Abstract
Introduction
Diabetes related distress is the most common psychological co-morbid condition among type 2 diabetes patients. However, although the number of people living with diabetes has continued to increase over the last 10 years, information regarding diabetes related distress is limited in Ethiopia.
Objective
The present study aimed to assess the prevalence of diabetes related distress and associated factors among type 2 diabetes patients attending hospitals in Southwest Ethiopia.
Methods
A cross-sectional study was employed on 360 type 2 diabetes patients attending hospitals from January 1 to March 30, 2020. Convenient sampling technique was used to select study participants. Data were entered into EpiData manager version 4.2.2 and exported to Statistical Package for the Social Sciences (SPSS) version 20.0 and analyzed using descriptive statistics, bivariate and multivariate logistic regressions. The statistical significance was set at P < 0.05.
Results
Out of a total 360 patients recruited, 321 (89.2%) patients (201 male and 120 female) were involved in the study. The mean age of the participants was 41.3 (SD = 12.8) years. The prevalence of diabetes related distress was 118 (36.8%) in which emotional distress was the most prevalent (43.6%) domain. Level of education [AOR 4.55; 95% CI: 1.28–16.19], family or social support [AOR 0.62; 95% CI: 0.33–1.06], duration of diabetes [AOR 0.75; 95% CI: 0.35–1.55], having diabetes complications [AOR 1.98; 95% CI: 1.0–3.86], smoking status [AOR 1.6; 95% CI: 1.12–2.97] and alcohol consumption status [AOR 1.4; 95% CI: 1.07–2.53] were the identified factors of diabetes related distress.
Conclusion
Diabetes related distress was highly prevalent in type 2 diabetes patients. Healthcare providers need to address this through integrating psychosocial care with collaborative medical care.
Keywords: diabetes mellitus, diabetes distress, prevalence, associated factors
Introduction
Type 2 diabetes mellitus (T2DM) is a leading cause of non-traumatic amputations, blindness, stroke, and end-stage renal disease.1,2 These can be prevented or delayed by strict adherence to prescribed medications and a variety of self-management behaviors. Many people with T2DM may become emotionally overwhelmed, frustrated, and discouraged by the threat of developing complications and the challenges of the complicated set of self-care activities.3 This condition is termed diabetes related distress (DRD). DRD is defined as patients’ negative emotional reactions to the diagnosis, the threat of complications, self-management, and concerns about support and access to care.3,4 It encompasses four domains including regimen related distress, emotional distress, physical related distress, and interpersonal distress.5,6
Diabetes related distress is distinctively different from depression, which is not disease-specific or context-specific to diabetes care. It is considered as a risk factor for depression, a condition associated with increased risks of diabetes related morbidity and mortality.7 Previous studies showed that DRD could progress to depression or a more severe form of emotional distress.3,4,8,9 Although depression and DRD are associated conditions, research has found that diabetes distress is more prevalent than depression.10 In addition, DRD has a greater impact on biomedical outcomes than depression.5
Diabetes related distress is the most common psychological co-morbid condition among patients with type 2 diabetes mellitus.11 Recent meta-analysis studies demonstrated that 36%5 and 22%12 of people with T2DM experience DRD. Other recent studies found that 49.2%,13 42.15%,14 25%, and 22.3%15 of patients with T2DM had DRD. A single study conducted in Northern Ethiopia found that 37.6% of type 2 diabetic patients had high DRD.16 Although burden of illness is a key contributor to DRD, presence of diabetes complications, co-morbid medical conditions, and more intensive treatment have been associated with increased DRD.17,18 Studies illustrated that younger age, lower level of education, longer duration of diabetes, use of insulin injection, and higher HbA1c were factors strongly associated with higher DRD in the cross-sectional analyses.19–21
High levels of DRD have been found to be a significant contributor to low levels of physical activity and non-adherence to diet and prescribed medications which in turns leads to poor glycemic control.22,23 When compared with patients with diabetes alone, patients with diabetes and co-morbid DRD have poorer glycemic control.24 Uncontrolled glycemia is also associated with various serious complications including heart disease, stroke, blindness, kidney failure, and lower-limb amputation.1,2 Moreover, adults with both DRD and diabetes are more likely to have poorer self-management behaviors and a higher risk of morbidity and mortality than those with only diabetes.5,25,26 However, DRD can be effectively treated using behavioral techniques to improve both psychological well-being and diabetes related health outcomes. Studies have found that people with a high level of diabetes empowerment have lower DRD than those with a low level of diabetes empowerment.27,28 In addition, high levels of social support are associated with reduced psychosocial problems in people with T2DM, particularly with low levels of DRD.29,30
In general addressing DRD improves diabetes self-care, glycemic control, diabetes self-efficacy, and quality of life.31,32 It is therefore imperative to assess DRD among people living with diabetes mellitus (PWD) early and intervene in a timely manner. However, a systematic review of studies on T2DM in Sub-Saharan Africa reported a lack of studies on the psychosocial aspect of diabetes.33 Similarly, although the number of people living with diabetes has continued to increase over the last 10 years,1 information regarding DRD is limited in Ethiopia. In addition, less is known about the factors that contribute to DRD and which could be targeted for intervention in the country. Therefore, the present study aimed to assess the prevalence of DRD and associated factors among type 2 diabetes patients attending hospitals in Southwest Ethiopia.
