Abstract
Background
Femoral neck fractures in children are rare injuries, occurring due to high-energy trauma. Due to the unique anatomy and blood supply of the proximal femur in growing children, these fractures are notorious for high rates of complications despite appropriate management. Classification of these fractures is according to the Delbet system, which not only guides management but also gives prognostic clues. Multiple fixation methods have been described and there is no consensus on what constitutes the best treatment. Osteonecrosis, non-union, coxa vara and premature physeal arrest are the most frequent complications.
Purpose
To review the current knowledge, discuss controversial aspects, and provide suggestions for future research.
Methods
We have reviewed the literature on paediatric proximal femur fractures and have provided an evidence-based guide to the diagnosis and management of these injuries. Common complications have been elaborated and options for their prevention and/or management discussed.
Conclusion
There is universal agreement that anatomic reduction and stable internal fixation, supplemented by spica immobilization in younger children, are essential to obtain good outcomes. The role of capsular decompression, choice and configuration of implant, and appropriate timing of surgery are aspects that continue to be debated. Multicenter prospective studies are necessary to standardize treatment of these challenging injuries.
Keywords: Fracture neck femur, Paediatric, Avascular necrosis, Non-union, Coxa vara
Introduction
Fractures of the femoral neck in children are rare injuries, comprising < 1% of all childhood fractures per year [1]. This fracture has traditionally been associated with high complication rates and poor outcomes. However, in recent years, trends towards aggressive surgical intervention and availability of better implants has led to reduced complications and better outcomes. Appropriate and timely management of these injuries can prevent life-long disability from hip osteoarthritis. In this review, we will discuss the current knowledge on paediatric proximal femoral fractures.
We identified relevant articles by searching the Cochrane Database of Systematic Reviews (1993–2020; http://www.cochrane.org), PubMed (1970–early 2020), EMBASE and Google Scholar, using the search terms ‘fracture neck femur’ and ‘children’. Inclusion criteria were: diagnosis of proximal femur fracture; subjects younger than 18 years; and English language. Systematic reviews, meta-analyses, randomized and quasi-randomized clinical trials, prospective and retrospective cohort studies, and case series that met the inclusion criteria were included. Bibliographies of the retrieved articles were manually scanned for citations missed by the initial search. Studies were excluded if they were exclusively concerned with pathological fractures or subtrochanteric fractures.
Epidemiology
The incidence of femoral neck fractures in children is between 0.3 and 0.5% of all childhood fractures per year [1]. The incidence is maximum at the ages of 11 and 12 years [2], with a male preponderance ranging from 1.3 to 1.7:1 [3, 4]. In contrast to the osteoporotic proximal femur fractures in the elderly, the majority of cases in children occur due to high-energy trauma such as road traffic accidents and falls from heights [5].
Classification
The most commonly used system for classification of femoral neck fractures in children is that of Delbet, popularized by Colonna [6]. Type I are transphyseal fractures; II, transcervical; III, cervicotrochanteric; and IV, intertrochanteric. Most large series report type II Delbet fractures to be the most common (34–54%) followed by types III, IV and I respectively (Table 1). Ju et al. [7] subdivided type I Delbet injuries into type IA (without dislocation of the femoral head from the acetabulum) and type IB (with dislocation of the femoral head from the acetabulum). Azouz et al. [4] added a type V injury—a fracture in the immediate subtrochanteric region. Moon and Mehlman [8] clarified that while applying the Delbet classification, the most proximal portion of an oblique fracture line should be used to decide the fracture type. Panigrahi et al. [9] further classified Delbet fracture types II and III, by dividing the femoral neck into four equal zones (25% each) on a traction X-ray of the pelvis with both hips after fracture reduction. This system was proposed to guide implant selection, with zone I fractures being situated just beside the head and thus highly unstable, while zone IV fractures are situated near the intertrochanteric region.
Table 1.
Reported frequency of each Delbet fracture type
| Author | Total cases | I | II | III | IV |
|---|---|---|---|---|---|
| Moon and Mehlman [8] | 360 | 29 (8%) | 145 (40%) | 120 (33%) | 66 (18%) |
| Togrul [43] | 103 | 3 (2.9%) | 35 (34%) | 41 (39.8%) | 24 (23.3%) |
| Ratliff [2] | 71 | 2 (3%) | 38 (54%) | 26 (37%) | 4 (6%) |
| Canale and Bourland [62] | 61 | 5 (8%) | 27 (44%) | 22 (36%) | 7 (11%) |
| Ju et al. [7] | 58 | 0 | 30 (51.7%) | 21 (36.2%) | 7 (12.1%) |
| Morsy [63] | 53 | 1 (1.9%) | 28 (52.8%) | 21 (39.6%) | 3 (5.7%) |
The classification of these fractures as displaced vs non-displaced also has prognostic significance, with displaced types more likely to develop major complications. Pauwels classification of neck femur fractures, usually applied in adults, has relevance in paediatric fractures as well [10]. A higher Pauwels angle with a more vertical fracture causes greater shear forces at the fracture site, thus predisposing to loss of fixation and non-union.
Pathophysiology
Femoral neck fractures in children are associated with higher rates of osteonecrosis, but lower rates of non-union as compared to adults. The unique biology of the proximal femur in childhood is responsible for this phenomenon.
Vascular Supply to the Head of Femur
Blood supply to the proximal femoral epiphysis is precarious during childhood. Throughout life, the blood supply to the femoral head is predominantly from the lateral epiphyseal vessels, which are the terminal branches of the medial circumflex femoral artery, arising from its deep branch [11]. After piercing the capsule, the lateral epiphyseal vessels (also known as retinacular arteries or lateral ascending cervical arteries), run along the posterior and superior aspects of the femoral neck, before penetrating the outer edge of the proximal femoral epiphysis [12, 13] (Fig. 1).
Fig. 1.

Illustration showing blood supply of the proximal femur (right hip, posterior view). 1 Femoral head; 2 deep branch of medial circumflex femoral artery (MCFA); 3 terminal sub-synovial branches of MCFA; 4 insertion of piriformis tendon; 5 insertion of gluteus medius tendon; 6 lesser trochanter with nutrient branches; 7 trochanteric branches; 8 branch of the first perforating artery.
Adapted from Ref. [11]
This blood supply is supplemented by additional vessels and the pattern of vascularity passes through five phases [14]. At birth, straight vessels arising from the metaphysis directly penetrate the cartilaginous femoral head. Between 4 months and 4 years, epiphyseal ossification begins and these metaphyseal vessels decrease in size and number. The physeal plate constitutes a barrier to the passage of intra-osseous blood vessels from the metaphysis into the epiphysis, and hence, between 4 and 7 years, the lateral epiphyseal vessels constitute the sole supply to the epiphysis. Between 7 and 10 years, the vessels of the ligamentum teres (medial epiphyseal vessels) become more prominent and contribute to the blood supply of the epiphysis. During adolescence, as skeletal maturity approaches, the growth plate is gradually obliterated and the vessels of the metaphysis, epiphysis and ligamentum teres anastomose freely with each other. In adults, this anastomosis provides robust blood supply to the epiphysis, which is not completely dependent on the retinacular end arteries; accounting for the lesser incidence of AVN after femoral neck fractures in adults as compared to children [15, 16].
