Abstract
Purpose of Review
Increasingly sophisticated systems for monitoring the brain have led to an increase in the use of multimodality monitoring (MMM) to detect secondary brain injuries before irreversible damage occurs after brain trauma. This review examines the challenges and opportunities associated with MMM in this population.
Recent Findings
Locally and internationally, the use of MMM varies. Practical challenges include difficulties with data acquisition, curation, and harmonization with other data sources limiting collaboration. However, efforts toward integration of MMM data, advancements in data science, and the availability of cloud-based infrastructures are now affording the opportunity for MMM to advance the care of patients with brain trauma.
Summary
MMM provides data to guide the precision management of patients with traumatic brain injury in real time. While challenges exist, there are exciting opportunities for MMM to live up to this promise and to drive new insights into the physiology of the brain and beyond.
Keywords: Brain trauma, ICU, Multimodality monitoring, ICP, EEG, Big data
Introduction
The development of neurocritical care over the last half century has led to improvements in patient care in part through a focus on continuous, bedside monitoring of the brain [1]. Technological innovations have resulted in the widespread adoption of devices to complement the clinical neurological examination, such as parenchymal pressure sensors and continuous electroencephalography (cEEG). Increasingly sophisticated devices have been more recently developed to measure the oxygenation and metabolism within the brain tissue. Multimodality monitoring (MMM) is characterized by the integration and interpretation of these multiple sources of information to more comprehensively understand and monitor the brain after injury.
The sheer quantity of data available in a typical intensive care environment is overwhelming [2]. The additional complexity that results from integrating and responding to multiple real-time measurements of brain physiology highlights the significant challenges to the use of MMM in the critically ill [3]. However, there is promise in the use of MMM to guide the management of patients with severe brain injuries more precisely and the next wave of technological progress in computer science and engineering provides exciting opportunities for the future.
MMM in TBI
In the US each year, 56,000 people die from severe traumatic brain injury (sTBI) [4] and an estimated 30,000 with sTBI require intensive care [5]. Primary brain injuries are characterized by the pathoanatomic damage incurred by the specific mechanism of trauma, and include contusions, intracranial hemorrhage, and axonal shear injuries. Secondary brain injuries refer to downstream pathology that evolves following the primary brain injury. In patients who eventually die after sTBI, secondary brain injuries such as herniation or necrosis are seen in half and histopathologic evidence of ischemia has been reported in more than 90% [6]. However, “secondary brain injury” is a broad term. Brain injuries such as TBI create heterogeneous zones of vulnerable tissue at high risk for further injury [7••], resulting from mismatches between the metabolic supply and demand of the brain. After sTBI, inadequate perfusion pressure, brain tissue hypoxia, autoregulatory dysfunction, seizures, and spreading depolarizations of brain tissue have been observed in 50–90% of patients with ramifications for the health and recovery of the brain [8–11].
The goal of neurocritical care is to prevent or mitigate secondary brain injuries through prediction, early detection, or by monitoring treatment response [12]. Clinically, secondary brain injury manifests as neurological deterioration, which occurs in one-quarter of patients with sTBI, increasing mortality from 10 to 56% [8]. The clinical neurological exam is the standard for detecting the clinical sequelae of secondary brain injury. However, early detection is challenging in patients with sTBI due to coma or concomitant injuries that limit the sensitivity of the neurological examination. Snapshots of the brain, such as computed tomography (CT) or magnetic resonance imaging (MRI) may provide important information about secondary brain injuries, but typically at a time when damage is no longer reversible. The central use of MMM is to leverage real-time objective measurements of the mechanics, metabolism, and function of the brain to guide clinical management based on each patient’s individual pathophysiology and to detect physiologic alterations before secondary brain injuries can occur.
There are no standards for what technologies constitute “multimodality monitoring.” An understanding of brain physiology requires standard contextual ICU measurements such as arterial blood pressure (ABP) or temperature in addition to brain-specific measurements, such as EEG activity or brain tissue oxygenation (PbtO2). In the absence of standards, there is significant variability in the clinical practice of neuromonitoring. Intracranial pressure (ICP) monitoring is the most common modality [13]. However, in the USA, as few as 11.5% of patients who might be eligible for ICP monitoring actually undergo the procedure [14] and internationally, significant variability exists in the clinical criteria for its use [15••]. When brain monitoring is performed, a survey of primarily US institutions showed that most (95%) reported monitoring ICP, whereas cEEG was used by only 58% of the intensivists who responded, followed by transcranial Doppler (TCD; 49%) [13]. This experience mirrors that across 66 centers in Europe, in which TCD was used by 38% and brain tissue oxygen monitoring by 19%. The use of other devices was rare, including jugular venous oximetry (9%), microdialysis (6%), regional cerebral blood flow (5%), near-infrared spectroscopy (NIRS; 2%), and EEG (< 5%) [15••].
In contrast to stand-alone measurements, integrated MMM enables an understanding of physiologic dynamics that may not be captured or quantified by commercial measurement devices. For instance, the correlation between ABP and ICP has been validated as an index of autoregulatory function [16], but requires time-synchronized capture of both measurements at a sampling frequency of at least once-per-minute [17]. Furthermore, computational algorithms are required to infer optimum targets for cerebral perfusion pressure (ICM+®; Cambridge, UK). Tools such as this highlight the need for access to time-resolute data and an ability to manipulate that data through either existing or home-grown software. In a review of the capabilities of centers involved in TBI research internationally, barriers to the use of MMM data included lack of access to waveform-level data; variability in the recording, capture, and labeling of specific measurements; a lack of standard annotations to understand the impact of bedside events; and a lack of automated integration with other clinical information, such as imaging [18••].