Methods
Study Area and Period
The study was conducted in Ilu AbaBor and Bunno Bedelle zones, Oromia Regional state, Southwest Ethiopia. Ilu AbaBor zone is one of the 20 zones of Oromia regional state situated in the southwest of the region and located at a distance of about 650 km from the center of the country. Two hospitals, namely Mettu Karl hospital and Darimu hospital, are found in the zone. Mettu Karl hospital is the only referral hospital in the zone and serves as a referral hospital for the zone and adjacent regional states. It also serves as a training hospital for health sciences, medical interns and masters of emergency surgery students from different universities. Darimu hospital, which is the only district hospital in the zone, serves the people of Darimu town and surrounding rural kebeles and districts. Bunno Bedelle is another Oromia regional state zone situated in the southwest of the region and located at a distance of about 500 km from Addis Ababa, the capital city of the country. Bedelle hospital and Didhessa hospital are the two district hospitals found in the zone, serving the population of the zone and adjacent districts. Both hospitals have serve as training hospitals for health science students from different universities. The study period spanned from January 1 to March 30, 2020.
Study Design
An institution-based cross-sectional study design was conducted.
Source Population
The source population of the study was all type 2 diabetes patients attending public hospitals in Ilu AbaBor and Bunno Bedelle zones.
Study Populations
The study population was all selected Type 2 diabetes patients attending public hospitals in Ilu AbaBor and Bunno Bedelle zones.
Inclusion Criteria
At the onset of the study, all registered Type 2 diabetes patients aged ≥18 years in public hospitals of Ilu Aba Bor and Bunno Bedelle zones were included to the study.
Exclusion Criteria
Patients who were seriously ill during the data collection period were excluded from the study.
Sample Size Determination and Sampling Procedure
The sample size was determined using a single population proportion formula by considering the following assumptions:
95% level of confidence interval
5% margin of error (d)
37.6% as a prevalence of diabetes related distress from previous study.16
 |
Therefore, the sample size for this particular study was 360. In selecting study participants, first, the total sample size was allocated proportionally to the number of registered T2DM patients in each hospital. Then, an individual patient was selected by conveniently sampling until the required sample size was achieved.
Variables
The dependent variable of this study was diabetes related distress and independent variables were age, sex, marital status, residence, religion, family or social support, educational status, occupation, level of education, duration of diabetes, mode of current treatment, having diabetic complications, level of fasting blood sugar (FBS), level of systolic blood pressure (SBP), level of diastolic blood pressure (DBP), body mass index (BMI), smoking status, and status of alcohol consumption.
Data Collection Tool and Method
Data were collected through face to face interviews. The interviews were conducted in a quiet room in which patients came for routine follow up. The collected data consisted of socio-demographic characteristics, clinical related history, social history, clinical parameters, and questions related to diabetes related distress. Clinical parameters (levels of fasting blood glucose, blood pressure, and weight and height (BMI)) were retrieved from the patients’ latest medical records. Diabetes Distress Scale (DDS17) was used to measure each patient’s diabetes related distress. The tool is a widely used and well-validated 17-item questionnaire that measures different diabetes related stressors.13,15 Each question has six answer choices: 1 – no problem, 2 – slight problem, 3 – moderate problem, 4 – somewhat serious problem, 5 – a serious problem and 6 – a very serious problem. The questionnaire contains four domains: Emotional Burden (5 items: questions 1, 3, 8, 11, and 14); Physician related distress (4 items: questions 2, 4, 9, and 15); Regimen related distress (5 items: questions 5, 6, 10, 12, and 16); and Interpersonal related distress (3 items: questions 7, 13, and 17). An overall mean score of less than 2.0 was considered as little to no distress, a score between 2.0 and 2.9 was considered as moderate distress, and a score of 3.0 or higher was considered as a high level of distress.34
Data Analysis
Data were entered after being checked for completeness and accuracy into Epi Data version 4.2.2 and exported to SPSS version 20.0. Frequencies, means, and standard deviations of independent variables and level of DRD were analyzed using descriptive statistics. Associations between independent and dependent variables were performed by means of bivariate and multivariate logistic regressions. All variables with p-value less than 0.025 in the bivariate analysis were fitted to the multivariate logistic regression to control the possible effect of confounders. An adjusted odds ratio (AOR) with 95% confidence interval was used to identify the strength of the associated factors with DRD. Statistical significance was considered at P-value < 0.05 in the multivariate logistic regression. The results of study were described in the form of text, tables, and a figure.
Results
Participants’ Characteristics
Out of the 360 patients recruited, 321 (89.2%) patients were involved in the study, of which 201 (62.6%) were male. The mean age of the participants was 41.3 (SD = 12.8) years, and 97 (30.3%) of them were in the range of 40–49 years (Table 1).
Table 1.