Bone Healing at the Femur Neck
The periosteum of the femur neck in children is thicker and more cellular as compared to adults. Sferopoulos and Papavasiliou [17] demonstrated healing of femoral neck fractures in children of all ages by formation of bridging callus, despite the intra-articular location of these fractures. Hence, if stable reduction can be maintained, these fractures are very likely to unite soundly.
Fracture Pattern
Pediatric femoral neck fractures are highly unstable injuries since the fracture lines are often uniplanar and smooth with very little interlocking of the fragments [9], unlike the spiral fracture lines often seen in adults. Furthermore, the more oblique the fracture line, the greater the instability due to high shear forces acting at the fracture site [10]. High rates of displacement of initially undisplaced fractures treated conservatively [18, 19] are a testament to the instability of these fractures.
Muscle Forces
The actions of muscles around the hip cause typical displacements after femur neck fractures [20]. The fulcrum for movement, which normally lies at the center of the femoral head, is shifted to the femoral shaft after a fracture. The net effect of the pull of the iliopsoas, abductors, external rotators, gluteus maximus and adductors on the distal fragment is proximal and medial translation and external rotation of the shaft. The proximal fragment, having no muscle attachments, is pushed passively by the trochanteric fragment so that its fracture surface comes to face antero-supero-laterally.
Clinical Features
There is usually a history of significant trauma followed by pain and inability to bear weight on the affected limb. Such children are often polytraumatized, with associated head, chest, abdomen or facio-mandibular injuries, as well as pelvic and other long bone fractures [19]. It is thus important for such children to be examined thoroughly, preferably in collaboration with a general surgeon. If there is no clear history of significant trauma, an underlying cause should be sought in any child presenting with femoral neck fracture [4]; this includes pathologies like bone cysts, fibrous dysplasia and osteomyelitis as well as non-accidental trauma. Typically, the child presents with a shortened, externally rotated lower extremity, with pain localized to the groin or referred to the knee. Rarely, in undisplaced or incomplete fractures, the child may be able to walk with a limp.
Diagnosis
The diagnosis is usually straightforward and can be made on plain radiographs of the pelvis with both hips. A cross-table lateral view should be obtained instead of the Lauenstein frog-leg view to avoid pain and risk of further displacement with manipulation of the hip. In complex injuries, such as Delbet type IB and those associated with pelvic ring fractures, a CT scan is useful [15]. In rare cases involving infants, prior to appearance of the capital femoral epiphyseal ossific nucleus, a sonography may be necessary to identify the injury [5]. In undisplaced fractures where a high index of suspicion exists, an MRI or technetium bone scan can help in confirming the diagnosis [15]. On T2-weighted MRI, a well-defined line of low-signal intensity surrounded by an area of high-signal intensity due to bone marrow edema confirms the presence of a fracture. MRI/CT are also helpful for diagnosing pathological fractures [1, 15].
Management
Anatomic reduction and adequate stabilization are essential to minimize the risk of complications [21–23]. Other important considerations that influence final outcomes include the role of hip decompression and timing of surgery.
Reduction
Reduction Criteria
The adequacy of reduction is assessed as per criteria proposed by Song [24]. ‘Anatomical reduction’ is when there is no displacement or angulation; ‘acceptable reduction’ consists of < 2 mm displacement or up to 20° angulation (on both anteroposterior and lateral views); and ‘unacceptable reduction’ consists of > 2 mm displacement or > 20° angulation.
Closed vs Open Reduction
Closed reduction (CR) maneuvers include those of Whitman [25], Leadbetter [26] and Flynn [27]. The principle is to counteract the muscle forces acting on the distal fragment and realign it with the proximal fragment which cannot be controlled. Initially longitudinal traction is applied with the hip in flexion and abduction to dis-impact the fragments. Subsequently the hip is brought into extension and internal rotation. In this position the spirally arranged ligaments around the hip joint are tightened, thus maintaining the fragments in the reduced position [27].
Open reduction (OR) has the advantages of direct visualization leading to better reduction and simultaneous decompression of the intra-capsular hematoma. However, this must be weighed against longer operative time, greater blood loss and risk of post-operative joint infection. Numerous studies have reported better quality of reduction, better outcomes and fewer complications with OR as compared to CR [7, 19, 24, 28]. OR may be accomplished using the Smith-Petersen (anterior) approach or the Watson-Jones (antero-lateral) approach. The anterior approach allows better exposure of the proximal neck and peri-articular area and easier placement of reduction tools into the head, but needs a second incision to place definitive fixation. It is best suited for epiphyseal separations and trans-cervical fractures [29]. The anterolateral approach, on the other hand, gives better access to the peri-trochanteric area and is better suited for basicervical and intertrochanteric fractures [29].
Reduction can be performed using a fracture table or with the leg free. In the latter scenario, a Schanz pin inserted into the femoral shaft is a useful reduction tool [30]. It allows lateral traction to dis-impact the fragments and gives better rotational control of the distal fragment. Similarly, Kirschner wires placed in the proximal fragment can be used as ‘joy-sticks’ to manipulate it [30].
Maintenance of Reduction
Non-operative
Historically, treatment for femoral neck fractures in children consisted of manipulation followed by immobilization using spica casts, Thomas splints or traction frames. Such non-operative treatment is now largely obsolete, except for undisplaced or incomplete femoral neck fractures in very small children (< 2 years). Minimally displaced intertrochanteric fractures in small children can also be managed by a period of traction followed by spica application. The chief concern with non-operative treatment is the risk of late displacement, which occurs not only with initially displaced fractures that are reduced and placed in cast, but also with initially undisplaced fractures which can undergo displacement while in cast [2, 19]. Older children with undisplaced fractures have also been shown to have displacement when treated by being kept non-weight bearing [18].
If a decision is made to treat this fracture non-operatively, the application of hip spica is a must and should preferably be done after assessing fracture stability under C-arm. Regular radiographic follow-up in the initial weeks after spica application is essential to check for displacement.
Operative
Closed or open reduction followed by stable internal fixation is the current standard of care for all displaced femoral neck fractures in children and is now increasingly preferred for undisplaced fractures as well. Implants used include smooth Kirschner wires, fully and partially threaded cannulated cancellous (CC) screws, fixed-angle sliding hip screws and fixed-angle locking plates [15, 31]. A recent study found that the type of fixation used does not affect the incidence of AVN or final outcome [32].
