Abstract
Purpose
Disturbance of scapulohumeral rhythm has been shown to play a major role in subacromial impingement syndrome. Exercise, taping and subacromial injection are first ray conservative treatment modalities. We aimed to correct scapulohumeral rhythm with kinesio taping and exercise program via focusing on especially periscapular muscles not on glenohumeral structures to achieve scapulothorasic stabilization.
Material and Methods
Seventy five patients were divided into three groups randomly with different treatment modalities which are only exercise group (Group 1), kinesiotaping + exercise group (Group 2), and injection + exercise group (Group 3). Western Ontario Rotator Cuff Index (WORCI), Quick Disability of arm, shoulder, hand (Q-DASH), Constant- Murley Scores (CMS) were evaluated for each patient at the beginning, 15th and 60th days and compared in time and technique manner. Scores were analyzed statistically with One-way ANOVA and Chi-square tests.
Results
All the three groups had better results in short and long term follow ups as compared to initial admission. But in the second group 15th and 60th day results were superior to other groups significantly (p < 0,001).
Conclusions
Most of recent studies using kinesio taping were focused on mechanical correction of humerus which will be an impaired treatment to correct the main cause of impingement. Not only mechanical correction of periscapular muscles and also stabilization of scapulae will help to gain scapulohumeral rhythm.
Keywords: Impingement syndorme, Shoulder, Taping, Subacromial injection
Introduction
Shoulder pain is the second suffering complaint in orthopedic and sports medicine clinics after neck and back pain [1, 2]. Most common reason for shoulder pain is subacromial impingement syndrome (SIS) which may be primary or secondary [3]. Compression leading to abrasion of shoulder cuff structures beneath the coracoacromial arch during the elevation of arm causes symptomatic subacromial impingement syndrome [4]. Although mechanical reasons narrowing the subacromial space may play a role, mainly dyskinetic causes are more reasonable for this situation [5, 6]. Scapular dyskinesia which is alterations in scapular movement according to humerus is the most proven dyskinetic reason for impingement of shoulder [4, 7, 8]. Although many factors have been described, changes in shoulder kinematics leading to narrowing of supraspinatus outlet or subacromial space are most evident pathogenesis in SIS [5, 9].
First-row treatment of SIS is conservative modalities, which are oral medications, subacromial injections (SAI), physiotherapy, shock wave treatment and acupuncture [10–13]. A combination of non-steroidal anti-inflammatory drugs and rehabilitation is the most proven treatment modality [14, 15]. Rehabilitation protocols for SIS are including stretching, strengthening exercises and sometimes manual therapy for soft tissues surrounding the shoulder complex [7]. Another conservative treatment method for impingement syndrome is SAI of corticosteroids combined with local anaesthetics [11, 16]. In case of persistent impingement symptoms, mainly in the short term, it’s one of the most effective modalities to maintain pain relief and increase function [17]. Kinesio taping method (KT), developed by Dr. Kenso Kase, has been widely used also for many musculoskeletal diseases including shoulder problems. In recent studies, kinesio taping also has been used for SIS to obtain early effect on decreasing pain and improved functioning [18, 19]. Most of taping methods are aimed to provide a mechanical stimulus for proprioception or to decrease pain by lifting skin and subcutaneous tissues [19, 20]. In our study, we applied a novel taping method, a combined mechanical correction technique (both glenohumeral and scapulathorasic joints) to regain scapular synchronization with thorax and humerus. By this way, we aimed to highlight the importance of scapulothorasic alignment and/or muscular coordination on the treatment of SIS by focusing on scapulothorasic joint both in exercise and KT programs.
Materials and Methods
Participants
Patients who have admitted to our orthopedic clinic with shoulder pain between May 2017 and May 2018 are included in our study. All patients signed an informed consent, and all the rights of participants were protected. With permission of the ethical committee approved in our institute with a number of 2016/002, a randomized controlled prospective clinical study has been conducted in our clinic. All patients (n = 75) with shoulder pain were examined to rule out rotator cuff tears or glenohumeral instability. Patients between 18–70 aged with positive Hawkins test, Neer test and impingement Jobe test with minimum 1 month duration of symptoms were included [21]. Exclusion criterias were any rheumatic disease, infection, tumor, previous history of shoulder trauma, injection or surgery. All patients were randomly divided into three groups with a randomizer program. First group was subjected to exercise program; the second group to exercise and KT program; whereas the third group was subjected to exercise and subacromial injection (SAI) intervention. Study has been finished at the end of the 60th day because injection therapies mostly have been shown effective until 8–12 weeks of period [22].
