Abstract
Accessing Meckel’s cave (MC) is surgically challenging. Open approaches are complex and often correlated with high morbidity. Endoscopic approaches emerged in the last decade as feasible alternatives to open approaches, especially for sampling indeterminate lesions. This article first analyses available routes to approach Meckel’s cave and presents furthermore an illustrative case. We conducted a systematic review and reported according to the guidelines for preferred reporting items for systematic reviews and meta-analyses (PRISMA). Various surgical approaches identified through the search are evaluated and discussed in detail. Additionally, we report on a case of woman with a lesion in MC, which was accessed through an endoscopic transpterygoid approach subsequently diagnosed as a diffuse large B cell lymphoma. Our search delivered 75 articles that included case reports (n = 21), cadaveric studies (n = 32), clinical articles (n = 16), review of the literatures (n = 3), as well as technical notes (n = 2) and a radiological manuscript (n = 1). Open routes included lateral approaches with many variations, mainly intra- and extradural pterional approaches and anterior petrosal, as well as a retrosigmoid intradural suprameatal and a lateral transorbital approach. Endoscopically, MC was reached via approaches that included transpterygoid, transorbital or infraorbital fissure routes. Percutaneous approaches, e.g. through the foramen ovale, were also described. Multiple surgical approaches to MC are currently available. Their different characteristics as well as individual patient factors, such as clinical history and the localization of the disease, have to be considered when choosing a surgical corridor. Studies included in this review highlight the endonasal endoscopic transpterygoidal technique as an excellent corridor for biopsies in the ventral MC.
Electronic supplementary material
The online version of this article (10.1007/s10143-020-01247-w) contains supplementary material, which is available to authorized users.
Keywords: Meckel’s cave, Approaches, Indeterminate lesions, Endoscopic endonasal approach, Skull base surgery
Introduction
Named after Johann Friedrich Meckel, a German anatomist, the cavum meckeli, also known as Meckel’s cave, trigeminal cave or cisterna trigeminalis, is a region with a complex neurovascular array and, therefore, anatomically speaking, presenting a surgical challenge.
Meckel’s cave is located at the petrous apex between two dural layers originating from the floor of the middle fossa and dividing at the trigeminal notch, complemented by the dura propria of the posterior fossa [1–3]. Laterally, Meckel’s cave is limited by a meningeal layer covering the temporal lobe, whereas its medial wall separates the intercavernous carotid and sphenoid body from the trigeminal nerve [3]. Infero-medially, Meckel’s cave meets the bony part of the temporal fossa, as well as the petrous carotid canal [4, 5].
Due to Meckel’s cave location interfacing the posterior and middle fossae, lesions can spread between compartments, and thereby requiring access through a multi-corridor surgery.
External approaches have been historically applied to access this region [6–9]. The introduction of rod-lens-endoscopes allowed for minimal-access routes to the sellar and parasellar region affording exposure of the anterolateral and inferior portion of Meckel’s cave [5], thus improving cosmetic results and potentially decreasing surgical morbidity [10]. Since these approaches offer a wide visualization of relevant structures through a small surgical window, both biopsies and larger resections are feasible [5, 7, 11–14].
In lesions where the junction of clinical, radiological and laboratory data are not conclusive to suggest a therapy algorithm, tissue sampling might be imperative to establish a definitive diagnosis and treatment plan. This study aims to analyze different surgical approaches to reach Meckel’s cave for tissue sampling of such indeterminate lesions.
Methods
PRISMA literature search protocol
In this article, we searched and reported according to guidelines established by Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA statement). The protocol included articles published until November 2018 without omission of earlier dates. Terms for searching title and abstract were “Meckel’s cave” and “biopsies”, “Meckel’s cave” and “biopsy”, “Meckel’s cave” and “endoscopic”, “Meckel’s cave” and “approach”, “Meckel’s cave” and “door”, “Meckel’s cave” and “access”, and “Meckel’s” and “resection”. Articles delivered by the initial search were screened for duplicates and non-English abstracts. After eliminating these studies, abstracts were screened and relevant full-texts were evaluated. The search was conducted according to the outlined protocol using commercially available software (Endnote X7, Thompson Reuters, Carlsbad, California, USA).
Results
The initial search yielded 271 articles. First, duplicates (n = 89) and non-English abstracts (n = 25) were removed; thereafter, 157 abstracts were screened for relevance resulting in the full-text evaluation of 112 articles. Subsequently, 75 articles were identified for our qualitative synthesis and included case reports (n = 21) [15–35], cadaveric studies (n = 32) [3, 6, 7, 10, 13, 36–60], clinical articles (n = 16) [2, 5, 8, 9, 16, 61–71], review of the literatures (n = 3) [72–74], as well as technical notes (n = 2) [75, 76] and a radiological manuscript (n = 1) [77]. These outlined articles were published between February 1978 and November 2018. Additional citations were included when relevant. Rather than describing each approach in detail, the study aimed to outline essential information. The authors refer to the respective publications for further details.
Approaches to Meckel’s cave in the literature (Fig. 1)
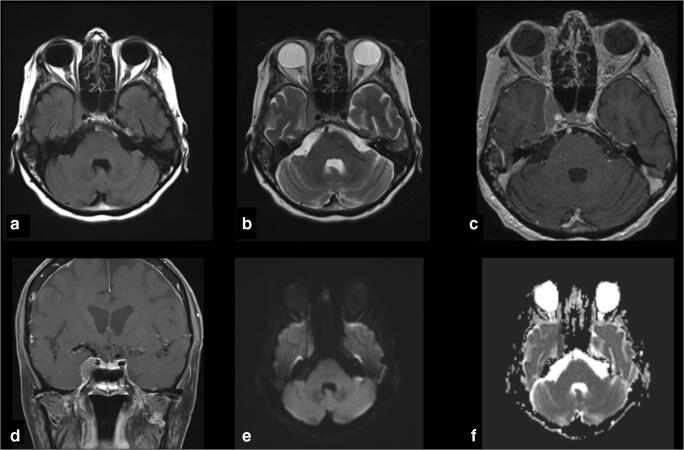
Fig. 1.
Skull base illustration highlighting available routes to Meckel’s cave. These can be divided in antero-medial, antero-lateral, lateral and posterior (red arrows from upper right to lower left, respectively)
Antero-medial
Extended endonasal endoscopic-assisted approach (with illustrative case)
Endoscopic approaches to the skull base are promising due to improved visualization and reduced morbidity in comparison to external approaches. Furthermore, they lack the need for crossing cranial nerves and vessels [7]. In a sufficiently pneumatized sinus, a wide sphenotomy will already provide access to the anterior portion of Meckel’s cave [12, 58, 74]. However, this might not be sufficient if targeting the lower lateral skull base [53]. For more extended visualization of Meckel’s cave, several approaches have been reported in the literature:
Transpterygoid approach
The transpterygoid approach extends the endonasal corridor to address tumors in the middle and posterior fossa [77]. Removing the medial aspect of the pterygoid process base can already provide sufficient access to Meckel’s cave [17]. An ipsilateral middle turbinectomy and uncinectomy, followed by a posterior ethmoidectomy and a wide sphenotomy are normally performed [5]. Lateralization of the inferior turbinate and the contralateral middle turbinate by out-fracturing their bony attachment can increase working space [78]. Additionally, a wide maxillary antrostomy with lateral exposure of the infraorbital fissure with its neurovascular structures can increase the panoramic view of the skull base [5, 70]. The infraorbital nerve delineates the pterygopalatine fossa (PPF) laterally increasing orientation during the procedure.
The Vidian nerve and artery have become an important landmark to identify the inner anterior genu of the petrous segment of the ICA, for improving depth perception during the surgical procedure and avoid injury of the ICA [7, 11, 38, 77–79]. The Vidian neurovascular bundle is identified where the medial pterygoid plate meets the floor of the sphenoid sinus, in average 12.78 mm (range 9.4–15.8 mm) from the midline [77]. This bundle can be either coagulated and divided [5, 78], facilitating lateralization of the PPF content, i.e. int. max. art, V2 and pterygopalatine ganglion [7], or preserved if approaching strictly superior to the Vidian nerve [14, 70]. The Vidian nerve, however, transports sympathetic and parasympathetic fibers important for lacrimation [7]. Hence, Vidian nerve injury can impair lacrimation in the ipsilateral eye. The complex relationship of the ICA at the posterior limit of this route with the Vidian nerve and the quadrangular space is essential for the safety of these surgeries [44, 52, 80]. Skeletonizing the ICA is only required if mobilization is needed for posterior access [7].