In small children (< 10 years), attempts should be made to spare the physis by using screws stopping short of it or by using smooth Kirschner wires where spanning the physis is unavoidable [1]. All such children must be placed in a hip spica post-operatively to protect the internal fixation [5, 23, 33]. Achieving fracture stability is the most important goal of treatment, however, and trans-physeal fixation provides the most stability. Trans-physeal screw placement is preferable in children ≥ 10 years or whenever required for stable fracture fixation, irrespective of age [1, 15, 23].
Selection of implant for fracture fixation is chiefly guided by fracture type and the child’s size and skeletal maturity [15]. Generally speaking, fracture types I–III should be fixed with multiple Kirschner wires in children < 3 years of age; Kirschner wires or 4 mm CC screws in children 4–10 years of age; and with 6.5/7.3 mm CC screws in children > 10 years of age [15] (see Figs. 2 and 3 for case examples). Type IV (intertrochanteric) fractures are a special sub-set; they must ideally be fixed with sliding hip screw and side-plate constructs, the screw stopping short of the physis in younger children [15]. When using screws for fixation, three parallel, well spread-out lag screws placed in an inverted triangle perpendicular to the fracture line is the ideal configuration [30, 34]. Placement of an additional fourth screw transversely into the calcar has also been described [35]. Another alternative construct consists of one screw perpendicular to the fracture line in the inferior head and neck plus one or two screws parallel to the femoral neck axis [30]. An advantage of screw fixation is that their insertion does not disturb the reduction and can even help in fine-tuning the reduction (for example, tightening a superior screw to correct varus angulation). The drawbacks of screw constructs are that they are not very effective against shear forces, and hence prone to collapse into varus and retroversion; and that inadvertent lack of parallelism may adversely affect compression and fracture healing.
Fig. 2.

A 12 years old girl with Delbet type II neck femur fracture. a Pre-operative radiograph of the right hip anteroposterior (AP) and lateral views showing displacement. b Radiograph of the right hip AP and lateral views at 1 year follow-up showing complete union. The fracture was closed reduced and fixed using two 6.5 mm cannulated cancellous screws
Fig. 3.
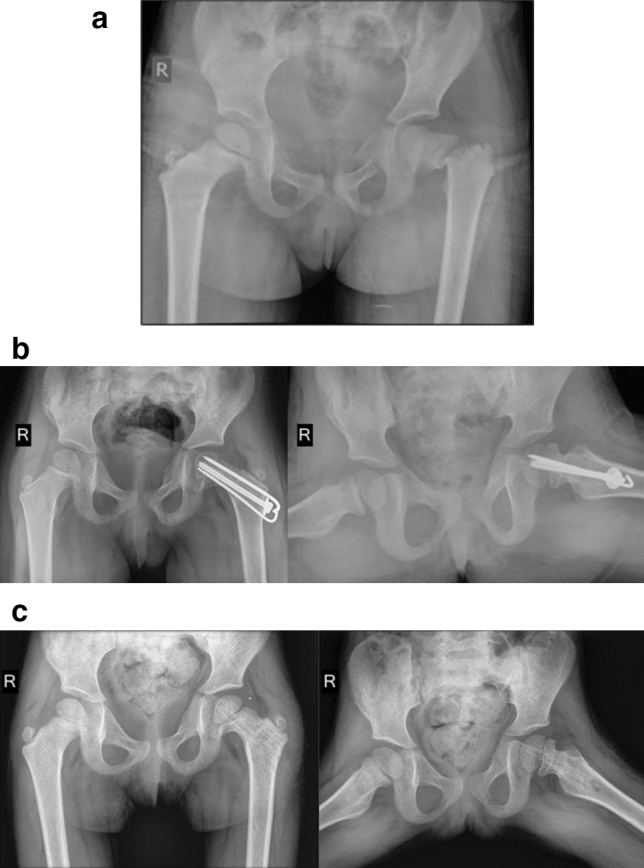
A 5 years old girl with Delbet type II neck femur fracture. a Pre-operative radiograph of pelvis with both hips showing displacement. b Radiograph of pelvis with both hips AP and frog-leg lateral views at 6 months follow-up showing good alignment and union. The fracture underwent open reduction through Watson-Jones approach and fixation with one 4.5 mm cannulated cancellous screw and two 1.6 mm Kirshner wires. Decision was made to cross the physis due to marked instability of the fracture. c Radiograph of pelvis with both hips AP and frog-leg lateral views at 2 years follow-up, after implant removal. The fracture is well-united, but there is growth disturbance with coxa vara and narrowing of the femoral neck. She subsequently underwent greater trochanter epiphysiodesis and is currently asymptomatic
The dynamic hip screw (DHS) better resists shear forces, but it is often associated with disruption of provisional reduction during implant placement, particularly due to rotation of the proximal fragment [31]. This can be minimized, but not completely avoided, by use of a de-rotation screw or wire placed in the superior head and neck [34]. Recently, mini-fragment plates placed along the calcar have been described to stabilize provisional reduction prior to definitive fixation, and also to reinforce traditional constructs by counteracting shear forces [31]. Another disadvantage of DHS is that healing often occurs with undesirable neck shortening. Proximal femoral locking plates (PFLPs) have been advocated as fixed-angle length-stable constructs to avoid this [36]. However, while PFLPs are biomechanically promising, clinical studies have shown poor outcomes, probably due to lack of compression and excessive stiffness preventing micromotion at the fracture site.
Role of Hip Decompression
Multiple studies have documented low rates of AVN when treatment for femoral neck fractures is combined with joint decompression [9, 32, 37]. Most recently, Bukva et al. [32] found significantly lower incidence of AVN and better final outcomes with hip decompression; with needle aspiration and open drainage being equally effective. Contrarily, several authors have reported no significant difference in rates of AVN with and without decompression [21, 22, 33, 38, 39]. Interpretation of various reports is difficult as there are a number of confounding factors affecting the incidence of AVN, such as fracture type, displacement, time to surgery, fixation type etc. A recent systematic review concluded that capsular decompression provided no significant protection against AVN [22]. Direct vascular injury occurring at the time of the fracture is an important cause for AVN [15]; in such cases, the tamponade effect does not play a role and capsular decompression may not be able to prevent AVN.
Although its benefits have not definitively been proven, needle decompression is a simple procedure without any complications, and we advise that it be performed in all fractures treated by CR. A percutaneous capsulotomy can be performed under C-arm guidance using a no. 10 surgical blade during closed reduction and fixation [40]. After making sure that the blade is firmly fixed to the BP handle, slide the blade over the anterior aspect of the greater trochanter (knife edge facing the bone), in line with the center of the femoral neck on anteroposterior view. Complete the capsulotomy while observing the blade on the lateral view, making sure that the blade is right on top of the femur neck, both by feel and on imaging. A gush of hematoma fluid should be seen to ooze out of the wound once the capsulotomy is complete. A safer option is to perform an open anterior capsulotomy with direct visualization of the capsule, or to simply aspirate the hematoma using a large-bore needle [1].