Challenges in MMM
Data Acquisition
Multiple challenges restrict the full extent to which MMM can be deployed to improve neurocritical care. Neurocritical monitoring involves supplementing standard ICU data such as the electrocardiogram, ABP, respiratory and ventilator parameters, and temperature with brain-specific measurements such as ICP, PbtO2, or EEG. The volume of this waveform-level, high-resolution data at scale is incredibly large precluding permanent storage at most institutions, although device-specific data from individual patients can often be acquired and stored locally. For example, ICP recorded through the Camino® Intracranial Pressure Monitor (Natus Medical Incorporated; Pleasanton, CA) can be exported as a continuous, high-resolution waveform. However, this often requires direct interaction with the monitor itself or additional connectivity solutions to send the data to an intermediary server. When several such devices are used to generate measurements, a significant barrier occurs when each device manufacturer uses proprietary methods for collecting and converting signals or unique communication protocols. Details about the name of the device, the location of the monitoring probe, the units used to measure the ICP, and the sampling frequency may be missing or variably expressed based on the proprietary format of the metadata. These include important considerations in terms of how the data were recorded, too. The validity of ICP measurement using an external ventricular drainage catheter (EVD) depends on whether or not cerebrospinal fluid drainage was being performed concomitantly with ICP measurements, and at what level the catheter had been leveled. Additionally, even when signals can be acquired, they lack synchronization with other contextual data, such as medication administration. Without adequate synchronized, time-stamped annotations, data interpretation may be limited.
Obstacles to the clinical use of MMM also involve connectivity with clinical data and a lack of a standard data formats. Existing electronic health record (EHR) systems do not enable the collection of waveform-resolution data in neurocritical care units such that this potentially rich source of data is not integrated with a patient’s clinical record. Systems have been developed to collect and integrate data from multiple devices, such as the bedside CNS Monitor (Moberg Solutions, Inc; Ambler, PA), the BedMasterExTM software platform (Excel Medical Electronics, Inc; Jupiter, FL), the PC-based ICM + ® software, or the cloud-based SickbayTM platform (Medical informatics Corp; Houston, TX). Yet, to date, these solutions do not integrate seamlessly with the EHR. MMM research often requires development of ad hoc data infrastructures in order to collect, integrate, and share data between sites. This process can be extremely time-consuming and expensive, resulting in scattered systems all attempting to achieve a similar task. Currently, there is no universally agreed-upon standard format for multidimensional data including the high-resolution data recorded in neurocritical care, but there are examples of frameworks that are being adopted, such as the HDF5 format [19]. For EEG data, the EDF/EDF+ standard has been widely adopted, and as a result there are data repositories and analysis software solutions that have grown to support this format independent of the EEG platform used for data collection. Developing a standard data format with defined metadata to capture critical device information and contextual clinical events in the form of annotations will prove invaluable for systems in which collected data then can be easily organized, shared, and stored for clinical or research use.
Data Curation
The use of continuous physiologic data has been shown to predict subsequent clinical outcomes, including patient deterioration, better than intermittent data [20]. However, physiologic monitoring data is typically linked with EHR data only as sparse, discrete numerical data validated by ICU staff every hour. Concurrent clinical data, including medication doses and administration times, can add valuable information to help contextualize these physiologic data. As a result, MMM data is often curated with clinical data post hoc, following the completion of monitoring. The creation of a platform for seamless, real-time integration of EHR data with physiologic waveforms needed for MMM is an area of opportunity for streamlining utilization of existing technologies.
Integrating recorded data from different technologies also poses challenges. Pre-processing, which refers to data cleaning and manipulation prior to use, is often required to facilitate compatibility between data formats. For example, in paradigms that link EEG temporally to MRI data, pre-processing is required to remove artifacts prior to source localization. Stimulation-based paradigms that link clinical activity or neurologic examination to physiologic data may shed light on phenotypes such as coma recovery [21, 22], but these techniques similarly require pragmatic data cleaning in order to facilitate test-retest reliability. Spatial co-registration is also required for functional imaging, for instance, merging metabolic imaging data with EEG [23, 24]. Software used for analyzing different data modalities depends upon the type of data and may employ data-specific processing (e.g., Persyst® [Persyst; Solana Beach, CA] for EEG data; ICM + ® for ICP and ABP data) before the data can be linked. This suggests a role for an application programming interface (API) to facilitate interoperability and analysis in the clinical environment.
Physiologic data is increasingly being curated in conjunction with metabolomic or genomic data. For example, the genotype of SIRT-1 has been associated with ICP trajectory [25], and inflammatory markers have been associated with seizures [26] as well as worsening epileptiform abnormalities [27]. As with the types of data mentioned above, the process of linking MMM data with -omics data requires pre-processing. However, systematic efforts at research-level prospective data integration are being developed [28]. The use of -omics data for clinical MMM will depend on the development of increasingly efficient methods of both sequencing and analysis.
