Abstract
Purpose
The amount of studies performed regarding a link between socioeconomic status (SES) and fatal outcome after traumatic injury is limited. Most research is focused on work-related injuries without taking other important characteristics into account. The aim of this study is to examine the association between SES and outcome after traumatic injury.
Methods
The study involved polytrauma patients [Injury Severity Score (ISS) ≥ 16] admitted to the Amsterdam University Medical Center (location VUmc) and Northwest Clinics Alkmaar (level 1 trauma centers). The SES of every patient was based on their postal code and represented with a “status score”. Univariate and multivariable analyses were performed to estimate the association between SES and mortality, length of stay at the hospital and length of stay at the Intensive Care Unit (ICU). Z-statistics were used to determine the difference between the expected and actual survival, based on Trauma Revised Injury Severity Score (TRISS) and PSNL15 (probability of survival based on the Dutch population).
Results
A total of 967 patients were included in this study. The lowest SES group was significantly associated with more penetrating injuries and a younger age (45 years versus 55 years). Additionally, severely injured patients with lower SES were noted to have a prolonged stay at the ICU. Furthermore, differences were found in the expected and observed survival, especially for the lower SES groups.
Conclusion
Polytrauma patients with lower SES have more often penetrating injuries, are younger and have a longer stay at the ICU. No association was found between SES and length of hospital stay and neither between SES and mortality.
Keywords: Socioeconomic status, Severe traumatic injury, Polytrauma
Introduction
Trauma is one of the main causes of death in the Netherlands, especially in the younger population, and the number of trauma victims is increasing significantly. In 2015, more than 80,000 patients have been admitted to a Dutch hospital due to traumatic injury [1]. The majority of these injuries were related to fall accidents, road traffic accidents and suicide [2, 3]. Previous research suggested that there was an association between the social characteristics of the patients and their outcome after traumatic injury. For example, patients with a lower intelligence level, specific racial-ethnic background and no insurance policy had a higher risk on hospitalization and mortality due to trauma [4–10].
However, there is a scarcity of studies which examined the association between socioeconomic status (SES) and outcome after traumatic injury. Moreover, most research is focused on work-related injuries and does not take other important characteristics, like comorbidity of the patient, into account. In addition, nearly all reviews used only the education level to determine SES, whereas other indicators, such as household income and employment status, should be taken into consideration as well [11, 12].
The aim of this study is to examine whether there is an association between the SES and the clinical outcome of polytrauma patients after injury. Examining the association between SES and traumatic injuries can be useful for public health organizations in guiding their allocation of resources and to prioritize the implementation of preventative measures in specific neighborhoods.
Methods
Study design
A cross-sectional analysis was performed, including data from polytrauma patients [Injury Severity Score (ISS) ≥ 16] who were admitted to the level 1 trauma centers of the Amsterdam University Medical Center (Amsterdam UMC, location VUmc) and Northwest Clinics Alkmaar (NCA) between 1-1-2015 and 1-1-2018. Polytrauma patients were selected using the database of our trauma region (Network Acute Care Northwest), which is part of the National Trauma Registry (NTR) of the Netherlands. In the NTR, injuries are classified by the Abbreviated Injury Scale (AIS) 2005, update 2008 [13, 14]. All transport modes were included (ambulance, helicopter or self-referral). In addition, patients from all ages, gender and ethnicities are included.
Data extraction
Patient characteristics, type of injury (blunt versus penetrating) and mechanism of injury (low and high energy falls, different types of road accidents, burning, shot or stabbing accidents and drowning) of each patient was extracted from the NTR. Mechanism of injury was reclassified into three main groups: traffic accidents (1), fall accidents (2) and others (3). In addition to the ISS and AIS, data concerning patients’ comorbidity status level were collected, including their Anesthesiologists Physical Status (ASA-PS) score [15, 16]. The ASA-PS classification system was used to determine the level of comorbidity based on the medical history before the time of injury. For this analysis, the variable was recoded into either a mild (ASA-PS ≤ 2) or severe (ASA-PS ≥ 3) comorbidity status before injury. Clinically relevant outcome measures included in-hospital mortality, length of stay at the hospital and at the ICU (in days).