Role of Timing of Surgery
Although most studies agree that earlier surgery leads to better outcomes [9, 32, 33, 39, 41], there is no consensus on how early surgery must be done to avoid complications. Studies have defined ‘early treatment’ variably as within 12, 24, 48 h and even 7 days from the injury [9, 32, 33, 41, 42]. A recent meta-analysis found no significant difference in AVN rates between early vs late treated cases (defined as < 24 and > 24 h from injury respectively) [42]. Furthermore, some authors suggest that the emphasis on early treatment may in fact lead to more complications, due to intra-operative errors by inexperienced surgeons; and that, delaying surgery in favor of skill may be preferable to the failures of early but inexperienced surgery [43].
Role of Primary Valgus Osteotomy
Although the valgus intertrochanteric osteotomy is usually used in cases of established non-union, a number of authors advocate its use in the primary treatment of displaced femoral neck fractures, particularly those with a high Pauwels angle and delayed presentation [44–46]. The osteotomy improves the likelihood of fracture healing by converting shear forces to compressive forces by placing the fracture line perpendicular to the resultant forces; the buttressing effect of the distal fragment on the head of femur from below also improves the stability of fixation [45]. An additional advantage is that the increased local blood flow due to the osteotomy has been shown to restore viability of a non-collapsed femoral head with AVN in children [47].
Management of Delbet Type IB Injuries
A special mention must be made of the trans-physeal separation with hip dislocation. This rare pattern of injury is typically seen after high-energy trauma, but has been also reported after attempted closed reduction for hip dislocations [1, 48]. There may be associated acetabular fractures and chondral damage [48–50]. Plain radiographs can be misleading and CT scanning is essential for assessing the true nature of the injury. Open reduction is always required, using either direct anterior, posterior (Kocher-Langenbeck) or safe surgical dislocation approach, depending upon the direction of dislocation and location of the epiphysis [1]. Care should be taken to preserve any remaining blood supply to the femoral head. The capital epiphysis must first be reduced into the acetabulum, followed by fixation with trans-physeal screws in the routine manner. Despite prompt and aggressive treatment, osteonecrosis almost always occurs; the poor prognosis must be explained.
The authors’ preferred approach to the management of paediatric femoral neck fractures is outlined in Table 2.
Table 2.
Authors’ preferred approach to management
| Timing |
Treat urgently, but not emergently (preferably within 12–24 h of trauma) An experienced surgeon should be present |
| Reduction |
A good reduction is essential Give one or two attempts at gentle closed reduction → If this fails, proceed to open reduction Delbet I, II: Smith-Petersen approach, separate lateral incision for implant placement Delbet III, IV: Watson-Jones approach for both reduction and fixation |
| Capsular decompression | If closed reduced, decompress the joint by percutaneous aspiration/capsulotomy |
| Fixation |
Choose implant according to fracture type and child’s skeletal maturity Delbet I–III: Multiple smooth pins in children < 3 years 4.5 mm CC screws in children 3–10 years 6.5/7 mm CC screws in adolescents Delbet IV: Paediatric size dynamic hip screw and de-rotation screw Do not compromise fixation to spare the physis! Have a low threshold for placing trans-physeal screws |
| Post-operatively |
Hip spica for children < 8 years of age for 6 weeks Knee immobilizer for older children and adolescents for 6 weeks |
CC cannulated cancellous
Complications
Despite recent advances, femoral neck fractures continue to be associated with higher rates of complications as compared to other childhood injuries [22]. A systematic review [22] comprising 935 cases of paediatric femur neck fracture reported complication rates as given in Table 3. All complications other than non-union are commoner in type I fractures [22].
Table 3.
Rates of various complications of paediatric femoral neck fractures [22]
| Complication | Overall rate (%) | Number of cases (number of studies that reported on the complication) |
|---|---|---|
| Avascular necrosis | 23 | 203 of 894 (30) |
| Non-union | 10.8 | 83 of 770 (24) |
| Coxa vara | 18.5 | 153 of 828 (27) |
| Premature physeal closure | 21.8 | 159 of 731 (22) |
| Chondrolysis | 13.5 | 10 of 74 (4) |
| Revision surgery | 19.2 | 74 of 386 (12) |
| Infections | 5.2 | 20 of 387 (11) |
Avascular Necrosis (AVN)
AVN is the most devastating and unfortunately the most frequent complication of paediatric femur neck fractures (Fig. 4). It is usually diagnosed within a year of the injury [2]. Prognosis is worse in adolescents (12–18 years) compared to small children (1–11 years) [51].
Fig. 4.

A 13 years old boy with a Delbet Type II neck femur fracture of the left hip. a One month post-operative radiograph of pelvis with both hips. He was treated with closed reduction and fixation with three cannulated cancellous lag screws. b Radiographs of pelvis with both hips AP and frog-leg lateral views at 1 year follow-up showing non-union of the fracture and avascular necrosis of the femoral head with collapse and deformation. The patient has pain and restriction of left hip joint motion
Risk Factors
A meta-analysis by Moon and Mehlman [8] identified four main risk factors for AVN, namely fracture type, displacement, age and treatment. AVN rate by Delbet classification was 38, 28, 18, and 5% for fracture types I–IV respectively. AVN developed in 25% of displaced fractures, compared to 9% of undisplaced fractures. AVN occurred in 26% fractures treated surgically vs 11% treated non-operatively. On logistic regression analysis, fracture type and age were identified as the only significant predictors of AVN. Fracture types I, II and III were 15, 6, and 4 times, respectively, more likely to develop AVN than type IV fractures; and older children were 1.14 times more likely to develop AVN for each year of increasing age. Another recent meta-analysis found that displaced and types I/II fractures were 3.8 and 2.4 times more likely to develop AVN, as compared to undisplaced and types III/IV fractures, respectively [42].
Younger children seem to be less at risk of AVN due to their superior capacity to revascularize and remodel the femoral head [8]. Adolescents on the other hand, retain the tenuous blood supply of childhood while lacking the remodeling capacity, which puts them at greater risk for developing AVN [8]. Although few studies have reported AVN rates to be higher following open as compared to closed reduction [22, 52], this likely represents a selection bias, as fractures that require OR are usually more severe ones, with an inherently higher risk of complications [22]. Most studies report lower rates of AVN and better outcomes in patients treated with OR [7, 28, 53]. Multiple attempts at CR probably cause more damage to the retinacular vessels, increasing the risk of AVN.
Management of AVN
There is no satisfactory treatment for established AVN. Qi et al. [54] described vascularized greater trochanter periosteal flap transposition at the time of fracture fixation as a technique to reduce the risk of AVN by increasing proximal femoral blood supply. Once AVN is diagnosed, prolonged periods of non-weight bearing may prevent severe femoral head collapse [55]. Scintigraphy has been advocated for assessment of vascularity to guide post-operative regimens [56]. Newer techniques such as intravenous bisphosphonate therapy and intraosseous injection of bone-marrow and bone morphogenetic protein-2 (BMP-2) in conjunction with core decompression have shown promise as therapeutic options for AVN, particularly in pre-collapse stages [57, 58]. Local injection of Ibandronate and BMP-2 has also shown improved bone healing and decreased deformity in animal models [59].
