Abstract
Introduction
Paediatric ankle fractures represents about 5% of all paediatric fractures. It is the most common physis to be injured in the lower limb accounting to approximately 15–20% of all physeal injuries. This article reviews the literature on this common injury which still has many controversial areas and gives guidelines to management based on the existing evidence along with clinical experience gained from a Level I trauma center.
Classification
The original Salter–Harris Classification with the additional types is a good system to guide on the management. The transitional fractures form a separate group with technically two broad types—biplane and triplane injuries. Though there are many sub-types in this group with some popular eponymous fractures, the treatment principles remain the same.
Management
A very low threshold for CT scan is recommended when there is a clinical suspicion of fracture with a negative radiograph or an intra-articular fracture in the radiograph especially in the adolescent age group. CT scan helps in accurate quantification of the intra-articular displacement and also helps to comprehend the fracture geometry better. All the intra-articular fractures with displacement > 2 mm need perfect anatomical reduction and stabilization. Assisted closed reduction and percutaneous fixation along with arthrogram to confirm articular congruity is acceptable as long as the reduction is perfect. Irrespective of the method of treatment, in children with more than 2 years of growth remaining it is important to counsel regarding the high incidence of pre-mature physeal closure and the need for regular follow-up.
Keywords: Ankle, Fracture, Paediatric, Treatment, Physeal, Injury
Introduction
Paediatric ankle fractures are those fractures involving the distal end of the tibia and fibula from the metaphysis to the epiphysis. With an approximate incidence of 1 in 1000 children per year, ankle fractures represent approximately 5% of all pediatric fractures [1, 2]. The incidence of paediatric ankle fractures in our trauma center is 4%, based on the data from 2015 to 2019. Ankle fractures are the most common physeal injuries in the lower limb representing 15–20% of all physeal injuries [2]. The frequency is twice in boys as compared to girls, partially attributed to the delayed physeal closure in boys. The peak incidence is between the age of 8 and 15 years. Sports and twisting injuries are the most common mechanism followed by low energy falls and motor vehicle injuries.
Ankle Anatomy
The ankle joint or the talocrural joint is the only example of a true mortise joint in the human body where the mortise is formed by the distal tibia, fibula and the distal tibio-fibular syndesmosis and the tenon is formed by the talar dome. Though a hinge joint with dorsiflexion and plantarflexion as the main movements, the axis of rotation of ankle joint is dynamically shifting during plantar flexion and dorsiflexion. As the talar dome is wider anteriorly, the joint adopts a close-packed position with maximum congruence and ligamentous tension in dorsiflexion. On the contrary, during plantar flexion there is some room for minimal translation and rotational movements which places the ankle at higher risk of fracture in this position.
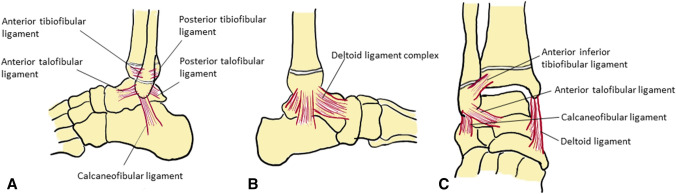
The ankle is stabilized by a very strong complex of ligaments (Fig. 1). The medial collateral ligament or deltoid ligament has superficial and deep parts and the lateral collateral ligament is formed of anterior and posterior talo-fibular and calcaneo-fibular ligaments. The distal tibio-fibular joint is a syndesmotic joint formed by the anterior, interosseous and posterior tibio-fibular ligaments. The anterior inferior tibio-fibular ligament plays a role in transitional fractures. The paediatric ankle fractures are distinctly different from the adult counterpart because of the basic anatomical difference with the existence of physis in the distal tibia and fibula. The collateral ligaments are attached below the level of the physis and are stronger compared to the physis. An undue force results in physeal injuries rather than ligamentous injuries in children [3]. A fracture involving the physis can potentially lead to physeal bar formation or premature physeal closure resulting in angular deformities and shortening which needs to be vigilantly observed and addressed appropriately.
Fig. 1.