Socioeconomic status
Demographic and socioeconomic characteristics of the patients were determined using data from Statistics Netherlands (CBS) and The Dutch Institute for Social Research (SCP). The SES of every district was calculated and characterized by a ‘status score’, where a low status score represents a low SES. These scores included the following four indicators: the average income of people living within the district, the proportion of people with a lower level of education in the district, the proportion of people living with a low income and the proportion of unemployed residents. The study population was then divided into quantiles, based on the national SES [lowest (1)—highest (5)]. Postal code areas with less than 100 inhabitants were not included in this database to preserve the anonymity of the inhabitants and to exclude irrelevant areas such as industrial zones.
Statistical analysis
Chi-squared analyses, one-way analyses of variance (ANOVA) and Kruskal–Wallis analyses were used for demographic and clinical characteristics. Multiple logistic regression and multiple linear regression were used to estimate the association between, respectively, SES and mortality and SES and (log-transformed) length of stay. Adjustments were made for known confounders, such as age, gender, comorbidity level, ISS, type, and mechanism of injury [17].
Additionally, a subanalysis for the probability of survival was performed to determine the difference between predicted mortality and actual mortality. This was determined using the Trauma and Injury Severity Score (TRISS) and the PSNL15 (Probability of survival specified for the Dutch population) [2, 18–21].
Results
Descriptives
A total of 967 patients were included in the study population, 676 patients from VUmc and 291 patients from NCA. Excluded were duplicates and patients with missing data. Missing data were mainly based on absent postal codes and status scores, as well as foreign patients. The study population consisted predominantly of male patients (68.9%) with a median ISS of 22 (range = 59). The five SES groups varied in size between 165 and 232 patients, with overall status scores ranging between − 3.42 and 2.53 (compared with a minimum of − 8.19 and a maximum of 2.93 in the national Dutch database). Most of the patients suffered from blunt trauma (96.2%), mainly due to traffic accidents (42.6%). An overview of baseline characteristics of each group can be found in Table 1.
Table 1.
Patient and injury characteristics by socioeconomic status
| Patient characteristics | Total population (n = 967) | Socioeconomic status | p value | ||||
|---|---|---|---|---|---|---|---|
| 1 (lowest) N = 165 (17.1%) |
2 N = 203 (21.0%) |
3 N = 177 (18.3%) |
4 N = 190 (19.6%) |
5 (highest) N = 232 (24.0%) |
|||
| Age, mean (SD)* | 52 (23) | 45 (21) | 50 (23) | 56 (23) | 53 (25) | 55 (22) | < 0.001b |
| Gender male, n (%) | 666 (68.9%) | 119 (72.7%) | 142 (70.4%) | 118 (66.7%) | 129 (67.9%) | 155 (67.2%) | 0.71c |
| ISS, median (range) | 22 (16–75) | 22 (16–75) | 22 (16–50) | 22 (16–59) | 22 (16–75) | 22 (16–75) | 0.75d |
| Comorbidity level, n (%)a | |||||||
| Severe (III–IV) (versus mild) | 59 (6.1%) | 8 (4.8%) | 10 (4.9%) | 14 (7.9%) | 12 (6.3%) | 15 (6.5%) | 0.73c |
| Cause of injury*, n (%) | 0.013c | ||||||
| Traffic accident | 412 (42.6%) | 41.8% | 47.8% | 36.2% | 45.8% | 50.9% | |
| Falling accident | 376 (38.9%) | 32.7% | 31.5% | 46.9% | 39.5% | 43.1% | |
| Other | 179 (18.5%) | 25.5% | 20.7% | 16.9% | 14.7% | 15.9% | |
| Type of injury*, n (%) | |||||||
| Penetrating (versus blunt) | 29 (3.8%) | 14 (8.5%) | 7 (3.4%) | 7 (4.0%) | 2 (1.1%) | 7 (3.0%) | 0.007c |
| Mortality, n (%) | 230 (23.8%) | 39 (23.6%) | 41 (20.2%) | 45 (25.4%) | 47 (24.7%) | 58 (25%) | 0.74c |
aComorbidity level based on ASA-PS (comorbidity state before injury): mild (ASA-PS ≤ 2) versus severe (ASA-PS ≥ 3)
bOne-way ANOVA
cChi-squared analysis
dKruskal–Wallis analysis
*Statistically significant (p < 0.05)
Univariate analyses showed that the lowest SES group (1) had severe traumatic injuries at a significantly younger age compared to the highest SES group (5) (45 years versus 55 years, p < 0.001). Furthermore, penetrating injuries occurred more frequently in the lowest SES group (1) (8.5% versus 3.0%, p = 0.007).