Study design
Patients in the 1st group were evaluated and educated on an exercise program by an experienced physiotherapist in orthopaedic rehabilitation and also controlled in each visit for the accuracy of the exercise program focused on scapular stabilization. For the following 15 days, the exercise program was conducted by the patient himself three times a day with 10 repeats. At the end of 15th day, first control of exercise program was supervised by a blinded physiotherapist and scoring of all patients was made in this second evaluation. At the end of 30th day, theraband assisted strengthening exercises were shown and added to the program. At the end of 60th day, patients were re-examined and evaluated for scoring for the last time.
In the 2nd group, KT was applied to all patients according to mechanical correction technique. Especially scapular stabilization and medial periscapular muscles were focused on this technique unlike previous studies. All patients in this group also underwent the same exercise program as the first group. Tapes were changed regularly each 3 days and at the end of 15th day all patients were re-examined and scored. With exercise program conducted until 60th day, last evaluation and scoring were made by the blinded physiotherapist.
In the third group; following the evaluation process, SAI of 1 ml bethamethasone dipropionate + bethametasone sodium phosphate combined with 2 ml local anaesthetic (bupivacaine hydroclorate) was applied to patients at the first visit subacromially after antiseptic preparation of shoulder joint [23]. Posterior injection was applied by an orthopaedic surgeon as described by Cole et al. [22]. All patients were referred to the same blinded physiotherapist for education with the same exercise program as in group 1. The evaluation and scoring were repeated at the end of 15th and 60th days. The physiotherapist did not know the group of patients before she started the evaluation processes (at the 1st, 15th and 60th days).
Outcome Measure
Western Ontario Rotator Cuff Index
Western Ontario Rotator Cuff Index (WORCI), of which Turkish version was found to be reliable and valid, is used to measure the quality of life of patients along the time frame of study. It is a self-assessment instrument containing 21 items and representing all aspects of shoulder function.
Quick DASH
Quick Disability of arm, shoulder, hand (Q-DASH), a shortened version of DASH is used to reveal the differences in physical function and symptoms of patients following various treatment protocols. It has three subscales which are disability/symptom scale, work scale, sports/performing arts scale and their scores range between 0 (no disability) and 100 (most severe disability).
Constant-Murley Score
The impact of the existing pathology on shoulder functions and treatment effects of exercise/kinesiotaping/ injection interventions were also measured by using Constant-Murley Score (CMS) which is in widespread clinical use and often serves as the mandatory part of the evaluation process in Europe. This scoring system is focused primarily on pain, strength, daily activities and range of motion.
Kinesiotaping Techniques
Combination of mechanical correction techniques directed both to glenohumeral and scapulothoracic joints was applied to patients in group 2. Taping procedure focused on the mechanical correction of glenohumeral and scapulothoracic joints. For this purpose %50–75 tensile force was applied to the tapes with the active assistance of the patient. Glenohumeral parts of taping provided centralization of humeral head to glenoid cavity (Figs. 1, 2) whereas scapulothoracic parts aided the eccentric contraction of serratus anterior and lower trapezius muscles by supporting scapulae on thorax mechanically (Fig. 3). Glenohumeral joint was mechanically corrected within two steps by thrusting the humeral head in inferior and posterior directions (Figs. 1, 2). Scapulothoracic joint was corrected again with the active assistance of the patient to provide depression and adduction of scapula on the thoracic cage with the use of a single long I shaped tape (Fig. 3). By stabilizing scapula and centralizing humeral head, scapulohumeral rhythm, which was supposed to be in pathological ranges was tried to normalize in order to eliminate subacromial impingement signs.
Fig. 1.