Non-union
The prevalence of non-union in paediatric femoral neck fractures has been reported to range from 0 to 44% [60]. The primary cause for non-union is failure to achieve or maintain adequate reduction [20, 43, 61–63].
Risk Factors
Non-union is most common in type II, and least common in type IV Delbet fractures [22]. In a review of 24 studies including 110 cases of non-union, 65% were type II fractures; 29% type III; 6% type I; and 0% type IV [60]. Fracture displacement, vertical orientation of fracture line, and damage to proximal femoral vascularity are other injury-related factors that contribute to poor fracture healing [16, 61, 62, 64]. Non-union used to be common in fractures treated non-operatively [2]; with recent trends towards internal fixation, non-union rates have declined [18, 19, 60, 65]. Nevertheless, it is still seen in fractures fixed in poor reduction [16, 43, 63]; fixed using less rigid implants (threaded pins/Kirschner wires) [60, 64]; and when fixation does not cross the physis thus compromising stability [22, 66]. Delayed presentation remains an important cause for non-union in developing countries [7, 39]. Resorption of the femoral neck and osteonecrosis usually complicate management of these ‘neglected’ cases [47].
Management of Non-union
In the treatment of femoral neck non-unions, the basic principle is to convert the shearing forces acting on the vertically oriented fracture line into compressive forces [47, 64, 66]. This is achieved by the valgus osteotomy, which not only corrects the abnormal biomechanics, but also addresses the coxa vara, shortening and deranged abductor moment arm (Fig. 5). The second important aspect of treatment is improvement of local biology by addition of bone graft [67, 68]. Vascularized iliac crest or fibula grafts are useful in cases with concomitant AVN. Fibula grafts have the advantage of providing structural support in addition to osteoconductive properties. Non-union and AVN frequently co-exist, however, this is not a contra-indication for surgery. In fact, once union is achieved, the femoral head tends to revascularize in children, and clinically significant collapse may not occur [60].
Fig. 5.

An 11 years old girl with a 6 months old neglected neck femur fracture of the right hip (case courtesy of Dr. Mandar Agashe). a Pre-operative radiographs of pelvis with both hips AP and frog-leg lateral views, showing non-union fracture neck femur on the right side. Note the sclerosis of the fracture edges. b Intra-operative c-arm AP and lateral views of the right hip after valgus osteotomy and fixation with paediatric DHS and cannulated cancellous de-rotation screw. The hip joint capsule was not opened and the fracture fragments were not debrided. c Radiograph of pelvis with both hips AP and frog-leg lateral views at 2 years follow-up showing complete union of the fracture and osteotomy, with excellent alignment
Sanghavi et al. [60] recently described an algorithm for the management of non-unions depending upon the underlying cause. Non-unions due to failure of fixation can be managed by removal of the offending implant, refixation without bone grafting, and valgus osteotomy. In non-unions due to delayed presentation, intervening fibrous tissue at the fracture site and resorption of the neck pose additional challenges; such cases must additionally receive a fibula strut graft to reconstruct the inferomedial aspect of the femoral neck. Open reduction with clearance of fibrous tissue risks damage to femoral head vascularity and is not recommended.
Coxa Vara
Coxa vara [neck-shaft angle (NSA) < 130°], is the second most common complication of paediatric femoral neck fractures. It is caused by malunion, osteonecrosis, premature physeal closure (PPC) or a combination of these factors. Historically, when these fractures were treated by manipulation and casting, rates of varus malunion were high; recent reports indicate that incidence of coxa vara may be reduced by use of internal fixation [5, 21, 43, 63]. However, internal fixation does not completely eliminate the risk; in a recent series [65], out of 22 children with type II and III fractures treated by cannulated screw fixation, coxa vara occurred in 12. The high incidence was attributed to loss of reduction because of implant failure. Early weight bearing and high shearing forces in vertical fracture lines may be important causes for implant failure [65].
In view of the potential for remodeling, a 2 year observation period is appropriate before considering surgery such as subtrochanteric valgus osteotomy for residual coxa vara [5].
Premature Physeal Closure
The factors most significantly associated with PPC are AVN and penetration of the physis by the fixation device [2, 62, 63]. Partial arrest results in coxa vara or valga, whereas complete closure results in limb length discrepancy (LLD). As the proximal femoral physis contributes to only 15% of the length of the femur, the LLD may not be significant, particularly when it occurs in older children. When PPC occurs in children < 10 years old, or those with > 2 years growth remaining, the resulting LLD may be severe enough to warrant treatment with contra-lateral femoral/tibial epiphysiodesis.
Other Complications
Other rare complications include chondrolysis, post-operative infection, LLD, coxa valga and slipped capital femoral epiphysis (SCFE). Chondrolysis is most often associated with AVN and has poor outcomes [38, 61]. Post-operative infections are usually superficial, but cases of septic arthritis have been reported [62, 63]. LLD occurs due to either PPC, coxa vara, AVN or a combination of these factors. Coxa valga (NSA > 150°) may occur due to lateral proximal femoral or trochanteric physeal arrest, and may rarely be iatrogenic [3, 37, 43, 63].
Outcomes
Long term outcomes of paediatric femoral neck fractures are most often described according to the classification of Ratliff [2] (Table 4). In a systematic review, out of 608 patients reported in 19 studies, outcomes were good in 59.7%, fair in 19.6% and poor in 20.7% [22].
Table 4.
Ratliff classification for evaluating outcomes of paediatric femoral neck fractures [2]
| Good | Fair | Poor | |
|---|---|---|---|
| Pain | None or ‘ignores’ | Occasional | ‘Disabling’ |
| Movement | Full or terminal restriction | Greater than 50% | Less than 50% |
| Activity | Normal or avoids games | Normal or avoids games | Restricted |
| Radiographic appearance | Normal or some deformity of the femoral neck |
Severe deformity of the femoral neck ‘Mild’ AVN |
Severe AVN Degenerative arthritis Arthrodesis |
Future Directions
The literature related to paediatric femoral neck fractures is limited by small sample sizes, inadequate follow-up, and non-standardized use of varied treatment modalities, thus making it difficult to compare outcomes. Most studies have been retrospective reports/series with low levels of evidence (III/IV). Large-scale prospective studies with long-term follow-up are needed to solve the unanswered questions regarding paediatric femoral neck fractures. Due to the rarity of this fracture, such studies would have to be multi-centered.
Summary
Femoral neck fractures in children usually result from high-energy trauma and are often associated with other injuries.
Either open or closed reduction may be performed, but the quality of reduction is paramount. An anatomical reduction leads to better outcomes.
Stable internal fixation should be the rule. Fracture stability is more important than sparing the physis—internal fixation should cross the physis whenever necessary.
