korean adults were confirmed. More stringent efforts are needed to improve the comprehensive management of diabetes to reduce diabetes-related morbidity and mortality.
Keywords: Comorbidity, Diabetes mellitus, Hypercholesterolemia, Hypertension, Prediabetic state, Prevalence
INTRODUCTION
Over the past few decades, the prevalence of diabetes has steadily increased [1-3]. Globally, 425 million people, representing 8.8% of the global adult population (20 to 79 years) in 2017 and 463 million (9.3%) in 2019, are estimated to be living with diabetes according to the International Diabetes Federation (IDF) Diabetes Atlas [1]. The global prevalence of diabetes has nearly doubled since 1980, rising from 4.7% to 9.3% in the adult population [2,3]. In addition, of the 463 million people living with diabetes, half (50.1%) are unaware of their condition [1].
A high burden of diabetes complications as well as diabetes itself have a significant impact on population health. Diabetes was the eighth leading cause of death among both sexes and the fifth leading cause of death in women in 2012 globally [4]. In Korea, diabetes was the sixth leading cause of death among both sexes [5]. In particular, age-standardized mortality due to diabetes was higher in Korea than in other countries that are part of the Organisation for Economic Co-operation and Development (OECD) [6]. Therefore, there is an urgent need to implement interventions that prevent diabetes, enhance its early detection, and promote lifestyle modifications and aggressive medical treatment to prevent or delay complications. In addition, valid and consistent estimates of diabetes prevalence are needed to evaluate the effect of interventions, compare trends over time, and estimate reaching diabetes targets.
Since 2012, the Korean Diabetes Association (KDA) has published Diabetes Fact Sheets (DFS) based on the Korea National Health and Nutrition Examination Survey (KNHANES), a nationwide survey conducted by the Korean Centers for Disease Control and Prevention (KCDC). The purpose of this DFS is to provide national representative statistics on the prevalence and numbers of diabetes and impaired fasting glucose (IFG) and the management status of diabetes and its comorbidities in Korea. The objective of this study was to investigate the prevalence, total number, management, and comorbidities of diabetes among Korean adults ≥30 years by analyzing nationally representative KNHANES data. In addition, energy intake and percentage of energy intake from each macronutrient were investigated among those with diabetes, previously diagnosed diabetes, and those without diabetes.
METHODS
Study population
This study analyzed data from KNHANES VII (2016 to 2018). KNHANES is a population-based cross-sectional survey that employs a rolling sampling design involving a stratified, multistage, probability cluster survey of a representative sample of the Korean population [7,8]. It consists of three surveys: a health interview survey, a health examination survey, and a nutrition survey. The total number of subjects ≥30 years of age with diabetes and IFG were determined based on the National Population Census in 2018. We constructed two datasets from KNHANES as follows: (1) KNHANES 2018 and (2) KNHANES 2016 to 2018 (merged 3 years of data). Data from KNHANES 2018 were used to calculate the prevalence of diabetes and IFG. Data for KNHANES 2016 to 2018 (merged 3 years of data) were used to identify the management status of diabetes and comorbidities in diabetes and energy intake.
Informed consent was obtained during the process of KNHANES, and this manuscript was approved by the Institutional Review Board of Soonchunhyang University Bucheon Hospital (IRB No. 2020-05-001).
Biochemical measurements
After overnight fasting, fasting plasma glucose (FPG), total cholesterol (TC), high-density lipoprotein cholesterol (HDLC), and triglyceride (TG) levels were measured using a Hitachi Autonomic Analyzer 7600 (Hitachi, Tokyo, Japan). Low-density lipoprotein cholesterol (LDL-C) was measured by direct assay for persons with TG >200 mg/dL (Hitachi Automatic Analyzer 7600). Thus, we used either directly measured or calculated LDL-C according to the Friedewald formula: LDL-C=TC–HDL-C–(TG/5) [9]. Glycosylated hemoglobin (HbA1c) levels were measured using high-performance liquid chromatography (HLC-723G7; Tosoh, Tokyo, Japan).
Definitions of IFG, diabetes, and its related comorbidities
The diagnosis of diabetes was based on FPG ≥126 mg/dL, current use of anti-diabetic medication(s), a previous history of diabetes, or HbA1c ≥6.5% [10]. IFG was defined by FPG in the range of 100 to 125 mg/dL among those without diabetes [10]. The glycemic control rate in diabetes was defined as the rate of people with HbA1c <6.5% among people with diabetes (%). Overweight was defined as a body mass index (BMI; weight in kilograms divided by the square of height in meters) ≥23.0 kg/m2, and obesity was defined as a BMI ≥25.0 kg/m2 [11]. Abdominal obesity was defined as waist circumference ≥90 cm in men and ≥85 cm in women. Hypertension was defined as systolic blood pressure (SBP) ≥140 mm Hg or diastolic blood pressure (DBP) ≥90 mm Hg and/or current use of antihypertensive medications. Control of hypertension was defined as SBP and DBP <140/85 mm Hg according to the KDA clinical practice guideline for Diabetes 2019 [12]. Hypercholesterolemia was defined as LDL-C ≥100 mg/dL or current use of lipid-lowering medication(s), and control of hypercholesterolemia was defined as LDL-C <100 mg/dL [12,13]. The awareness rate was defined as the rate of people diagnosed with diabetes by a doctor among people with diabetes (%). The treatment rate was defined as the rate of people treated with antidiabetic drugs among people with diabetes (%). The definitions of health behaviors are as follows: current smoking: smoked at least five packs of cigarettes (100 cigarettes) during the lifetime; high-risk drinking: ≥7 glasses in men or ≥5 glasses in women on the same occasion on each of 2 or more days a week; regular walking exercise: ≥5 days/week and for ≥30 minutes/activity.