Ligaments of the ankle: a Lateral view of the ankle showing the lateral ligament complex and anterior and posterior tibiofibular ligaments; b Medial view of the ankle showing the deltoid ligament complex; c antero-posterior view showing anterior inferior tibifibular ligament, anterior talofibular ligament, calcaneofibular ligament and deltoid ligament
Classifications
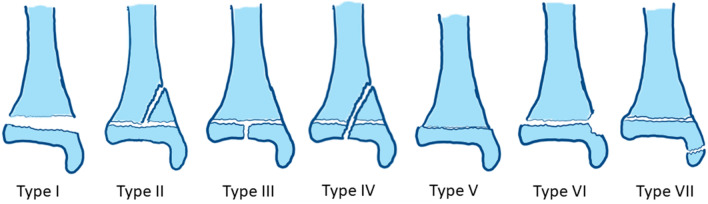
There are two common classification systems used for paediatric ankle fractures. The Salter & Harris classification of physeal injuries is commonly used in clinical practice for decision making and management. The original Salter–Harris (SH) classification had five types and Mercer Rang described type VI as the perichondrial ring injury. Type VII was described by Ogden in 1982 which are pure intra-epiphyseal fractures [4]. Ankle is one of the common areas to get Type VII fractures in form of medial and lateral malleolus avulsion fractures (Fig. 2).
Fig. 2.
Salter–Harris Classification: Type I—fracture through the physis and there is complete separation of the epiphysis; Type II—fracture through the physis and exiting into the metaphysis forming the Thurston–Holland fragment; Type III—fracture through the physis and exiting into the epiphysis; Type IV—fracture through metaphysis, physis and epiphysis; Type V—compression injury of physis; Type VI—perichondrial ring injury; Type VII—Intra-epiphyseal fracture
The Dias and Tachdjian Classification attempts to classify the injury based on the position of foot and direction of the deforming force similar to the Lauge-Hansen Classification in adults (Fig. 3). This could help the surgeon during closed manipulation of ankle fractures. The Supination-Inversion injuries are the most common injuries and it can have many variants depending on the stage of the injury. Stage I starts with isolated SH type I injury of distal fibula (Fig. 3a) and progress to either SH type I, II, III or IV injuries of the distal tibia (Fig. 3b–e). Supination-External rotation injury starts with the spiral fracture of the posterior part of distal tibia (Fig. 3f) and progress to the next stage of a spiral fracture of the distal fibula (Fig. 3g). The supination-plantar flexion injury causes SH type II fracture of the posterior distal tibia (Fig. 3h). Pronation-External rotation injuries result in SH type II fracture of the lateral aspect of the distal tibia with an associated fibular diaphyseal fracture (Fig. 3i). The Tillaux fractures and Triplane fractures are exclusive of these classification systems and are described separately as transitional fractures.
Fig. 3.
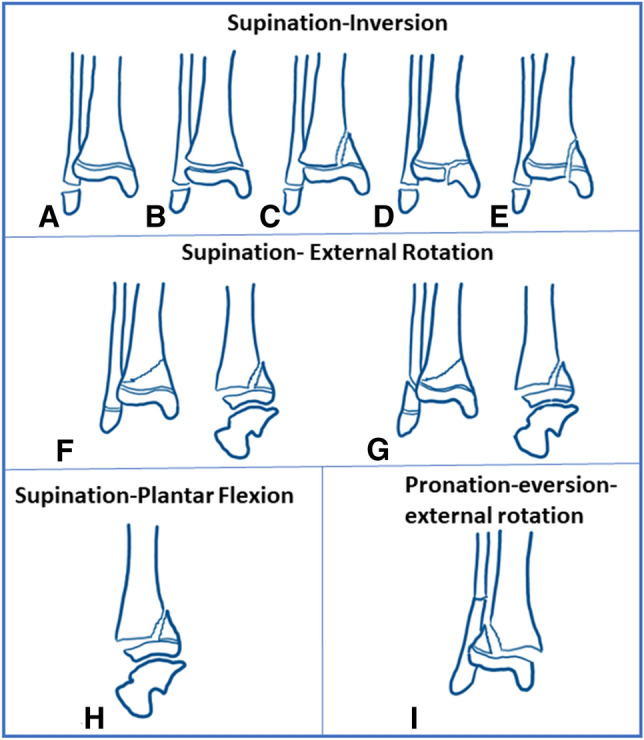
Dias–Tachdjian Classification: a–e various grades of Supination-Inversion injuries; f, g supination-external rotation injuries; h Lateral view of supination-plantar flexion injury; i Mortise view of pronation-eversion-external rotation injury
Evaluation
The details of the mechanism of injury and the course of symptoms is difficult to ascertain in the pediatric population. Despite this, a complete history is extremely important. A careful evaluation of the entire child and the affected lower limb is very important, as the underlying hip and knee malalignment may lead to an ankle injury event. The position of ankle and foot at times give a clue for the mechanism of injury and assist in the reduction maneuver.
