Abstract
Background
Robot-assisted surgery was developed to improve accuracy and outcomes in total knee arthroplasty (TKA). One important determinant of TKA success is a well-balanced knee throughout the range of motion. The purpose of this study is to determine if robot-assisted TKA (RA-TKA) results in improved intracompartmental ligament balance compared with conventional jig-based instrumentation (CM-TKA).
Methods
This retrospective cohort study included 2 cohorts—a CM-TKA (n = 49) vs RA-TKA (n = 37) cohort. Demographic and intraoperative data, including intraoperative compartment loads, were measured after final implant implantation in extension (10°), mid-flexion (45°), and full flexion (90°), using an intraoperative compartment pressure sensor. An a priori power analysis revealed our study exhibited >80% power in detecting a 5-pound (lb) difference in compartment loads in the 2 cohorts.
Results
There was no difference between medial and lateral compartment loads in extension, mid-flexion, and full flexion for the conventional (15.1 lbs, 15.9 lbs, and 13.4 lbs, respectively) vs RA-TKA (14.2 lbs, 15.1 lbs, and 10.3 lbs, respectively). The percentage of patients with high load compartment pressure in flexion (>40 lbs) by the conclusion of the surgery was significantly greater for the conventional (18%) vs the robotic TKA cohort (3%, P = .025). The percentage of patients with unbalanced knees (>20 lbs differential between medial and lateral compartments) in flexion was significantly greater in the conventional (24%) vs robotic TKA cohort (5%, P = .018).
Conclusions
In this series, RA-TKA resulted in improved intraoperative compartment balancing in flexion with no observed difference in mid-flexion and extension compared with CM-TKA.
Keywords: TKA, Total knee replacement, Compartmental balancing, Robotic assisted TKA, Robotic navigation
Introduction
While total knee arthroplasty (TKA) remains one of the most successful surgical interventions in the world, the dissatisfaction rate is not insignificant, with reported estimates of ~20% [1]. General consensus among arthroplasty specialists is that a successful TKA relies on accurate implant placement, limb alignment, patella tracking, coronal and sagittal ligamentous balancing, and soft-tissue balancing [2,3]. In an attempt to improve satisfaction, techniques for performing successful TKA are continually evolving. Robot-assisted surgery, which uses dynamic referencing and precision instrumentation for patient-specific bone cuts and implant placement, is one technology developed to help improve outcomes in TKA. Given the increased costs and resources associated with robot-assisted surgery, it is critical to determine if its utilization can result in improved outcomes compared with traditional, manual TKA.
An important determinant of a successful TKA is a well-balanced knee throughout the entire knee range of motion. Balancing, which is based off of bone resection and soft-tissue releases, is critical to achieve favorable postoperative functional performance and patient satisfaction after TKA [[4], [5], [6]]. A poorly balanced knee may be associated with instability, stiffness, increased polyethylene wear, aseptic loosening, and component mal-alignment, all of which can contribute to early implant failure, patient dissatisfaction, and possibly early revision surgery [[7], [8], [9]]. Robot-assisted technology may offer several advantages over traditional jig-based TKA in stability and function by reducing outliers, improving accuracy of component alignment and joint-line restoration and balancing of flexion and extension gaps [[10], [11], [12], [13]]. Newer generation robotic technology allows for assessment of the soft tissue tension throughout the range of motion of the knee providing surgeons real-time objective information to support subjective attempts at ligamentous balance. Ligamentous balance influences the loads on the medial and lateral compartments of the knee. To date, there is a paucity of literature specifically describing the impact of imageless robotic system used at our institution on the balancing of soft tissues and loads in these compartments after TKA. Therefore, the purpose of this study was to determine if utilization of an imageless robot-assisted surgery results in improved compartment balancing compared with conventional manual TKA. We hypothesized that imageless robot-assisted TKA would result in significantly improved compartmental balance throughout the entire range of motion compared with conventional manual TKA.
