Abstract
Bow Hunter's syndrome, also referred to as rotational occlusion of the vertebral artery, is caused by dynamic compression of a patient's dominant vertebral artery. We reported a case of successful clinical and imaging work up of Bow Hunter's Syndrome that occurred in a 79-year-old female patient. We discussed the clinical presentation, imaging findings, and subsequent management options of this rare syndrome. The gold standard for diagnosis is dynamic cerebral angiography, which allows the reproduction of symptoms with head turn greater than 30-45 degrees. Subsequent management is based on the underlying etiology causing rotational compression.
Keywords: Bow hunter syndrome, Positional vertebrobasilar insufficiency, Rotational occlusion of the vertebral artery
Case summary
Bow Hunter's syndrome, also known as rotational occlusion of the vertebral artery, is caused by dynamic compression of a patient's dominant vertebral artery. This results in vertebrobasilar insufficiency, and may lead to permanent neurological deficits. It may occur anywhere along the course of the vertebral artery, but the C1-C2 level is particularly prone to compression. Etiologies include, but are not limited to, large osteophytes, an aberrant vertebral artery, fascial bands of paravertebral musculature or atlantoaxial hypermobility. The name Bow Hunter's Syndrome came from the significance of the stance when bow hunting, which forces rotation of the head in one direction to stabilize the arrow.
A 79-year-old female patient presented for evaluation after referral from an outside institution. For the past few months, she had felt as though she would pass out whenever she turned her head to the left. Within seconds of turning her head leftward, she would experience lightheadedness, a ringing in her ears, and darkening of her vision. This would resolve almost immediately on return of her head to neutral position. She denied stroke-like symptoms, such as weakness, numbness, difficulty with speech, or other visual changes. Additional reported symptoms were intermittent bilateral upper extremity pain, chronic headaches and osteoarthritis. The patient's past medical history included hypertension, hyperlipidemia, and osteoporosis; she had no relevant past surgical history. The only relevant family history was that her mother had a stroke. Her social history included never smoking, socially drinking, and no drug use.
On initial evaluation, her vital signs were within normal limits and stable. During the physical examination, the neurologic and cranial nerve portion specifically were within normal limits. However, cervical spine evaluation elicited the patient's presenting complaints of abrupt lightheadedness and darkening vision during left head turning. No nystagmus was observed during these episodes. Based on this initial workup, a multidisciplinary evaluation was conducted involving neurology and vascular neurosurgery.
An initial carotid ultrasound revealed 16%-49% stenoses within the bilateral carotid arteries and antegrade Doppler flow present in the bilateral vertebral arteries. A subsequent CT angiogram of the head and neck (Fig. 1) demonstrated a hypoplastic right vertebral artery, most notably along the V4 segment, and a dominant left vertebral artery, which comparatively was approximately three-fold larger in caliber. Based on these initial imaging findings, neurosurgery recommended evaluation with dynamic provocative cerebral angiography (Fig. 2). This procedure showed nearly 100% stenosis of the left vertebral artery at the C4-C5 level with the patient's head turned to the left. In comparison, the left vertebral artery remained widely patent with the patient's head in neutral position.
Fig. 1.
Axial (A) and coronal (B) CT angiogram of the head and neck show a patent but hypoplastic right vertebral artery along the V4 segment (white arrow). The left vertebral artery (white circle) is dominant, with a diameter approximately three times the size of the right.
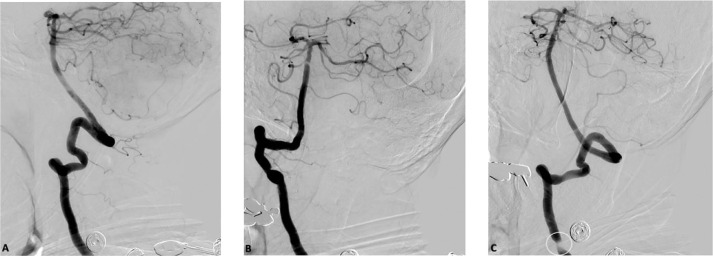
Fig. 2.