The skin condition (swelling, ecchymosis, skin tenting, open fracture), distal pulses, capillary refill, sensory and motor (active toe movements) function should be evaluated. Any severe fracture displacement or ankle subluxation with skin tenting (especially on the medial aspect of ankle) demands urgent reduction of the ankle joint and stabilization with a well-padded posterior splint in the emergency room. Although compartment syndrome is rare following isolated ankle fractures, it has been reported and should be carefully ruled out [5, 6]. The extensor retinaculum syndrome is reported to be due to compression of the structures (notably the deep peroneal nerve) in the anterior aspect of the ankle by the displaced fracture fragments. The classical clinical findings are pain out of proportion to the injury, hypoesthesia or anaesthesia of the first webspace, and weakness of toe extensors [7, 8].
Diffuse soft tissue swelling and ecchymosis should raise the suspicion of bony injury. Ankle sprains are a diagnosis of exclusion in children, especially under age 10, and should be differentiated from a subtle physeal injury, by focussed physical examination [1].
Child abuse and pathological fractures should be considered if the history and mechanism of injury do not match the fracture type present. Though classic radiographic findings, such as corner fractures and multiple fractures in different stages of healing is seen in child abuse, isolated fractures are seen in up to 50% of cases, and the fracture patterns are often unremarkable [9].
Imaging
Anteroposterior, lateral and mortise radiographs are the ‘ankle trauma series’ views which is recommended for children presenting with ankle trauma. The Ottawa Ankle rules recommend radiographs if the child cannot weight bear and walk four steps at the time of evaluation and has bony tenderness in the tip of either malleoli [10]. Radiographic images should be evaluated for physeal widening, which may indicate an SH-l fracture. The plafond and mortise should be carefully examined for evidence of an intra-articular fracture pattern, such as a Tillaux or triplane fracture, as these findings can be quite subtle. On a standard anteroposterior view, the lateral portion of the distal tibial physis is partially obscured by the distal fibula. The vertical component of a triplane or Tillaux fracture can be hidden behind the overlying fibular cortical shadow; so a good quality mortise view is essential to view the syndesmosis and subtle fractures [11]. The routine use of stress views is not recommended in pediatric ankle fractures as they are unlikely to change the treatment. The radiographic appearance of tibial incisura, tibiofibular clear space, tibiofibular overlap and medial clear space changes with age in children and hence the normal adult values cannot be extrapolated [12, 13]. Bozic et al. found that the incisura became detectable at a mean age of 8.2 years for girls and 11.2 years for boys [13]. The range of clear space measurements in normal children was 2 to 8 mm, with 23% of children having a clear space greater than 6 mm, a distance considered abnormal in adults. Acquiring the radiograph of the normal contralateral ankle for comparison will be of great value for decision making in doubtful clinical situations.
Computed tomography has a significant role in the evaluation of paediatric ankle fractures. If radiographs are suspicious for an intraarticular fracture, computed tomography (CT) imaging should be obtained to evaluate the amount of displacement and articular congruity. In the adolescent age group, it is better to have a low threshold for obtaining CT scans rather than missing an innocuous fracture. At times, a CT scan is indicated to rule out fracture even with a normal looking X-ray when there is a strong clinical suspicion of fracture and the child is not able to bear weight (Fig. 4). CT scan is most commonly indicated for transitional fractures to study the configuration of fracture, the number of fracture fragments and displacement and also to plan the fixation. Though some authors have concluded that CT scan would not significantly change the way these fractures are managed, there is enough evidence in the literature to support the use of routine CT scan to analyse and treat these fractures [14–17]. Many a time, there would be a change of treatment plan after viewing CT imaging because of the significant intraarticular displacement that is difficult to appreciate on plain radiographs [16].