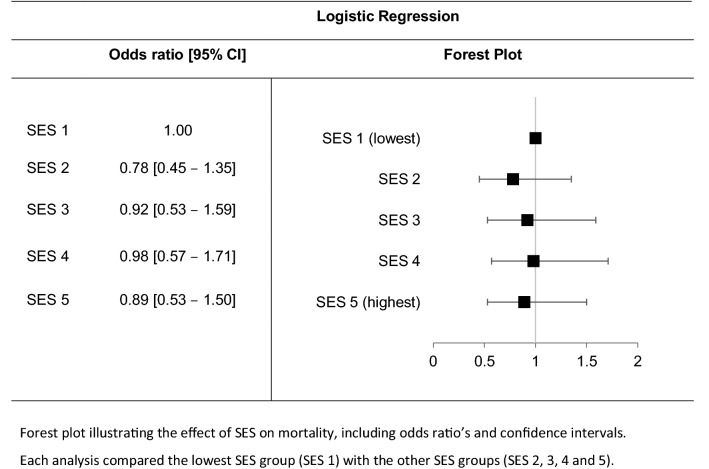
Mortality
Initially, no significant association was found between SES and mortality (Table 1, p = 0.74). Table 2 shows that, after adding covariates to the model, there still was no association between the five SES groups and mortality. Only age, comorbidity level, mechanism of injury, ISS and AIS-head seemed to be significantly related to mortality (p < 0.05).
Table 2.
The effect of SES on mortality
Length of stay
Length of stay at the ICU, however, was significantly related to SES (p = 0.04). Even after using a combined predictor model including SES, age, gender, comorbidity, type of injury, mechanism of injury, ISS and AIS, the results remained significant (p = 0.03). Length of stay at the hospital was not significantly associated with the SES groups (Table 3).
Table 3.
The effect of SES on length of stay at the hospital and at the ICU
| Unstandardized coefficients | p value | [95% CI] | |
|---|---|---|---|
| Length of stay at hospital | |||
| Model 1 | − 0.016 | 0.17 | [− 0.04 to 0.01] |
| Model 2 | − 0.021 | 0.08 | [− 0.04 to 0.00] |
| Length of stay at IC | |||
| Model 1* | − 0.020 | 0.04 | [− 0.04 to 0.00] |
| Model 2* | − 0.020 | 0.03 | [− 0.04 to 0.00] |
Predictors model 1: socioeconomic status only
Predictors model 2: socioeconomic status, age, gender, comorbidity, type of injury, mechanism of injury, ISS and AIS
*Statistically significant (p < 0.05)
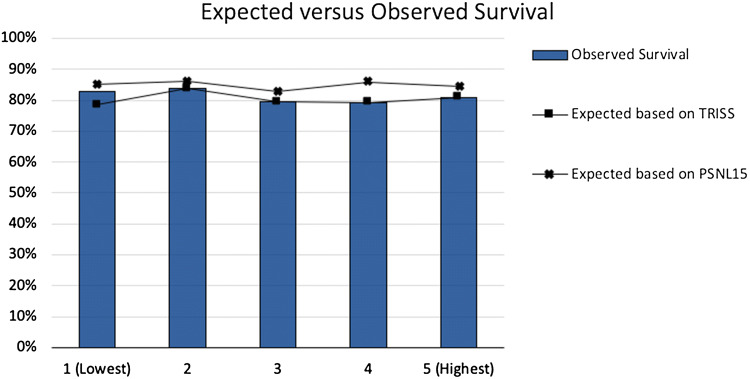
Probability of survival
The subanalysis showed differences between expected survival (based on TRISS and PSNL15) and actual survival. Both the TRISS and the PSNL15 scores do not adequately correspond with the actual survival. The greatest difference between expected and observed survival can be seen in the lowest SES group (1). However, Z scores were only significant for SES 4. Details can be found in Table 4 and Fig. 1.