The daily food and energy intake were measured using a single day 24-hour dietary recall and semiquantitative food frequency questionnaire method [8]. For estimation of nutrient intake, the 2015 Dietary Reference Intake for Koreans was used [14]. Excessive energy intake was defined as the condition wherein the percentage of energy intake was greater than 125% of the estimated energy requirement recommended by the Korean Dietary Reference Intake [14]. The percentage of energy intake from carbohydrate, protein, and fat was calculated using the following methods: the percentage of energy intake from carbohydrate=(g of carbohydrate intake×4)/[(g of carbohydrate intake×4)+(g of protein intake ×4)]+(g of fat intake×9)]×100; the percentage of energy intake from protein=(g of protein intake×4)/[(g of protein intake×4)+(g of carbohydrate intake× 4)+(g of fat intake×9)]×100; the percentage of energy intake from fat=(g of fat intake×9)/[(g of fat intake×9)+(g of carbohydrate intake×4)+(g of protein intake×4)]×100.
RESULTS
Prevalence of diabetes and IFG
Table 1 shows the prevalence of diabetes and IFG in 2018. Among Korean adults aged ≥30 years in 2018, the prevalence of diabetes was 13.8% (4.94 million). The prevalence of diabetes among Korean adults aged ≥65 years was 27.6%. There were differences in diabetes prevalence by sex, age group, and household income. The prevalence of diabetes in men was higher than that in women (15.9% vs. 11.8%). The prevalence of diabetes increased with age in both sexes. The prevalence exceeded 10% in their forties for men, while for women, it exceeded 10% in their 50s. In the group aged 40 to 49 years, the prevalence of diabetes was 3.7 times higher in men than in women (13% vs. 3.5%). However, in individuals aged 70 years and older, diabetes was more prevalent in women than in men (29.4% vs. 28.8%). By household income quintile, the prevalence in the lowest household income quintile was 14.4%, while that in the highest quintile was 8.6%.
Table 1.
Estimated prevalence of adults with diabetes and impaired fasting glucose
| Variable | Diabetes |
Impaired fasting glucose |
||||
|---|---|---|---|---|---|---|
| Total | Men | Women | Total | Men | Women | |
| By age group, yr | ||||||
| ≥30 | 13.8 (4,940) | 15.9 (2,774) | 11.8 (2,166) | 26.9 (9,485) | 32 (5,535) | 22 (3,951) |
| ≥65 | 27.6 (2,044) | 27.7 (879) | 27.5 (1,165) | 29.6 (2,178) | 31.6 (993) | 28.1 (1,185) |
| 30–39 | 3.7 (95) | 2.7 (143) | 22.9 (410) | 11.4 (891) | ||
| 40–49 | 13.0 (148) | 3.5 (565) | 34 (826) | 19.7 (1,474) | ||
| 50–59 | 17.9 (476) | 11.3 (760) | 39 (1,057) | 25.1 (1,656) | ||
| 60–69 | 25.7 (563) | 19.0 (720) | 31.8 (847) | 28.7 (891) | ||
| ≥70 | 28.8 (883) | 29.4 (586) | 31 (810) | 27.1 (622) | ||
| By family income (quintiles)a | ||||||
| Quintile 1 | 14.4 | 16.8 | 12 | |||
| Quintile 2 | 14 | 17.1 | 10.9 | |||
| Quintile 3 | 10.6 | 11.5 | 9.6 | |||
| Quintile 4 | 10.6 | 13.9 | 7.1 | |||
| Quintile 5 | 8.6 | 11.7 | 5.8 | |||
Values are presented as percentages (number; thousands).
From the lowest to the highest.
The prevalence of IFG in Korean adults aged ≥30 years in 2018 was 26.9% (9.48 million). IFG was more prevalent in men than in women (32% vs. 22%).
Current status of managing diabetes
From 2016 to 2018, only 65% of adults with diabetes were aware of their condition, and 60.1% were in treatment (oral hypoglycemic agent, 56%; insulin therapy, 4.1%) (Table 2). Most adults with previously diagnosed diabetes were being treated with oral hypoglycemic agents (86.1%), while 6.4% were treated with insulin with or without an oral hypoglycemic agent; 6.9% were not receiving any treatment for their disease (Supplementary Fig. 1). The glycemic control rate among people with diabetes was 28.3% for a target goal of HbA1c <6.5% (Supplementary Fig. 2). Of people with diabetes, 19.1% had HbA1c above 8.0%. According to the target level of the KDA treatment guidelines, 28.3% of people with diabetes achieved HbA1c <6.5%, 54.4% achieved blood pressure (BP) <140/85 mm Hg, and 53.3% achieved LDL-C <100 mg/dL.