A quadrangular space delineated by the ICA medially and inferiorly, the V2 nerve laterally, which is superolateral to the ICA [7], and the abducens nerve with the CS superiorly, provides access to Meckel’s cave [79]. The ICA course should be carefully studied to define the feasibility of this approach [13] and avoid injury while drilling.
To prevent injury of the abducens nerve, V2 should not be crossed superiorly and intraoperative electrophysiological monitoring should be applied [5, 39]. Furthermore, drilling near the petrous apex can induce thermal injury of the VIth nerve [39]. As an orientation, the superior part of the lacerum segment of the ICA correlates with the dural entry point of the VIth nerve posteriorly [39]. Access to the petrous apex requires bypassing the ICA [50]. This route carries limitations for lesions extending into the posterior fossa. However, lesions in the anterior-medial and inferior portion of Meckel’s cave can be easily accessed.
Illustrative case
A 78-year-old female patient presented to the James Comprehensive Skull Base and Pituitary Center, Columbus, Ohio, USA due to a progressive cranial nerve VI palsy, retro-orbital pain and proptosis on the right side. The patient had a pre-medical history of non-Hodgkin lymphoma with a newly identified Meckel’s cave mass (Fig. 2).
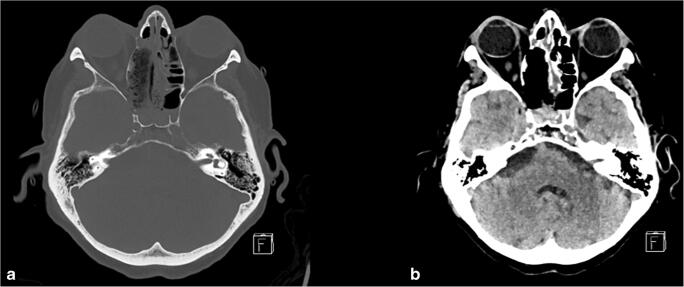
Fig. 2.
Preoperative imaging of a 78-year-old female patient harboring a lesion in Meckel’s cave. No hyperintensity was observed in the a FLAIR- or b T2-weighted scan. There was however contrast-enhancement demonstrated in the c axial and d coronal T1-weighted imaging. No diffusion restriction could be seen in the e DWI, but hypercellularity was demonstrated in the f ADC-sequence
Intending biopsy, the lesion in the right Meckel’s cave was accessed through an extended endonasal endoscopic-assisted transpterygoidal approach (Video 1; Fig. 3). A free mucosal graft was employed for reconstruction of the skull base defect (from the right middle turbinate). The mass was later diagnosed as a diffuse large B cell lymphoma with double expressor (C-MYC+ and Bcl-2+). More in detail, the tumor was classified as germinal center type given CD10 positivity, in the presence of strong MUM-1 staining; these cases have been reported to follow a more aggressive clinical course. The patient postoperative recovery was uneventful. The right retro-orbital pain diminished and double vision improved. There was no sign of new facial numbness or paresthesia.
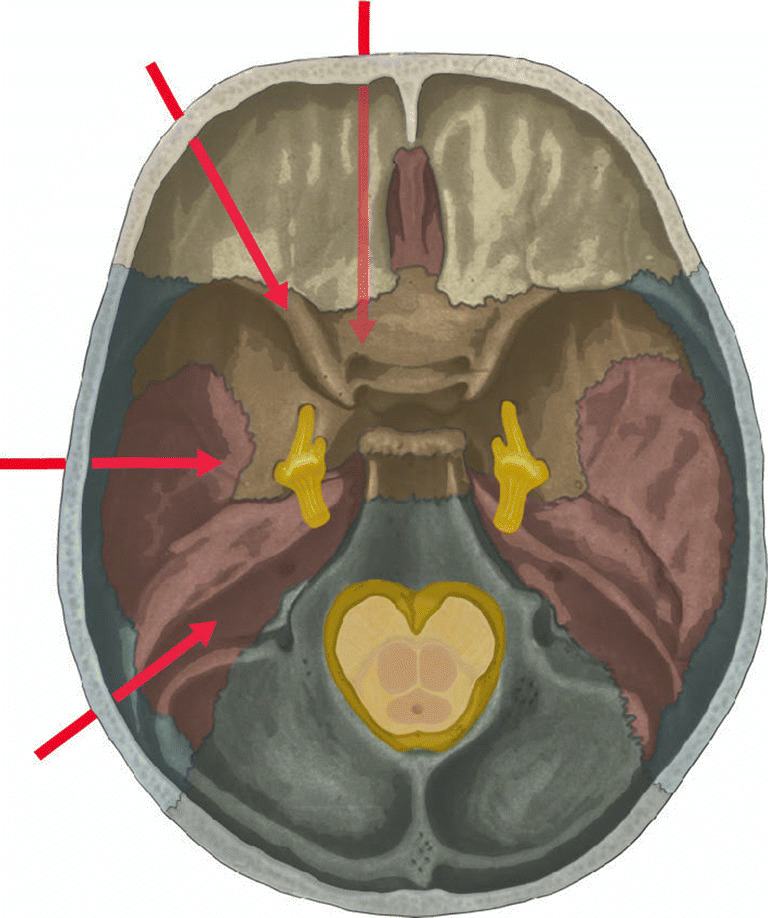
Fig. 3.
Postoperative CT-imaging after endonasal endoscopic transpterygoidal approach to Meckel’s cave with a bony and b tissue windowing demonstrating the bone access to Meckel’s cave, as well as the defect after extended endonasal transpterygoidal approach with right side turbinectomy, uncinectomy, posterior ethmoidectomy and wide sphenotomy
Transmaxillary
As an alternative to the transpterygoid approach, removing the posterior maxillary sinus will also lead to Meckel’s cave [57, 60, 71]. Zhang et al. [60] described an endoscopic access through the inferior orbital fissure. They describe an approach lateral to the middle turbinate, where—after performing an uncinectomy and medial maxillectomy—the infraorbital neurovascular bundle could be transposed inferiorly, providing space for drilling the anterior portion of the sphenoid wing lateral to the foramen rotundum and gain anterolateral access to Meckel’s cave. Previously, Bai et al. [38] described a similar approach reaching the anteromedial portion of Meckel’s cave. As a variance, a sublabial transantral route might lessen the need of removing the anterior sphenoid wall [10, 57]. An anterior antrostomy through a sublabial incision provides access superior to the alveolar ridge. Through the canine fossa, an anterior antrostomy is performed, and dorsal to the maxillary sinus, the infraorbital nerve and subsequently V2 are dissected to reach Meckel’s cave. Access to Meckel’s cave will, however, be limited [57]. These articles discuss the advantage of less manipulation to the structures within the pterygopalatine and infratemporal fossa, as well as within the cavernous sinus and the petroclival carotid, arguing to cause less trauma and providing a safer approach. However, the nasolacrimal duct needs to be transposed and the infraorbital neurovascular array with emerging nerves, i.e. the zygomatic or lacrimal nerve, manipulated; clinical sequela can therefore be of relevance.