Taping of shoulder to provide centralization of humeral head to glenoid cavity
Fig. 2.

Taping of shoulder to achieve glenohumeral stabilization in inferior and posterior directions
Fig. 3.

Taping aimed to provide depression and adduction of scapulae on the thoracic cage
Exercise Protocol
Exercises began with isometric strengthening of muscles surrounding the glenohumeral joint and closed kinetic chain exercises focusing on serratus anterior and lower trapezius muscles performed on the wall and/or table and integrated with stretching exercises for related muscles and glenohumeral joint capsule. In late phase of the program, exercises with theraband in patient-specific resistance were added and carried out till the end of the 60th day.
Statistical and Data Analysis
IBM SPSS Statistics version 23 (IBM Corp., Armonk, NY) software was used for all statistical analysis. Mean ± standard deviation for continuous variables and frequency (percentage) for categorical variables were presented as descriptive statistics. One-way ANOVA and Chi-square test were used for continuous and categorical variables comparison among groups, respectively. A linear mixed-effects model was used for the change of WORC, CMS and Q-DASH scores within time according to the groups. All statistical significances were set at p < 0.05.
Results
In our study, 75 patients were divided into three groups who were admitted to our orthopedic clinic with shoulder pain diagnosed as SIS. All patients were evaluated at 1st, 15th and 60th days. Two patients from group 1 (exercise only), 3 patients from group 2 (exercise + taping) and 8 patients from group 3 (exercise + injection) were discontinued to controls at 60th day. Although the study was randomized, female gender was higher than male gender in the second group significantly (p < 0.05). And in the exercise group, right-sided patients were significantly higher (p < 0.05). All other demographic properties like age, height, weight and body mass index (BMI) were similar between groups (Table 1).
Table 1.
Characteristics of study groups and p value
| Variables | Groups | p | ||
|---|---|---|---|---|
| Group 1 Exercise only |
Group 2 Exercise + banding |
Group 3 Exercise + injection |
||
| Age | 52.1 ± 13.3 | 50.2 ± 9.7 | 51.1 ± 11.1 | 0.898 |
| Height | 165.4 ± 9.4 | 163.4 ± 6.9 | 165.2 ± 9.3 | 0.856 |
| Weight | 79.6 ± 12 | 79.9 ± 12.1 | 79.1 ± 13.2 | 0.985 |
| Body Mass Index | 29.1 ± 4 | 30.1 ± 5.3 | 28.9 ± 3.9 | 0.796 |
| Gender (male) | 11 (47.8) | 4 (15.4) | 10 (43.5) | 0.033 |
| Side (right) | 20 (87) | 13 (50) | 15 (65.2) | 0.024 |
Bold values indicate statistically significant differences
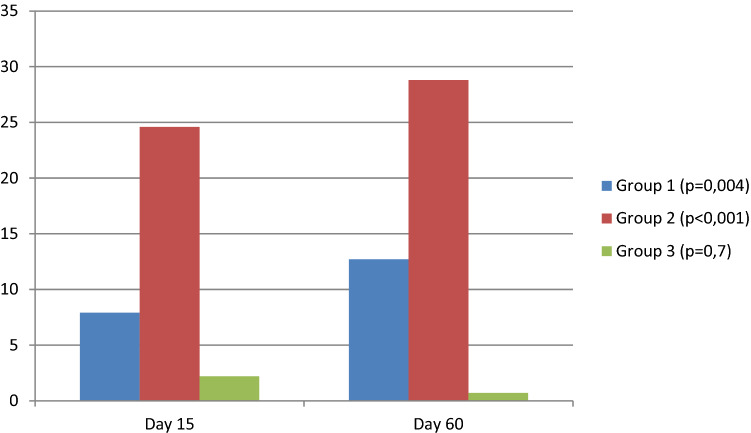
Constant-Murley scores of injection (Group 3) and taping (Group 2) groups were compared to the exercise group (Group 1) using regression analyses. Group 2 scores were significantly higher in 1st, 15th and 60th days than group 1 (p < 0.001). But group 3 had similar scores as the first group. As compared to the 1st examination of each group itself, all groups have had clinical progression in 15th and 60th days (p = 0.004).