Metadata
Metadata captures critical context for understanding data at hand. There is a clear need for metadata related to physiologic signals in order to better contextualize, utilize, and understand MMM. For instance, there is limited focus on the location of MMM devices relative to injury; yet after sTBI, PbtO2 values have been found to be prognostically significant only when probes are located near a lesion [29] and nonconvulsive seizures ipsilateral to microdialysis probes have been associated with greater metabolic crisis [9]. Metadata including information about additional devices (including potential interference), clinical context such the presence of a decompressive hemicraniectomy, and signal quality may be similarly important to the interpretation of MMM data.
Collaborative Use
Increased interest in the use of MMM data has resulted in a number of inter-institutional collaborative research efforts. Due to HIPAA-related privacy constraints, MMM data may require deidentification depending on the nature of Data Use Agreements (DUA) between sites and the intended users of the data. Fully deidentified data requires all 18 HIPAA-defined identifiers be removed, which includes date-time information critical to the time-series data captured in neurocritical care. Inclusion of this data may be considered as part of a limited dataset subject to typical human subjects’ research approvals. Currently, there are few available tools to provide robust deidentification across different types of data. Data is typically deidentified locally, often manually, prior to uploading data into common resources, such as a shared database or cloud-based storage solution.
In addition to privacy concerns, there are issues related to the interoperability of terminologies used to describe clinical data, in particular physiologic data. Terminologies exist broadly for data captured in EHR systems, such as the Systematized Nomenclature of Medicine Clinical Terms (SNOMED CT®), and for specific data types such as laboratory data (e.g., Logical Observation Identifiers Names and Codes [LOINC]). The National Institutes of Health have further defined core, supplemental, and exploratory Common Data Elements for patients with specific clinical phenotypes, including TBI [30]. In the case of the Digital Imaging and Communications in Medicine (DICOM) format used for imaging data, terminologies were developed in conjunction with the data format, but this standard has suffered from significant variability in the structure and use of its metadata. A strategy to define terminology as part of the core metadata within a data format may allow for hierarchical file structures that incorporate distinct data types, including timestamps for high-resolution physiologic data, as in the open-source HDF5 format [19]. More recently, standards have evolved to define concepts and their relationship with other ontologies, including SNOMED and LOINC mentioned above. The Observational health Data Sciences and Informatics (OHDSI) consortium has adopted the Observational Medical Outcomes Partnership (OMOP) Common Data Model. Other standards such as the Informatics for Integrating Biology at the Bedside (i2B2) data model have been developed and tools are now available to harmonize between standards such that an increasing number of sites may be able to combine health data for collaborative research [31].
In the space between concerns about privacy and interoperability, there are opportunities for federated approaches to combining MMM data for research. Data federation involves the creation of virtual database structures, meaning data may be stored, analyzed, and retained locally while being accessed using common data models [32]. This approach can be flexible. For instance, summary descriptive data can be created prior to aggregation (e.g., PCORnet Common Data Model), or complex data modeling can be carried out on premises and the weights calculated for the model may be shared limiting concerns for patient privacy or inadvertent regulatory non-compliance within local frameworks [33].
Opportunities in MMM
Data Analytics
Despite challenges in the acquisition, curation, and collaborative use of MMM data in clinical practice and research, advances in data science provide exciting opportunities to integrate and summarize complex brain physiology in order to more precisely guide clinical care. Computational tools that leverage data to describe, predict, or prescribe a course of action can be collectively referred to as analytics. These tools require methods to identify clinically relevant features within the data. For instance, the mean ICP over an epoch may be less important than the relationship between ICP and perfusion in specific patients [34]. The features of MMM that map to clinically important endpoints have yet to be defined [35]. Far from an existential challenge to the use of MMM, this need provides an exciting avenue for data science to define the fingerprints of an individual’s physiologic response to injury—a concept that expands the systems biology and integrative physiology approaches underlying physiomics [36], incorporating patient-specific networks of physiologic interactions [37] to define physiologic endophenotypes. This concept may allow for innovations in treatment strategies to improve outcome after TBI.
Data analytics approaches respond to several of the challenges discussed above, but also require specific solutions of their own in order to realize the potential for MMM. For instance, overcoming data acquisition hurdles reduces the need for pre-processing procedures, thereby fostering real-time use of MMM data. Efforts are underway to standardize acquisition of clinical and high-resolution data for research purposes, including the Data Access Quality and Curation for Observational Research Designs (DAQCORD; daqcord.org) project [38••]. Work is also being done to formalize data labels and metadata specific to brain monitoring data leveraging large multi-institutional clinical trials as a test bed for data harmonization (including Transforming Research and Clinical Knowledge in Traumatic Brain Injury [TRACK-TBI; NIH U01NS086090] and the Brain Oxygen Optimization in Severe TBI Phase III studies [BOOSTIII; NIH U01NS099046]. Once data is harmonized, common algorithms for artifact rejection and normalization can be deployed, from simple threshold-based tools to AI-based open-source software solutions [39].