Characteristics of Patients with Type 2 Diabetes Mellitus Attending Hospitals in Southwest Ethiopia, 2020 (n=321)
| Variables | Categories | Frequency | Percent |
|---|---|---|---|
| Sex | Male | 201 | 62.6 |
| Female | 120 | 37.4 | |
| Age | 18–29 | 60 | 18.7 |
| 30–39 | 83 | 25.9 | |
| 40–49 | 94 | 29.3 | |
| 50+ | 84 | 26.2 | |
| Marital status | Single | 93 | 29 |
| Married | 207 | 64.5 | |
| Others | 21 | 6.5 | |
| Residence | Urban | 171 | 53.3 |
| Rural | 150 | 46.7 | |
| Religion | Orthodox | 122 | 38 |
| Muslim | 158 | 49.2 | |
| Protestant | 41 | 12.8 | |
| Family/social support | Yes | 192 | 59.8 |
| No | 129 | 40.2 | |
| Occupation/Employment | Governmental | 110 | 34.3 |
| Farmer | 168 | 52.3 | |
| Merchant | 43 | 13.4 | |
| Level of education | Primary school | 161 | 50.1 |
| Secondary school | 92 | 28.7 | |
| Diploma | 36 | 11.2 | |
| Degree and above | 32 | 10.0 |
Participants’ Clinical Related Details
The study found that the mean duration of living with type 2 diabetes was 6.4 (SD = 5.1) years with minimum of 1 and maximum of 22 years. The most frequently (204; 63.6%) reported mode of type 2 diabetes treatment was oral medication (Table 2).
Table 2.
Clinical Related Details of Patients with Type 2 Diabetes Mellitus Attending Hospitals in Southwest Ethiopia, 2020 (n = 321)
| Variables | Categories | Frequency | Percent |
|---|---|---|---|
| Duration with diabetes | ≤2 | 90 | 28 |
| 3–4 | 70 | 21.8 | |
| 5–9 | 84 | 26.2 | |
| 10+ | 77 | 24 | |
| Mode of current treatment | Oral | 204 | 63.6 |
| Insulin | 34 | 10.6 | |
| Oral and insulin | 39 | 12.1 | |
| Lifestyle modification | 44 | 13.7 | |
| Having diabetes complications | Yes | 59 | 18.4 |
| No | 262 | 81.6 |
Participants’ Social History
The study found that out of 321 participants, 68 (21.2%) and 82 (25.5%) of participants had a history of cigarette smoking and alcohol consumption, respectively.
Participants’ Clinical Parameters
The blood glucose level of most participants (301; (93.8%) was out of control with mean of 152.1±35.5 mg/dl. The blood pressure of the majority of participants was in the pre-hypertension stage on both SBP 230 (71.7%) and DPB 189 (58.9%) Table 3).
Table 3.
Clinical Parameters of Patients with Type 2 Diabetes Mellitus Attending Hospitals in Southwest Ethiopia, 2020 (n = 321)
| Variables | Categories | Frequency | Percent |
|---|---|---|---|
| FBS (mg/dl), 152.1±35.5 | Pre-diabetes (100–125) | 20 | 6.2 |
| Overt diabetes (≥126) | 301 | 93.8 | |
| SBP (mmHg), 126.3±11.6 | Normal (<120) | 49 | 15.3 |
| Pre-hypertension (120–130) | 230 | 71.7 | |
| Hypertension (≥140) | 42 | 13.1 | |
| DBP (mmHg), 81.8±9.3 | Normal (<80) | 90 | 28 |
| Pre-hypertension (80–89) | 189 | 58.9 | |
| Hypertension (≥90) | 42 | 13.1 | |
| BMI (kg/m2), 24.0±3.6 | Normal (18.5–24.9) | 205 | 63.9 |
| Overweight (25–29.9) | 95 | 29.6 | |
| Obese (≥30) | 21 | 6.5 |
Note: BMI = weight (kg)/height (m)2.
Abbreviations: FBS, fast blood sugar; SBP, systolic blood pressure; DBP, diastolic blood pressure; BMI, body mass index.
Prevalence of Diabetes Related Distress
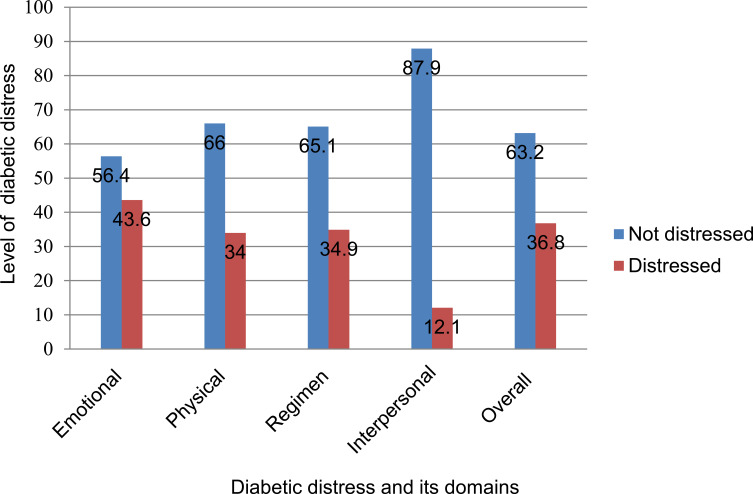
Prevalence of DRD among the study participants was 118 (36.8%) of which the majority (104; 32.4%) were in moderate distress (Table 4). As illustrated in Figure 1 regarding prevalence of diabetes distress and its domains, the highest prevalence of diabetes distress was found in the emotional domain with lowest prevalence being in the interpersonal domain (Figure 1).