In relation to time versus group comparison, 2nd Group had a significant progression in 15th and 60th days (p < 0.05). In 15th day C-M score of Group 2 was 24.6 point higher than Group 1. In 60th day Group 3 and Group 1 had similar scores. So exercise + taping group had better scores in short and long term controls (Fig. 4).
Fig. 4.
Changes in Constant-Murley Scores as referred to day 0. (Linear mixed-effects model results)
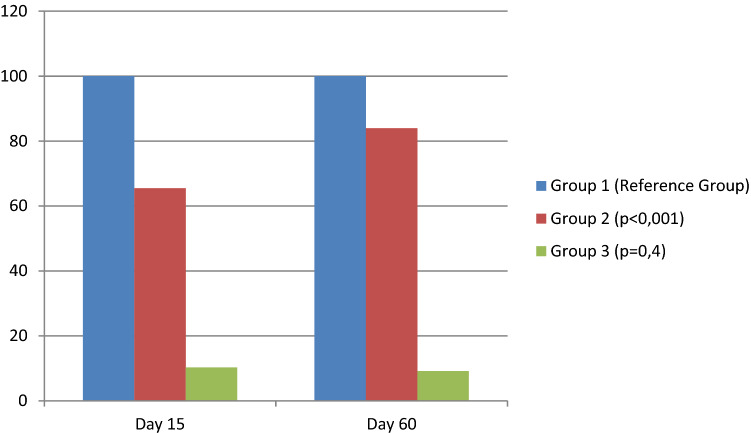
Western Ontario Rotator Cuff Index (WORCI) was better in all groups in 15th and 60th days. But the second group had a better prognosis as compared to other groups in short and also long time period (p < 0.001) (Fig. 5).
Fig. 5.
Decrease in Western Ontario Rotator Cuff Index as referred to group 1. (Linear mixed-effects model results)
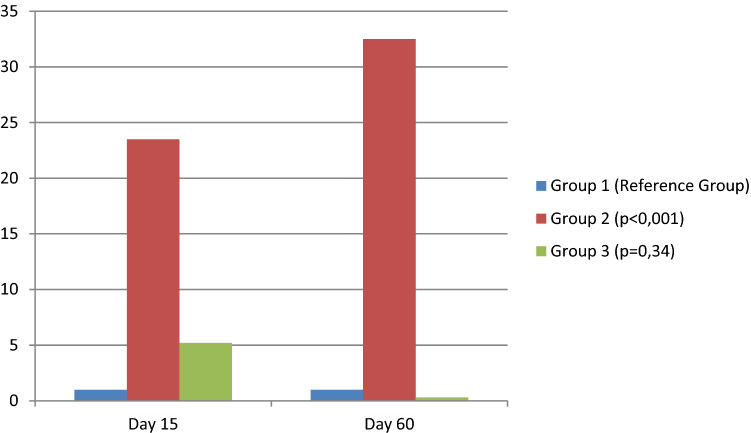
All groups were also evaluated for functionality with Quick DASH Score in 1st, 15th and 60th days. Group 1 and Group 3 had similar prognosis, but Group 2 had significantly better results in all control measurements (p < 0.001). In group 2, short time and long time prognosis were also significant as compared to initial examination. (Fig. 6).
Fig. 6.
Changes in Quick DASH Scores as referred to Group 1. (Linear mixed-effects model results)
Discussion
Although exercise therapy is a traditional physiotherapy method in SIS treatment, Kinesio Taping (KT) increasingly become an adjunct treatment option in recent years. Taping has been commonly using in orthopedic and sports settings. We believe that mechanical correction technique of KT primarily support and realign the articular structures, reduce pain and increase the ROM via elevating the epidermis which increase the pressure of the mechanoreceptors below the dermis [24]. In the current study, we demonstrated that KT and home exercise treatment is significantly has better early and late period outcomes of ROM and functional activity than subacromial injection and home exercise treatment in SIS and also we find out that subacromial steroid injection in addition to a home exercise program and only home exercise program have similar outcomes. Similar to our study there are various studies have previously reported that KT therapy improves pain control and ROM in SIS treatment when compared to the exercise [18, 25], NSAID [26], and subacromial steroid injection treatments [27].