Transorbital
Two cadaveric studies outlined the anatomical and technical nuances of the lateral endoscopic orbital route to access Meckel’s cave [47, 54]. This corridor was used to reach the middle fossa and the lateral ventral skull base and Meckel’s cave. The skin incision was made either in the superior eyelid [54], or at the inferior orbital rim [47]. Accessing through the lateral orbit and between the superior and inferior orbital fissure, a triangular [47] or trapezoid [54] shape craniotomy was described. Finding an extradural space superior to V2 and by further drilling posterior to V3, Meckel’s cave could be accessed in an oblique anterosuperior way. The trigeminal nerve could be visualized from the cisternal portion in the posterior fossa until its division in V1-V3 [54]. Additionally, the superior and posterior CS, as well as the superior petrosal sinus, were identified [47]. The region medial to V1 and posterior to the ICA appears an anatomical limitation of this approach. This approach targets the anterolateral and superior region of Meckel’s cave. Jeon et al. demonstrated in a recent series of nine patients, seven of them with diseases involving Meckel’s cave, the feasibility of this novel technique [65]. Even though the sample size is small and the follow-up time was short, the authors reported low morbidity with a single patient suffering of ptosis, which eventually recovered after 6 months. Gross total resection was achieved in seven of nine patients.
Percutaneous
Transforamen ovale image-guided approaches are regularly used for rhizotomy in the context of atypical trigeminus neuralgia [81]. In 1997, Sindou et al. described the percutaneous approach to Meckel’s cave for biopsies of indeterminate lesions, based on their trigeminal thermocoagulation experience [82]. CT-guidance might increase safety [35]. Even though this approach appears feasible, highly vascularized tumors can be of high risk for hemorrhagic complications. Tumor consistency is further important, since hard tumor tissue is difficult to aspirate through a needle [18]. Messerer et al. reported contamination of sample tissue with fat, CSF or blood, leading to diagnostic difficulties [83]. Drainage of arachnoid cysts, however, has been reported as feasible [21]. In the further course, an endoscopic transforamen ovale approach and observation of Meckel’s cave were reported [48]. However, vision was restricted by the lack of space and mobility of the endoscope and by oozing from small veins. Variations of the internal maxillary artery can be of relevance and should be carefully evaluated preoperatively [37]. Nevertheless, this approach should be kept in mind as an option to manage indeterminate lesions, as it is associated with low morbidity and not all pathologies require a surgical therapy [18]. Hence, unnecessary open surgery could be avoided.
Anterolateral and lateral approaches
Anterolateral approaches consist of frontotemporal or orbitozygomatic approaches with intra- or extradural corridors. Major drawback from this corridor is the need of temporal lobe retraction, especially when targeting the inferior part of Meckel’s cave. Augmenting this approach with an orbitozygomatic removal, as well as the dissection of the temporal muscle [31], can decrease retraction of the temporal lobe [62, 84]. By opening the sylvian fissure, the view into Meckel’s cave and cavernous sinus (CS) can be extended [4, 22, 85].
When approaching from the extradural space, elevation of the middle fossa dura is limited medially due to attachment to the V3-Branch and the CS [6]. Furthermore, the meningeal medial artery at the foramen spinosum and V3 at the foramen ovale can be identified before exiting the skull base [6]. Skeletonizing the superior orbital fissure and foramen rotundum and ovale will help delineate the plane of dura elevation [56].
A frontotemporal extra-/interdural approach (Dolenc’s approach [86]) can avoid exposition of the temporal lobe and enable exposure of the trigeminal ganglion [59, 62]. From lateral, Meckel’s cave is best identified around 7.5 mm medial of the foramen spinosum and just posterior to the foramen ovale [6]. The meningeal dura is kept covering the temporal lobe and the entire lateral surface of Meckel’s cave is exposed.
Most of these approaches were created to excise schwannomas or meningiomas in the petroclival or parasellar region [67, 68]; they provide wide access to the superior lateral Meckel’s cave in exchange of higher risk of morbidity.
Subtemporal transpetrosal-transtentorial approach with anterior petrosectomy (Kawase-Shiobara approach)
Kawase et al. described an anterior petrosectomy by removing the bone ventral to the IAM. This route can target pathologies in the upper petroclival region, Meckel’s cave and brainstem [1, 55]. There is a risk of IVth nerve injury if the tentorium is incised with the aim to improve access to the infra- and supratentorial petroclival region [50]. However, this incision is not necessary in most cases.
Great superficial petrosal nerve (GSPN) is identified as an important landmark during anterior petrosectomy [66, 87]. Drilling anterior to the bone of the internal acoustic meatus can cause damage to the cochlea [6]. The approach will be limited by the lower edge of the porus trigeminus, inferior petrosal vein and the petrous ICA [6, 87]. Removal of the Kawase triangle is only essential when exposure of the ventral brainstem and clivus is needed [1, 88]. Lesions from Meckel’s cave with lateral or posterior fossa extension can be reached through this approach.
Excessive retraction of the temporal lobe should be avoided, since this could damage the V. Labbe [89], or induce seizures [90]. Further risks are cranial nerve or vascular injury, CSF leak and damage to the intrapetrous otologic structures, i.e. geniculate ganglion (facial palsy) or cochlea (hearing loss) [91]. To avoid brain stem and cerebellum edema, the superior petrosal vein should be sheltered [92].
Postero-lateral
Retrosigmoid intradural suprameatal approach
The retrosigmoid approach has been discussed as a route to the petroclival region since the beginning of the neurosurgical era [93]. As a modification of the retrosigmoidal approach for lesions extending to the middle fossa, postero-lateral approaches interconnect both the middle and the posterior cranial fossa [8, 72]. Even though a semi-sitting position is commonly used, park-bench positioning might reduce the risk of venous air embolism. The surgical corridor consists of a retrosigmoid approach with additional drilling of the suprameatal bone prominence and the posterior portion of the petrous apex [51]. The latter step can further expose the lateral trigeminal nerve by an average of 10 mm (range 6–13 mm) [3, 36, 41]. The trigeminal impression represents the anterior limit of the bony resection [3, 8].
Optionally, the tentorium can be divided above the Vth nerve for further access to the middle fossa. Drilling the suprameatal tubercle in a pyramidal shape, with the base towards the trigeminus nerve, can avoid injuries to both superior and posterior semicircular canal, as well as to the common crus of both canals [36]. Additionally, endoscopic-assistance with 0- and 30-degree endoscopes has been reported to be feasible for identifying deep-seated neurovascular structures [36, 45, 94]. The trochlear nerve can be identified in the cisterna ambiens medially under the tentorium before trespassing dorsal to the posterior clinoid process [36]. The abducens nerve regularly lies underneath and medial to the IVth cranial nerve traveling to the clivus before it enters into the Dorello’s canal and towards the CS [36].
An advantage of this approach is that no blind tentorial splitting or petrosectomy is needed. However, risks that merit mention are cranial nerves and vessels injury, e.g. superior petrosal vein, sigmoid and transverse sinus, anterior and posterior inferior cerebellar artery, and potential injury through a cerebellum and brainstem retraction.
Other postero-lateral approaches with posterior transpetrosal modifications and presigmoid access can be retrolabyrinthine, translabyrinthine or transcochlear maximizing the petroclival window. Those bear, however, a greater risk of hearing impairment or facial palsy and normally do not provide enough exposure of Meckel’s cave [95–97].
A partial labyrinthectomy petrous apicectomy combining potential advantages of retro- and translabyrinthine corridors has also been described as a modification of these approaches [40], but is likely to be too invasive if solely used for biopsies.
Other approaches
A midface degloving approach has been also described to access the anterior skull base [16]. However, approaching Meckel’s cave required sacrifice of the maxillary nerve and the approach itself appears to be invasive in terms of scaring.
Discussion
Historically, approaches to Meckel’s cave have been divided in anterolateral, lateral and posterolateral, comprising frontotemporal extra- or intradural, orbitozygomatic, subtemporal anterior petrosal, presigmoid posterior petrosal and suboccipital approaches [5, 43]. More recently, the anterior-medial route with the help of rod-lens endoscopy is providing minimal-invasive access to this region [70].