An important opportunity exists in understanding which aspects of MMM matter to patient care. The canary in the coal mine has been the traditional use of average ICP measurements to guide management, an approach that has been recently reframed [34, 35]. Movements to standardize the clinical reporting and interpretation of MMM data may serve as a guide to a more systematic understand of how MMM may be interpreted clinically. Yet, the ability for humans to process multiple sources of independent data is inherently limited. Computational analytic approaches integrating MMM data complement these efforts by uncovering complex inter-relationships between the body and the brain [40, 41], the network architecture of the brain itself [42], and the regulation of cerebral blood flow after injury [16]. The clinical utility of MMM data will require clinical experience married with sophisticated computational tools. Early examples of this include cluster-based analyses uncovering patterns within MMM data that correspond to unique cohorts of patients with different outcomes and individual physiologic states that evolve over time [43, 44]. Hidden Markov models have similarly demonstrated time-dependent physiologic states defined by time-series ICP, cerebral perfusion pressure (CPP), autoregulatory capacity, and compensatory reserve [45].
Traditional statistical learning approaches such as regression modeling typically focus on discrete clinical data. For example, in patients with moderate to severe TBI, a combination of clinical and radiologic variables available at the time of admission have been used to create a model of unfavorable outcome or death that has been validated across more than 15,000 patients with an area under the receiver operating characteristic curve (AUC) of ~ 80% [46]. The addition of physiologic data to this model has consistently improved its predictive ability. In one study, the use of cEEG monitoring within the first 24 h of trauma improved the AUC from 65 to 77% [47]. In another, the addition of minute-to-minute ICP and ABP values increased the AUC from 72 to 90% [48]. Further integration of MMM data with the rich clinical information captured within the EHR is critical to understanding the impact of injury severity and ICU care (e.g., sedation) on patient trajectory.
A “Medical Record” for the Brain
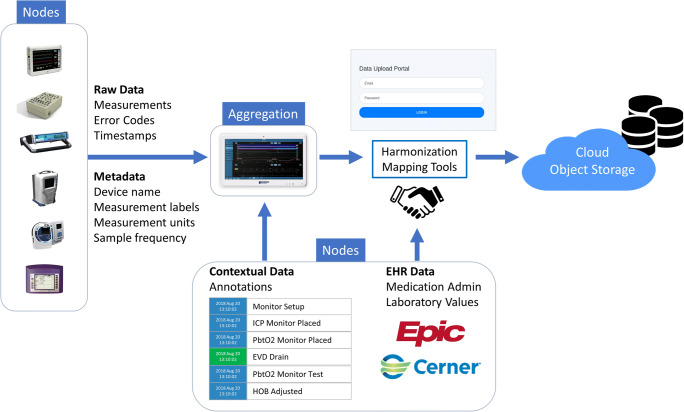
MMM serves to guide clinicians in their management of patients by detecting subtle changes in brain physiology prior to irreversible secondary brain injury. We describe here our recent work in overcoming many of the challenges to the use of MMM by designing a dynamic medical record focused on brain monitoring data, one that ultimately aims to provide real-time precision management of TBI (Fig. 1).
Fig. 1.
A medical record for the brain. A schematic depicting an architecture designed to overcome many of the challenges to the use of multimodality monitoring for clinical and research use. Nodes refer to sources of data including devices such as bedside vital sign monitoring devices, intracranial monitoring devices, or systems designed to capture electroencephalography activity. Nodes also refer to sources of clinical and contextual data such as the electronic health record (EHR) or annotations made at bedside, as shown here through an interactive touchscreen interface. Blue arrows indicate data pathways, which refer to methods of moving data from one node to another. Harmonization mapping refers to methods that allow for disparate data paths to link to a specific patient encounter and to synchronize with date/time stamps using standard definitions or labels. These standards further allow harmonization across patients and institutions. Harmonized data is then uploaded to a cloud-based object storage repository in order to maximize collaboration while limiting local resource utilization
First, we designed an architecture for a cloud-based analytics platform for neurocritical care data. In brief, this platform consists of three basic elements: components, data paths, and standards. A component is a “node” in the system and can be a source of data such as a medical device or a data repository. Data paths refer to getting data from one node to another such as from the EHR to an analytics tool. Standards are those required to harmonize data from different patients or multiple institutions including uniform data labels, archive formats, and/or transfer protocols.
We have implemented our design using cloud-based object storage as a repository for high-resolution physiological data from TBI patients. Nodes consist of devices collecting vital signs data (Intellivue [Philips North American Corporation; Andover, MA) and CarescapeTM [GE Healthcare; Chicago, IL]), ICP (Camino® ICP Monitor [Natus Medical Inc; Pleasanton, CA], RAUMEDIC DATALOGGER and EASY logo [Raumedic; River Mills, NC), PbtO2 (Licox® [Integra LifeSciences; Plansboro Township, NJ] and RAUMEDIC devices), and others. Device data is sent to a bedside CNS monitor which acts to aggregate data sources. For the data path from devices to aggregator, we used the devices’ proprietary protocols since no standard medical device communications protocol has yet been widely adopted. Software was written to implement the data path subsequently from clinical sites to the cloud object storage repository. This upload portal is capable of user authentication, initial error-checking, and secure transfer to cloud object storage. Data is mapped to standardized labels and metadata is extracted. Events and annotations noted at the bedside are extracted from a separate data file.
Additional data paths are being developed from the EHR to the cloud object storage repository to incorporate laboratory and medication administration information. Interoperable cloud-based applications comprise additional nodes. For example, a visualization tool has been implemented that provides flexible views of the data alongside events and medications. An API is currently under development to allow for modular data analytic “plug-ins” allowing clinicians and researchers to choose computational analytics as needed for specific applications or specific patients.