Taping is an adjunct treatment method during rehabilitation to improve functional recovery in SIS treatment. The principal of mechanical correction technique of KT is under control unwanted joint movements and supporting and protecting the joints structures. Kaya et al. [18] compared the effectiveness of KT and physiotherapy treatment with the only physiotherapy treatment and they find out that KT treatment leads the functional improvements in SIS, due to KT provides sensory, motor and proprioceptive feedback, and patients report improved comfort level, symptom relief, and improved stability of joint. Subası et al. [27] reported that KT with an exercise program is an effective, safe and inexpensive treatment in SIS. In the current study, KT and home exercise treatments’ early and late functionally outcomes were significantly better than both only home exercise program and subacromial steroid injection treatments and home exercise program.
Disability scores of KT and home exercise group were also significantly decreased in the early and late periods of treatment significantly more than other treatments. Thus, we can conclude that KT stimulates neuromuscular pathways via increasing afferent feedback and/or increasing reinforcement the motor units of shoulder muscles due to an increased proprioception [18, 25, 27]. Selkowitz et al. demonstrated that taping decreases upper trapezius muscle’s electromyographic activity whereas increasing lower trapezius activity [28]. Simsek et al. reported that KT improve the functional status and reduce pain via mechanical correction techniques in addition to exercises therapy in patients with SIS [25]. We believe that KT reduces pain at the spinal level via gate control mechanism by elevating the epidermis thus also make improvements in ROM and functional activity [29, 30]. We believe that these findings also demonstrate the role of the muscle imbalance that should be applied to adjunct treatment methods such as KT. On the other hand, there is a few studies advocate that KT has no improvements in pain and functional status [31, 32]. Scapular stabilization was reported as a most important factor in shoulder impingement in the latest studies [33, 34].
Several investigations have evaluated the effectiveness of subacromial steroid injection [20, 26, 27]. Some previous studies were underlying the concern regarding potential damage of repeated corticosteroid injections to the cuff tendons [35, 36]. Although some authors reported that corticosteroid injection was effective in the treatment of SIS, some demonstrated that this effect was not more than NSAIDs [3, 26, 27]. The current literature has conflicting outcomes of subacromial injection success in SIS. Sahin Onat et al. [26] find out that subacromial corticosteroid injection in addition to NSAIDs improve functional activity, ROM and reduce pain when compared the only using NSAIDs. Another study from Subaşı et al. reported that both KT and steroid injection in addition to the exercise program effective in the rehabilitation of SIS [27]. In contrast, a recent study reported that local injection therapy in addition to home exercise program improve shoulder ROM and functional capacity and reduce pain more than KT and home exercise program in SIS [20]. Because the corticosteroid injection is an invasive treatment, some patients avoid injections and choose more non-invasive methods as reported in a recent comparative study [34].
Limitations of our study can be analyzed in two ways. The small sample size and also discontinuity of some patients to study protocol may a disadvantage to show the effectiveness of our method for SIS treatment. We did studied patients from the same clinic which also restricts our study to reflect our population. We have no any taping group treated with placebo taping, so we cannot exclude the effect of taping as a placebo also.
Conclusion
As the distortion of the scapulothoracic rhythm considered as a proven factor for SIS, we need a different type of taping focusing on this pathology. As we improve scapular stabilization and mechanical correction of scapulae with taping and exercise, we will achieve good results as much as injection like interventional therapies.
Acknowledgements
We would like to thank Erdem Karabulut M.D. for supporting the statistical analyses of this manuscript.
Author contributions
OV collected the data and contributed to the final version of the manuscript. BO conceived the design of the manuscript, collected and analyzed the data and prepared the final approval of the version to be submitted. IDC conceived the design of the manuscript and drafted the article as well.
Funding
There is no any foundation about this work privately or publicly.