Table 4.
Differences between observed and expected survival
| Socioeconomic status | |||||
|---|---|---|---|---|---|
| 1 (lowest) | 2 | 3 | 4 | 5 (highest) | |
| TRISS | |||||
| Expected survival | 78.5% | 80.9% | 77.4% | 80.5% | 81.1% |
| Z score | − 1.68 | − 1.25 | − 0.81 | 0.58 | 0.03 |
| PSNL15 | |||||
| Expected survival | 85.3% | 86.0% | 82.9% | 85.9% | 84.5% |
| Z score | 1.02 | 0.98 | 1.37 | 2.96 | 1.66 |
| Observed (actual) survival | 82.9% | 83.8% | 79.5% | 79.2% | 81.0% |
Fig. 1.
Differences between observed and expected survival
Discussion
This analysis of polytrauma patients was performed to investigate a possible association between patients’ SES and clinical outcome after traumatic injury. We hypothesized that trauma patients with low SES levels were associated with worse clinical outcomes.
The analyses revealed that the lowest SES group seemed to include younger patients, with a doubled number of penetrating injuries compared to the highest SES group. However, in contrast with previous research in other countries, we could not find a significant association between socioeconomic status and mortality. Possible explanations include the following.
First of all, the geographical location of our trauma region was advantageous for this study, since it is considered as one of the most culturally diverse cities in the Netherlands. However, it is important to point out the current SES of the Dutch society. Indeed, there is a gap between the lowest and highest SES, but—compared to many other countries— this is quite small. Additionally, the social safety net of the Dutch government is actively supporting cases of socioeconomic deterioration, to promote equality within the society. Therefore, it is quite evident that we could not find any significant associations with our relatively homogeneous study population.
However, we did find a significant association between SES and length of stay at the ICU. Even though the association was minimal (unstandardized coefficient − 0.02), it is important to identify possible causes for these findings. As can be seen in Table 1, no significant differences were found in gender, ISS or comorbidity to explain these results. The combined predictor model, correcting for SES, age, gender, comorbidity, type of injury, mechanism of injury, ISS and AIS, still showed significant differences. Psychological factors in the lower SES groups, with more often mental stress and pressure to achieve due to work-related subjects, might have decreased their state of health in advance, resulting in a longer stay at the ICU [22]. However, additional analyses are recommended, for example regarding hypotension rate or amount of blood loss to eliminate or confirm these as possible confounders for our results.
Unexpected results were found in the subanalysis regarding the expected survival and the actual (observed) survival. The actual survival does not correspond with the predicted survival (based on TRISS) in the lowest SES group, with a difference of approximately 3–4% (Table 4, Fig. 1). This might suggest that other factors are required in analyses including lower SES groups. Furthermore, it is important to notice the more deviant PSNL15 scores, which do not match the TRISS nor the actual survival. Further adjustments for more accurate calculations can, therefore, be advisable.