Examples of Modular Analytics
EEG and Sedative Medication Data
Seizures and periodic or rhythmic discharges occur in 14–61% of patients with TBI admitted to the ICU. When recurrent seizures or status epilepticus (SE) occurs, patients may be treated with anesthetic coma. However, when sedation is weaned, uncertain EEG patterns may emerge that mimic SE [49], albeit transiently, before EEG begins to improve [50]. In contrast, weaning sedative medications may be informed by changes in EEG activity not apparent to the human eye [51]. Therefore, inclusion of medication data from the EHR may be instrumental to understanding EEG monitoring data during liberation from anesthetics, limiting morbidity associated with prolonged mechanical ventilation and sedation.
Optimum CPP
The concept of optimum CPP (CPPopt) derives from observations that while autoregulation is frequently dysfunctional following TBI, there is often a narrow range of CPP at which autoregulatory mechanisms continue to function. Operating at CPPopt may limit the sequelae of falling below the lower limits of autoregulation (ischemia, hypoxia, elevations in ICP) or riding above the upper limits of autoregulation (hyperemia, elevations in ICP). Identification of CPPopt requires 10-s measurements of average ICP and mean arterial pressure to generate a 5-min moving average correlation coefficient termed the pressure reactivity index (PRx), which is mapped against average CPP values yielding a U-shaped curve [16]. As a proof of concept, we developed a graphical user interface that incorporates second-by-second ICP and ABP from the CNS monitor translated to Matlab (MathWorks; Natick, MA) format and published multi-window weighting algorithms [52] to generate a time-series of estimated CPPopt values. Communication of CPPopt into the EHR forms a critical next step through the Substitutable Medical Applications, Reusable Technologies (SMART) standard using a Fast Healthcare Interoperability Resources (FHIR) API.
The Future of MMM
There are several hurdles that will need to be addressed in the near future. First, data workflows to eliminate artifacts in real time are critical. For example, ICP measurements recorded while an EVD is clamped are not useful for calculating the PRx, but these epochs can be readily distinguished from valid, pulsatile ICP waveform data. Artifact reduction technologies for EEG data are more mature, but there is a need for data-specific algorithms. Second, contextual clinical data requires automated methods of accurate time-synchronized annotation. Currently, bedside annotations are not standardized and medication administration data contained within the EHR may be inaccurate by minutes or even hours in some cases. Finally, metadata that captures data critical for the interpretation of MMM data is needed, likely as an extension of the existing NIH/NINDS Common Data Elements and incorporated into Common Data Models and/or open-source, portable data formats.
Conclusions
While the goal of MMM is to provide critical information about the health and function of brain tissue in real time to guide patient-specific management, the promise of MMM for clinical and research purposes is limited by challenges in data acquisition, curation, and collaboration. Efforts are underway to create scalable solutions to overcome these barriers and provide (a) methods for integrating and harmonizing high-resolution MMM data with biological, clinical, radiographic, and outcomes data; (b) a common resource that will leverage data science tools to derive novel insights into patient-level physiology; and (c) an open-source API to allow data exploration and analysis ad hoc by clinicians and researchers without the need for computer science expertise. MMM provides an exciting opportunity to develop tools for clinicians to use in order to provide patients with TBI the precise management that they require and to develop new scientific insights into the physiology of brain trauma and beyond.
Funding
Funding was provided by the National Institute of Neurological Disorders and Stroke (Grant No. K23NS105950; ESR and Grant No. K23NS101123; BF) and U.S. Department of Defense (Grant No. W81XWH-18-DMRDP-PTCRA; BF, ESR, DM). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Department of Defense or the National Institutes of Health.
Declarations
Ethics Approval and Consent to Participate
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
Authors BF, ESR, and DM receive grant funding support from the Department of Defense through a subcontract from Moberg ICU Solutions, Inc. ESR receives financial compensation as a member of the scientific advisory board for UCB Pharmaceuticals and Ceribell, Inc. BF receives financial compensation as a member of the scientific advisory board and speakers’ bureau for UCB Pharmaceuticals. DM is the founder of Moberg ICU Solutions, Inc maker of the CNS Monitor. Other authors declare no conflicts of interest.
Footnotes
This article is part of the Topical Collection on Neurotrauma
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Brandon Foreman, Email: foremabo@ucmail.uc.edu.
India A Lissak, Email: ilissak@mgh.harvard.edu.
Neha Kamireddi, Email: nk593@drexel.edu.
Dick Moberg, Email: dick.moberg@micromedgroup.com.