In young children, always protect the fixation with a spica cast or brace.
Role of capsular decompression is controversial, however, it is simple to perform and without complications.
Timing of surgery is also controversial. Surgery should be performed as soon as possible, but in the presence of an experienced surgeon.
Osteonecrosis is the most common and devastating complication. Initial fracture displacement and disruption of retinacular vessels are factors causing AVN that are outside the surgeon’s control.
Non-union occurs primarily due to failure to achieve or maintain adequate reduction. Consider primary valgus osteotomy for displaced fractures that present late after injury.
Acknowledgements
We thank Mr. Darrell J. D’souza for illustrating Fig. 1.
Author Contributions
AA contributed to the study conception and design. Material preparation, data collection and analysis were performed by DP and AA. The first draft of the manuscript was written by DP and both authors commented on previous versions of the manuscript. Both authors read and approved the final manuscript.
Funding
This study has no funding support.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Standard Statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed Consent
The authors affirm that participants provided informed consent for publication of the images in Figs. 2, 3, 4, 5.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Deepika A. Pinto, Email: deepupinto@gmail.com
Alaric Aroojis, Email: aaroojis@gmail.com.
References
- 1.Patterson JT, Tangtiphaiboontana J, Pandya NK. Management of pediatric femoral neck fracture. Journal of American Academy of Orthopaedic Surgeons. 2018;26(12):411–419. doi: 10.5435/JAAOS-D-16-00362. [DOI] [PubMed] [Google Scholar]
- 2.Ratliff AH. Fractures of the neck of the femur in children. The Journal of Bone and Joint Surgery British Volume. 1962;44B(3):528–542. doi: 10.1302/0301-620X.44B3.528. [DOI] [PubMed] [Google Scholar]
- 3.Mirdad T. Fractures of the neck of femur in children: An experience at the Aseer Central Hospital, Abha, Saudi Arabia. Injury. 2002;33(9):823–827. doi: 10.1016/s0020-1383(02)00013-x. [DOI] [PubMed] [Google Scholar]
- 4.Azouz EM, Karamitsos C, Reed MH, Baker L, Kozlowski K, Hoeffel J-C. Types and complications of femoral neck fractures in children. Pediatric Radiology. 1993;23(6):415–420. doi: 10.1007/BF02012436. [DOI] [PubMed] [Google Scholar]
- 5.Hughes LO, Beaty JH. Fractures of the head and neck of the femur in children. The Journal of Bone and Joint Surgery. 1994;76(2):283–292. doi: 10.2106/00004623-199402000-00019. [DOI] [PubMed] [Google Scholar]
- 6.Colonna PC. Fracture of the neck of the femur in children. American Journal of Surgery. 1929;6(6):793–797. [Google Scholar]
- 7.Ju L, Jiang B, Lou Y, Zheng P. Delayed treatment of femoral neck fractures in 58 children: Open reduction internal fixation versus closed reduction internal fixation. Journal of Pediatric Orthopaedics Part B. 2016;25(5):459–465. doi: 10.1097/BPB.0000000000000339. [DOI] [PubMed] [Google Scholar]
- 8.Moon ES, Mehlman CT. Risk factors for avascular necrosis after femoral neck fractures in children: 25 Cincinnati cases and meta-analysis of 360 cases. Journal of Orthopaedic Trauma. 2006;20(5):323–329. doi: 10.1097/00005131-200605000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Panigrahi R, Sahu B, Mahapatra AK, Palo N, Priyadarshi A, Biswal MR. Treatment analysis of paediatric femoral neck fractures: A prospective multicenter theraupetic study in Indian scenario. International Orthopaedics. 2015;39(6):1121–1127. doi: 10.1007/s00264-015-2677-y. [DOI] [PubMed] [Google Scholar]
- 10.Shen M, Wang C, Chen H, Rui YF, Zhao S. An update on the Pauwels classification. Journal of Orthopaedic Surgery and Research. 2016;11(1):1–7. doi: 10.1186/s13018-016-0498-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gautier E, Ganz K, Krügel N, Gill T, Ganz R. Anatomy of the medial femoral circumflex artery and its surgical implications. The Journal of Bone and Joint Surgery. 2000;82(5):679–683. doi: 10.1302/0301-620x.82b5.10426. [DOI] [PubMed] [Google Scholar]
- 12.Chung S. The arterial supply of the developing proximal end of the human femur. The Journal of Bone and Joint Surgery. 1976;58(7):961–970. [PubMed] [Google Scholar]
- 13.Seeley MA, Georgiadis AG, Sankar WN. Hip vascularity: A review of the anatomy and clinical implications. Journal of American Academy of Orthopaedic Surgeons. 2016;24(8):515–526. doi: 10.5435/JAAOS-D-15-00237. [DOI] [PubMed] [Google Scholar]
- 14.Trueta J. The normal vascular anatomy of the human femoral head during growth. Journal of Bone and Joint Surgery. British Volume. 1957;39B(2):358–394. doi: 10.1302/0301-620X.39B2.358. [DOI] [PubMed] [Google Scholar]
- 15.Boardman MJ, Herman MJ, Buck B, Pizzutillo PD. Hip fractures in children. Journal of American Academy of Orthopaedic Surgeons. 2009;17(3):162–173. doi: 10.5435/00124635-200903000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Dial BL, Lark RK. Pediatric proximal femur fractures. Journal of Orthopaedics. 2018;15(2):529–535. doi: 10.1016/j.jor.2018.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sferopoulos NK, Papavasiliou VA. “Natural” healing of hip fractures in childhood. Injury. 1994;25(8):493–496. doi: 10.1016/0020-1383(94)90087-6. [DOI] [PubMed] [Google Scholar]
- 18.Forster NA, Ramseier LE, Exner GU. Undisplaced femoral neck fractures in children have a high risk of secondary displacement. Journal of Pediatric Orthopaedics Part B. 2006;15(2):131–133. doi: 10.1097/01.bpb.0000188249.17148.eb. [DOI] [PubMed] [Google Scholar]
- 19.Bali K, Sudesh P, Patel S, Kumar V, Saini U, Dhillon MS. Pediatric femoral neck fractures: our 10 years of experience. Clinics in Orthopedic Surgery. 2011;3(4):302–308. doi: 10.4055/cios.2011.3.4.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kay SP, Hall JE. Fracture of the femoral neck in children and its complications. Clinical Orthopaedics and Related Research. 1971;80:53–71. doi: 10.1097/00003086-197110000-00009. [DOI] [PubMed] [Google Scholar]