Expanse of Meckel’s cave is predominantly determined by the size of the trigeminal ganglion. Its width correlates with the medial to lateral dimension, and its length with the distance from the trigeminal porus to the anterior edge of the trigeminal ganglion [6]. The dura carpeting the floor of the middle fossa, splits at the trigeminal notch in two-sheets that build the layers covering Meckel’s cave and exit through the porus trigeminus posteriorly towards the posterior fossa [3]. The lateral dural wall is formed by the tentorium, whereas the cavernous sinus and the petrolingual ligament, as a continuity of the carotid canal periosteum, constitute the medial wall [2]. Meckel’s cave interconnects the middle and posterior fossa and tumors can spread through these regions [98], creating unphysiological spaces, that should be considered for planning approaches. Content of Meckel’s cave includes the Gasserian ganglion and postganglionic trigeminal rootlets lying in the trigeminal cistern [6]. In most cases, a thin bony lamina is found between trigeminal ganglion and internal carotid artery (ICA), but dehiscence occurred in up to 30% of analyzed specimens in a recent study [6]. The abducens nerve travels in the posterior inferior cavernous sinus, in close vicinity inferior and medial to the TG and Meckel’s cave [43]. Oculomotor and trochlear nerve run superior to the trigeminal ganglion (~ 5–6 mm) [6].
Differential diagnosis of lesions in Meckel’s cave
Decision-making
We have highlighted the anatomic limitations, technical nuances and potential advantages of each route. Especially for biopsies, a small window towards the lesion might be sufficient. A large portion of tumors in Meckel’s cave will have an extra-/intradural location [67], intradural approaches are often not needed. However, case selection has been to date discussed according to the radiological appearance of lesions and their relationship to the dural sheets [2], which is not always feasible when dealing with the indeterminate lesions discussed in this article (Table 1). If a further resection is required, the feasibility of each approach need to be evaluated according to the specific anatomical situation.
Table 1.
Differential diagnosis of lesions within Meckel’s cave
| Benign | Meningioma [61] |
| Benign Schwannoma [61] | |
| Benign melanotic schwannoma [99] | |
| Xanthoma [100] | |
| Lipoma [61] | |
| Neuromuscular hamartoma [33] | |
| Hemangioblastoma [27] | |
| Cavernous hemangioma [63] | |
| Pituitary adenoma [63] | |
| Malignant | Malignant peripheral nerve sheet tumor [63] |
| Primary | Nasal glioma [25] |
| Atypical teratoid-rhabdoid [20] | |
| Intradural chordoma [15] | |
| Chondrosarcoma [63] | |
| Paraganglioma [30] | |
| Rhabdomyosarcoma [63] | |
| Metastatic | |
| Neuroendocrine carcinoma [63] | |
| Adenoid cystic carcinoma [5] | |
| Malignant melanotic schwannoma [23, 61, 101] | |
| Squamous cell carcinoma [63] | |
| Adenocarcinoma [63] | |
| Inflammatory | Sarcoidosis [19, 69] |
| Amyloidoma [22, 24, 28] | |
| IgG4 disease [63] | |
| Necrotizing granulomatous inflammation [63] | |
| Inflammatory pseudotumor [63] | |
| Hematologic malignancies | Primary malignant lymphoma [26] |
| Multiple myeloma [32] | |
| NK/T lymphoma [63] | |
| Diffuse B-cell lymphoma* | |
| Plasmacytoma [63] | |
| Marginal zone lymphoma [63] | |
| Chronic eosinophilic leukemia [63] | |
| Lymphoplasmocytic lymphoma [63] | |
| Non-Hodgkin lymphoma [63] | |
| Cystic | Arachnoid cyst [5, 21, 34, 61, 64] |
| Epidermoid cyst [17, 29] | |
| Meningoceles [102] | |
*Illustrative case report presented in this article
Tumor consistency is important, as hard, fibrous tumors might require a wider exposure, than cystic or soft tumors, where a narrow approach could be sufficient [49]. Thorough imaging with MRI and CT is therefore essential. Cavernous sinus invasion is suspicious of meningioma or hemangiopericytoma [2]. Hence, an approach where further resection is possible should be chosen. Tumor extension might be the most important factor towards surgery planning of these lesions. Patient’s morbidity and age might steer surgeons towards only biopsing lesions, or simply decompressing important neurovascular structures. Finally, the surgeon’s experience will always lead the discussion. The available equipment and capacities of each institution will also play a role in decision-making. However, whatever skull base approach is applied, it has to be studied in detail and performed with experience to achieve excellent results.
The endoscopic endonasal approach provides safe access to Meckel’s cave [7], with the transpterygoidal route supported by the most clinical reporting. If needed, the possibility for further tumor removal is given. The discussed approaches should, however, be seen as complementary and not competitive [73], since each one of them carries its own risks and advantages. Even though newly described endoscopic approaches appear promising, clinical experiences remain to be reported and an advanced anatomical knowledge of the neurovascular array within and surrounding the skull base is of utmost priority to assure safety during and after procedures. Hence, outcome reports from clinical series are further needed and case selection should be thoroughly discussed (Table 2).
Table 2.
Outline of available approaches highlighting advantages and risks as well as potential complications
| Portion MC access | Advantages | Structures at risk/complications | Limits | ||
|---|---|---|---|---|---|
| Anterio-medial | Transpterygoid | Antero-medial inferior | No brain retraction | CSF leak, vidian nerve/artery, corneal keratopathy, internal carotid artery | Content infratemporal fossa, region lateral and posterior to the GG |
| Transantral/-maxillary | Antero-lateral | Less ICA/PPF manipulation | Oro-antral fistula, nasolacrimal duct | Posterior fossa | |
| Transorbital | Superior and anterolateral | Limited temporal retraction, no manipulation of PPF content | Orbital content, cranial nerves, M. levator palpebrae, CSF leak and pulsatile exopthalmus | Region medial to V1, posterior to ICA | |
| Percutaneous | Foramen rotundum | Minimal invasive | Internal maxillary artery, cranial nerves, e.g. trigeminal and oculomotor nerves | Lack of surgical field visualization | |
| Antero-lateral | Pterional and orbitozygomatic extension | Antero-lateral-superior | Standard skull base surgery approach | Cranial nerve injury (III, IV, VI), temporal muscle disruption/translocation brain retraction | Inferior portion of MC |
| Lateral | Anterior petrosectomy | Lateral, dorsal | Posterior fossa extension, if required | Brain retraction, wide craniotomy, tentorial division, otologic structures, superior petrosal vein | Lower edge porus trigeminus, petrous ICA, inferior petrosal vein |
| Posterior | Retrosigmoid-suprameatal | Dorso-medial | Small craniotomy | Cranial nerve injury (VII-VIII), sinus sigmoideus, cerebellum retraction | Middle fossa |
CSF cerebral spinal fluid, ICA internal carotid artery, GG Gasserian ganglion, MC Meckel’s cave, PPF pterygopalatine fossa
Limitations
The amount of data available in the literature is by now immense. Our description is limited by the amount of data that is possible to include in a review article. We hope, however, to have provided a practical review of 360-degree approaches to Meckel’s cave, encouraging critical thinking and evaluation of lesions.
Conclusions
This work, in an effort to shed light on the various routes to this region, provides an overview of the variance of approaches for reaching Meckel’s cave. Anatomical landmarks and their variations, as well as the disease extension, are essential when planning a surgical approach to Meckel’s cave. For lesions especially in the anterior, inferior and medial compartment of Meckel’s cave, the extended endoscopic endonasal transpterygoidal approach is an excellent approach for targeting these lesions [69]. Numerous of these approaches are complementary to each other. Hence, open approaches are to be selected when necessary.
It is clear that skull base surgeons should learn and study the different approaches and include them in their surgical armamentarium, to provide the safest route according to the underlying pathology.
Electronic supplementary material
(MP4 96372 kb)
Acknowledgments
We would like to thank Paula Frasch for her contribution in creating Fig. 1.
Funding Information
Open Access funding provided by Projekt DEAL.