Compliance with Ethical Standards
Conflict of interest
There is not any conflict of interests regarding the submission and publication of this manuscript and its’ potential implications. Manuscript has been read and approved by all the authors. All authors declare that this study represents our honest work. The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Ethical approval
The study was approved by Kirikkale University Institutional Ethics Committee (Date:12.01.2014, Approval no. 26/11).
Informed consent
Patient, whose photograph has been used for describing of the procedure, has signed consent form. The original form is available from the corresponding author on reasonable request. The data and materials are available from the medical records department of the Research and Practice Hospital of Kirikkale University. The datasets used during the current study are available from the corresponding author on reasonable request.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ozge Vergili, Email: kocaacar@yahoo.co.uk.
Birhan Oktas, Email: birhanoktas@kku.edu.tr.
Ibrahim Deniz Canbeyli, Email: denizcanbeyli@gmail.com.
References
- 1.Green, S., Buchbinde, R., Glazier, R., & Forbes, A. (2000). Interventions for shoulder pain. Cochrane Database Systematic Reviews (2):CD001156. [DOI] [PubMed]
- 2.Bernhardsson S, Klintberg IH, Wendt GK. Evaluation of an exercise concept focusing on eccentric strength training of the rotator cuff for patients with subacromial impingement syndrome. Clinical Rehabilitation. 2011;25(1):69–78. doi: 10.1177/0269215510376005. [DOI] [PubMed] [Google Scholar]
- 3.van der Windt DA, Koes BW, de Jong BA, Bouter LM. Shoulder disorders in general practice: Incidence, patient characteristics, and management. Annals of the Rheumatic Diseases. 1995;54(12):959–964. doi: 10.1136/ard.54.12.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Physical Therapy. 2000;80(3):276–291. doi: 10.1093/ptj/80.3.276. [DOI] [PubMed] [Google Scholar]
- 5.Kamkar A, Irrgang JJ, Whitney SL. Nonoperative management of secondary shoulder impingement syndrome. Journal of Orthopaedic and Sports Physical Therapy. 1993;17(5):212–224. doi: 10.2519/jospt.1993.17.5.212. [DOI] [PubMed] [Google Scholar]
- 6.Kibler WB, McMullen J. Scapular dyskinesis and its relation to shoulder pain. Journal of the American Academy of Orthopaedic Surgeons. 2003;11(2):142–151. doi: 10.5435/00124635-200303000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Camargo PR, Alburquerque-Sendin F, Avila MA, Haik MN, Vieira A, Salvini TF. Effects of stretching and strengthening exercises, with and without manual therapy, on scapular kinematics, function, and pain in individuals with shoulder impingement: A randomized controlled trial. Journal of Orthopaedic and Sports Physical Therapy. 2015;45(12):984–997. doi: 10.2519/jospt.2015.5939. [DOI] [PubMed] [Google Scholar]
- 8.Cools AM, Dewitte V, Lanszweert F, et al. Rehabilitation of scapular muscle balance: which exercises to prescribe? American Journal of Sports Medicine. 2007;35(10):1744–1751. doi: 10.1177/0363546507303560. [DOI] [PubMed] [Google Scholar]
- 9.Singh B, Bakti N, Gulihar A. Current concepts in the diagnosis and treatment of shoulder impingement. Indian Journal of Orthopedics. 2017;51(5):516–523. doi: 10.4103/ortho.IJOrtho_187_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johansson K, Bergstrom A, Schroder K, Foldevi M. Subacromial corticosteroid injection or acupuncture with home exercises when treating patients with subacromial impingement in primary care—A randomized clinical trial. Family Practice. 2011;28(4):355–365. doi: 10.1093/fampra/cmq119. [DOI] [PubMed] [Google Scholar]