- 21.Shrader MW, Jacofsky DJ, Stans AA, Shaughnessy WJ, Haidukewych GJ. Femoral neck fractures in pediatric patients: 30 years experience at a level 1 trauma center. Clinical Orthopaedics and Related Research. 2007;454:169–173. doi: 10.1097/01.blo.0000238794.82466.3d. [DOI] [PubMed] [Google Scholar]
- 22.Yeranosian M, Horneff JG, Baldwin K, Hosalkar HS. Factors affecting the outcome of fractures of the femoral neck in children and adolescents. The Bone Joint Journal. 2013;95-B(1):135–142. doi: 10.1302/0301-620X.95B1.30161. [DOI] [PubMed] [Google Scholar]
- 23.Sankar WN, Mehlman CT. The community orthopaedic surgeon taking trauma call: pediatric femoral neck fracture pearls and pitfalls. Journal of Orthopaedic Trauma. 2019;33(8):S22–S26. doi: 10.1097/BOT.0000000000001541. [DOI] [PubMed] [Google Scholar]
- 24.Song K-S. Displaced fracture of the femoral neck in children. The Journal of Bone and Joint Surgery. British Volume. 2010;92-B(8):1148–1151. doi: 10.1302/0301-620X.92B8.24482. [DOI] [PubMed] [Google Scholar]
- 25.Whitman R. A new method of treatment for fracture of the neck of the femur, together with remarks on coxa vara. Annals of Surgery. 1902;36(5):746–761. doi: 10.1097/00000658-190211000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leadbetter GW. Non-operative treatment for fracture of the neck of the femur. American Journal of Surgery. 1937;38(3):612–618. [Google Scholar]
- 27.Flynn M. A new method of reduction of fractures of the neck of the femur based on anatomical studies of the hip joint. Injury. 1973;5(4):309–317. [PubMed] [Google Scholar]
- 28.Chen Y, Zhang X, Guo H, Liu N, Ren J, Lu C. Poor outcomes of children and adolescents with femoral neck fractures: a meta-analysis based on clinical studies. Orthopaedic Surgery. 2020;12(2):639–644. doi: 10.1111/os.12629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lichstein PM, Kleimeyer JP, Githens M, Vorhies JS, Gardner MJ, Bellino M, et al. Does the Watson-Jones or modified Smith-Petersen approach provide superior exposure for femoral neck fracture fixation? Clinical Orthopaedics and Related Research. 2018;476(7):1468–1476. doi: 10.1097/01.blo.0000533627.07650.bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chan DS. Femoral neck fractures in young patients. Journal of Orthopaedic Trauma. 2019;33(1):S7–S11. doi: 10.1097/BOT.0000000000001366. [DOI] [PubMed] [Google Scholar]
- 31.Medda S, Snoap T, Carroll EA. Treatment of young femoral neck fractures. Journal of Orthopaedic Trauma. 2019;33(1):S1–S6. doi: 10.1097/BOT.0000000000001369. [DOI] [PubMed] [Google Scholar]
- 32.Bukva B, Abramović D, Vrgoč G, Marinović M, Bakota B, Dučić S, et al. Femoral neck fractures in children and the role of early hip decompression in final outcome. Injury. 2015;46:S44–S47. doi: 10.1016/j.injury.2015.10.059. [DOI] [PubMed] [Google Scholar]
- 33.Flynn JM, Wong KL, Yeh GL, Meyer JS, Davidson RS. Displaced fractures of the hip in children. The Journal of Bone and Joint Surgery. 2002;84(1):108–112. doi: 10.1302/0301-620x.84b1.11972. [DOI] [PubMed] [Google Scholar]
- 34.Augat P, Bliven E, Hackl S. Biomechanics of femoral neck fractures and implications for fixation. Journal of Orthopaedic Trauma. 2019;33(1):S27–S32. doi: 10.1097/BOT.0000000000001365. [DOI] [PubMed] [Google Scholar]
- 35.Duffin M, Pilson HT. Technologies for young femoral neck fracture fixation. Journal of Orthopaedic Trauma. 2019;33(1):S20–S26. doi: 10.1097/BOT.0000000000001367. [DOI] [PubMed] [Google Scholar]
- 36.Levack AE, Gausden EB, Dvorzhinskiy A, Lorich DG, Helfet DL. Novel treatment options for the surgical management of young femoral neck fractures. Journal of Orthopaedic Trauma. 2019;33(1):S33–S37. doi: 10.1097/BOT.0000000000001368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ng GPK, Cole WG. Effect of early hip decompression on the frequency of avascular necrosis in children with fractures of the neck of the femur. Injury. 1996;27(6):419–421. doi: 10.1016/0020-1383(96)00025-3. [DOI] [PubMed] [Google Scholar]
- 38.Dhammi IK, Singh S, Jain AK. Displaced femoral neck fracture in children and adolescents: Closed versus open reduction—A preliminary study. Journal of Orthopaedic Science. 2005;10(2):173–179. doi: 10.1007/s00776-004-0875-3. [DOI] [PubMed] [Google Scholar]
- 39.Varshney MK, Kumar A, Khan SA, Rastogi S. Functional and radiological outcome after delayed fixation of femoral neck fractures in pediatric patients. Journal of Orthopaedics and Traumatology. 2009;10(4):211–216. doi: 10.1007/s10195-009-0072-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ly TV, Swiontkowski MF. Treatment of femoral neck fractures in young adults. Instructional Course Lectures. 2009;58(11):69–81. [PubMed] [Google Scholar]
- 41.Dhar SA, Ali MF, Dar TA, Sultan A, Butt MF, Kawoosa AA, et al. Delayed fixation of the transcervical fracture of the neck of the femur in the pediatric population: results and complications. Journal of Children’s Orthopaedics. 2009;3(6):473–477. doi: 10.1007/s11832-009-0209-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.AlKhatib N, Younis MH, Hegazy A, Ibrahim T. Early versus late treatment of paediatric femoral neck fractures: a systematic review and meta-analysis. International Orthopaedics. 2019;43(3):677–685. doi: 10.1007/s00264-018-3998-4. [DOI] [PubMed] [Google Scholar]
- 43.Togrul E, Bayram H, Gulsen M, Kalaci A, Özbarlas S. Fractures of the femoral neck in children: long-term follow-up in 62 hip fractures. Injury. 2005;36(1):123–130. doi: 10.1016/j.injury.2004.04.010. [DOI] [PubMed] [Google Scholar]
- 44.Singh MP, Aggarwal AN, Arora A, Dhammi IK, Singh J. Unstable recent intracapsular femoral neck fractures in young adults: osteosynthesis and primary valgus osteotomy using broad dynamic compression plate. Indian Journal of Orthopaedics. 2008;42(1):43–48. doi: 10.4103/0019-5413.38580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Magu NK, Singh R, Mittal R, Garg R, Wokhlu A, Sharma AK. Osteosynthesis and primary valgus intertrochanteric osteotomy in displaced intracapsular fracture neck of femur with osteoporosis in adults. Injury. 2005;36(1):110–122. doi: 10.1016/j.injury.2004.02.017. [DOI] [PubMed] [Google Scholar]