Material and methods
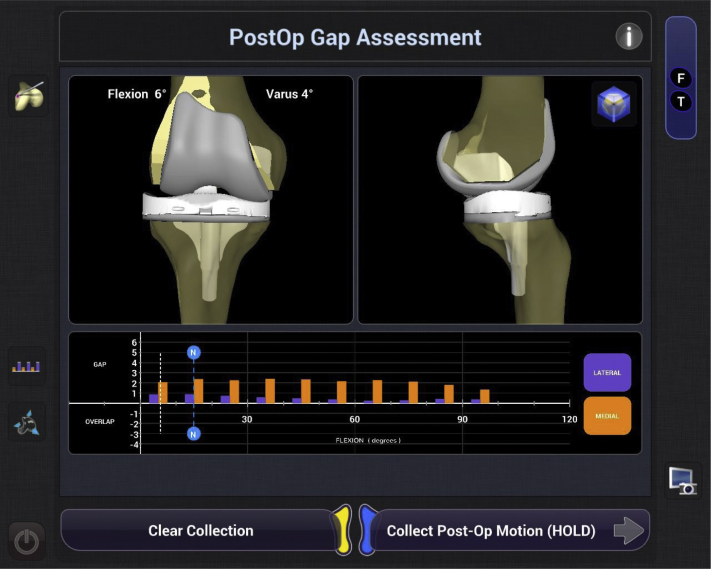
In this retrospective review, we identified 2 cohorts of patients who underwent a primary TKA by one surgeon at a single institution. The first cohort was patients who underwent conventional jig-based TKA (n = 49) between January 1, 2018, and December 10, 2018. For both cohorts, the standard medial mid-vastus approach was used in the manner routinely used by the senior author of the study. Surgical technique for the conventional jig-based TKA group consisted of measured resection using an anterior referencing system. Bone cut orientation is prepared using a combination of methods. For a varus knee, the senior author starts with 3° of external rotation based of the posterior condyles. This is then checked manually to ensure this is parallel to the transepicondylar axis. A final confirmation is undertaken by ensuring Whiteside’s line is perpendicular to the transepicondylar axis. The method holds true to a valgus knee, except the senior author prefers to start with 5° of external rotation compared to the posterior condylar axis because of the posterolateral condylar hypoplasia typically seen in this patient cohort. The second cohort was patients who underwent robot-assisted TKA in this same time period (n = 37). Robot-assisted TKA was performed using the NAVIO surgical system (Smith & Nephew, Memphis, TN). Surgical technique for the robot-assisted TKA cohort is also based off measured resection; however, it is more of a hybrid technique incorporating aspects of gap balancing, as it allows for intraoperative assessment of compartment gaps with fine adjustments using the robotic navigation. The robotic system allows for assessment of the joint intraoperatively through mapping of the articular surface, measurement of the mechanical axis, and measurement of soft tissue tension throughout the full range of motion of the knee (Fig. 1). Soft tissue tension, specifically laxity, is measured by applying varus and valgus stress to the knee as it is ranged and allows for the assessment of gap balancing in real time. A surgical plan for component selection and placement, as well as the required bony resection, is created and can be adjusted by the surgeon. Feedback on gap balancing is provided based on the surgical plan and the real-time modifications. In addition to being performed during planning, measurement of soft tissue tension can be repeated during the trialing phase and after soft tissue releases.
Figure 1.
Example of postreconstruction soft tissue/ligamentous tension with provisional components using imageless robot-assisted technology.
For both cohorts, either Journey II or Legion Posterior-Stabilized Primary Total Knee Systems were used (Smith & Nephew, Memphis, TN). Patients were excluded from both groups if Verasense (OrthoSensor Inc., Dania Beach, FL) was not used during the procedure. The senior surgeon used Verasense in his elective cases, and the data were collected prospectively for research purposes. The senior surgeon operates at multiple locations, and the decision to use Verasense was based on institutional site availability, not based on patient characteristics or deformity. In addition to compartment loads, demographic, intraoperative, and postoperative data were collected for each patient. Arc of motion of the operative knee was measured preoperatively and at 1, 3, and 12 months postoperatively by the senior arthroplasty surgeon and collected from the clinical documentation. Patient-reported outcome measures (PROMs) are collected prospectively at our institution for each patient undergoing arthroplasty surgery and stored in a single database. Patients are surveyed preoperatively and postoperatively at 3 months, 12 months, and then annually. Collected scores include the Short Form 12 Mental and Physical Scores; Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) divided into the subcategories pain (WOMAC P), stiffness (WOMAC S), and function (WOMAC F); and the functional score of the Knee Society Score.