Compliance with ethical standards
Conflict of interest
Dr. Prevedello is a consultant for Medtronic, Integra and Stryker; has received honoraria from Mizuho and has a royalty agreement with Mizuho, KLS-Martin and ACE Medical. Dr. Carrau is a consultant for Medtronic. The other authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Ethical statement and informed consent
For this type of systematic review, formal ethic committee consent is not required. Written informed patient consent for the illustrative case was acquired.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kawase T, Toya S, Shiobara R, Mine T. Transpetrosal approach for aneurysms of the lower basilar artery. J Neurosurg. 1985;63:857–861. doi: 10.3171/jns.1985.63.6.0857. [DOI] [PubMed] [Google Scholar]
- 2.Muto J, Kawase T, Yoshida K. Meckel's cave tumors: relation to the meninges and minimally invasive approaches for surgery: anatomic and clinical studies. Neurosurgery. 2010;67:291–298. doi: 10.1227/01.NEU.0000382967.84940.52. [DOI] [PubMed] [Google Scholar]
- 3.Seoane E, Rhoton AL., Jr Suprameatal extension of the retrosigmoid approach: microsurgical anatomy. Neurosurgery. 1999;44:553–560. doi: 10.1097/00006123-199903000-00065. [DOI] [PubMed] [Google Scholar]
- 4.Inoue T, Rhoton AL, Jr, Theele D, Barry ME. Surgical approaches to the cavernous sinus: a microsurgical study. Neurosurgery. 1990;26:903–932. doi: 10.1097/00006123-199006000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Kassam AB, Prevedello DM, Carrau RL, Snyderman CH, Gardner P, Osawa S, et al. The front door to meckel's cave: an anteromedial corridor via expanded endoscopic endonasal approach- technical considerations and clinical series. Neurosurgery. 2009;64:71–82. doi: 10.1227/01.NEU.0000335162.36862.54. [DOI] [PubMed] [Google Scholar]
- 6.Arslan M, Deda H, Avci E, Elhan A, Tekdemir I, Tubbs RS, Silav G, Yilmaz E, Baskaya MK. Anatomy of Meckel's cave and the trigeminal ganglion: anatomical landmarks for a safer approach to them. Turk Neurosurg. 2012;22:317–323. doi: 10.5137/1019-5149.JTN.5213-11.1. [DOI] [PubMed] [Google Scholar]
- 7.Fortes FS, Sennes LU, Carrau RL, Brito R, Ribas GC, Yasuda A, Rodrigues AJ Jr, Snyderman CH, Kassam AB. Endoscopic anatomy of the pterygopalatine fossa and the transpterygoid approach: development of a surgical instruction model. Laryngoscope. 2008;118:44–49. doi: 10.1097/MLG.0b013e318155a492. [DOI] [PubMed] [Google Scholar]
- 8.Samii M, Tatagiba M, Carvalho GA. Retrosigmoid intradural suprameatal approach to Meckel's cave and the middle fossa: surgical technique and outcome. J Neurosurg. 2000;92:235–241. doi: 10.3171/jns.2000.92.2.0235. [DOI] [PubMed] [Google Scholar]
- 9.Taha JM, Tew JM, Jr, van Loveren HR. Keller JT, el-Kalliny M: comparison of conventional and skull base surgical approaches for the excision of trigeminal neurinomas. J Neurosurg. 1995;82:719–725. doi: 10.3171/jns.1995.82.5.0719. [DOI] [PubMed] [Google Scholar]
- 10.Truong HQ, Sun X, Celtikci E, Borghei-Razavi H, Wang EW, Snyderman CH, et al. Endoscopic anterior transmaxillary "transalisphenoid" approach to Meckel's cave and the middle cranial fossa: an anatomical study and clinical application. J Neurosurg. 2018;130:227–237. doi: 10.3171/2017.8.JNS171308. [DOI] [PubMed] [Google Scholar]
- 11.Alfieri A, Jho HD, Schettino R, Tschabitscher M. Endoscopic endonasal approach to the pterygopalatine fossa: anatomic study. Neurosurgery. 2003;52:374–378–378–380. doi: 10.1227/01.neu.0000044562.73763.00. [DOI] [PubMed] [Google Scholar]
- 12.Cavallo LM, Cappabianca P, Galzio R, Iaconetta G, de Divitiis E, Tschabitscher M. Endoscopic transnasal approach to the cavernous sinus versus transcranial route: anatomic study. Neurosurgery. 2005;56:379–389. doi: 10.1227/01.neu.0000156548.30011.d4. [DOI] [PubMed] [Google Scholar]
- 13.Dolci RL, Upadhyay S, Ditzel Filho LF, Fiore ME, Buohliqah L, Lazarini PR, et al. Endoscopic endonasal study of the cavernous sinus and quadrangular space: Anatomic relationships. Head Neck. 2016;38(Suppl 1):E1680–E1687. doi: 10.1002/hed.24301. [DOI] [PubMed] [Google Scholar]
- 14.Hofstetter CP, Singh A, Anand VK, Kacker A, Schwartz TH. The endoscopic, endonasal, transmaxillary transpterygoid approach to the pterygopalatine fossa, infratemporal fossa, petrous apex, and the Meckel cave. J Neurosurg. 2010;113:967–974. doi: 10.3171/2009.10.JNS09157. [DOI] [PubMed] [Google Scholar]
- 15.Akay A, Gode S, Cagli MS (2017) Neuronavigation-guided endoscopic endonasal excision of schwannoma-like chordoma of the Meckel's cave: a case report. Turk Neurosurg [DOI] [PubMed]
- 16.Allibone JB, Casey AT, Powell M, Cheeseman AD. The midface degloving approach for intracranial tumours. Br J Neurosurg. 2001;15:109–115. doi: 10.1080/02688690120036784. [DOI] [PubMed] [Google Scholar]
- 17.Arai A, Sasayama T, Koyama J, Fujita A, Hosoda K, Kohmura E. Epidermoid cyst in Meckel's cave with unusual computed tomography and magnetic resonance imaging findings. Case report. Neurol Med Chir (Tokyo) 2010;50:701–704. doi: 10.2176/nmc.50.701. [DOI] [PubMed] [Google Scholar]
- 18.Arishima H, Sindou M. Benefits and pitfalls of percutaneous biopsy for cavernous sinus tumors through the foramen ovale: two case reports. Minim Invasive Neurosurg. 2010;53:194–197. doi: 10.1055/s-0030-1263114. [DOI] [PubMed] [Google Scholar]
- 19.Bangiyev L, Kornacki S, Mikolaenko I. Rare isolated trigeminal nerve sarcoidosis mimicking schwannoma. Clin Imaging. 2015;39:133–135. doi: 10.1016/j.clinimag.2014.08.012. [DOI] [PubMed] [Google Scholar]
- 20.Beschorner R, Mittelbronn M, Koerbel A, Ernemann U, Thal DR, Scheel-Walter HG, Meyermann R, Tatagiba M. Atypical teratoid-rhabdoid tumor spreading along the trigeminal nerve. Pediatr Neurosurg. 2006;42:258–263. doi: 10.1159/000092366. [DOI] [PubMed] [Google Scholar]
- 21.Bigder MG, Helmi A, Kaufmann AM: Trigeminal neuropathy associated with an enlarging arachnoid cyst in Meckel's cave: case report, management strategy and review of the literature. Acta Neurochir, 2017 [DOI] [PubMed]
- 22.Bookland MJ, Bagley CA, Schwarz J, Burger PC, Brem H. Intracavernous trigeminal ganglion amyloidoma: case report. Neurosurgery. 2007;60:E574–discussion E574. doi: 10.1227/01.NEU.0000255361.32689.B3. [DOI] [PubMed] [Google Scholar]
- 23.Falavigna A, Borba LA, Ferraz FA, Almeida GC, Krindges Junior JV. Primary melanoma of Meckel's cave: case report. Arq Neuropsiquiatr. 2004;62:353–356. doi: 10.1590/s0004-282x2004000200030. [DOI] [PubMed] [Google Scholar]