Diagnostic provocative cerebral angiogram shows the left vertebral artery with the head positioned straight (A), turned to the right (B) and turned to the left (C). There is complete patency of the left vertebral artery with the head positioned straight and turned to the right. However, there is 100% stenosis of the left vertebral artery at the level of C4-C5 (white circle) with the patient's head turned to the left.
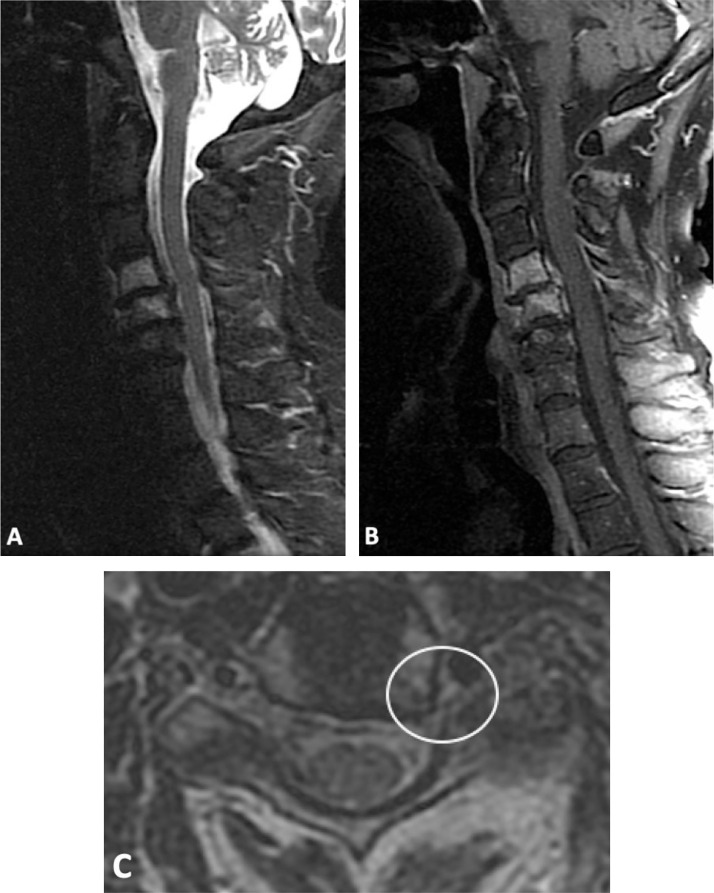
When the patient turned her head to the left, the dominant left vertebral artery was dynamically but reversible stenosed at the C4-5 level, resulting in presenting symptoms of vertebrobasilar insufficiency consistent with Bow Hunter Syndrome (BHS). She underwent an MRI of the cervical spine to further elucidate an underlying etiology (Fig. 3). The MRI detected chronic degenerative changes at C4-5 through C6-7, with significant facet hypertrophy at C4-5 and associated spondylolisthesis. After consideration of the clinical and imaging findings, neurosurgery recommended cervical spine decompression at C4-5 with anterior cervical discectomy and fusion. Currently, the patient is considering surgery but, in the meantime, is avoiding rotational head movement leftward so as to not induce her symptoms.
Fig. 3.
Sagittal T2 STIR (A) and sagittal T1 fat-saturated contrast-enhanced (B) images of the cervical spine show hyperintense marrow signal and enhancement of the C4 and C5 vertebral bodies, consistent with active bone marrow edema and advanced osteoarthritis. Axial T2 (C) imaging is shown through the level of the C5 exiting nerve roots. There is severe left neural foraminal stenosis causing impingement of the exiting C5 nerve root (white circle) secondary to degenerative osteoarthritis.