Verasense was used during both implant trialing and after final implant insertion, but for the purposes of this study, only final implant insertion measurements were included. Verasense is a sensor that is inserted as a trial polyethylene, and it is removed before final polyethylene insertion. The sensor measures peak load at the tibiofemoral interface and is reported in pounds to the single digit [14]. Tibial rotation is typically oriented to the position of the tibial tubercle, with the anterior aspect of the tibial tray in line with the junction of the medial-middle third of the tibial tubercle. The tibial component is then rotationally aligned with the femoral component and finally confirmed to be within 5° of rotation of the Verasense trial insert. Medial compartment loads are then recorded with the knee in full extension (10° of flexion to unload the posterior capsule), mid-flexion (45°), and 90° flexion. Soft tissue releases were typically done during the trial phase to help achieve optimal ligament balance between the medial and lateral compartments. If pressures were elevated in the CM-TKA cohort, there was an attempt to improve them with soft tissue balance techniques. As for RA-TKA, a combination of both soft tissue releases and component position alteration was performed. Component position alterations could only be performed after trialing pressures, and not after final pressures. If necessary, final soft tissue balancing adjustments were made before final polyethylene liner insertion as well.
Before data analysis, the clinically important comparisons of compartment load measurements were determined. Identified measurements included mean difference in compartment loads (medial vs lateral) in extension, mid-flexion, and 90-degrees flexion; percentage of unbalanced compartments (>20 lbs difference between medial and lateral sides) in extension, mid-flexion, and 90-degrees flexion; percentage of cases with overstuffed compartments (>40 lbs of compartment pressure on either medial or lateral sides) in extension, mid-flexion, and 90-degrees flexion. Although there is still no gold standard for defining a balanced compartment, these clinically important measurements were defined according to prior studies [[15], [16], [17]]. For example, Gustke et al. observed significant declination in postoperative outcomes scores in patients with an intercompartmental loading difference which exceeded 20 lbs [15].
A power analysis revealed our sample size was powered to detect a difference of 5 lbs of compartment pressure between groups. Continuous measures such as mean difference in compartment pressure, arc of motion, and PROMs were compared using unpaired t-tests. Categorical measures such as percentage of patients with >40 lbs of compartment pressure and differences in implant design between the 2 groups were compared using chi-square analysis. Statistical significance was defined as P < .05.
Results
Demographics and intraoperative results
There was no significant difference in age, sex, or estimated intraoperative blood loss for the 2 patient cohorts (Table 1). Robot-assisted TKA resulted in significantly longer operative time (127 minutes vs 106 minutes, P < .001). The number of Journey II and Legion implants was not significantly different between the 2 groups (Table 2).
Table 1.
Patient demographics and intraoperative results.
| Preoperative demographics and intraoperative results | Conventional TKA (n = 49) | Robotic TKA (n = 37) | P value |
|---|---|---|---|
| Age (years) | 73 ± 8 | 71 ± 9 | .62 |
| Gender, F (%) | 77% | 73% | .51 |
| Operative time (minutes) | 106 ± 18 | 127 ± 20 | <.001 |
| Estimated blood loss (milliliters) | 233 ± 85 | 264 ± 59 | .06 |
Values are given as mean ± standard deviation or percentile.
Table 2.
Implant design by technique.
| Implant design | Conventional TKA |
Robotic TKA |
P value |
|---|---|---|---|
| Conventional | Robotically assisted | ||
| Journey II | 31 | 25 | .679 |
| Legion | 18 | 12 |
Compartment load
The mean difference in compartment loads (absolute value of lateral minus medial side) for the conventional TKA cohort in extension, mid-flexion, and 90° flexion was 15.1 ± 15.3 lbs, 15.9 ± 16.2 lbs, and 13.4 ± 15.6 lbs, respectively. The mean difference in compartment load for the robotic TKA cohort was 14.2 ± 8.9 lbs (P = .54), 15.1 ± 15.2 lbs (P = .96), and 10.3 ± 6.4 lbs (P = .52) (Table 3).
Table 3.