Fig. 4.
a, b, c AP, mortise and lateral views of the ankle in a 12-year-old girl who presented with ankle trauma which apparently looks normal and no fracture lines are seen; d–g coronal, sagittal and axial CT sections of the same patient showing a three-part triplane fracture with significant intra-articular displacement
Role of MRI in acute pediatric ankle fractures is limited and is not usually recommended. The relative indication may be to differentiate low-risk ankle injuries such as sprains from nondisplaced SH-l and SH-ll fractures, and in suspected osteochondral lesions. In radiograph-negative lateral ankle injuries in children, though MRI helps to detect the subtle physeal injuries, it does not significantly change the treatment plan and clinical outcomes [18, 19].
Treatment
General Principles
The main goals in the treatment of paediatric ankle fractures are to get an anatomical union, achieve physeal alignment and articular congruity, avoid growth arrest and prevent deformities which would ensure normal functioning of the ankle joint without the early onset of degenerative arthritis.
All undisplaced fractures are amenable for a trial of conservative treatment. All displaced fractures need closed reduction with or without internal fixation depending on the stability of the fracture post-reduction. Failure to achieve closed reduction is an indication for open reduction and internal fixation. It is important to ensure that the child is adequately relaxed with general or regional anaesthesia before an attempted closed reduction. One should avoid multiple forceful attempts at a reduction which could inflict damage to the growth plate, though studies have not shown a significant association between a number of attempts at reduction and development of premature physeal closure(PPC) [20, 21]. Assisted reduction techniques using K wires and Steinmann pins as joysticks along with intra-operative arthrogram to assess the articular congruity is acceptable as long as a perfect reduction is achieved. The internal fixation should preferably be a physis sparing construct. In situations where crossing the physis is deemed mandatory to achieve adequate stability, smooth wires are preferred. For tension band wiring, delayed absorbable suture materials should be used instead of stainless wires which would need removal to restore the growth of the physis.
In delayed fractures which are presenting more than one week, the general principle is to avoid forceful manipulation as it would damage the growth plate. However, in grossly displaced Salter-Harris Type I & II fractures and displaced Type III & IV fractures open reduction and internal fixation is needed to restore the normal ankle anatomy. In these instances, the parents must be counselled in detail pre-operatively about the chances of growth arrest, shortening, angular deformities and need for later interventions to address all these problems. It is best to have a shared decision making on a case-to-case basis after discussing all options including the possibility of ipsilateral osteosynthesis with epiphysiodesis combined with primary contralateral epiphysiodesis to avoid further complications and limb length discrepancy.
Salter–Harris Type I Injuries
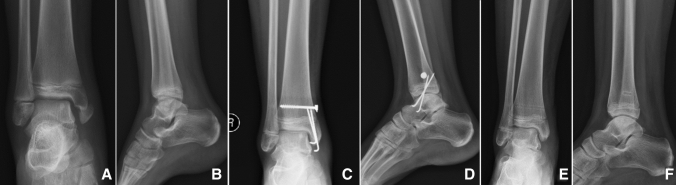
Salter-Harris Type I injuries of the distal tibia account to about 15% of all distal tibial physeal injuries [22]. Isolated distal tibial type I injuries are rarely displaced when there is no concomitant distal fibular injury [23]. A below-knee cast is recommended for all undisplaced distal tibial type I injuries for a period of 3 to 4 weeks. If there are concerns about patient compliance, an above-knee cast may be applied. All displaced distal tibial physeal injuries need closed reduction and above-knee cast application with the knee in 20° flexion. A check X-ray at 1 week is recommended to look for loss of reduction. A below-knee cast is sufficient if the surgeon opts to internally stabilize the fracture, when the reduction is unstable (Fig. 5).