Table 2.
Estimated proportion of awareness, treatment, and control within target glycosylated hemoglobin
| Variable | Awareness, % | Treatment, % | Glucose management (<6.5%), % |
|---|---|---|---|
| ≥30 yr | 65 | 60.1 | 28.3 |
| Men | 61.2 | 56.6 | 29.2 |
| Women | 69.8 | 64.6 | 27.2 |
| ≥65 yr | 77.9 | 72.9 | 29.3 |
Comorbidities in adults with diabetes and health behaviors
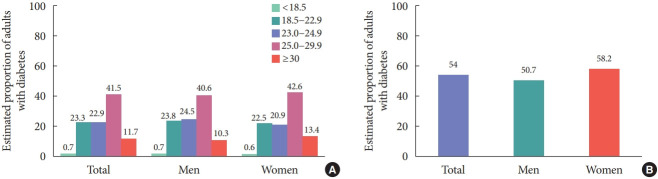
From 2016 to 2018, the prevalence of obesity and abdominal obesity in adults with diabetes was 53.2% (50.9% in men and 56.0% in women) and 54% (50.7% in men and 58.2% in women), respectively (Fig. 1). When obesity was categorized as class I to III, obesity class I (BMI 25.0 to 29.9 kg/m2) accounted for 41.5% of diabetes, obesity class II (BMI 30.0 to 34.9 kg/m2) accounted for 10.1%, and obesity class III (BMI ≥35 kg/m2) accounted for 1.6%. Morbid obesity of class II and III was 11.7% in adults with diabetes. In addition, the estimated prevalence and control rate of comorbidities are presented in Table 3. The prevalence of hypertension in adults with diabetes was 61.3%. Only 54.4% of adults with diabetes were controlled to the target level of BP. Regarding the prevalence of hypercholesterolemia, the prevalence was 72% when based on LDL-C >100 mg/dL or antilipidemic agents, and the control rate of hypercholesterolemia was 53.5%.
Fig. 1.
Estimated proportion of adults with diabetes according to (A) body mass index (kg/m2) and (B) abdominal obesity. Values are presented as percentage.
Table 3.
Estimated prevalence and control rate of comorbidities in adults with diabetes
| Variable | Hypertension |
Hypercholesterolemia |
Hypertension and hypercholesterolemia |
||
|---|---|---|---|---|---|
| Prevalence, % | Treatment rate, % | Prevalence, % | Treatment rate, % | Prevalence, % | |
| ≥30 yr | |||||
| Total | 61.3 | 54.4 | 72 | 53.3 | 43.7 |
| Men | 58.9 | 51.6 | 67.2 | 55.3 | 39.4 |
| Women | 64.4 | 57.9 | 77.8 | 51 | 49 |
| ≥65 yr | |||||
| Total | 74.3 | 63.3 | 68.6 | 59.5 | 51.4 |
| Men | 67.3 | 69.6 | 63.1 | 60.6 | 43.8 |
| Women | 79.7 | 59.2 | 72.8 | 58.8 | 57.2 |
Regarding health behaviors, 21% were current smokers (men 34.9% vs. women 3.7%), 23.1% were high-risk drinkers (men 30.7% vs. women 6.8%), and 35.7% were walking regularly (men 36.4% vs. women 34.9%) among adults 30 years of age with diabetes (Supplementary Table 1).
Prevalence of both hypertension and hypercholesterolemia in adults with diabetes
The prevalence of both hypertension and hypercholesterolemia was 43.7% (39.4% in men, 49% in women) in adults ≥30 years of age with diabetes and 51.4% (43.8% in men, 57.2% in women) in adults ≥65 years (Table 3). Only 11.5% of subjects with diabetes met all three target levels (HbA1c <6.5%, BP <140/85 mm Hg, and LDL-C <100 mg/dL).
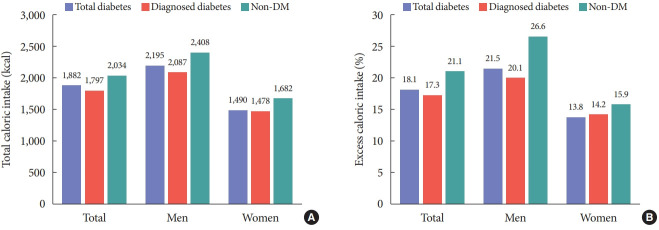
Dietary intake in adults with diabetes from 2016 to 2018
Total daily energy intake, excess energy intake, and percentage of energy intake from macronutrients were evaluated among subjects with diabetes, with previously diagnosed diabetes, and those without diabetes (Table 4 and Fig. 2). Total energy intake and excess energy intake were higher in subjects without diabetes than in those with diabetes (total or previously diagnosed) (Fig. 2). The percentage of energy intake from carbohydrates was high in the diabetes group compared to those without diabetes (68.3% in diabetes, 69.9% in diagnosed diabetes, and 64.7% in without diabetes) (Table 4). On the other hand, the percentage of energy intake from protein and fat was lower in subjects with diabetes than in those without diabetes (for protein: 14.5% in diabetes, 14.1% in diagnosed diabetes, and 15.2% in without diabetes, respectively; for fat: 17.1% in diabetes, 16.0% in diagnosed diabetes, and 20.1% in without diabetes, respectively) (Table 4).