Differences in compartment pressure between conventional and robot-assisted TKA.
| Surgical technique | Mean difference in compartment pressure (lbs)a |
Percentage of unbalanced kneesb |
Percentage of overstuffed compartmentsc |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Extension | Mid-flexion | Flexion | Extension | Mid-flexion | Flexion | Extension | Mid-flexion | Flexion | |
| Conventional TKA (n = 49) | 15.1 ± 15.3 | 15.9 ± 16.2 | 13.4 ± 15.6 | 35% | 35% | 24% | 20% | 18% | 18% |
| Robotic TKA (n = 37) | 14.2 ± 8.9 | 15.1 ± 15.2 | 10.3 ± 6.4 | 27% | 24% | 5%d | 24% | 19% | 3%d |
Values are given as mean ± standard deviation or percentile.
Absolute value of lateral minus medial side compartment pressure.
>20 lbs absolute value difference between medial and lateral side.
>40 lbs of compartment pressure on medial or lateral side.
P value < .05 compared with conventional TKA.
The percentage of unbalanced knees (>20 lbs difference between medial and lateral side) in extension, mid-flexion, and 90° flexion in the conventional TKA cohort was 35%, 35%, and 24%, respectively. The percentage of unbalanced knee in the robotic TKA cohort was 27% (P = .56), 24% (P = .56), and 5% (P = .028).
The percentage of cases with overstuffed compartments (>40 lbs of compartment load) in extension, mid-flexion, and 90° flexion in the conventional TKA cohort was 20%, 18%, and 18%, respectively. The percentage of cases with overstuffed compartments in the robotic TKA cohort was 24% (P = .96), 19% (P = .92), and 3% (P = .024).
Arc of motion and patient-reported outcome measures
Arc of motion was not significantly different between the 2 groups preoperatively, at 1, 3, or 12 months postoperatively (Table 4). Only the Short Form 12 Mental score at 12 months postoperatively was significantly lower in the robotically assisted vs conventional group (49.28 vs 44.13, P = .004). Otherwise, there were not statically significant differences between the 2 groups (Table 5).
Table 4.
A comparison of total arc of motion between technique.
| Followup visit | Arc of motion (degrees) |
P value | |
|---|---|---|---|
| Conventional | Robotically assisted | ||
| Preoperative | 109 ± 14 | 112 ± 11 | .310 |
| 1 mo | 100 ± 11 | 97 ± 15 | .360 |
| 3 mo | 114 ± 11 | 116 ± 9 | .362 |
| 12 mo | 117 ± 11 | 121 ± 9 | .212 |
Table 5.
Patient-reported outcome measures by technique.
| Patient-reported outcome measures | Patient-reported outcome measures |
P value | |
|---|---|---|---|
| Conventional | Robotically assisted | ||
| SF-12 P | |||
| Preoperative | 37.93 ± 8.1 | 39.21 ± 7.2 | .491 |
| 3 mo | 43.40 ± 8.7 | 43.34 ± 5.9 | .979 |
| 12 mo | 44.31 ± 5.4 | 46.69 ± 6.0 | .102 |
| SF-12 M | |||
| Preoperative | 49.25 ± 5.8 | 47.93 ± 7.7 | .407 |
| 3 mo | 47.02 ± 8.0 | 48.05 ± 6.8 | .606 |
| 12 mo | 49.28 ± 5.3 | 44.13 ± 8.3 | .004a |
| WOMAC P | |||
| Preoperative | 46.28 ± 21.3 | 45.36 ± 25.4 | .872 |
| 3 mo | 73.78 ± 21.0 | 79.77 ± 14.3 | .242 |
| 12 mo | 82.43 ± 19.9 | 86.43 ± 12.6 | .360 |
| WOMAC S | |||
| Preoperative | 40.66 ± 19.7 | 47.32 ± 23.9 | .219 |
| 3 mo | 64.47 ± 19.8 | 63.07 ± 14.7 | .773 |
| 12 mo | 68.38 ± 23.7 | 74.07 ± 19.0 | .314 |
| WOMAC F | |||
| Preoperative | 42.93 ± 20.5 | 44.39 ± 17.8 | .764 |
| 3 mo | 70.67 ± 19.8 | 74.94 ± 11.6 | .360 |
| 12 mo | 75.42 ± 19.0 | 78.73 ± 23.0 | .534 |
| KSS-FS | |||
| Preoperative | 50.49 ± 20.3 | 45.00 ± 23.3 | .295 |
| 3 mo | 58.42 ± 24.6 | 55.23 ± 16.5 | .590 |
| 12 mo | 64.71 ± 19.4 | 66.67 ± 20.1 | .701 |
KSS-FS, functional score of Knee Society Score; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
Denotes statistical significance (P < .05).