Discussion
This case report highlights a rare case of vertebrobasilar insufficiency due to underlying dynamic stenosis of the vertebral artery during neck rotation of greater than 30-45 degrees. Within the literature, descriptions of BHS are limited to case reports due to the rarity of the diagnosis. The exact etiology can be divided into primary versus acquired causes. Primary etiologies include anatomic compression from osteophytes/bone spurs (most common), idiopathic skeletal hyperostosis, cervical spondylosis, disc herniation, fibrous bands, neck muscle hypertrophy, intrinsic vascular disease (such as vertebral artery dissection or atherosclerosis), or tumors. Acquired etiologies include complications from cervical spine surgery and head/neck trauma/injury [4,6,10,15]. Our case demonstrated reversible dynamic compression of a dominant left vertebral artery with leftward head turn on the basis of underlying cervical spinal degenerative changes at C4-5.
The vertebral arteries course caudally through the transverse foramina of the cervical spine vertebra, entering at the C6 level and exiting at the C1 level. According to the literature, BHS is most commonly observed at or above C2. The left vertebral artery is more commonly involved, with a higher likelihood of symptoms occurring when the left vertebral artery is dominant [8,16]. Typical presentation of symptoms occurs during the 5th to 7th decade of life with a high male predominance [2,3,7,11]. Our case is atypical, as our patient is female and presents in almost her 8th decade, although her left vertebral artery is dominant and is the side that elicits symptoms on rotation. General symptoms described in the literature include transient vertigo, nausea, dysarthria, dysphagia, transient blurred vision, gait disturbances, and headaches. One significant risk due to the repetitive decrease in distal flow and/or vessel wall injury is thromboembolism with potentially posterior circulation strokes [4,7,9].
Imaging plays an instrumental role in confirming the clinician's suspected diagnosis of BHS. It is important to note, however, that standard noninvasive neurovascular imaging does not always exclude the diagnosis. The gold standard for diagnosis remains a provocative cerebral angiogram, wherein the patient is able to reproduce or exacerbate symptoms with neck rotation [14,16]. Neutral and rotated positionings are utilized for comparison [5,8]. As cerebral angiography is invasive, a risk/benefit discussion with the patient is required before proceeding. CT/MR angiography and transcranial Doppler ultrasound are noninvasive tests that can provide additional evidence in support of the diagnosis or other diagnostic considerations [1,5]. The differential diagnosis also includes vertebral artery occlusion, atlantoaxial subluxation, and subclavian steal phenomenon.
Once a diagnosis of BHS has been established, treatment options include conservative and/or surgical management. Conservative approaches include prolonged head/neck nonrotation and anticoagulation. However, surgery appears to be the preferred approach in the literature, specifically decompression with or without fusion, with favorable outcomes documented, [8,12]. Intraoperative angiography allows for real time visualization and assessment of the adequacy of the surgical intervention [5,13]. Overall, there is no standard option due to the rarity of cases and a literature largely comprised of case reports. However, the combination of clinical presentation, imaging work-up, and subsequent management allows for a multidisciplinary approach to BHS, as well demonstrated with our case.
Patient consent statement
Written, informed consent for publication was obtained from the patient.
Footnotes
Financial support: None.
Competing Interest: There are no conflicts of interest.