Apart from that, there are limitations in our study that might (partially) explain the discrepancy in findings as well. One of them includes the difference in SES data that were used to examine the association. To improve the accuracy of the results, we used the database of StatLine Netherlands, which used four indicators to determine SES. However, the use of postal codes might have created risk of bias since the assumption of population homogeneity within a postal code is made, especially in emerging areas. Another limitation was the limited size of the included area. We were only able to obtain data from two level 1 trauma centers (Amsterdam UMC, location VUmc, and Northwest Clinics Alkmaar), whereas the inclusion of more hospitals in the Netherlands might have given a more accurate insight. Furthermore, our database did not include patients who died on scene due to their injuries. Exploring the proportion of patients who died on scene per socioeconomic status might provide additional insight in the association between SES and mortality. Finally, appropriate attention should be paid to the external validity of our results and how these can be extrapolated, given the uniqueness of our mixed study population.
Conclusion
No direct association was found between SES and mortality. However, patients from lower SES suffered from severe injuries at a younger age, showed more penetrating injuries and a longer stay at the ICU. Additionally, discrepancies were found between the expected and actual survival. Therefore, additional research is recommended to find explanations for these findings and to create a more enhanced overview.
Acknowledgements
We genuinely thank Corline Brouwers (Ph.D., former staff member of the Department of Public and Occupational Health, EMGO + Institute, VU University Medical Center) for her generous help during the statistical analyses.
Abbreviations
- AIS
Abbreviated Injury Score
- ASA-PS
American Society of Anesthesiologists Physical Status
- CBS
Statistics Netherlands
- GCS
Glasgow Coma Score
- IC
Intensive care
- ISS
Injury Severity Score
- NTR
National Trauma Register
- PSNL15
Probability of survival based on the Dutch population (2015)
- RTS
Revised Trauma Scores
- SCP
The Dutch Institute for Social Research
- SES
Socioeconomic status
- TRISS
Trauma Revised Injury Severity Score
Compliance with ethical standards
Conflict of interest
There are no conflicts of interest to declare.
References
- 1.Central Bureau for Statistics (2017) Statistics Netherlands: deaths; accidents, residents. https://statline.cbs.nl/Statweb/publication/?VW=T&DM=SLEN&PA=81452eng&D1=0-21&D2=0&D3=0&D4=a&HD=171114-1819&LA=EN&HDR=G1,G2,G3&S. Retrieved on 12 Dec 2017.
- 2.Dutch Network for Acute Care (2015). Report of the Dutch Trauma Registry 2011–2015. Available at: https://www.lnaz.nl/cms/LTR_landelijk_jaarrapport_2011-2015.pdf. Accessed 30 Aug 2018.
- 3.Rockett IRH, Regier MD, Kapusta ND, Coben JH, Miller TR, Hanzlick RL, et al. Leading causes of unintentional and intentional injury mortality: United States, 2000–2009. Am J Public Health. 2012;102:e84–e92. doi: 10.2105/AJPH.2012.300960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wachelder JJH, van Drunen I, Stassen PM, Brouns SHA, Lambooij SLE, Aarts MJ, et al. Association of socioeconomic status with outcomes in older adult community-dwelling patients after visiting the emergency department: a retrospective cohort study. BMJ Open. 2017;7:e019318. doi: 10.1136/bmjopen-2017-019318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mikhail JN, Nemeth LS, Mueller M, Pope C, Nesmith EG, Wilson KL, et al. The association of race, socioeconomic status, and insurance on trauma mortality. J Trauma Nurs. 2016;23:347–356. doi: 10.1097/JTN.0000000000000246. [DOI] [PubMed] [Google Scholar]