Discussion
Robot-assisted TKA has the potential to improve surgical accuracy, which may lead to improved outcomes. Although improved coronal and sagittal balance did not prove to have an effect on satisfaction rates after TKA, it became clearer that soft tissue balance could play a more significant role. Balancing intracompartmental loads may prove to be a critical aspect of TKA as it has already shown to effect patient satisfaction, function, and implant survival. To date, no studies have examined the effect of robot-assisted TKA with this system on knee ligament balancing. In this study, we found that robot-assisted TKA resulted in similar intraoperative compartment balancing in extension but much improved flexion balancing. Specifically, we identified more symmetric medial and lateral compartments and a lower rate of overstuffing in flexion for robot-assisted TKA than conventional TKA.
The use of robot-assisted TKA is still controversial, and surgeons must balance the positives and negatives compared to manual TKA. The first generation of robot-assisted surgery demonstrated significantly improved alignment and joint line restoration [[10], [11], [12]]. Compared with jig-based TKA, most studies show robotic TKA results in more accurate implant placement and more reliable restoration for the mechanical axis [12]. Critics report that these minor advantages in surgical accuracy do not correlate with improved clinical outcomes or lower complication rates. In fact, some studies have shown higher complication rates in this group, such as pin site fracture, as well increased operating room time [11,18]. Indeed, our study showed increased operative time with robot-assisted TKA. In addition, robot-assisted TKA is associated with significantly increased costs [19]. In the setting of bundled payments and rising health-care costs, expensive technologies with little benefit must be considered with caution.
The newer generation of robots may have potential advantages not seen in the older models. Current robot-assisted TKA allows for dynamic assessment of soft tissues over the full range motion. With these models, there is some evidence for superior outcomes, including more accurate ligament balancing, in UKA with robot assisted vs conventional surgery [20,21]. We hypothesized, given the newer dynamic assessment abilities of robotic models, robot-assisted TKA would lead to similar improved compartmental balancing, as measured through compartment loads. There are a number of modalities for measuring balancing in TKA. Traditionally, surgeons relied on qualitative assessments, such as manual feedback and gross visualization, to assess balancing. More quantifiable methods include measuring gapping (in mm) through a tensioning device. In this study, we measured compartment loads using Verasense, which can be used for both clinical guidance and quantitative measurement [15,22]. By giving us actual measurements in pounds for both the medial and lateral compartment throughout knee range of motion, this allowed to systematically assess compartment balancing from extension to flexion.
We are the first study to compare the effects of robotic vs traditional TKA on compartment loads and balancing. Overall, we saw similar compartment balancing in extension and mid-flexion but improved balancing at 90° flexion, when using robot-assisted TKA. The robotic group had significantly lower rates of compartment loads >40 lbs in flexion, a potentially clinically significant cutoff for overstuffing [17,23,24]. In addition, the robot-assisted group had more symmetrically balanced compartments in flexion (<20 lbs difference between sides) than the nonrobotic side. Interestingly, in terms of balance and overstuffing, the use of robotics only showed advantage in full flexion, not in extension and mid-flexion. The reasons for this remain unclear, but we hypothesize it could be influenced by the specific robotic balancing algorithm and the single surgeon’s preferences on fine-tuning component positioning using the robotic system. This is an area of future investigation to see if the same pattern holds true when multiple surgeons are included. Flexion instability has been recognized as a significant and increasing cause of early TKA failure and cause for revision [3]. Robotic feedback in producing appropriately aligned bone cuts, as well as real-time dynamic soft tissue assessment, likely contributed to these improved balancing findings. In addition, the more accurate alignment, particularly precise joint line preservation, may likely have led to the isolated finding of more balanced flexion gaps.