Table 4.
Percentage of energy intake from carbohydrate, protein, and fat among people with diabetes, diagnosed diabetes, and without diabetes
| Variable | Carbohydrate |
Protein |
Fat |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Total diabetes, % | Diagnosed diabetes, % | Non-DM, % | Total diabetes, % | Diagnosed diabetes, % | Non-DM, % | Total diabetes, % | Diagnosed diabetes, % | Non-DM, % | |
| Total | 68.3 | 69.9 | 64.7 | 14.5 | 14.1 | 15.2 | 17.1 | 16.0 | 20.1 |
| Men | 66.5 | 68.3 | 63.6 | 15.2 | 14.8 | 15.7 | 18.3 | 16.9 | 20.7 |
| Women | 70.6 | 71.5 | 65.8 | 13.8 | 13.4 | 14.6 | 15.7 | 15.0 | 19.6 |
DM, diabetes mellitus.
Fig. 2.
(A) Total caloric intake and (B) excess caloric intake among people with diabetes, diagnosed diabetes, and without diabetes mellitus (DM).
DISCUSSION
In 2018, the prevalence and estimated number of diabetes cases among adults ≥30 years were 13.8% and 4.94 million, respectively. The prevalence of diabetes steadily increased over 17 years from 2001 (8.6%) to 2018 (13.8%) in adults ≥30 years of age in a nationally representative sample of Koreans [15-18]. HbA1c has been included in the diagnostic criteria for the diagnosis of diabetes since KNHANES 2011. More specifically HbA1c increased from 12.4% in 2011 to 14.5% in 2013 and then decreased slightly to 13.0% and 11.4% in 2014 and 2015, respectively [17,19]. Then, it increased again to 14.4% in 2016 and stayed at approximately 14% [18,20]. In addition, the estimated number of people with diabetes (30 to 79 years) has increased by 54% during the past 8 years, from 3.20 million in 2010 to 4.94 million in 2018 [18,21].
The global age-standardized diabetes prevalence has grown from 4.7% in 1980 to 8.5% in 2014, and this rise in prevalence has been compounded by population growth, aging, and increasing overweight or obesity, nearly quadrupling the number of adults with diabetes over these 35 years [3]. In the IDF Atlas, the global prevalence of diabetes in adults aged 20 to 79 years representing 138 countries was estimated to be 8.8% in 2017 and 9.3% in 2019 and is predicted to rise to 10.9% in 2045 [1]. Although it is difficult to fully compare differences in diabetes prevalence worldwide due to different data sources, study sample sizes, ages of the study population, and heterogeneity of definitions of diabetes, it is clear that the prevalence of diabetes has been steadily increasing for the past 3 decades globally.
Prevalence can be affected by the mortality and incidence of diabetes [22]. The prevalence can rise by improving the survival of people with diabetes and aging but can also decrease by decreasing or stabilizing the incidence. In Korea, the prevalence of diabetes has mainly increased due to population aging and increasing obesity [23,24]. Recently, in terms of incidence, some countries, including Korea, have shown decreasing or stable incidences of diabetes for several possible reasons [22]. It might be starting to benefit from prevention activities of type 2 diabetes mellitus (T2DM) and reductions in the pool of undiagnosed diabetes through increased uptake of the national health screening program. Based on the reported DFS thus far, the trend of prevalence during the past 7 years in Korea appears stable at a high rather than substantial rise.
Consistent with the results of previous DFS 2016 and 2018, DFS 2020 also showed that the prevalence of diabetes increased with age in both sexes [18-20]. The prevalence of diabetes over the age of 65 was 27.6%, which was twice the prevalence of diabetes over the age of 30 (13.8%). Consistent with previous DFS and other countries, the prevalence of diabetes showed variations according to sex; that is, it was higher among men than women [18,19,25]. DFS 2020 also showed that lower family income level was associated with higher prevalence of diabetes in both sexes. The burden of diabetes has increased at a greater rate in low- and middle-income countries than in high-income countries globally [3].