Table 4.
Level of DRD Among Patients with Type 2 Diabetes Mellitus Attending Hospitals in Southwest Ethiopia, 2020 (n = 321)
| Level of DRD | Frequency | Percent |
|---|---|---|
| Little/no distress | 203 | 63.2 |
| Moderate distress | 104 | 32.4 |
| High distress | 14 | 4.4 |
Notes: Low, no distress, mean DDs score <2; medium, moderate distress, mean DDs score 2–2.9; high, distress worthy of clinical attention, mean DDs score ≥3.
Figure 1.
Prevalence of diabetes related distress and its domains among patients with type 2 diabetes mellitus attending hospitals in Southwest Ethiopia, 2020 (n = 321).
Factors Associated with Diabetes Related Distress
Logistic regression analysis was conducted to identify factors associated with DRD. In the bivariate analysis age, level of education, family or social support, duration of diabetes, having diabetes related complications, smoking status, alcohol consumption status, level of systolic blood pressure, and level of BMI were identified factors associated with DRD at P < 0.025. However, the remaining variables sex, marital status, residence, religion, occupation, and mode of current treatment were not significantly associated with DRD. In the multivariate analysis, level of education [AOR 4.55; 95% CI: 1.28–16.19], family or social support [AOR 0.62; 95% CI: 0.33–1.06], duration of diabetes [AOR 0.75; 95% CI: 0.35–1.55], having diabetes related complications [AOR 1.98; 95% CI: 1.0–3.86], smoking status [AOR 1.6; 95% CI: 1.12–2.97], and alcohol consumption status [AOR 1.4; 95% CI: 1.07–2.53] were factors significantly associated with DRD at P< 0.05 (Table 5).
Table 5.
Bivariate and Multivariate Analysis of Factors Associated with DRD Among Patients with Type 2 Diabetes Mellitus Attending Hospitals in Southwest Ethiopia, 2020 (n = 321)
| Variables | Diabetes Distress | OR with 95% CI | P-value | ||
|---|---|---|---|---|---|
| Not Distressed | Distressed | Crude | Adjusted | ||
| Age | 0.06 | ||||
| 18–29 | 39(12.1) | 21(6.4) | 0.65(0.33–1.30) | 1.2(0.46–2.23) | |
| 30–39 | 58(18.1) | 25(7.8) | 0.52(0.28–0.30) | 0.72(0.35–1.47) | |
| 40–49 | 60(18.7) | 34(10.6) | 0.7(0.37–1.25) | 0.94(0.49–1.99) | |
| 50+ | 46(14.3) | 38(11.8) | 1 | 1 | |
| Level of education | 0.003 | ||||
| Primary school | 92(28.7) | 37(21.5) | 7.25(2.12–24.77) | 4.55(1.28–16.19) ** | |
| Secondary school | 55(17.1) | 37(11.5) | 6.5(1.84–22.91) | 3.86(1. 4–14.36) * | |
| Diploma | 27(8.4) | 9(2.9) | 3.22(0.78–13.170) | 2.46(1.56–10.76) * | |
| Degree and above | 29(9.0) | 3(0.9) | 1 | ||
| Family/social support | 0.04 | ||||
| Yes | 136(42.4) | 56(17.4) | 0.44(0.28–0.70) | 0.62(0.33–1.06) * | |
| No | 67(20.9) | 62(19.4) | 1 | 1 | |
| Duration with diabetes | 0.047 | ||||
| ≤2 | 59(18.4) | 31(9.7) | 0.44(0.23–0.81) | 0.75(0.35–1.55) * | |
| 3–4 | 61(19.0) | 16(5.0) | 0.22(0.10–0.44) | 0.35(0.16–0.83) * | |
| 5–9 | 48(15.0) | 29(9.0) | 0.5(0.26–0.95) | 0.65(0.32–1.33) * | |
| 10+ | 35(10.9) | 42(13.1) | 1 | 1 | |
| Having diabetes complications | 0.031 | ||||
| Yes | 26(8.1) | 33(10.3) | 2.64(1.48–4.70) | 1.98(1–3.86) * | |
| No | 177(55.1) | 85(26.5) | 1 | 1 | |
| Smoking status | 0.01 | ||||
| Yes | 30(9.3) | 38 (11.8) | 2.74(1.58–4.73) | 1.6(1.12–2.97) * | |
| No | 173(53.9) | 80(25.0) | 1 | 1 | |
| Taking alcohol | 0.045 | ||||
| Yes | 53(16.6) | 29(9.0) | 2.1(1.26–3.50) | 1.4(1.07–2.53) * | |
| No | 150(46.7) | 77(27.8) | 1 | 1 | |
| SBP (mmHg) | 0.067 | ||||
| Normal (<120) | 32(10.0) | 17(5.3) | 0.6(0.4–2.53) | 0.09(0.03–2.52) | |
| Pre-hypertension (120–130) | 143(44.5) | 87(27.1) | 0.2(0.12–2.44) | 0.25(0.15–2.6) | |
| Hypertension (≥140) | 28(8.7) | 14(4.4) | 1 | 1 | |
| BMI (kg/m2) | 0.054 | ||||
| Normal (18.5–24.9) | 125(38.9) | 80(24.9) | 0.2(0.5–3.3) | 0.97(0.31–3.05) | |
| Overweight (25–29.9) | 64(19.9) | 31(9.7) | 0.96(0.35–2.64) | 0.81(0.25–2.60) | |
| Obese (≥30) | 14(4.4) | 7(2.2) | 1 | 1 | |
Notes: *P < 0.05; **P < 0.01.