- 24.Gultasli N, van den Hauwe L, Bruneau M, D'Haene N, Delpierre I, Baleriaux D. Bilateral Meckel's cave amyloidoma: a case report. J Neuroradiol. 2012;39:119–122. doi: 10.1016/j.neurad.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 25.Kasliwal MK, Anand VK, Lavi E, Schwartz TH. Endoscopic management of a rare case of nasal glioma in Meckel's cave in an adult: case report. Minim Invasive Neurosurg. 2010;53:191–193. doi: 10.1055/s-0030-1262812. [DOI] [PubMed] [Google Scholar]
- 26.Kinoshita M, Izumoto S, Oshino S, Nonaka M, Moriuchi S, Maruno M, et al. Primary malignant lymphoma of the trigeminal region treated with rapid infusion of high-dose MTX and radiation: case report and review of the literature. Surg Neurol. 2003;60:343–348. doi: 10.1016/s0090-3019(02)01046-7. [DOI] [PubMed] [Google Scholar]
- 27.Kord Valeshabad A, Xiao L, Amin-Hanjani S, Alsadi A, Valyi-Nagy T, Kim J. Sporadic Hemangioblastoma of the cavernous sinus and Meckel's cave. J Neurol Surg Rep. 2018;79:e98–e102. doi: 10.1055/s-0038-1676455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Menetti F, Bartolomei I, Ambrosini-Spaltro A, Salvi F, Agati R, Leonardi M. Amyloidoma involving the orbit, Meckel's cave and Infratemporal Fossa: 3T MRI findings. Neuroradiol J. 2009;22:41–47. doi: 10.1177/197140090902200107. [DOI] [PubMed] [Google Scholar]
- 29.Nadkarni T, Dindorkar K, Muzumdar D, Goel A. Epidermoid tumor within Meckel's cave--case report. Neurol Med Chir (Tokyo) 2000;40:74–76. doi: 10.2176/nmc.40.74. [DOI] [PubMed] [Google Scholar]
- 30.Prajsnar A, Balak N, Walter GF, Stan AC, Deinsberger W, Tapul L, et al. Recurrent paraganglioma of Meckel's cave: case report and a review of anatomic origin of paragangliomas. Surg Neurol Int. 2011;2:45. doi: 10.4103/2152-7806.79763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Seckin H, Patel N, Avci E, Dempsey RJ, Baskaya MK. Removal of cavernous malformation of the Meckel's cave by extradural pterional approach using Heros muscle dissection technique. Surg Neurol. 2009;72:733–736. doi: 10.1016/j.surneu.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 32.Thiruvengadam SS, Prayson RA. Multiple myeloma presenting with unilateral abducens and trigeminal nerve palsies. J Clin Neurosci. 2016;26:143–144. doi: 10.1016/j.jocn.2015.10.015. [DOI] [PubMed] [Google Scholar]
- 33.Tobias S, Kim CH, Sade B, Staugaitis SM, Lee JH. Neuromuscular hamartoma of the trigeminal nerve in an adult. Acta Neurochir (Wien) 2006;148:83–87. doi: 10.1007/s00701-005-0642-z. [DOI] [PubMed] [Google Scholar]
- 34.Worner BA, Noll M, Rahim T, Fink U, Oeckler R. Recurrent arachnoid cyst of Meckel's cave mimicking a brain stem ischaemia Report of a rare case. Zentralbl Neurochir. 2003;64:76–79. doi: 10.1055/s-2003-40376. [DOI] [PubMed] [Google Scholar]
- 35.Yong XZ, Dillon J, Smith P, Salinas-La Rosa C, Jhamb A. Novel CT-guided biopsy of isolated perineural spread of adenoid cystic carcinoma along the trigeminal nerve masquerading as chronic trigeminal neuropathy. J Med Imaging Radiat Oncol. 2017;61:77–81. doi: 10.1111/1754-9485.12557. [DOI] [PubMed] [Google Scholar]
- 36.Acerbi F, Broggi M, Gaini SM, Tschabitscher M. Microsurgical endoscopic-assisted retrosigmoid intradural suprameatal approach: anatomical considerations. J Neurosurg Sci. 2010;54:55–63. [PubMed] [Google Scholar]
- 37.Alvernia JE, Sindou MP, Dang ND, Maley JH, Mertens P. Percutaneous approach to the foramen ovale: an anatomical study of the extracranial trajectory with the incorrect trajectories to be avoided. Acta Neurochir. 2010;152:1043–1053. doi: 10.1007/s00701-010-0604-y. [DOI] [PubMed] [Google Scholar]
- 38.Bai ZQ, Cai EY, Wang SQ, Li ZJ, Wang SB. Nasal cavity-maxillary sinus-pterygopalatine fossa-Meckel's cave: a preliminary anatomic study of an endoscopy-based operative approach. Neurosci Bull. 2009;25:376–382. doi: 10.1007/s12264-009-0605-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Barges-Coll J, Fernandez-Miranda JC, Prevedello DM, Gardner P, Morera V, Madhok R, et al. Avoiding injury to the abducens nerve during expanded endonasal endoscopic surgery: anatomic and clinical case studies. Neurosurgery. 2010;67:144–154. doi: 10.1227/01.NEU.0000370892.11284.EA. [DOI] [PubMed] [Google Scholar]
- 40.Chanda A, Nanda A. Partial labyrinthectomy petrous apicectomy approach to the petroclival region: an anatomic and technical study. Neurosurgery. 2002;51:147–159. doi: 10.1097/00006123-200207000-00022. [DOI] [PubMed] [Google Scholar]
- 41.Chanda A, Nanda A. Retrosigmoid intradural suprameatal approach: advantages and disadvantages from an anatomical perspective. Neurosurgery. 2006;59:1–6. doi: 10.1227/01.NEU.0000220673.79877.30. [DOI] [PubMed] [Google Scholar]
- 42.Chang SW, Wu A, Gore P, Beres E, Porter RW, Preul MC, et al. Quantitative comparison of Kawase's approach versus the retrosigmoid approach: implications for tumors involving both middle and posterior fossae. Neurosurgery. 2009;64:44–51. doi: 10.1227/01.NEU.0000334410.24984.DD. [DOI] [PubMed] [Google Scholar]
- 43.de Jesus O. Petrous apex region. Surgical anatomy, lesions, and operative techniques. P R Health Sci J. 1996;15:107–112. [PubMed] [Google Scholar]
- 44.Dolci RLL, Ditzel Filho LFS, Goulart CR, Upadhyay S, Buohliqah L, Lazarini PR, Prevedello DM, Carrau RL. Anatomical nuances of the internal carotid artery in relation to the quadrangular space. J Neurosurg. 2018;128:174–181. doi: 10.3171/2016.10.JNS16381. [DOI] [PubMed] [Google Scholar]
- 45.Ebner FH, Koerbel A, Kirschniak A, Roser F, Kaminsky J, Tatagiba M. Endoscope-assisted retrosigmoid intradural suprameatal approach to the middle fossa: anatomical and surgical considerations. Eur J Surg Oncol. 2007;33:109–113. doi: 10.1016/j.ejso.2006.09.036. [DOI] [PubMed] [Google Scholar]
- 46.Ebner FH, Koerbel A, Roser F, Hirt B, Tatagiba M. Microsurgical and endoscopic anatomy of the retrosigmoid intradural suprameatal approach to lesions extending from the posterior fossa to the central skull base. Skull Base. 2009;19:319–323. doi: 10.1055/s-0029-1220199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ferrari M, Schreiber A, Mattavelli D, Belotti F, Rampinelli V, Lancini D, Doglietto F, Fontanella MM, Tschabitscher M, Rodella LF, Nicolai P. The inferolateral Transorbital endoscopic approach: a preclinical anatomic study. World Neurosurg. 2016;90:403–413. doi: 10.1016/j.wneu.2016.03.017. [DOI] [PubMed] [Google Scholar]
- 48.Fukushima T. Endoscopy of Meckel's cave, cisterna magna, and cerebellopontine angle technical note. J Neurosurg. 1978;48:302–306. doi: 10.3171/jns.1978.48.2.0302. [DOI] [PubMed] [Google Scholar]