Fig. 5.
a, b AP & lateral view of radiographs showing a displaced and angulated SH I fracture of the distal tibia; c, d AP & lateral post-operative radiographs after closed reduction and percutaneous pin stabilization; e, f AP & lateral radiographs at 6 months follow-up showing good union
SH type I distal fibular fractures are not as common as it was previously thought [18]. Studies have shown that the clinical diagnosis of SH I injuries of the distal fibula in children with normal-looking X-rays could be erroneous. MRI based studies have shown that 80% of these children have ligament injuries [19]. These suspected SH I injuries can be safely treated with a below-knee walking cast as tolerated or an ankle brace, as the outcomes between those children with MRI proven physeal injury and those with ligament sprain were the same.
Salter–Harris Type II Injuries
Salter-Harris Type II is the most common type of paediatric ankle fracture and constitutes 32–58% of all distal tibial physeal injuries in various series [20–22, 24]. An undisplaced SH type II fracture can be treated on a below-knee cast for 4 weeks followed by gradual weight bearing and mobilization.
The treatment of displaced SH type II injuries is quite controversial in the literature [20, 25–27]. Closed reduction and immobilization in an above knee cast with knee in 20° flexion are recommended for all displaced fractures. Phan et al. has reported that up to 61% of patients in their series had external rotation deformity and hence recommended an above-knee cast to control the rotations[28]. The adequacy of closed reduction is determined by the gap at the fracture site post-reduction. A gap of > 3 mm is reported to result in premature physeal closure in up to 60% of the patients [20].
There have been controversial reports in the literature on the need for open reduction in Salter-Harris Type II fractures. The overall incidence of PPC in SH I & II injuries is 13% in the meta-analysis published in 2018 [29]. The reported incidence varies between 14% and 42.7% in different series (Table 1) [20, 21, 25–27, 30]. In 2003, Barmada et al. analysed 92 SH type I & II factures and reported that those fractures with post-reduction residual gap of > 3 mm had high rates of PPC [20]. They postulated that this could be due to periosteal interposition and recommended open reduction. In 2006, Rohmiller et al. concluded that open reduction resulted in significantly less incidence of PPC in supination-external rotation injuries; however, there was no significant difference while all injuries were taken into consideration [26]. Later in 2013, Russo et al. published an analysis of 96 patients and concluded that open reduction did not reduce the risk of PPC [27]. In the meta-analysis by Asad et al. published in 2018, it was concluded that the method of treatment has no bearing with the development of PPC and surgery-related complications were less in those who were treated non-operatively [29].
Table 1.
Incidence of PPC in SH I & II injuries in various published series
| Series | Total number of cases (SH I&II) | Incidence of PPC | Treatment details | Incidence of PPC |
|---|---|---|---|---|
| Cai et al. (2015) | 286 (195) | 16.4% | Non-op/CR (70) | 24/147 (31.2%) |
| CRIF (77) | ||||
| ORIF | 8/48 (16.6%) | |||
| Russo et al. (2013) | 96 (96) | 42.7% | CR | 34% |
| OR | 51% | |||
| Seel et al. (2011) | 225 (131) | 14% | Not available | Not available |
| Leary et al. (2009) | 124 (44) | 22.7% | Not available | Not available |
| Rohimiller et al. (2006) | 91 (91) | 39.6% | Non-op | 29% |
| CR | 50% | |||
| CRIF | 36% | |||
| ORIF | 41% | |||
| Barmada et al. (2003) | 92 (44) | 36% | NR/CR | 11/26 (42.3%) |
| CRPP | 3/9 (33.3%) | |||
| ORIF | 3/9 (33.3%) |
The aim of treatment in SH II injuries would be to achieve anatomical reduction which could be either by closed or open methods. We would like to recommend closed reduction and above knee casting for all displaced SH Type II injuries. Surgical stabilization is indicated if the reduction is unstable. Open reduction is needed in all the patients in whom closed reduction could not be achieved. Irrespective of the method of treatment, it is important to counsel that about 40% of them would have PPC and need further surgical procedures.