Discussion
Diabetes related distress is a very common and highly prevalent psychological problem in diabetic patients.35 Evidence shows that it is highly linked with poor glycemic control, low levels of physical activity, and non-adherence to diets and medications.23,36 The American Diabetes Association’s psychosocial care guidelines recommended that peoples with diabetes (PWD) should be assessed for DRD.27 However, there are very few studies about DRD in Ethiopia. The present study was aimed to investigate the prevalence of DRD and associated factors among diabetes patients in Southwest Ethiopia. The researchers believed that the results obtained from present study would be beneficial in initiation of early detection and intervention for DRD among people with type 2 diabetes.
In the present study the overall prevalence of DRD among the participants was 118 (36.8%) in which the majority (101; 31.5%) were in moderate distress on a DDS-17 scale. This finding is relatively high in comparison with previous studies conducted in India (13.3%),37 the Netherlands,20 Taif, Saudi Arabia (25%),38 Jazan, Saudi Arabia (22.3%)15 and Thailand (8.9%).34 The higher prevalence in the present study could be due to poor quality of diabetes care service, lower level of education, the measurement tool used to quantify the level of diabetic distress, and other forms of stressors.
Several studies among diabetic patients had found higher prevalence of DRD than the present study. Studies that were done in Bangladesh39 and Malaysia13 using the DDS-17 scale showed that almost half of patients with T2DM had DRD. Studies in Ghana22 and Nigeria19 reported that 44.7% and 51.9% of patients had high levels of DRD, respectively. This discrepancy between the previously reported DRD magnitude and the current prevalence might result from better family and social support implemented in our societies and patients might have under-rated their level of distress. The difference might also be due to variation in coexisting medical problems besides diabetes among study participants. A number of studies have shown that developing healthy coping skills and increasing diabetes related self-efficacy through structured education among PWD can lower diabetes distress.40–43 Therefore, researchers recommended that diabetic self-management education and support (DSME/S) intervention should be implemented to reduce DRD.
In line with previous studies,15,44 the present study showed that most of the participants had poor glycemic control. This could be explained by the fact that DRD has a negative impact on blood glucose levels. In DRD regulatory hormones and neurotransmitters such as catecholamine, glucocorticoids, growth hormones, and glucagon are activated. Therefore, blood glucose levels increase as a result of these hormones and neurotransmitters interfere with the action of insulin.45,46 A study in Ghana found that the odds of high DRD among patients with T2DM increased by 12% with every additional unit increase in the glucose level.22 In contrast to this blood glucose level did not significantly associate with DRD in the current study. This could be due to the small number of participants with adequately controlled glycemia in the current study.
In the present study patients who had family or social support were 0.62 times less likely to have DRD than those who had no support. Prior studies found lack of family support was positively associated with DRD.30,34 The current study also found that participants who had diabetic complications were almost two times more likely to experience DRD than their counterparts. This finding was consistent with the results of prior studies.39,47,48 However, some studies have found no association between having diabetic complications and DRD.13,20,49 In contrast to previous studies, lower education level was a major factor for high diabetes distress scores in the present study.34,50 This could be the fact that low education level leads to poor knowledge about the illness and its complications, which in turn increases the risk of poor dietary habits, poor medication compliance, and fewer health check-ups.
As with prior studies,15,44 smoking was significantly associated with DRD in the present study. The possible explanation for this consistent finding could be that long-term exposure to nicotine dysregulates the hypothalamic-pituitary-adrenal system. This results in changes in the monoamine neurotransmitter system which regulates reactions to stressors. Although the present study did not reveal any significant association between mode of diabetic treatment and DRD, a number of studies indicated that using insulin treatment had a significant effect on DRD.21,38,51 This inconsistent result with other findings may be due to the small proportion of participants who used insulin treatment in the present study and there may be other factors that have hidden the effect of insulin.
Limitations
There are several potential limitations of this study that should be considered in the interpretation of the present findings. First, the study was based on participants’ reports of data and therefore, there may be recall bias. Second, the cross-sectional design of the study limits the ability to draw conclusions about causality or directions of the relationships between DRD and the independent variables. The last potential limitation of this study to be considered was the non-probable sampling technique used to select individual participants.