In addition, the prevalence and estimated number of IFGs were 26.9% and 9.48 million in adults aged ≥30 years and 29.6% and 2.17 million in adults aged ≥65 years, respectively. The estimated number of IFGs in this group was already 1.3 million. The prevalence of IFG gradually increased from 24.8% in DFS 2016 to 25.3% in DFS 2018 and to 26.9% in DFS 2020. We investigated the distribution of IFG prevalence according to sex and age. A higher prevalence of IFG was observed in men than in women at all ages. A drastic increase in the prevalence of IFG was observed among men aged 30 and 40 years and then decreased among elderly individuals above 60 years, whereas the prevalence among women showed a continuous increase with age. The estimated number of IFGs was reversed in both men and women for the elderly population aged above 70 years. Prevalence estimates of IFG reported in the literature vary greatly due to the diagnostic criteria used, the screening test, and characteristics of the study population [26-28]. A large meta-analysis of studies that reported prevalences in Caucasian and Asian cohorts estimated the IFG prevalence to be 53.1% [27]. In another meta-analysis, the mean overall prevalence of IFG in Europe was 8.4% (7.1 to 9.9) [28]. The prevalence of IFG is clearly increasing rapidly in all parts of the world. Because of the increasing risks of T2DM and cardiovascular disease (CVD) in prediabetic (IFG, impaired glucose tolerance) subjects and the possible reversibility of IFG, contrary to the irreversibility of diabetes, IFG has received increasingly widespread attention [29]. For the young age group, long-term exposure to IFG risks can lead to the early development of diabetes and vascular complications. Therefore, early identification of people with IFG and preventive lifestyle modifications should be strongly recommended.
Early intensive and continuous glucose control in people with diabetes can delay progression to microvascular and macrovascular complications. However, the effectiveness of these interventions at the population level has been unsatisfactory because considerable people with diabetes remain undiagnosed, and adherence to treatment may be low in the general population. In this study, the awareness and treatment of diabetes were 65% and 60.5%, respectively. Despite the improvements in screening and health promotion, 35% of the people with diabetes were unaware of their condition. In addition, 39.5% did not take treatment with glucose-lowering agents or modify their lifestyle. Nonetheless, the awareness and treatment proportion in this study were higher than those found in 2013 to 2016 (62.5% and 56.7%, respectively) and those found in China and Switzerland [18,30,31].
Regarding glycemic control, the rate of good glycemic control (HbA1c <6.5%) in people with diabetes rose steadily from 24.8% in 2013–2014 to 25.1% in 2013–2016 to 28.3% in 2016–2018 [18,19]. The control rates of HbA1c <7.0% were 43.3%, 52.6%, and 56.9% in 2013–2014, 2013–2016, and 2016–2018, respectively [18,19]. In particular, the poor control rate (defined as HbA1c ≥9.0%) decreased steadily from 15.5% in 2013–2014 to 10.8% in 2013–2016 to 9.6% in 2016–2018 [18, 19]. Although the rate of good glycemic control of HbA1c <6.5% has increased steadily over the past 7 years, it is still as low as 30%.
Regarding health behaviors, the rate of current smoking decreased from 27.4% in DFS 2016 to 24.1% in DFS 2018 and to 21.1% in DFS 2020, but the rate of high-risk alcohol drinking increased from 21.9% in DFS 2016 to 23.1% in DFS 2020. The rate of regular walking did not improve (37.9% in DFS 2016, 36.0% in DFS 2018, and 35.7% in DFS 2020). Large reductions in smoking rates occurred in the 1970s and 1980s, followed by gradual reductions thereafter [32]. Korea is no exception. According to the study by Park [33] investigating adherence to dietary recommendations between diagnosed and undiagnosed subjects with T2DM using 1998 to 2012 KNHANES, adherence to moderate alcohol drinking habits decreased over time, as was observed in the current DFS. In the present study, high-risk drinking was defined as ≥7 drinks/day in men, ≥5 drinks/day in women, and 2 times/week, whereas moderate alcohol consumption was defined as ≤1–2 drinks/day in Park’s study [33]. Although the definition of alcohol consumption was not identical between the two studies, the two studies all indicated decreasing trends in healthy alcohol consumption habits.
Adults with diabetes continue to have a two to three times higher rates of CVD than adults without diabetes [34]. An increased prevalence of the comorbid conditions obesity, hypertension, and dyslipidemia, along with poor rates of glucose control, may potentiate CVD risk. Therefore, intense efforts for the prevention and proper management of diabetes and comorbid diseases are required.
The prevalence of obesity steadily increased from 44.4% in 2011 to 48.6% in 2013–2014 to 50.4% in 2013–2016 and to 53.2% in 2016–2018 [18,19,24]. The rate of normal BMI was only 23.3% in this study. There has been little success in preventing and combating obesity despite global efforts and campaigns.
The prevalence of hypertension in diabetes increased (54.6% in 2011, 54.7% in 2013–2014, 55.3% in 2013–2016, and 61.3% in 2016–2018). However, the control rate of hypertension was improved compared to KNHANES in 2011 (25.2% in new DM, 39.9% in known DM), whereas it showed no improvement thereafter (69.1% in 2013–2014, 68.4% in 2013–2016, and 67.9% in 2016–2018) [35]. The prevalence of hypercholesterolemia in this study was much higher than that of previous reports (72% vs. 31.6% in 2013–2014 and 34.9% in 2013–2016). This was largely caused by differences in the definition of hypercholesterolemia. Previous DFS defined hypercholesterolemia based on TC ≥240 mg/dL, whereas DFS 2020 defined hypercholesterolemia as LDL-C ≥100 mg/dL. In this study, when it was defined based on TC ≥240 mg/dL, the prevalence was 42.4% (37.1% in men, 49.1% in women, data not shown). Therefore, we cannot directly compare the differences in the prevalence of hypercholesterolemia between studies. The control rate of hypercholesterolemia as LDL-C <100 mg/dL increased somewhat from 49.8% in 2013–2016 to 55.3% in this study. In addition, nearly half of people with diabetes had both hypertension and hypercholesterolemia (43.7% in adults ≥30 years and 51.4% in adults ≥65 years).