This study is not without limitations. First, while a number of studies have shown significant correlations between successful balancing and improved postoperative outcomes in TKA [[2], [3], [4],25], we cannot draw these conclusions from this study. This study was unique because we had the opportunity to quantifiably measure balancing through an intraoperative pressure sensor. However, improvements in outcomes, such as patient satisfaction, are the ultimate goal, and we failed to show meaningful differences at 1-year follow-up. Second, the degree and type of preoperative deformity can influence compartmental pressures. However, to determine the role of deformity, severity, and soft tissue releases on pressure differences, larger sample sizes would be needed. In this study, we did not have that sample size availability. Third, while the goal was to attain the acceptable pressure parameters, these were not always achieved and could be left based on clinical feel and decision-making. Overall, balancing can be more an art than a science, and it is often surgeon dependent on how far to go, which is a limitation of this study. Fourth, although a 20lb intercompartmental differential has been shown to significantly effect outcomes in a single study, other studies have not confirmed and validated this differential and its effect on PROMs. Also, while this study showed differences in absolute values of target loads, these are not validated measures and can vary by patient, thus cannot reliably predict outcomes. Fifth, although compartmental load measurements were performed in a standardized fashion, it should be noted that variability in flexion angle and the rotational position of the leg can affect the observed values.
In addition, the present study was not a randomized clinical trial, and instead was a cohort study based on robotic knee availability at our surgical sites. While all TKAs were performed by the same surgeon, in the same time period, using the same preoperative and intraoperative protocols, there is always potential for confounding in a nonrandomized study. Finally, our sample size, particularly for the robot-assisted group, was not large and was limited to one surgeon. However, given this is a unique patient population (robot-assisted TKA + compartment pressure sensing device), we felt there was significant value in studying these patients, and we were indeed able to achieve statistical significance with our sample size.
Conclusion
Compartmental balancing throughout knee range of motion is a critical component to a successful TKA. In this study, we found that robot-assisted TKA results in improved intraoperative compartment flexion balancing vs traditional TKA, at the expense of increased operative time. Further studies are needed to help determine if improved intraoperative compartment balancing with robot-assisted surgery leads to improved clinical outcomes and implant survivorship.
Conflict of Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Jeffrey A. Geller is a paid consultant for Smith & Nephew, Inc.
For full disclosure statements refer to https://doi.org/10.1016/j.artd.2020.12.022.
Supplementary data
References
- 1.Gunaratne R., Pratt D.N., Banda J. Patient dissatisfaction following total knee arthroplasty: a systematic review of the literature. J Arthroplasty. 2017;32(12):3854. doi: 10.1016/j.arth.2017.07.021. [DOI] [PubMed] [Google Scholar]
- 2.Fehring T.K., Odum S., Griffin W.L., Mason J.B., Nadaud M. Early failures in total knee arthroplasty. Clin Orthop Relat Res. 2001;(392):315. doi: 10.1097/00003086-200111000-00041. [DOI] [PubMed] [Google Scholar]
- 3.Sharkey P.F., Hozack W.J., Rothman R.H., Shastri S., Jacoby S.M. Insall Award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;(404):7. doi: 10.1097/00003086-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Whiteside L.A., Saeki K., Mihalko W.M. Functional medical ligament balancing in total knee arthroplasty. Clin Orthop Relat Res. 2000;(380):45. doi: 10.1097/00003086-200011000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Krackow K.A., Mihalko W.M. The effect of medial release on flexion and extension gaps in cadaveric knees: implications for soft-tissue balancing in total knee arthroplasty. Am J Knee Surg. 1999;12(4):222. [PubMed] [Google Scholar]