Conclusion
Diabetes related distress was highly prevalent in type 2 diabetes patients. This suggests that DRD requires special attention by healthcare providers to prevent and reduce it through integrating psychosocial care with collaborative medical care. Education level, having family or social support, duration of diabetes, having diabetic complications, smoking status, and alcohol consumption status were the identified factors associated with DRD. Therefore, these factors should be targeted in the system of diabetes care to take immediate intervention and prevent further problems. Moreover, healthcare professionals should pay more attention to non-clinical factors such as social support when addressing DRD. Incorporating routine screening for DRD into diabetes care and adopting holistic approaches to diabetes management to improve adherence to self-care behaviors and health outcomes of type 2 diabetes patients is recommended.
Acknowledgments
Our deepest gratitude goes to Mettu University, College of Health sciences for giving us the opportunity to conduct this study. We would also like to extend our sincere gratitude to the data collectors, supervisors and the study participants for being involved in the study.
Funding Statement
This study was conducted in collaboration with Mettu University. Every step of the study was followed by Mettu University, College of Health sciences, department of Nursing. The university has no role in designing, analysis and writing of the study.
Abbreviations
AOR, adjusted odds ratio; CI, confidence interval; DDS, diabetes distress scale; DM, diabetes mellitus; DRD, diabetes related distress; DSME/S, Diabetic Self-management Education and Support; HbA1c, glycated hemoglobin; PWD, peoples with diabetes; SPSS, Statistical Package for the Social Sciences; T2DM, Type 2 Diabetes Mellitus.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval and Informed Consent
Ethical approval was obtained from Mettu University, College of Health Sciences, Research review committee (Protocol number = Meu/CHS/RCS/05/2019). The study protocol was performed in accordance with the Declaration of Helsinki. Supportive letter was given and permission was obtained from each hospital. Informed consent was obtained from participants after they were informed about the objectives of the study. Confidentiality and privacy of participants was also ensured.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
- 1.Cho N, Shaw J, Karuranga S, et al. IDF diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–281. doi: 10.1016/j.diabres.2018.02.023 [DOI] [PubMed] [Google Scholar]
- 2.Control CfD. Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States. Atlanta, GA: US Department of Health and Human Services; 2014:2014. [Google Scholar]
- 3.Stanković Ž, Jašović-Gašić M, Lečić-Toševski D. Psychological problems in patients with type 2 diabetes: clinical considerations. Vojnosanitetskipregled. 2013;70(12):1138–1144. [DOI] [PubMed] [Google Scholar]
- 4.Fisher L, Mullan JT, Arean P, Glasgow RE, Hessler D, Masharani U. Diabetes distress but not clinical depression or depressive symptoms is associated with glycemic control in both cross-sectional and longitudinal analyses. Diabetes Care. 2010;33(1):23–28. doi: 10.2337/dc09-1238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Perrin N, Davies M, Robertson N, Snoek F, Khunti K. The prevalence of diabetes‐specific emotional distress in people with type 2 diabetes: a systematic review and meta‐analysis. Diabetic Med. 2017;34(11):1508–1520. doi: 10.1111/dme.13448 [DOI] [PubMed] [Google Scholar]
- 6.Wardian J, Sun F. Factors associated with diabetes-related distress: implications for diabetes self-management. Soc Work Health Care. 2014;53(4):364–381. doi: 10.1080/00981389.2014.884038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Park M, Katon WJ, Wolf FM. Depression and risk of mortality in individuals with diabetes: a meta-analysis and systematic review. Gen Hosp Psychiatry. 2013;35(3):217–225. doi: 10.1016/j.genhosppsych.2013.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fisher L, Gonzalez J, Polonsky W. The confusing tale of depression and distress in patients with diabetes: a call for greater clarity and precision. Diabet Med. 2014;31(7):764–772. doi: 10.1111/dme.12428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fisher L, Hessler DM, Polonsky WH, Mullan J. When is diabetes distress clinically meaningful? Establishing cut points for the diabetes distress scale. Diabetes Care. 2012;35(2):259–264. doi: 10.2337/dc11-1572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Isher L, Mullan JT, Skaff MM, Glasgow RE, Arean P, Hessler D. Predicting diabetes distress in patients with type 2 diabetes: a longitudinal study. Diabetic Med. 2009;26(6):622–627. doi: 10.1111/j.1464-5491.2009.02730.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Egede LE, Ellis C. Diabetes and depression: global perspectives. Diabetes Res Clin Pract. 2010;87(3):302–312. doi: 10.1016/j.diabres.2010.01.024 [DOI] [PubMed] [Google Scholar]