Salter–Harris Type III & IV Fractures
These are intra-articular fractures and each constitutes about 25% of all the paediatric ankle fractures. They are commonly seen in children younger than 12 years of age. Undisplaced fractures can be treated non-operatively with a below-knee cast and repeat X-rays at 1 week to look for displacement. For fractures with more than 2 mm displacement and articular step-off the recommendation is the open anatomical reduction and internal fixation. Some series have reported a significantly low incidence of PPC in those patients treated with surgical stabilization compared to this treated non-operatively [25, 31]. In our experience, assisted reduction and percutaneous screw fixation along with arthrogram to confirm the articular congruity is an acceptable option with equally good outcomes (Fig. 6). The measurement of displacement on plain radiographs could be ambiguous and what seems to be an undisplaced fracture on X-rays could have more than 2 mm displacement on the CT Scan. However, getting a routine CT scan for all the children with SH type III & IV fractures might be an overkill considering the age and the amount of radiation. Hence, our recommendation for these fractures is surgical stabilization with compression screws even if they are undisplaced, with an aim to minimize physeal bar formation. In type III fractures, the screw should be intra-epiphyseal without crossing the physis and in type IV fractures an additional metaphyseal screw can be placed if the metaphyseal fragment is big enough.
Fig. 6.

a, b AP & lateral X-rays of the ankle joint showing a SH Type IV injury of the distal tibia in a 10 yr old boy; c, d AP & Mortise views of the intra-operative C –arm images following closed reduction, fixation and arthrogram showing good reduction and articular congruity; e, f AP & Lateral X-rays done at 6 weeks follow-up showing good healing of the fracture
Salter–Harris Type VII Injuries
Ankle joint is one of the common areas to get this pure intra-epiphyseal type of fractures in form of medial or lateral malleolar avulsions. Displaced medial malleolus fractures (SH VII) will need open reduction and fixation with a tension band construct using delayed absorbable suture materials instead of the SS wire (Fig. 7). The SH type VII injuries of the distal fibula can mimic a symptomatic os subfibulare and can be differentiated by classical radiographic findings. In a type VII injury, the fracture line is located in the middle of the fibular epiphysis and has irregular edges compared to a more distal location and smooth edges in os subfibulare [32]. SH type VII injuries of the fibula are managed with a walking cast for a period of four weeks.
Fig. 7.
a, b AP & lateral X-rays of the ankle joint showing a SH Type VII injury of the medial malleolus in a 9 yr old girl; c, d AP & lateral radiographs at 8 weeks follow-up after open reduction and tension band wiring for medial malleolus showing good union; e, f AP & lateral radiographs after implant exit at 7 months with no evidence of growth arrest
Transitional Fractures
The fractures of the ankle happening during the transition from a child to adult (closure of physis) are termed as transitional fractures. Titze and Ehalt first introduced this term in 1961 [33]. Transitional fractures occur due to the asymmetric closure of the distal tibial physis, which is usually complete by the age of 14 in girls and 16 in boys. The closure begins around Poland’s hump also called as the Kump’s bump, progresses antero-medially, postero-laterally and finally antero-laterally. Tillaux fracture and Triplane fractures are the transitional fractures and the management of these are discussed separately as they form a special group of fractures pertaining to this region. Tillaux fractures involve the tibial plafond and hence are always intra-articular. On the contrary, triplane fractures can be either intra-articular or completely extra-articular [34, 35]. The most common mechanism of injury is supination and external rotation, which otherwise would cause a SH-I or II fracture when the physis is completely open.
Tillaux Fracture
An isolated fracture of the anterolateral distal tibial epiphysis is called juvenile Tillaux fracture and is always a SH-III fracture. This is also called as a ‘biplane fracture’ by some authors as the fracture line runs in two different planes [33] (Fig. 8a). This fracture is the adolescent counterpart of the fracture in adults described by the French surgeon Paul Tillaux in 1982. It occurs between 12 and 15 years of age and represents 2.9% of the epiphyseal injuries in juveniles. During supination and external rotation of the foot, the anterior-inferior tibiofibular ligament avulses from its attachment with a bony fragment corresponding to the open portion of the distal tibial physis. This is also attributed to the stronger ligaments than the bone at this age. The fibula usually prevents marked displacement of the fragment and clinical deformity is generally absent. Swelling is usually slight, and tenderness is localised to the antero-lateral joint line, in contrast to ankle sprains where the tenderness tends to be below the level of the ankle joint.