- 6.Jarman MP, Haut ER, Curriero FC, Castillo RC. Mapping areas with concentrated risk of trauma mortality. J Trauma Acute Care Surg. 2018;85(1):54–61. doi: 10.1097/TA.0000000000001883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burrows S, Auger N, Gamache P, Hamel D. Individual and area socioeconomic inequalities in cause-specific unintentional injury mortality: 11-year follow-up study of 2.7 million Canadians. Accid Anal Prev. 2012;45:99–106. doi: 10.1016/j.aap.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 8.Haider AH, Chang DC, Efron DT, Haut ER, Crandall M, Cornwell EE. Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008;143:945–949. doi: 10.1001/archsurg.143.10.945. [DOI] [PubMed] [Google Scholar]
- 9.Bosma H, Traag T, Berger-van Sijl M, van Eijk J, Otten F. Intelligence, socio-economic status and hospital admissions of young adults. Ned Tijdschr Geneeskd. 2007;151:1076–1082. [PubMed] [Google Scholar]
- 10.Janssen C, Ommen O, Neugebauer E, Lefering R, Pfaff H. Predicting health-related quality of life of severely injured patients: Sociodemographic, economic, trauma, and hospital stay-related determinants. Eur J Trauma Emerg Surg. 2008;34:277–286. doi: 10.1007/s00068-008-7054-8. [DOI] [PubMed] [Google Scholar]
- 11.Brattström O, Eriksson M, Larsson E, Oldner A. Socio-economic status and co-morbidity as risk factors for trauma. Eur J Epidemiol. 2015;30:151–157. doi: 10.1007/s10654-014-9969-1. [DOI] [PubMed] [Google Scholar]
- 12.Kruithof N, de Jongh MAC, de Munter L, Lansink KWW, Polinder S. The effect of socio-economic status on non-fatal outcome after injury: a systematic review. Injury. 2017;48:578–590. doi: 10.1016/j.injury.2017.01.013. [DOI] [PubMed] [Google Scholar]
- 13.Gennarelli TA, Wodzin EAIS. A contemporary injury scale. Injury. 2005;2006(37):1083–1091. doi: 10.1016/j.injury.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 14.Stewart KE, Cowan LD, Thompson DM. Changing to AIS 2005 and agreement of injury severity scores in a trauma registry with scores based on manual chart review. Injury. 2011;42:934–939. doi: 10.1016/j.injury.2010.05.033. [DOI] [PubMed] [Google Scholar]
- 15.Skaga NO, Eken T, Sovik S, Jones JM, Steen PA. Pre-injury ASA physical status classification is an independent predictor of mortality after trauma. J Trauma Inj Infect Crit Care. 2007;63:972–978. doi: 10.1097/TA.0b013e31804a571c. [DOI] [PubMed] [Google Scholar]
- 16.Ringdal KG, Skaga NO, Steen PA, Hestnes M, Laake P, Jones JM, et al. Classification of comorbidity in trauma: the reliability of pre-injury ASA physical status classification. Injury. 2013;44:29–35. doi: 10.1016/j.injury.2011.12.024. [DOI] [PubMed] [Google Scholar]
- 17.Gad MA, Saber A, Farrag S, Shams ME, Ellabban GM. Incidence, patterns, and factors predicting mortality of abdominal injuries in trauma patients. N Am J Med Sci. 2012;4:129–134. doi: 10.4103/1947-2714.93889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schluter PJ. The Trauma and Injury Severity Score (TRISS) revised. Injury. 2011;42:90–96. doi: 10.1016/j.injury.2010.08.040. [DOI] [PubMed] [Google Scholar]
- 19.Boyd CR, Tolson MA, Copes WS. Evaluating trauma care: the TRISS method. Trauma Score and the Injury Severity Score. J Trauma. 1987;27:370–378. doi: 10.1097/00005373-198704000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Flora JDJ. A method for comparing survival of burn patients to a standard survival curve. J Trauma. 1978;18:701–705. doi: 10.1097/00005373-197810000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Vles WJ, Kroezen F, Meeuwis JD, Leenen LPH. Trauma registration in a Dutch trauma population with emphasis on quality of care. Eur J Trauma Emerg Surg. 2000;26:248–255. doi: 10.1007/PL00002448. [DOI] [Google Scholar]
- 22.Chen E, Miller G. Socioeconomic status and health: mediating and moderating factors. Eur J Trauma Emerg Surg. 2013;28:723–749. doi: 10.1146/annurev-clinpsy-050212-185634. [DOI] [PubMed] [Google Scholar]