- 12.Dennick K, Sturt J, Hessler D, et al. High rates of elevated diabetes distress in research populations: a systematic review and meta-analysis. Int Diabetes Nurs. 2015;12(3):93–107. doi: 10.1080/20573316.2016.1202497 [DOI] [Google Scholar]
- 13.Chew B-H, Vos R, Mohd-Sidik S, Rutten GE, Hashimoto K. Diabetes-related distress, depression and distress-depression among adults with type 2 diabetes mellitus in Malaysia. PLoS One. 2016;11(3):e0152095. doi: 10.1371/journal.pone.0152095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhou H, Zhu J, Liu L, et al. Diabetes-related distress and its associated factors among patients with type 2 diabetes mellitus in China. Psychiatry Res. 2017;252:45–50. doi: 10.1016/j.psychres.2017.02.049 [DOI] [PubMed] [Google Scholar]
- 15.Alzughbi T, Badedi M, Darraj H, et al. Diabetes-related distress and depression in saudis with type 2 diabetes. Psychol Res Behav Manag. 2020;13:453–458. doi: 10.2147/PRBM.S255631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wolde K, G. Wondim M. Diabetic distress among diabetic patients in the referral hospital of Amhara regional state, Ethiopia. Int Q Community Health Educ. 2020;40(2):105–114. doi: 10.1177/0272684X19857580 [DOI] [PubMed] [Google Scholar]
- 17.Baek RN, Tanenbaum ML, Gonzalez JS. Diabetes burden and diabetes distress: the buffering effect of social support. Ann Behav Med. 2014;48(2):145–155. doi: 10.1007/s12160-013-9585-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dieter T, Lauerer J. Depression or diabetes distress? Perspect Psychiatr Care. 2017;54(1):84–87. doi: 10.1111/ppc.12203 [DOI] [PubMed] [Google Scholar]
- 19.Onyenekwe BM, Young EE, Nwatu CB, Okafor CI, Ugwueze CV. Diabetes distress and associated factors in patients with diabetes mellitus in south east Nigeria. Dubai Diabetes Endocrinol J. 2020: 1–7. [Google Scholar]
- 20.Özcan B, Rutters F, Snoek FJ, et al. High diabetes distress among ethnic minorities is not explained by metabolic, cardiovascular, or lifestyle factors: findings from the Dutch diabetes pearl cohort. Diabetes Care. 2018;41(9):1854–1861. doi: 10.2337/dc17-2181 [DOI] [PubMed] [Google Scholar]
- 21.Islam M, Karim M, Habib S, Yesmin K. Diabetes distress among type 2 diabetic patients. Int J Med Biomed Res. 2013;2(2):113–124. doi: 10.14194/ijmbr.224 [DOI] [Google Scholar]
- 22.Kretchy IA, Koduah A, Ohene-Agyei T, Boima V, Appiah B. The association between diabetes-related distress and medication adherence in adult patients with type 2 diabetes mellitus: a cross-sectional study. J Diabetes Res. 2020;2020. doi: 10.1155/2020/4760624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Egede LE, Dismuke CE. Serious psychological distress and diabetes: a review of the literature. Curr Psychiatry Rep. 2012;14(1):15–22. doi: 10.1007/s11920-011-0240-0 [DOI] [PubMed] [Google Scholar]
- 24.Peña-Purcell N, Han G, Smith ML, Peterson R, Ory MG. Impact of diabetes self-management education on psychological distress and health outcomes among African Americans and Hispanics/Latinos with diabetes. Diabetes Spectr. 2019;32(4):368–377. doi: 10.2337/ds18-0081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nouwen A, Speight J, Pouwer F, Holt R. How psychosocial and behavioural research has shaped our understanding of diabetes. Diabetic Med. 2020;37(3):377–379. doi: 10.1111/dme.14254 [DOI] [PubMed] [Google Scholar]
- 26.Zhu Y, Fish AF, Li F, Liu L, Lou Q. Psychosocial factors not metabolic control impact the quality of life among patients with type 2 diabetes in China. Acta Diabetol. 2016;53(4):535–541. doi: 10.1007/s00592-015-0832-y [DOI] [PubMed] [Google Scholar]
- 27.Young-Hyman D, De Groot M, Hill-Briggs F, Gonzalez JS, Hood K, Peyrot M. Psychosocial care for people with diabetes: a position statement of the American diabetes association. Diabetes Care. 2016;39(12):2126–2140. doi: 10.2337/dc16-2053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gonzalez JS, Tanenbaum ML, Commissariat PV. Psychosocial factors in medication adherence and diabetes self-management: implications for research and practice. Am Psychol. 2016;71(7):539. doi: 10.1037/a0040388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rubin RR, Peyrot M. Psychosocial adjustment to diabetes and critical periods of psychological risk. Psicosoc Care People Diabetes. 2012;219–228. [Google Scholar]
- 30.Karlsen B, Oftedal B, Bru E. The relationship between clinical indicators, coping styles, perceived support and diabetes‐related distress among adults with type 2 diabetes. J Adv Nurs. 2012;68(2):391–401. doi: 10.1111/j.1365-2648.2011.05751.x [DOI] [PubMed] [Google Scholar]
- 31.Lin K, Park C, Li M, et al. Effects of depression, diabetes distress, diabetes self-efficacy, and diabetes self-management on glycemic control among Chinese population with type 2 diabetes mellitus. Diabetes Res Clin Pract. 2017;131:179–186. doi: 10.1016/j.diabres.2017.03.013 [DOI] [PubMed] [Google Scholar]