- 46.Eid A. Valgus osteotomy for delayed presentation of femoral neck fractures Pauwels Grade III. Journal of Orthopaedic Trauma. 2010;24(2):115–119. doi: 10.1097/BOT.0b013e3181bdc2c3. [DOI] [PubMed] [Google Scholar]
- 47.Magu NK, Singh R, Sharma AK, Ummat V. Modified Pauwels’ intertrochanteric osteotomy in neglected femoral neck fractures in children: a report of 10 cases followed for a minimum of 5 years. Journal of Orthopaedic Trauma. 2007;21(4):237–243. doi: 10.1097/BOT.0b013e31804cfdad. [DOI] [PubMed] [Google Scholar]
- 48.Mohammad S, Port A, Montgomery RJ. Transepiphyseal fracture of the femoral neck with dislocation of the femoral head and fracture of the posterior column of the acetabulum in a child. Journal of Bone and Joint Surgery. British Volume. 2002;84(1):113–115. doi: 10.1302/0301-620x.84b1.11889. [DOI] [PubMed] [Google Scholar]
- 49.Elmadag M, Ceylan HH, Erdem AC, Bilsel K, Uzer G, Acar MA. Pediatric transepiphyseal seperation and dislocation of the femoral head. Case Reports in Orthopedics. 2013;2013:703850. doi: 10.1155/2013/703850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shaath MK, Shah H, Adams MR, Sirkin MS, Reilly MC. Management and outcome of transepiphyseal femoral neck fracture-dislocation with a transverse posterior wall acetabular fracture: a case report. JBJS Case Connector. 2018;8(3):e64. doi: 10.2106/JBJS.CC.18.00043. [DOI] [PubMed] [Google Scholar]
- 51.Pforringer W, Rosemeyer B. Fractures of the hip in children and adolescents. Acta Orthopaedica Scandinavica. 1980;51(1–6):91–108. doi: 10.3109/17453678008990774. [DOI] [PubMed] [Google Scholar]
- 52.Dendane MA, Amrani A, El Alami ZF, El Medhi T, Gourinda H. Displaced femoral neck fractures in children: are complications predictable? Orthopaedics & Traumatology: Surgery & Research. 2010;96(2):161–165. doi: 10.1016/j.rcot.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 53.Stone JD, Hill MK, Pan Z, Novais EN. Open reduction of pediatric femoral neck fractures reduces osteonecrosis risk. Orthopedics. 2015;38(11):e983–e990. doi: 10.3928/01477447-20151020-06. [DOI] [PubMed] [Google Scholar]
- 54.Qi B, Yu A, Zhang G, Yu G, Shi Y, Zhu S, et al. The treatment of displaced femoral neck fractures with vascularized great trochanter periosteal flap transposition in children. Microsurgery. 2008;28(1):21–24. doi: 10.1002/micr.20439. [DOI] [PubMed] [Google Scholar]
- 55.Maeda S, Kita A, Fujii G, Funayama K, Yamada N, Kokubun S. Avascular necrosis associated with fractures of the femoral neck in children: histological evaluation of core biopsies of the femoral head. Injury. 2003;34(4):283–286. doi: 10.1016/s0020-1383(02)00281-4. [DOI] [PubMed] [Google Scholar]
- 56.Juréus J, Geijer M, Tiderius CJ, Tägil M. Vascular evaluation after cervical hip fractures in children: a case series of eight children examined by scintigraphy after surgery for cervical hip fracture and evaluated for development of secondary radiological changes. Journal of Pediatric Orthopaedics Part B. 2016;25(1):17–23. doi: 10.1097/BPB.0000000000000217. [DOI] [PubMed] [Google Scholar]
- 57.Ramachandran M, Ward K, Brown RR, Munns CF, Cowell CT, Little DG. Intravenous bisphosphonate therapy for traumatic osteonecrosis of the femoral head in adolescents. The Journal of Bone and Joint Surgery. 2007;89(8):1727–1734. doi: 10.2106/JBJS.F.00964. [DOI] [PubMed] [Google Scholar]
- 58.Gao F, Sun W, Guo W, Wang B, Cheng L, Li Z. Combined with bone marrow-derived cells and rhBMP-2 for osteonecrosis after femoral neck fractures in children and adolescents: a case series. Scientific Reports. 2016;6(1):30730. doi: 10.1038/srep30730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Vandermeer JS, Kamiya N, Aya-ay J, Garces A, Browne R, Kim HKW. Local administration of ibandronate and bone morphogenetic protein-2 after ischemic osteonecrosis of the immature femoral head. The Journal of Bone and Joint Surgery-American Volume. 2011;93(10):905–913. doi: 10.2106/JBJS.J.00716. [DOI] [PubMed] [Google Scholar]
- 60.Sanghavi S, Patwardhan S, Shyam A, Nagda T, Naik P. Nonunion in pediatric femoral neck fractures. The Journal of Bone and Joint Surgery. 2020;102(11):1000–1010. doi: 10.2106/JBJS.19.01117. [DOI] [PubMed] [Google Scholar]
- 61.Forlin E, Guille JT, Kumar SJ, Rhee KJ. Complications associated with fracture of the neck of the femur in children. Journal of Pediatric Orthopedics. 1992;12(4):503–509. doi: 10.1097/01241398-199207000-00017. [DOI] [PubMed] [Google Scholar]
- 62.Canale ST, Bourland WL. Fracture of the neck and intertrochanteric region of the femur in children. Journal of Bone and Joint Surgery. American Volume. 1977;59(4):431–443. [PubMed] [Google Scholar]
- 63.Morsy HA. Complications of fracture of the neck of the femur in children. A long-term follow-up study. Injury. 2001;32(1):45–51. doi: 10.1016/s0020-1383(00)00109-1. [DOI] [PubMed] [Google Scholar]
- 64.Neto PFT, dos Reis FB, Filho JL, Fernandes HJA, Fujiki EN, Bensahel H, et al. Nonunion of fractures of the femoral neck in children. Journal of Children’s Orthopaedics. 2008;2(2):97–103. doi: 10.1007/s11832-008-0078-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Eberl R, Singer G, Ferlic P, Weinberg AM, Hoellwarth ME. Post-traumatic coxa vara in children following screw fixation of the femoral neck. Acta Orthopaedica. 2010;81(4):442–445. doi: 10.3109/17453674.2010.501744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Eamsobhana P, Keawpornsawan K. Nonunion paediatric femoral neck fracture treatment without open reduction. Hip International. 2016;26(6):608–611. doi: 10.5301/hipint.5000382. [DOI] [PubMed] [Google Scholar]
- 67.Elgeidi A, El-Negery A. Fibular strut graft for nonunited femoral neck fractures in children. Journal of Children’s Orthopaedics. 2017;11(1):28–35. doi: 10.1302/1863-2548-11-160221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Nagi ON, Dhillon MS, Gill SS. Fibular osteosynthesis for delayed type II and type III femoral neck fractures in children. Journal of Orthopaedic Trauma. 1992;6(3):306–313. doi: 10.1097/00005131-199209000-00007. [DOI] [PubMed] [Google Scholar]