References
- 1.Anaizi A.N., Sayah A., Berkowitz F., McGrail K. Bow hunter's syndrome: the use of dynamic magnetic resonance angiography and intraoperative fluorescent angiography. J Neurosurg Spine. 2014;20:71–74. doi: 10.3171/2013.9.SPINE121019. [DOI] [PubMed] [Google Scholar]
- 2.Bulsara K.R., Velez D.A., Villavicencio A. Rotational vertebral artery insufficiency resulting from cervical spondylosis: case report and review of the literature. Surg Neurol. 2006;65:625–627. doi: 10.1016/j.surneu.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 3.Cai D.Z., Roach R.P., Weaver J.P. Bow Hunter's syndrome in a patient with a right hypoplastic vertebral artery and a dynamically compressible left vertebral artery. Asian J Neurosurg. 2018;13(1):133–135. doi: 10.4103/1793-5482.181129. Jan-Mar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choi K.D., Choi J.H., Kim J.S., Kim H.J., Kim M.J., Lee T.H. Rotational vertebral artery occlusion: mechanisms and long-term outcome. Stroke. 2013;44:1817–1824. doi: 10.1161/STROKEAHA.113.001219. [DOI] [PubMed] [Google Scholar]
- 5.Ding D., Mehta G.U., Medel R., Liu K.C. Utility of intraoperative angiography during subaxial foramen transversarium decompression for bow hunter's syndrome. Interv Neuroradiol. 2013;19:240–244. doi: 10.1177/159101991301900215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duan G., Xu J., Shi J., Cao Y. Advances in the pathogenesis, diagnosis and treatment of Bow Hunter's syndrome: a comprehensive review of the literature. Intervent Neurol. 2016;5:29–38. doi: 10.1159/000444306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gordhan A., Lockhart C. Congenital bilateral C2 transverse foramina stenosis causing adult-onset vertebrobasilar insufficiency and posterior circulation stroke. Case Rep Neurol. 2017;9(2):137–142. doi: 10.1159/000476031. May 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hasan A., Zaidi Felipe C., Albuquerque Shakeel A., Chowdhry Joseph M., Zabramski Andrew F., Ducruet Robert F.S. Diagnosis and management of Bow Hunter's syndrome: 15-year experience at barrow neurological institute. World Neurosurg. 2014;82(5):733–738. doi: 10.1016/j.wneu.2014.02.027. November. [DOI] [PubMed] [Google Scholar]
- 9.Jadeja N., Nalleballe K. Pearls & Oy-sters: Bow Hunter syndrome: a rare cause of posterior circulation stroke: do not look the other way. Neurology. 2018;91(7):329–331. doi: 10.1212/WNL.0000000000006009. Aug 14. [DOI] [PubMed] [Google Scholar]
- 10.Jost G.F., Dailey A.T. Bow hunter's syndrome revisited: 2 new cases and literature review of 124 cases. Neurosurg Focus. 2015;38:E7. doi: 10.3171/2015.1.FOCUS14791. [DOI] [PubMed] [Google Scholar]
- 11.Liu X., Zhao J. Pay attention to the diagnosis and management of bow hunter’s syndrome. World Neurosurg. 2004;82(5):593–594. doi: 10.1016/j.wneu.2014.04.073. [DOI] [PubMed] [Google Scholar]
- 12.Ng S., Boetto J., Favier V., Thouvenot E., Costalat V., Lonjon N. Bow Hunter's syndrome: surgical vertebral artery decompression guided by dynamic intraoperative angiography. World Neurosurg. 2018;118:290–295. doi: 10.1016/j.wneu.2018.07.152. Oct. [DOI] [PubMed] [Google Scholar]
- 13.Nguyen H.S., Doan N., Eckardt G., Pollock G. Surgical decompression coupled with diagnostic dynamic intraoperative angiography for bow hunter's syndrome. Surg Neurol Int. 2015;6:147. doi: 10.4103/2152-7806.165173. Sep 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Park J.H., Ihn Y.K., Hong J.T. Significance of provocative perfusion computed tomography for evaluation of Bow Hunter syndrome. World Neurosurg. 2019;121:1–3. doi: 10.1016/j.wneu.2018.09.107. Jan. [DOI] [PubMed] [Google Scholar]
- 15.Rastogi V., Rawls A., Moore O., Victoria B., Khan S., Saravanapavan P. Rare Etiology of Bow Hunter's Syndrome and Systematic Review of Literature. J Vasc Interv Neurol. 2015;8(3):7–16. Jul. [PMC free article] [PubMed] [Google Scholar]
- 16.Xue S., Shi H., Du X., Ma X. Bow Hunter's syndrome combined with ipsilateral vertebral artery dissection/pseudoaneurysm: case study and literature review. Br J Neurosurg. 2020:1–5. doi: 10.1080/02688697.2020.1718604. Feb 3. [DOI] [PubMed] [Google Scholar]