The comprehensive management of diabetes through achievement of ABC clinical targets (A, HbA1c <6.5%; B, BP <140/85 mm Hg; C, LDL-C <100 mg/dL) is important to prevent and delay vascular complications. However, only 11.5% of subjects achieved all three ABC targets in this study. Although all target achievement rates were still low, they showed increasing trends (9.4% in 2013–2014, 8.4% in 2013–2016, and 11.5% in 2016–2018).
In the present fact sheet, we investigated the total energy intake, excess energy intake, and percentage of energy intake from each macronutrient among people with diabetes, with previously diagnosed diabetes, and those without diabetes. Less energy, protein, and fat intake and more carbohydrate intake were shown in people with diabetes than in people without diabetes. Although there is no ideal percentage of macronutrients or eating patterns that can apply to all people with diabetes, low carbohydrate and lower caloric intake have been a focus in diabetes [36]. In particular, Koreans traditionally have a high carbohydrate eating pattern; therefore, they have been recommended to eat fewer carbohydrates [37]. Relatively, modification of protein intake has been less of a focus, although low protein intake in Korea has been previously reported [37]. Regarding fat, people with diabetes may have a tendency and make an effort to eat less fat to control diabetesassociated comorbidities, such as obesity and hypercholesterolemia. Lee et al. [37] evaluated food patterns of a high-carbohydrate diet among the Korean general population aged ≥20 years using data from the 2013 to 2015 KNHANES. Fifty-eight percent of men and 60% of women exceeded the recommended range of carbohydrate intake. A higher carbohydrate diet was associated with intake of low energy and saturated fats, with more grains and fruit but little consumption of proteincontaining foods, such as meat, fish, eggs, beans, and milk. Energy intake decreased across the carbohydrate groups. They found a positive association of dietary carbohydrates with metabolic disease. Our study showed that higher carbohydrate intake and lower energy intake were observed in the diabetes group than in the non-diabetes group irrespective of diagnosed or undiagnosed diabetes. Regarding the lower energy intake in the diabetes group, underreporting food intake has been suggested as a problem in diabetic patients [38]. Park [33] investigated the levels of adherence to dietary recommendations between diagnosed and undiagnosed subjects with T2DM in Korea from 1998 to 2012 KNHANES. The overall adherence levels to dietary recommendations were low regardless of awareness of disease. One of the least followed recommendations was moderating carbohydrate consumption. Both diagnosed and undiagnosed T2DM subjects had a low level of adherence in limiting carbohydrate consumption to 50% to 60% of total energy intake, with only 10% to 20% of subjects following this guideline. Carbohydrate intake is higher in the Korean population than in other Asian and Western populations [39,40]. However, another recent report demonstrated that the food sources of energy intake are changing [41]. Nonetheless, carbohydrate intake is still high in Korea. Because there were several limitations to assessing the nutritional patterns of Korean people with diabetes, the data should be interpreted with caution. First, because the study design was crosssectional, we do not know whether the pattern in subjects’ diets would contribute to the development of their disease or has been changed because of their diseases. In addition, the 1-day 24-hour recall report may not reflect the usual dietary intake of the people, and the retrospective assessment of dietary intake may induce some measurement errors. Further longitudinal studies are necessary to understand why diabetic patients showed higher carbohydrate and less energy intake than their nondiabetic counterparts.
In conclusion, a stable high prevalence of diabetes, a steadily increasing prevalence of IFG, and a low glycemic control rate in people with diabetes were again confirmed. In addition, nearly half of people with diabetes had both hypertension and hypercholesterolemia, and the target achievement rate was still very low. Therefore, more stringent efforts are needed to prevent the development of diabetes and improve the comprehensive management of diabetes to reduce diabetes-related morbidity and mortality.
Acknowledgments
This study was supported by The Korean Diabetes Association.
Highlights
• In 2018, 13.8% of Korean adults aged ≥30 years had diabetes, and 26.9% had impaired fasting glucose.
• Among subjects with diabetes, only 28.3% reached the target level of <6.5% of HbA1c.
• In people with diabetes, 53.2%, 61.3%, and 72% were obese and hypertensive, and hypercholesterolemia (LDL-C≥100 mg/dL), and 43.7% had both hypertension and hypercholesterolemia.
• Only 11.5% of subjects with diabetes met all three targets of glycosylated hemoglobin, blood pressure, and LDL-C.
• The percentage of energy intake from carbohydrates was higher in diabetes patients than in those without diabetes, while that from protein and fat was lower in subjects with diabetes.
Footnotes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS
Conception or design: C.H.J., W.J.K., H.S.K., S.J.J., J.O.M.