Eric S Rosenthal, Email: EROSENTHAL@mgh.harvard.edu.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
- 1.Suarez JI. Outcome in neurocritical care: advances in monitoring and treatment and effect of a specialized neurocritical care team. Crit Care Med. 2006;34(9 Suppl):S232–S238. doi: 10.1097/01.CCM.0000231881.29040.25. [DOI] [PubMed] [Google Scholar]
- 2.Foreman B. Neurocritical Care: bench to bedside (Eds. Claude Hemphill, Michael James) Integrating and Using Big Data in Neurocritical Care. Neurotherapeutics. 2020;17(2):593–605. doi: 10.1007/s13311-020-00846-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Foreman B, Ngwenya LB. The sustainability of applied intracranial multimodality neuromonitoring after severe brain injury. World Neurosurg. 2019. [DOI] [PubMed]
- 4.Taylor CA, Bell JM, Breiding MJ, Xu L. Traumatic brain injury–related emergency department visits, hospitalizations, and deaths—United States, 2007 and 2013. MMWR Surveill Summ. 2017;66(9):1. doi: 10.15585/mmwr.ss6609a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reddy GD, Gopinath S, Robertson C. Critical care management of the patient with traumatic brain injury. Semin Neurol. 2016;36(6):570–576. doi: 10.1055/s-0036-1592169. [DOI] [PubMed] [Google Scholar]
- 6.Shackford SR, Mackersie RC, Holbrook TL, Davis JW, Hollingsworth-Fridlund P, Hoyt DB, et al. The epidemiology of traumatic death. A population-based analysis. Arch Surg. 1993;128(5):571–575. doi: 10.1001/archsurg.1993.01420170107016. [DOI] [PubMed] [Google Scholar]
- 7.•• Launey Y, Fryer TD, Hong YT, Steiner LA, Nortje J, Veenith TV. et al., Spatial and temporal pattern of ischemia and abnormal vascular function following traumatic brain injury. JAMA Neurol. 2019; This work highlights the spatiotemporal heterogeneity in pathology after traumatic brain injury in a way that is critical to inform multimodality neuromonitoring. This builds on prior work to provide the most comprehensive view of the nature of secondary brain injury. [DOI] [PMC free article] [PubMed]
- 8.Juul N, Morris GF, Marshall SB, Marshall LF. Intracranial hypertension and cerebral perfusion pressure: influence on neurological deterioration and outcome in severe head injury. The Executive Committee of the International Selfotel Trial. J Neurosurg. 2000;92(1):1–6. doi: 10.3171/jns.2000.92.1.0001. [DOI] [PubMed] [Google Scholar]
- 9.Vespa P, Tubi M, Claassen J, Buitrago-Blanco M, McArthur D, Velazquez AG, et al. Metabolic crisis occurs with seizures and periodic discharges after brain trauma. Ann Neurol. 2016;79(4):579–590. doi: 10.1002/ana.24606. [DOI] [PubMed] [Google Scholar]
- 10.Hartings JA, Andaluz N, Bullock MR, Hinzman JM, Mathern B, Pahl C, et al. Prognostic value of spreading depolarizations in patients with severe traumatic brain injury. JAMA Neurol. 2020;77(4):489–499. doi: 10.1001/jamaneurol.2019.4476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Steiner LA, Czosnyka M, Piechnik SK, Smielewski P, Chatfield D, Menon DK, et al. Continuous monitoring of cerebrovascular pressure reactivity allows determination of optimal cerebral perfusion pressure in patients with traumatic brain injury. Crit Care Med. 2002;30(4):733–738. doi: 10.1097/00003246-200204000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Le Roux P, Menon DK, Citerio G, Vespa P, Bader MK, Brophy GM, et al. Consensus summary statement of the International Multidisciplinary Consensus Conference on Multimodality Monitoring in Neurocritical Care : a statement for healthcare professionals from the Neurocritical Care Society and the European Society of Intensive Care Medicine. Intensive Care Med. 2014;40(9):1189–1209. doi: 10.1007/s00134-014-3369-6. [DOI] [PubMed] [Google Scholar]
- 13.Sivakumar S, Taccone FS, Rehman M, Hinson H, Naval N, Lazaridis C. Hemodynamic and neuro-monitoring for neurocritically ill patients: an international survey of intensivists. J Crit Care. 2017;39:40–47. doi: 10.1016/j.jcrc.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 14.Aiolfi A, Benjamin E, Khor D, Inaba K, Lam L, Demetriades D. Brain trauma foundation guidelines for intracranial pressure monitoring: compliance and effect on outcome. World J Surg. 2017;41(6):1543–1549. doi: 10.1007/s00268-017-3898-6. [DOI] [PubMed] [Google Scholar]
- 15.Cnossen MC, Huijben JA, van der Jagt M, Volovici V, van Essen T, Polinder S, et al. Variation in monitoring and treatment policies for intracranial hypertension in traumatic brain injury: a survey in 66 neurotrauma centers participating in the CENTER-TBI study. Crit Care. 2017;21(1):233. doi: 10.1186/s13054-017-1816-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aries MJ, Czosnyka M, Budohoski KP, Steiner LA, Lavinio A, Kolias AG, et al. Continuous determination of optimal cerebral perfusion pressure in traumatic brain injury. Crit Care Med. 2012;40(8):2456–2463. doi: 10.1097/CCM.0b013e3182514eb6. [DOI] [PubMed] [Google Scholar]