- 32.Chew B-H, Mohd-Sidik S, Shariff-Ghazali S. Negative effects of diabetes–related distress on health-related quality of life: an evaluation among the adult patients with type 2 diabetes mellitus in three primary healthcare clinics in Malaysia. Health Qual Life Outcomes. 2015;13(1):187. doi: 10.1186/s12955-015-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stephani V, Opoku D, Beran D. Self-management of diabetes in Sub-Saharan Africa: a systematic review. BMC Public Health. 2018;18(1):1148. doi: 10.1186/s12889-018-6050-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tunsuchart K, Lerttrakarnnon P, Srithanaviboonchai K, Likhitsathian S, Skulphan S. Type 2 diabetes mellitus related distress in Thailand. Int J Environ Res Public Health. 2020;17(7):2329. doi: 10.3390/ijerph17072329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lloyd C, Nouwen A, Sartorius N, et al. Prevalence and correlates of depressive disorders in people with type 2 diabetes: results from the international prevalence and treatment of diabetes and depression (INTERPRET‐DD) study, a collaborative study carried out in 14 countries. Diabetic Med. 2018;35(6):760–769. doi: 10.1111/dme.13611 [DOI] [PubMed] [Google Scholar]
- 36.Association AD. Erratum glycemic targets. sec. 6. in standards of medical care in diabetes—2017. Diabetes Care. 2017;40(Suppl. 1):S48–S56. doi: 10.2337/dc17-S009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Symon A, Vargese SS, Mathew E, Akshay K, Abraham J. Diabetes related distress in adults with type 2 diabetes mellitus: a community-based study. Int J Community Med Public Health. 2018;6(1):151–155. doi: 10.18203/2394-6040.ijcmph20185234 [DOI] [Google Scholar]
- 38.Aljuaid MO, Almutairi AM, Assiri MA, Almalki DM, Alswat K. Diabetes-related distress assessment among type 2 diabetes patients. J Diabetes Res. 2018;2018:2018. doi: 10.1155/2018/7328128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Islam MR, Islam MS, Karim MR, Alam UK, Yesmin K. Predictors of diabetes distress in patients with type 2 diabetes mellitus. Bull Pharm Med Sci. 2014;2(1). [Google Scholar]
- 40.Robling M, McNamara R, Bennert K, et al. The effect of the talking diabetes consulting skills intervention on glycaemic control and quality of life in children with type 1 diabetes: cluster randomised controlled trial (DEPICTED study). BMJ. 2012;344(apr26 2):e2359. doi: 10.1136/bmj.e2359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pamungkas RA, Chamroonsawasdi K, Vatanasomboon P. A systematic review: family support integrated with diabetes self-management among uncontrolled type II diabetes mellitus patients. Behav Sci (Basel). 2017;7(3):62. doi: 10.3390/bs7030062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Aikens JE, Rosland A-M, Piette JD. Improvements in illness self-management and psychological distress associated with telemonitoring support for adults with diabetes. Prim Care Diabetes. 2015;9(2):127–134. doi: 10.1016/j.pcd.2014.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Machen ML, Borden HC, Hohmeier KC. The impact of a community pharmacy diabetes self-management education program on diabetes distress. J Pharm Technol. 2019;35(1):3–10. doi: 10.1177/8755122518805429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Darraj H, Badedi M, Poore KR, et al. Vitamin D deficiency and glycemic control among patients with type 2 diabetes mellitus in Jazan City, Saudi Arabia. Diabetes Metab Syndr Obes. 2019;12:853. doi: 10.2147/DMSO.S203700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nanayakkara N, Pease A, Ranasinha S, et al. Depression and diabetes distress in adults with type 2 diabetes: results from the Australian National Diabetes Audit (ANDA) 2016. Sci Rep. 2018;8(1):1–10. doi: 10.1038/s41598-018-26138-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kuniss N, Kramer G, Müller N, et al. Diabetes-related burden and distress is low in people with diabetes at outpatient tertiary care level. Exp Clin Endocrinol Diabetes. 2016;124(05):307–312. doi: 10.1055/s-0042-103685 [DOI] [PubMed] [Google Scholar]
- 47.Liu S-Y, Huang J, Dong Q-L, et al. Diabetes distress, happiness, and its associated factors among type 2 diabetes mellitus patients with different therapies. Medicine. 2020;99(11):e18831. doi: 10.1097/MD.0000000000018831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hu Y, Li L, Zhang J. Diabetes distress in young adults with type 2 diabetes: a cross-sectional survey in China. J Diabetes Res. 2020;2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stoop C, Nefs G, Pop V, et al. Diabetes‐specific emotional distress in people with type 2 diabetes: a comparison between primary and secondary care. Diabet Med. 2014;31(10):1252–1259. doi: 10.1111/dme.12472 [DOI] [PubMed] [Google Scholar]
- 50.Gahlan D, Rajput R, Gehlawat P, Gupta R. Prevalence and determinants of diabetes distress in patients of diabetes mellitus in a tertiary care centre. Diabetes Metab Syndr. 2018;12(3):333–336. doi: 10.1016/j.dsx.2017.12.024 [DOI] [PubMed] [Google Scholar]
- 51.Tol A, Baghbanian A, Sharifirad G, et al. Assessment of diabetic distress and disease related factors in patients with type 2 diabetes in Isfahan: a way to tailor an effective intervention planning in Isfahan-Iran. J Diabetes Metab Disord. 2012;11(1):20. doi: 10.1186/2251-6581-11-20 [DOI] [PMC free article] [PubMed] [Google Scholar]