Acquisition, analysis, or interpretation of data: C.H.J., J.W.S., S.Y.K., H.S.K., M.S., H.J.S., S.S.L., Y.C., S.J.H., H.M.J., M.R., S.L., S.R.K.
Drafting the work or revising: C.H.J., S.J.J., M.K., B.Y., J.W.M., H.Y.L., J.S.Y.
Final approval of the manuscript: C.H.J., W.J.K., H.S.K., S.J.J., S.Y.K., S.R.K., I.K.J., J.O.M., K.H.Y.
FUNDING
None
Supplementary Materials
Supplementary materials related to this article can be found online at https://doi.org/10.4093/dmj.2020.0254
Estimated proportion of health behaviors in adults with diabetes
Estimated proportion of adults with diabetes according to type of treatment for hyperglycemia. (A) Total diabetes. (B) Diagnosed diabetes.
Glycemic control rate in diabetes. Values are presented as percentage.
REFERENCES
- 1.Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843. doi: 10.1016/j.diabres.2019.107843. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization: Global report on diabetes. Available from: https://apps.who.int/iris/handle/10665/204871 (cited 2020 Dec 18)
- 3.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387:1513–30. doi: 10.1016/S0140-6736(16)00618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization: WHO Mortality Database. Available from: https://www.who.int/healthinfo/statistics/mort/en/ (cited 2020 Dec 18)
- 5.Statistics Korea: Causes of death statistics in 2018. Available from: http://kostat.go.kr (cited 2020 Dec 18)
- 6.Organisation for Economic Co-operation and Development (OECD): Health care quality indicators: primary care. Available from: http://www.oecd.org/els/health-systems/hcqi-primarycare.htm (cited 2020 Dec 18)
- 7.Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES) Int J Epidemiol. 2014;43:69–77. doi: 10.1093/ije/dyt228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ministry of Health and Welfare: Korean National Health and Nutrition Examination Survey (KNHANES) Available from: http://knhanes.cdc.go.kr (cited 2020 Dec 18)
- 9.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 10.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37 Suppl 1:S81–90. doi: 10.2337/dc14-S081. [DOI] [PubMed] [Google Scholar]
- 11.Oh SW, Shin SA, Yun YH, Yoo T, Huh BY. Cut-off point of BMI and obesity-related comorbidities and mortality in middle-aged Koreans. Obes Res. 2004;12:2031–40. doi: 10.1038/oby.2004.254. [DOI] [PubMed] [Google Scholar]
- 12.Kim MK, Ko SH, Kim BY, Kang ES, Noh J, Kim SK, et al. 2019 Clinical practice guidelines for type 2 diabetes mellitus in Korea. Diabetes Metab J. 2019;43:398–406. doi: 10.4093/dmj.2019.0137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Committee of Clinical Practice Guideline of the Korean Society of Lipid and Atherosclerosis . Korean guidelines for the management of dyslipidemia. 4th ed. Seoul: The Korean Society of Lipid and Atherosclerosis; 2018. [Google Scholar]
- 14.Ministry of Health and Welfare . Dietary reference intakes for Koreans 2015. Sejong: The Korean Nutrition Society; 2015. [Google Scholar]
- 15.Choi YJ, Kim HC, Kim HM, Park SW, Kim J, Kim DJ. Prevalence and management of diabetes in Korean adults: Korea National Health and Nutrition Examination Surveys 1998-2005. Diabetes Care. 2009;32:2016–20. doi: 10.2337/dc08-2228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim DJ. The epidemiology of diabetes in Korea. Diabetes Metab J. 2011;35:303–8. doi: 10.4093/dmj.2011.35.4.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jeon JY, Ko SH, Kwon HS, Kim NH, Kim JH, Kim CS, et al. Prevalence of diabetes and prediabetes according to fasting plasma glucose and HbA1c. Diabetes Metab J. 2013;37:349–57. doi: 10.4093/dmj.2013.37.5.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim BY, Won JC, Lee JH, Kim HS, Park JH, Ha KH, et al. Diabetes fact sheets in Korea, 2018: an appraisal of current status. Diabetes Metab J. 2019;43:487–94. doi: 10.4093/dmj.2019.0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Won JC, Lee JH, Kim JH, Kang ES, Won KC, Kim DJ, et al. Diabetes fact sheet in Korea, 2016: an appraisal of current status. Diabetes Metab J. 2018;42:415–24. doi: 10.4093/dmj.2018.0017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Korean Diabetes Association: Diabetes fact sheet in Korea 2020. Available from: https://www.diabetes.or.kr/pro/news/admin.php?category=A&code=admin&number=1972&mode=view (cited 2020 Dec 18)
- 21.Korean Diabetes Association: Diabetes fact sheet in Korea 2012. Available from: https://www.diabetes.or.kr/pro/news/admin.php?category=A&code=admin&number=1972&mode=view (cited 2020 Dec 18)