- 49.Jacquesson T, Berhouma M, Tringali S, Simon E, Jouanneau E. Which routes for Petroclival tumors? A Comparison Between the Anterior Expanded Endoscopic Endonasal Approach and Lateral or Posterior Routes. World Neurosurg. 2015;83:929–936. doi: 10.1016/j.wneu.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 50.Jacquesson T, Simon E, Berhouma M, Jouanneau E. Anatomic comparison of anterior petrosectomy versus the expanded endoscopic endonasal approach: interest in petroclival tumors surgery. Surg Radiol Anat. 2015;37:1199–1207. doi: 10.1007/s00276-015-1497-5. [DOI] [PubMed] [Google Scholar]
- 51.Koerbel A, Kirschniak A, Ebner FH, Tatagiba M, Gharabaghi A. The retrosigmoid intradural suprameatal approach to posterior cavernous sinus: microsurgical anatomy. Eur J Surg Oncol. 2009;35:368–372. doi: 10.1016/j.ejso.2008.02.011. [DOI] [PubMed] [Google Scholar]
- 52.Marcati E, Andaluz N, Froelich SC, Zimmer LA, Leach JL, Fernandez-Miranda JC, et al. (2018) Paratrigeminal, Paraclival, Precavernous, or all of the above? A circumferential anatomical study of the C3-C4 transitional segment of the internal carotid artery. Oper Neurosurg (Hagerstown) 14(4):432–440 [DOI] [PubMed]
- 53.Oyama K, Tahara S, Hirohata T, Ishii Y, Prevedello DM, Carrau RL, et al. Surgical anatomy for the endoscopic Endonasal approach to the Ventrolateral Skull Base. Neurol Med Chir (Tokyo) 2017;57:534–541. doi: 10.2176/nmc.ra.2017-0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Priddy BH, Nunes CF, Beer-Furlan A, Carrau R, Dallan I, Prevedello DM. A side door to Meckel's cave: anatomic feasibility study for the lateral Transorbital approach. Oper Neurosurg (Hagerstown) 2017;13:614–621. doi: 10.1093/ons/opx042. [DOI] [PubMed] [Google Scholar]
- 55.Rigante L, Herlan S, Tatagiba MS, Stanojevic M, Hirt B, Ebner FH. Petrosectomy and topographical anatomy in traditional Kawase and posterior Intradural petrous Apicectomy (PIPA) approach: an anatomical study. World Neurosurg. 2016;86:93–102. doi: 10.1016/j.wneu.2015.08.083. [DOI] [PubMed] [Google Scholar]
- 56.Roche PH, Troude L, Peyriere H, Noudel R. The epidural approach to the Meckel's cave: a how I do it. Acta Neurochir. 2014;156:217–220. doi: 10.1007/s00701-013-1916-5. [DOI] [PubMed] [Google Scholar]
- 57.Van Rompaey J, Suruliraj A, Carrau R, Panizza B, Solares CA. Meckel's cave access: anatomic study comparing the endoscopic transantral and endonasal approaches. Eur Arch Otorhinolaryngol. 2014;271:787–794. doi: 10.1007/s00405-013-2581-2. [DOI] [PubMed] [Google Scholar]
- 58.Wang J, Bidari S, Inoue K, Yang H, Rhoton A., Jr Extensions of the sphenoid sinus: a new classification. Neurosurgery. 2010;66:797–816. doi: 10.1227/01.NEU.0000367619.24800.B1. [DOI] [PubMed] [Google Scholar]
- 59.Youssef S, Kim EY, Aziz KM, Hemida S, Keller JT, van Loveren HR. The subtemporal interdural approach to dumbbell-shaped trigeminal schwannomas: cadaveric prosection. Neurosurgery. 2006;59:270–277. doi: 10.1227/01.NEU.0000227590.70254.02. [DOI] [PubMed] [Google Scholar]
- 60.Zhang X, Tabani H, El-Sayed I, Russell M, Feng X, Benet A. The endoscopic Endonasal Transmaxillary approach to Meckel's cave through the inferior orbital fissure. Oper Neurosurg (Hagerstown) 2017;13:367–373. doi: 10.1093/ons/opx009. [DOI] [PubMed] [Google Scholar]
- 61.Beck DW, Menezes AH. Lesions in Meckel's cave: variable presentation and pathology. J Neurosurg. 1987;67:684–689. doi: 10.3171/jns.1987.67.5.0684. [DOI] [PubMed] [Google Scholar]
- 62.Goel A. Infratemporal fossa interdural approach for trigeminal neurinomas. Acta Neurochir. 1995;136:99–102. doi: 10.1007/BF01411444. [DOI] [PubMed] [Google Scholar]
- 63.Hughes JD, Kapurch J, Van Gompel JJ, Meyer FB, Pollock BE, Atkinson J et al (2017) Diagnosis and outcome of biopsies of indeterminate lesions of the cavernous sinus and Meckel's cave: a retrospective case series in 85 patients. Neurosurgery [DOI] [PubMed]
- 64.Isaacson B, Coker NJ, Vrabec JT, Yoshor D, Oghalai JS. Invasive cerebrospinal fluid cysts and cephaloceles of the petrous apex. Otol Neurotol. 2006;27:1131–1141. doi: 10.1097/01.mao.0000244353.26954.71. [DOI] [PubMed] [Google Scholar]
- 65.Jeon C, Hong CK, Woo KI, Hong SD, Nam DH, Lee JI, et al. (2018) Endoscopic transorbital surgery for Meckel's cave and middle cranial fossa tumors: surgical technique and early results. J Neurosurg 1:1–10 [DOI] [PubMed]
- 66.Kawase T, Shiobara R, Toya S. Anterior transpetrosal-transtentorial approach for sphenopetroclival meningiomas: surgical method and results in 10 patients. Neurosurgery. 1991;28:869–875. [PubMed] [Google Scholar]
- 67.Mariniello G, de Divitiis O, Caranci F, Dones F, Maiuri F (2017) Parasellar Schwannomas: extradural vs extra-Intradural surgical approach. Oper Neurosurg (Hagerstown) [DOI] [PubMed]
- 68.Nakamura M, Krauss JK. Image-guided resection of small lesions in the cavernous sinus and Meckel's cave. Eur J Surg Oncol. 2010;36:208–213. doi: 10.1016/j.ejso.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 69.Palejwala SK, Zhao F, Lanker KC, Sivakumar W, Takasumi Y, Griffiths CF, Barkhoudarian G, Kelly DF. Imaging-ambiguous lesions of Meckel's cave-utility of endoscopic Endonasal Transpterygoid biopsy. World Neurosurg. 2018;118:e346–e355. doi: 10.1016/j.wneu.2018.06.190. [DOI] [PubMed] [Google Scholar]
- 70.Raza SM, Donaldson AM, Mehta A, Tsiouris AJ, Anand VK, Schwartz TH. Surgical management of trigeminal schwannomas: defining the role for endoscopic endonasal approaches. Neurosurg Focus. 2014;37:E17. doi: 10.3171/2014.7.FOCUS14341. [DOI] [PubMed] [Google Scholar]
- 71.Wang X, Zhang X, Hu F, Yu Y, Gu Y, Xie T, et al. Image-guided endoscopic Endonasal Transmaxillary Transpterygoid approach to Meckel's cave. Turk Neurosurg. 2016;26:309–314. doi: 10.5137/1019-5149.JTN.6430-12.0. [DOI] [PubMed] [Google Scholar]
- 72.Cheung SW, Jackler RK, Pitts LH, Gutin PH. Interconnecting the posterior and middle cranial fossae for tumors that traverse Meckel's cave. Am J Otol. 1995;16:200–208. [PubMed] [Google Scholar]
- 73.Hardesty DA, Montaser AS, Carrau RL, Prevedello DM. Limits of endoscopic endonasal transpterygoid approach to cavernous sinus and Meckel's cave. J Neurosurg Sci. 2018;62:332–338. doi: 10.23736/S0390-5616.18.04330-8. [DOI] [PubMed] [Google Scholar]