- 17.Depreitere B, Guiza F, Van den Berghe G, Schuhmann MU, Maier G, Piper I, et al. Pressure autoregulation monitoring and cerebral perfusion pressure target recommendation in patients with severe traumatic brain injury based on minute-by-minute monitoring data. J Neurosurg. 2014;120(6):1451–1457. doi: 10.3171/2014.3.JNS131500. [DOI] [PubMed] [Google Scholar]
- 18.Rodriguez A, Smielewski P, Rosenthal E, Moberg D. Medical device connectivity challenges outline the technical requirements and standards for promoting big data research and personalized medicine in neurocritical care. Mil Med. 2018;183(suppl_1):99–104. doi: 10.1093/milmed/usx146. [DOI] [PubMed] [Google Scholar]
- 19.Cabeleira M, Ercole A, Smielewski P. HDF5-based data format for archiving complex neuro-monitoring data in traumatic brain injury patients. Acta Neurochir Suppl. 2018;126:121–125. doi: 10.1007/978-3-319-65798-1_26. [DOI] [PubMed] [Google Scholar]
- 20.Adams H, Donnelly J, Czosnyka M, Kolias AG, Helmy A, Menon DK, et al. Temporal profile of intracranial pressure and cerebrovascular reactivity in severe traumatic brain injury and association with fatal outcome: an observational study. PLoS Med. 2017;14(7):e1002353. doi: 10.1371/journal.pmed.1002353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Edlow BL, Chatelle C, Spencer CA, Chu CJ, Bodien YG, O'Connor KL, et al. Early detection of consciousness in patients with acute severe traumatic brain injury. Brain. 2017;140(9):2399–2414. doi: 10.1093/brain/awx176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Claassen J, Doyle K, Matory A, Couch C, Burger KM, Velazquez A, et al. Detection of brain activation in unresponsive patients with acute brain injury. N Engl J Med. 2019;380(26):2497–2505. doi: 10.1056/NEJMoa1812757. [DOI] [PubMed] [Google Scholar]
- 23.Subramaniam T, Jain A, Hall LT, Cole AJ, Westover MB, Rosenthal ES, et al. Lateralized periodic discharges frequency correlates with glucose metabolism. Neurology. 2019;92(7):e670–e6e4. doi: 10.1212/WNL.0000000000006903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Struck AF, Westover MB, Hall LT, Deck GM, Cole AJ, Rosenthal ES. Metabolic correlates of the ictal-interictal continuum: FDG-PET during continuous EEG. Neurocrit Care. 2016;24(3):324–331. doi: 10.1007/s12028-016-0245-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jha RM, Elmer J, Zusman BE, Desai S, Puccio AM, Okonkwo DO, et al. Intracranial pressure trajectories: a novel approach to informing severe traumatic brain injury phenotypes. Crit Care Med. 2018;46(11):1792–1802. doi: 10.1097/CCM.0000000000003361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Claassen J, Albers D, Schmidt JM, De Marchis GM, Pugin D, Falo CM, et al. Nonconvulsive seizures in subarachnoid hemorrhage link inflammation and outcome. Ann Neurol. 2014;75(5):771–781. doi: 10.1002/ana.24166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lissak IA, Zafar SF, Westover MB, Schleicher RL, Kim JA, Leslie-Mazwi T, et al. Soluble ST2 is associated with new epileptiform abnormalities following nontraumatic subarachnoid hemorrhage. Stroke. 2020;51(4):1128–1134. doi: 10.1161/STROKEAHA.119.028515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bernard F, Gallagher C, Griesdale D, Kramer A, Sekhon M, Zeiler FA. The CAnadian high-resolution traumatic brain injury (CAHR-TBI) research collaborative. Can J Neurol Sci. 2020;47(4):551–556. doi: 10.1017/cjn.2020.54. [DOI] [PubMed] [Google Scholar]
- 29.Ponce LL, Pillai S, Cruz J, Li X, Julia H, Gopinath S, et al. Position of probe determines prognostic information of brain tissue PO2 in severe traumatic brain injury. Neurosurgery. 2012;70(6):1492–1502. doi: 10.1227/NEU.0b013e31824ce933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yue JK, Vassar MJ, Lingsma HF, Cooper SR, Okonkwo DO, Valadka AB, et al. Transforming research and clinical knowledge in traumatic brain injury pilot: multicenter implementation of the common data elements for traumatic brain injury. J Neurotrauma. 2013;30(22):1831–1844. doi: 10.1089/neu.2013.2970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Klann JG, Joss MAH, Embree K, Murphy SN. Data model harmonization for the All Of Us Research Program: transforming i2b2 data into the OMOP common data model. PLoS One. 2019;14(2):e0212463. doi: 10.1371/journal.pone.0212463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lin CP, Stephens KA, Baldwin LM, Keppel GA, Whitener RJ, Echo-Hawk A, et al. Developing governance for federated community-based EHR data sharing. AMIA Jt Summits Transl Sci Proc. 2014;2014:71–76. [PMC free article] [PubMed] [Google Scholar]
- 33.Sheller MJ, Edwards B, Reina GA, Martin J, Pati S, Kotrotsou A, et al. Federated learning in medicine: facilitating multi-institutional collaborations without sharing patient data. Sci Rep. 2020;10(1):12598. doi: 10.1038/s41598-020-69250-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chesnut RM, Videtta W. Situational intracranial pressure management: an argument against a fixed treatment threshold. Crit Care Med. 2020;48(8):1214–1216. doi: 10.1097/CCM.0000000000004395. [DOI] [PubMed] [Google Scholar]