- 22.Magliano DJ, Islam RM, Barr EL, Gregg EW, Pavkov ME, Harding JL, et al. Trends in incidence of total or type 2 diabetes: systematic review. BMJ. 2019;366:l5003. doi: 10.1136/bmj.l5003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ha KH, Kim DJ. Trends in the diabetes epidemic in Korea. Endocrinol Metab (Seoul) 2015;30:142–6. doi: 10.3803/EnM.2015.30.2.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim CS, Ko SH, Kwon HS, Kim NH, Kim JH, Lim S, et al. Prevalence, awareness, and management of obesity in Korea: data from the Korea National Health and Nutrition Examination Survey (1998-2011) Diabetes Metab J. 2014;38:35–43. doi: 10.4093/dmj.2014.38.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen CM, Yeh MC. The prevalence and determinants of impaired fasting glucose in the population of Taiwan. BMC Public Health. 2013;13:1123. doi: 10.1186/1471-2458-13-1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blum J, Aeschbacher S, Schoen T, Bossard M, Pumpol K, Brasier N, et al. Prevalence of prediabetes according to hemoglobin A1c versus fasting plasma glucose criteria in healthy adults. Acta Diabetol. 2015;52:631–2. doi: 10.1007/s00592-014-0659-y. [DOI] [PubMed] [Google Scholar]
- 27.Yip WC, Sequeira IR, Plank LD, Poppitt SD. Prevalence of prediabetes across ethnicities: a review of impaired fasting glucose (IFG) and impaired glucose tolerance (IGT) for classification of dysglycaemia. Nutrients. 2017;9:1273. doi: 10.3390/nu9111273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eades CE, France EF, Evans JM. Prevalence of impaired glucose regulation in Europe: a meta-analysis. Eur J Public Health. 2016;26:699–706. doi: 10.1093/eurpub/ckw085. [DOI] [PubMed] [Google Scholar]
- 29.Tabak AG, Herder C, Rathmann W, Brunner EJ, Kivimaki M. Prediabetes: a high-risk state for diabetes development. Lancet. 2012;379:2279–90. doi: 10.1016/S0140-6736(12)60283-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kaiser A, Vollenweider P, Waeber G, Marques-Vidal P. Prevalence, awareness and treatment of type 2 diabetes mellitus in Switzerland: the CoLaus study. Diabet Med. 2012;29:190–7. doi: 10.1111/j.1464-5491.2011.03422.x. [DOI] [PubMed] [Google Scholar]
- 31.Hu M, Wan Y, Yu L, Yuan J, Ma Y, Hou B, et al. Prevalence, awareness and associated risk factors of diabetes among adults in Xi’an, China. Sci Rep. 2017;7:10472. doi: 10.1038/s41598-017-10797-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cummings KM, Proctor RN. The changing public image of smoking in the United States: 1964-2014. Cancer Epidemiol Biomarkers Prev. 2014;23:32–6. doi: 10.1158/1055-9965.EPI-13-0798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Park K. Trends in adherence to dietary recommendations among Korean type 2 diabetes mellitus patients. Nutr Res Pract. 2015;9:658–66. doi: 10.4162/nrp.2015.9.6.658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Emerging Risk Factors Collaboration, Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375:2215–22. doi: 10.1016/S0140-6736(10)60484-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ko SH, Kwon HS, Kim DJ, Kim JH, Kim NH, Kim CS, et al. Higher prevalence and awareness, but lower control rate of hypertension in patients with diabetes than general population: the fifth Korean National Health and Nutrition Examination Survey in 2011. Diabetes Metab J. 2014;38:51–7. doi: 10.4093/dmj.2014.38.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Korean Diabetes Association . Treatment guideline for diabetes. 6th ed. Seoul: Korean Diabetes Association; 2019. [Google Scholar]
- 37.Lee YJ, Song S, Song Y. High-carbohydrate diets and food patterns and their associations with metabolic disease in the Korean population. Yonsei Med J. 2018;59:834–42. doi: 10.3349/ymj.2018.59.7.834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Salle A, Ryan M, Ritz P. Underreporting of food intake in obese diabetic and nondiabetic patients. Diabetes Care. 2006;29:2726–7. doi: 10.2337/dc06-1582. [DOI] [PubMed] [Google Scholar]
- 39.Park SH, Lee KS, Park HY. Dietary carbohydrate intake is associated with cardiovascular disease risk in Korean: analysis of the third Korea National Health and Nutrition Examination Survey (KNHANES III) Int J Cardiol. 2010;139:234–40. doi: 10.1016/j.ijcard.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 40.Lee H, Kim M, Daly BJ. Nutritional patterns of Korean diabetic patients: an exploratory study. Int Nurs Rev. 2008;55:442–6. doi: 10.1111/j.1466-7657.2008.00656.x. [DOI] [PubMed] [Google Scholar]
- 41.Yun S, Kim HJ, Oh K. Trends in energy intake among Korean adults, 1998-2015: results from the Korea National Health and Nutrition Examination Survey. Nutr Res Pract. 2017;11:147–54. doi: 10.4162/nrp.2017.11.2.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Estimated proportion of health behaviors in adults with diabetes
Estimated proportion of adults with diabetes according to type of treatment for hyperglycemia. (A) Total diabetes. (B) Diagnosed diabetes.
Glycemic control rate in diabetes. Values are presented as percentage.