- 11.Blair B, Rokito AS, Cuomo F, Jarolem K, Zuckerman JD. Efficacy of injections of corticosteroids for subacromial impingement syndrome. Journal of Bone and Joint Surgery. American Volume. 1996;78(11):1685–1689. doi: 10.2106/00004623-199611000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Kuhn JE. Exercise in the treatment of rotator cuff impingement: A systematic review and a synthesized evidence-based rehabilitation protocol. Journal of Shoulder and Elbow Surgery. 2009;18(1):138–160. doi: 10.1016/j.jse.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 13.Santamato A, Panza F, Notarnicola A, et al. Is extracorporeal shockwave therapy combined with isokinetic exercise more effective than extracorporeal shockwave therapy alone for subacromial impingement syndrome? A randomized clinical trial. Journal of Orthopaedic and Sports Physical Therapy. 2016;46(9):714–725. doi: 10.2519/jospt.2016.4629. [DOI] [PubMed] [Google Scholar]
- 14.Hallstrom E, Karrholm J. Shoulder kinematics in 25 patients with impingement and 12 controls. Clinical Orthopaedics and Related Research. 2006;448:22–27. doi: 10.1097/01.blo.0000224019.65540.d5. [DOI] [PubMed] [Google Scholar]
- 15.Michener LA, Walsworth MK, Burnet EN. Effectiveness of rehabilitation for patients with subacromial impingement syndrome: A systematic review. Journal of Hand Therapy. 2004;17(2):152–164. doi: 10.1197/j.jht.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 16.Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: A systematic review of randomised controlled trials. Lancet. 2010;376(9754):1751–1767. doi: 10.1016/S0140-6736(10)61160-9. [DOI] [PubMed] [Google Scholar]
- 17.Sumanont S, Boonard M, Peradhammanon E, et al. Comparative outcomes of combined corticosteroid with low volume compared to high volume of local anesthetic in subacromial injection for impingement syndrome: Systematic review and meta-analysis of RCTs. European Journal of Orthopaedic Surgery and Traumatology. 2018;28(3):397–407. doi: 10.1007/s00590-017-2056-z. [DOI] [PubMed] [Google Scholar]
- 18.Kaya E, Zinnuroglu M, Tugcu I. Kinesio taping compared to physical therapy modalities for the treatment of shoulder impingement syndrome. Clinical Rheumatology. 2011;30(2):201–207. doi: 10.1007/s10067-010-1475-6. [DOI] [PubMed] [Google Scholar]
- 19.Desjardins-Charbonneau A, Roy JS, Dionne CE, Desmeules F. The efficacy of taping for rotator cuff tendinopathy: A systematic review and meta-analysis. International Journal of Sports Physical Therapy. 2015;10(4):420–433. [PMC free article] [PubMed] [Google Scholar]
- 20.Goksu H, Tuncay F, Borman P. The comparative efficacy of kinesio taping and local injection therapy in patients with subacromial impingement syndrome. Acta Orthopaedica et Traumatologica Turcica. 2016;50(5):483–488. doi: 10.1016/j.aott.2016.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Diercks R, Bron C, Dorrestijn O, et al. Guideline for diagnosis and treatment of subacromial pain syndrome: A multidisciplinary review by the Dutch Orthopaedic Association. Acta Orthopaedica. 2014;85(3):314–322. doi: 10.3109/17453674.2014.920991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cole BJ, Schumacher HR., Jr Injectable corticosteroids in modern practice. Journal of the American Academy of Orthopaedic Surgeons. 2005;13(1):37–46. doi: 10.5435/00124635-200501000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Aksakal M, Ermutlu C, Ozkaya G, Ozkan Y. Lornoxicam injection is inferior to betamethasone in the treatment of subacromial impingement syndrome: A prospective randomized study of functional outcomes. Orthopade. 2017;46(2):179–185. doi: 10.1007/s00132-016-3302-5. [DOI] [PubMed] [Google Scholar]
- 24.Saavedra-Hernandez M, Castro-Sanchez AM, Arroyo-Morales M, Cleland JA, Lara-Palomo IC, Fernandez-de-Las-Penas C. Short-term effects of kinesio taping versus cervical thrust manipulation in patients with mechanical neck pain: A randomized clinical trial. Journal of Orthopaedic and Sports Physical Therapy. 2012;42(8):724–730. doi: 10.2519/jospt.2012.4086. [DOI] [PubMed] [Google Scholar]