- 35.Lazaridis C, Goldenberg FD. Intracranial pressure in traumatic brain injury: from thresholds to heuristics. Crit Care Med. 2020;48(8):1210–1213. doi: 10.1097/CCM.0000000000004383. [DOI] [PubMed] [Google Scholar]
- 36.Bassingthwaighte JB. Strategies for the physiome project. Ann Biomed Eng. 2000;28(8):1043–1058. doi: 10.1114/1.1313771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bashan A, Bartsch RP, Kantelhardt JW, Havlin S, Ivanov P. Network physiology reveals relations between network topology and physiological function. Nat Commun. 2012;3:702. doi: 10.1038/ncomms1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ercole A, Brinck V, George P, Hicks R, Huijben J, Jarrett M, et al. Guidelines for data acquisition, quality and curation for observational research designs (DAQCORD) J Clin Translat Sci. 2020;4(4):354–359. doi: 10.1017/cts.2020.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Edinburgh T, Smielewski P, Czosnyka M, Eglen SJ, Ercole A. DeepClean--self-supervised artefact rejection for intensive care waveform data using generative deep learning. arXiv preprint arXiv:190803129. 2019. [DOI] [PubMed]
- 40.Mowery NT, Norris PR, Riordan W, Jenkins JM, Williams AE, Morris JA., Jr Cardiac uncoupling and heart rate variability are associated with intracranial hypertension and mortality: a study of 145 trauma patients with continuous monitoring. J Trauma. 2008;65(3):621–627. doi: 10.1097/TA.0b013e3181837980. [DOI] [PubMed] [Google Scholar]
- 41.Gao L, Smielewski P, Czosnyka M, Ercole A. Early asymmetric cardio-cerebral causality and outcome after severe traumatic brain injury. J Neurotrauma. 2017;34(19):2743–2752. doi: 10.1089/neu.2016.4787. [DOI] [PubMed] [Google Scholar]
- 42.Claassen J, Velazquez A, Meyers E, Witsch J, Falo MC, Park S, et al. Bedside quantitative electroencephalography improves assessment of consciousness in comatose subarachnoid hemorrhage patients. Ann Neurol. 2016;80(4):541–553. doi: 10.1002/ana.24752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sorani MD, Hemphill JC, 3rd, Morabito D, Rosenthal G, Manley GT. New approaches to physiological informatics in neurocritical care. Neurocrit Care. 2007;7(1):45–52. doi: 10.1007/s12028-007-0043-7. [DOI] [PubMed] [Google Scholar]
- 44.Cohen MJ, Grossman AD, Morabito D, Knudson MM, Butte AJ, Manley GT. Identification of complex metabolic states in critically injured patients using bioinformatic cluster analysis. Crit Care. 2010;14(1):R10. doi: 10.1186/cc8864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Asgari S, Adams H, Kasprowicz M, Czosnyka M, Smielewski P, Ercole A. Feasibility of hidden Markov models for the description of time-varying physiologic state after severe traumatic brain injury. Crit Care Med. 2019;47(11):e880–e8e5. doi: 10.1097/CCM.0000000000003966. [DOI] [PubMed] [Google Scholar]
- 46.Steyerberg EW, Mushkudiani N, Perel P, Butcher I, Lu J, McHugh GS, et al. Predicting outcome after traumatic brain injury: development and international validation of prognostic scores based on admission characteristics. PLoS Med. 2008;5(8):e165. doi: 10.1371/journal.pmed.0050165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lee H, Mizrahi MA, Hartings JA, Sharma S, Pahren L, Ngwenya LB, et al. Continuous electroencephalography after moderate to severe traumatic brain injury. Crit Care Med. 2019;47(4):574–582. doi: 10.1097/CCM.0000000000003639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Guiza F, Depreitere B, Piper I, Van den Berghe G, Meyfroidt G. Novel methods to predict increased intracranial pressure during intensive care and long-term neurologic outcome after traumatic brain injury: development and validation in a multicenter dataset. Crit Care Med. 2013;41(2):554–564. doi: 10.1097/CCM.0b013e3182742d0a. [DOI] [PubMed] [Google Scholar]
- 49.Leitinger M, Trinka E, Gardella E, Rohracher A, Kalss G, Qerama E, et al. Diagnostic accuracy of the Salzburg EEG criteria for non-convulsive status epilepticus: a retrospective study. Lancet Neurol. 2016;15(10):1054–1062. doi: 10.1016/S1474-4422(16)30137-5. [DOI] [PubMed] [Google Scholar]
- 50.Das AS, Lee JW, Rosenthal ES, Vaitkevicius H. Successful wean despite emergence of ictal-interictal EEG patterns during the weaning of prolonged burst-suppression therapy for super-refractory status epilepticus. Neurocrit Care. 2018;29(3):452–462. doi: 10.1007/s12028-018-0552-6. [DOI] [PubMed] [Google Scholar]
- 51.Rubin DB, Angelini B, Shoukat M, Chu CJ, Zafar SF, Westover MB, et al. Electrographic predictors of successful weaning from anaesthetics in refractory status epilepticus. Brain. 2020;143(4):1143–1157. doi: 10.1093/brain/awaa069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Liu X, Maurits NM, Aries MJH, Czosnyka M, Ercole A, Donnelly J, et al. Monitoring of optimal cerebral perfusion pressure in traumatic brain injured patients using a multi-window weighting algorithm. J Neurotrauma. 2017;34(22):3081–3088. doi: 10.1089/neu.2017.5003. [DOI] [PubMed] [Google Scholar]