- 6.Bellemans J., Vandenneucker H., Van Lauwe J., Victor J. A new surgical technique for medial collateral ligament balancing: multiple needle puncturing. J Arthroplasty. 2010;25(7):1151. doi: 10.1016/j.arth.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 7.Bozic K.J., Kurtz S.M., Lau E. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res. 2010;468(1):45. doi: 10.1007/s11999-009-0945-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rodriguez-Merchan E.C. Instability following total knee arthroplasty. Hss j. 2011;7(3):273. doi: 10.1007/s11420-011-9217-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lombardi A.V., Jr., Berend K.R., Adams J.B. Why knee replacements fail in 2013: patient, surgeon, or implant? Bone Joint J. 2014;96-B(11 Supple A):101. doi: 10.1302/0301-620X.96B11.34350. [DOI] [PubMed] [Google Scholar]
- 10.Song E.K., Seon J.K., Yim J.H., Netravali N.A., Bargar W.L. Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop Relat Res. 2013;471(1):118. doi: 10.1007/s11999-012-2407-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park S.E., Lee C.T. Comparison of robotic-assisted and conventional manual implantation of a primary total knee arthroplasty. J Arthroplasty. 2007;22(7):1054. doi: 10.1016/j.arth.2007.05.036. [DOI] [PubMed] [Google Scholar]
- 12.Liow M.H., Xia Z., Wong M.K., Tay K.J., Yeo S.J., Chin P.L. Robot-assisted total knee arthroplasty accurately restores the joint line and mechanical axis. A prospective randomised study. J Arthroplasty. 2014;29(12):2373. doi: 10.1016/j.arth.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 13.Shalhoub S., Lawrence J.M., Keggi J.M., Randall A.L., DeClaire J.H., Plaskos C. Imageless, robotic-assisted total knee arthroplasty combined with a robotic tensioning system can help predict and achieve accurate postoperative ligament balance. Arthroplast Today. 2019;5(3):334. doi: 10.1016/j.artd.2019.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walker P.S., Meere P.A., Bell C.P. Effects of surgical variables in balancing of total knee replacements using an instrumented tibial trial. Knee. 2014;21(1):156. doi: 10.1016/j.knee.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 15.Gustke K.A., Golladay G.J., Roche M.W., Elson L.C., Anderson C.R. A new method for defining balance: promising short-term clinical outcomes of sensor-guided TKA. J Arthroplasty. 2014;29(5):955. doi: 10.1016/j.arth.2013.10.020. [DOI] [PubMed] [Google Scholar]
- 16.Gustke K.A., Golladay G.J., Roche M.W., Elson L.C., Anderson C.R. Primary TKA patients with quantifiably balanced soft-tissue achieve significant clinical gains sooner than unbalanced patients. Adv Orthop. 2014;2014:628695. doi: 10.1155/2014/628695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anderson C., Roche M., Golladay G., Elson L. Bony cuts or soft-tissue release? Using intra-operative sensors to refine balancing techniques in TKA. Orthop Proc. 2016;98-B(SUPP_1):16. [Google Scholar]
- 18.Bellemans J., Vandenneucker H., Vanlauwe J. Robot-assisted total knee arthroplasty. Clin Orthop Relat Res. 2007;464:111. doi: 10.1097/BLO.0b013e318126c0c0. [DOI] [PubMed] [Google Scholar]
- 19.Moschetti W.E., Konopka J.F., Rubash H.E., Genuario J.W. Can robot-assisted unicompartmental knee arthroplasty be cost-effective? A Markov decision analysis. J Arthroplasty. 2016;31(4):759. doi: 10.1016/j.arth.2015.10.018. [DOI] [PubMed] [Google Scholar]
- 20.Plate J.F., Mofidi A., Mannava S. Achieving accurate ligament balancing using robotic-assisted unicompartmental knee arthroplasty. Adv Orthop. 2013;2013:837167. doi: 10.1155/2013/837167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bell S.W., Anthony I., Jones B., MacLean A., Rowe P., Blyth M. Improved accuracy of component positioning with robotic-assisted unicompartmental knee arthroplasty: data from a prospective, randomized controlled study. J Bone Joint Surg Am. 2016;98(8):627. doi: 10.2106/JBJS.15.00664. [DOI] [PubMed] [Google Scholar]
- 22.Herschmiller T., Grosso M.J., Cunn G.J., Murtaugh T.S., Gardner T.R., Geller J.A. Step-wise medial collateral ligament needle puncturing in extension leads to a safe and predictable reduction in medial compartment pressure during TKA. Knee Surg Sports Traumatol Arthrosc. 2018;26(6):1759. doi: 10.1007/s00167-017-4777-2. [DOI] [PubMed] [Google Scholar]
- 23.Elmallah R.K., Mistry J.B., Cherian J.J. Can we really “feel” a balanced total knee arthroplasty? J Arthroplasty. 2016;31(9 Suppl):102. doi: 10.1016/j.arth.2016.03.054. [DOI] [PubMed] [Google Scholar]
- 24.Gustke K.A. Soft-tissue and alignment correction: the use of smart trials in total knee replacement. Bone Joint J. 2014;96-b(11 Supple A):78. doi: 10.1302/0301-620X.96B11.34339. [DOI] [PubMed] [Google Scholar]
- 25.Mihalko W.M., Miller C., Krackow K.A. Total knee arthroplasty ligament balancing and gap kinematics with posterior cruciate ligament retention and sacrifice. Am J Orthop (Belle Mead NJ) 2000;29(8):610. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.