- 25.Simsek HH, Balki S, Keklik SS, Ozturk H, Elden H. Does Kinesio taping in addition to exercise therapy improve the outcomes in subacromial impingement syndrome? A randomized, double-blind, controlled clinical trial. Acta Orthopaedica et Traumatologica Turcica. 2013;47(2):104–110. doi: 10.3944/AOTT.2013.2782. [DOI] [PubMed] [Google Scholar]
- 26.Sahin Onat S, Bicer S, Sahin Z, Kucukali Turkyilmaz A, Kara M, Ozbudak DS. Effectiveness of kinesiotaping and subacromial corticosteroid injection in shoulder impingement syndrome. American Journal of Physical Medicine and Rehabilitation. 2016;95(8):553–560. doi: 10.1097/PHM.0000000000000492. [DOI] [PubMed] [Google Scholar]
- 27.Subasi V, Cakir T, Arica Z, et al. Comparison of efficacy of kinesiological taping and subacromial injection therapy in subacromial impingement syndrome. Clinical Rheumatology. 2016;35(3):741–746. doi: 10.1007/s10067-014-2824-7. [DOI] [PubMed] [Google Scholar]
- 28.Selkowitz DM, Chaney C, Stuckey SJ, Vlad G. The effects of scapular taping on the surface electromyographic signal amplitude of shoulder girdle muscles during upper extremity elevation in individuals with suspected shoulder impingement syndrome. Journal of Orthopaedic and Sports Physical Therapy. 2007;37(11):694–702. doi: 10.2519/jospt.2007.2467. [DOI] [PubMed] [Google Scholar]
- 29.Gonzalez-Iglesias J, Fernandez-de-Las-Penas C, Cleland JA, Huijbregts P, Del Rosario G-V. Short-term effects of cervical kinesio taping on pain and cervical range of motion in patients with acute whiplash injury: a randomized clinical trial. Journal of Orthopaedic and Sports Physical Therapy. 2009;39(7):515–521. doi: 10.2519/jospt.2009.3072. [DOI] [PubMed] [Google Scholar]
- 30.Paoloni M, Bernetti A, Fratocchi G, et al. Kinesio Taping applied to lumbar muscles influences clinical and electromyographic characteristics in chronic low back pain patients. European Journal of Physical and Rehabilitation Medicine. 2011;47(2):237–244. [PubMed] [Google Scholar]
- 31.Fu TC, Wong AM, Pei YC, Wu KP, Chou SW, Lin YC. Effect of Kinesio taping on muscle strength in athletes—A pilot study. Journal of Science and Medical Sports. 2008;11(2):198–201. doi: 10.1016/j.jsams.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 32.Slupik A, Dwornik M, Bialoszewski D, Zych E. Effect of kinesio taping on bioelectrical activity of vastus medialis muscle. Preliminary report. Ortopedia Traumatologia Rehabilitacja. 2007;9(6):644–651. [PubMed] [Google Scholar]
- 33.Gunay Ucurum S, Kaya DO, Kayali Y, Askin A, Tekindal MA. Comparison of different electrotherapy methods and exercise therapy in shoulder impingement syndrome: A prospective randomized controlled trial. Acta Orthopaedica et Traumatologica Turcica. 2018;52(4):249–255. doi: 10.1016/j.aott.2018.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rhon DI, Boyles RB, Cleland JA. One-year outcome of subacromial corticosteroid injection compared with manual physical therapy for the management of the unilateral shoulder impingement syndrome: a pragmatic randomized trial. Annals of Internal Medicine. 2014;161(3):161–169. doi: 10.7326/M13-2199. [DOI] [PubMed] [Google Scholar]
- 35.Khan Y, Nagy MT, Malal J, Waseem M. The painful shoulder: shoulder impingement syndrome. The Open Orthopaedics Journal. 2013;7:347–351. doi: 10.2174/1874325001307010347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Camargo PR, Haik MN, Ludewig PM, Filho RB, Mattiello-Rosa SM, Salvini TF. Effects of strengthening and stretching exercises applied during working hours on pain and physical impairment in workers with subacromial impingement syndrome. Physiotherapy: Theory and Practice. 2009;25(7):463–475. doi: 10.3109/09593980802662145. [DOI] [PubMed] [Google Scholar]