- 74.Jouanneau E, Simon E, Jacquesson T, Sindou M, Tringali S, Messerer M, Berhouma M. The endoscopic endonasal approach to the Meckel's cave tumors: surgical technique and indications. World Neurosurg. 2014;82:S155–S161. doi: 10.1016/j.wneu.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 75.Roche PH, Lubrano VF, Noudel R. How I do it: epidural anterior petrosectomy. Acta Neurochir. 2011;153:1161–1167. doi: 10.1007/s00701-011-1010-9. [DOI] [PubMed] [Google Scholar]
- 76.Simal Julian JA, Miranda Lloret P, Garcia Pinero A, Botella Asuncion C. Full endoscopic endonasal suprapetrous approach to Meckel's cave. Acta Neurochir. 2014;156:1623–1626. doi: 10.1007/s00701-014-2113-x. [DOI] [PubMed] [Google Scholar]
- 77.Kasemsiri P, Solares CA, Carrau RL, Prosser JD, Prevedello DM, Otto BA, Old M, Kassam AB. Endoscopic endonasal transpterygoid approaches: anatomical landmarks for planning the surgical corridor. Laryngoscope. 2013;123:811–815. doi: 10.1002/lary.23697. [DOI] [PubMed] [Google Scholar]
- 78.Kassam AB, Vescan AD, Carrau RL, Prevedello DM, Gardner P, Mintz AH, Snyderman CH, Rhoton AL. Expanded endonasal approach: vidian canal as a landmark to the petrous internal carotid artery. J Neurosurg. 2008;108:177–183. doi: 10.3171/JNS/2008/108/01/0177. [DOI] [PubMed] [Google Scholar]
- 79.Kassam AB, Gardner P, Snyderman C, Mintz A, Carrau R. Expanded endonasal approach: fully endoscopic, completely transnasal approach to the middle third of the clivus, petrous bone, middle cranial fossa, and infratemporal fossa. Neurosurg Focus. 2005;19:E6. [PubMed] [Google Scholar]
- 80.Kaen A, Cardenas Ruiz-Valdepenas E, Di Somma A, Esteban F, Marquez Rivas J, Ambrosiani Fernandez J (2018) Refining the anatomic boundaries of the endoscopic endonasal transpterygoid approach: the "VELPPHA area" concept. J Neurosurg 131(3):911–919 [DOI] [PubMed]
- 81.Iwanaga J, Badaloni F, Laws T, Oskouian RJ, Tubbs RS. Anatomic study of Extracranial needle trajectory using Hartel technique for percutaneous treatment of trigeminal neuralgia. World Neurosurg. 2018;110:e245–e248. doi: 10.1016/j.wneu.2017.10.140. [DOI] [PubMed] [Google Scholar]
- 82.Sindou M, Chavez JM, Saint Pierre G, Jouvet A. Percutaneous biopsy of cavernous sinus tumors through the foramen ovale. Neurosurgery. 1997;40:106–110. [PubMed] [Google Scholar]
- 83.Messerer M, Dubourg J, Saint-Pierre G, Jouanneau E, Sindou M. Percutaneous biopsy of lesions in the cavernous sinus region through the foramen ovale: diagnostic accuracy and limits in 50 patients. J Neurosurg. 2012;116:390–398. doi: 10.3171/2011.10.JNS11783. [DOI] [PubMed] [Google Scholar]
- 84.Al-Mefty O, Anand VK. Zygomatic approach to skull-base lesions. J Neurosurg. 1990;73:668–673. doi: 10.3171/jns.1990.73.5.0668. [DOI] [PubMed] [Google Scholar]
- 85.Jian FZ, Santoro A, Innocenzi G, Wang XW, Liu SS, Cantore G. Frontotemporal orbitozygomatic craniotomy to exposure the cavernous sinus and its surrounding regions. Microsurgical anatomy. J Neurosurg Sci. 2001;45:19–28. [PubMed] [Google Scholar]
- 86.Dolenc VV. Frontotemporal epidural approach to trigeminal neurinomas. Acta Neurochir. 1994;130:55–65. doi: 10.1007/BF01405503. [DOI] [PubMed] [Google Scholar]
- 87.Day JD, Fukushima T, Giannotta SL. Microanatomical study of the extradural middle fossa approach to the petroclival and posterior cavernous sinus region: description of the rhomboid construct. Neurosurgery. 1994;34:1009–1016. doi: 10.1227/00006123-199406000-00009. [DOI] [PubMed] [Google Scholar]
- 88.Kawase T, Shiobara R, Toya S. Middle fossa transpetrosal-transtentorial approaches for petroclival meningiomas. Selective pyramid resection and radicality. Acta Neurochir. 1994;129:113–120. doi: 10.1007/BF01406489. [DOI] [PubMed] [Google Scholar]
- 89.Drake CG. Surgical treatment of ruptured aneurysms of the basilar artery. Experience with 14 cases. J Neurosurg. 1965;23:457–473. doi: 10.3171/jns.1965.23.5.0457. [DOI] [PubMed] [Google Scholar]
- 90.Spetzler RF, Hamilton MG, Daspit CP. Petroclival lesions. Clin Neurosurg. 1994;41:62–82. [PubMed] [Google Scholar]
- 91.Sanna M, Bacciu A, Pasanisi E, Taibah A, Piazza P. Posterior petrous face meningiomas: an algorithm for surgical management. Otol Neurotol. 2007;28:942–950. doi: 10.1097/MAO.0b013e31814b23f0. [DOI] [PubMed] [Google Scholar]
- 92.Goel A, Nadkarni T. Basal lateral subtemporal approach for trigeminal neurinomas: report of an experience with 18 cases. Acta Neurochir. 1999;141:711–719. doi: 10.1007/s007010050366. [DOI] [PubMed] [Google Scholar]
- 93.Cushing H: Tumors of the nervus acusticus and the syndrome of the cerebellopontine angle: Philadelphia Saunders, 1917
- 94.O'Donoghue GM, O'Flynn P. Endoscopic anatomy of the cerebellopontine angle. Am J Otol. 1993;14:122–125. [PubMed] [Google Scholar]
- 95.Bambakidis NC, Kakarla UK, Kim LJ, Nakaji P, Porter RW, Daspit CP, et al. Evolution of surgical approaches in the treatment of petroclival meningiomas: a retrospective review. Neurosurgery. 2007;61:202–209. doi: 10.1227/01.neu.0000303218.61230.39. [DOI] [PubMed] [Google Scholar]
- 96.Siwanuwatn R, Deshmukh P, Figueiredo EG, Crawford NR, Spetzler RF, Preul MC. Quantitative analysis of the working area and angle of attack for the retrosigmoid, combined petrosal, and transcochlear approaches to the petroclival region. J Neurosurg. 2006;104:137–142. doi: 10.3171/jns.2006.104.1.137. [DOI] [PubMed] [Google Scholar]
- 97.Xu F, Karampelas I, Megerian CA, Selman WR, Bambakidis NC. Petroclival meningiomas: an update on surgical approaches, decision making, and treatment results. Neurosurg Focus. 2013;35:E11. doi: 10.3171/2013.9.FOCUS13319. [DOI] [PubMed] [Google Scholar]
- 98.Cushing H, Eisenhardt L: Meningiomas: Their Classification, Regional Behavior, Life History, and Surgical End Results.: Springfield, Illinois, Charles C Thomas, 1938
- 99.Quencer RM, Stokes NA, Wolfe D, Page LK. Melanotic nerve sheath tumor of the gasserian ganglion and trigeminal nerve. AJR Am J Roentgenol. 1979;133:142–144. doi: 10.2214/ajr.133.1.142. [DOI] [PubMed] [Google Scholar]
- 100.Kimura H, Oka K, Nakayama Y, Tomonaga M. Xanthoma in Meckel's cave. A case report. Surg Neurol. 1991;35:317–320. doi: 10.1016/0090-3019(91)90012-x. [DOI] [PubMed] [Google Scholar]
- 101.Levy WJ, Ansbacher L, Byer J, Nutkiewicz A, Fratkin J. Primary malignant nerve sheath tumor of the gasserian ganglion: a report of two cases. Neurosurgery. 1983;13:572–576. doi: 10.1227/00006123-198311000-00015. [DOI] [PubMed] [Google Scholar]
- 102.Alobaid A, Schaeffer T, Virojanapa J, Dehdashti AR. Rare cause of trigeminal neuralgia: Meckel's cave meningocele. Acta Neurochir. 2015;157:1183–1186. doi: 10.1007/s00701-015-2434-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(MP4 96372 kb)