Fig. 8.
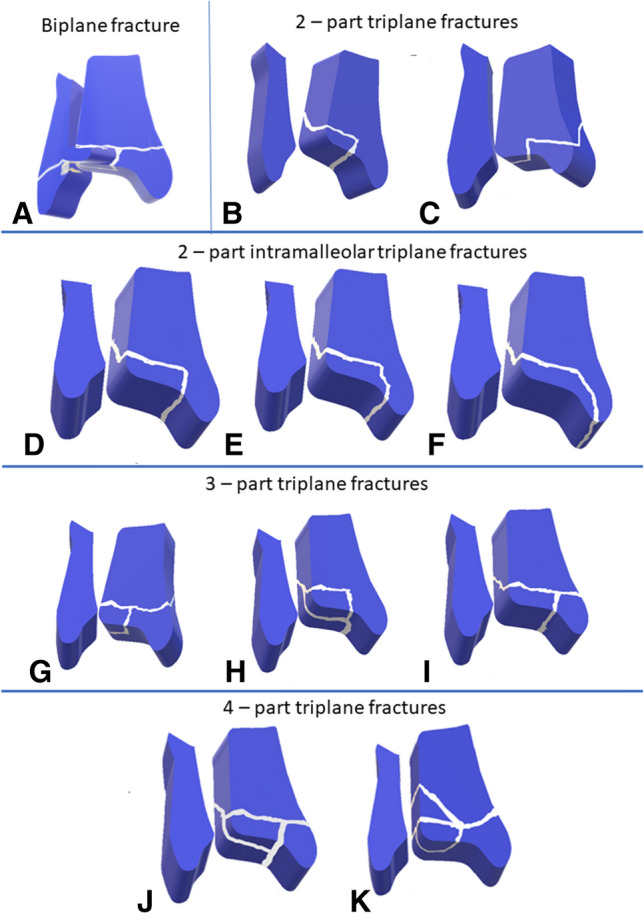
a Tillaux fracture also called as Kleiger fracture is a biplane fracture in which the fracture line passes in two planes; b the Cooperman fracture [43] is a two-part triplane fracture with medial malleolus attached to the tibial shaft and Thurston-Holland fragment attached to the Tillaux fragment; c the Denton fracture or the medial triplane fracture [44] is a two-part triplane fracture in which the medial malleolus attached to the Thurston-Holland fragment; d–f Intra-malleolar triplane fractures as described by Shin et al. [35]; d Intra-malleolar triplane fracture with fracture line exiting the junction of tibial plafond and medial malleolus; e Intra-malleolar triplane fracture with fracture line exiting in the articular portion of medial malleolus; f Extra-articular type of Intra-malleolar triplane fracture; g three-part triplane fracture with medial malleolus attached to Thurston–Holland fragment and Tillaux fragment is separate; h three-part triplane fracture with medial malleolus attached to the tibial shaft and separate Thurston–Holland and Tillaux fragments; i three-part triplane fracture with separate medial malleolar fragment and Thurston–Holland fragment is attached to the Tillaux fragment; j four-part triplane fracture with separate medial malleolus, Thurston–Holland and Tillaux fragments detached from the tibial shaft; k four-part triplane fracture with a double metaphyseal spike as described by van Laarhoven [45]
An ankle AP radiograph may miss the fracture and a mortise view is essential to see the distal tibial epiphysis unobstructed by the fibula. CT scan is needed to assess the intraarticular step and displacement to decide on the appropriate management [36].
Nondisplaced fractures and fractures with displacement less than 2 mm can be treated conservatively with below-knee plaster for 4 weeks. For fractures with displacement more than 2 mm on radiographs or CT scan, closed or open reduction and internal fixation is recommended [37, 38]. Closed reduction is attempted by internally rotating the foot and applying direct pressure over the anterolateral tibia. Occasionally, percutaneously inserted pins can be used to manipulate the displaced fragment into anatomical position and then advanced to fix the fragment in place. A cancellous screw placed within the epiphysis is usually the preferred method of fixation. The direction of the screw should be oblique, from lateral to medial and anterior to posterior to achieve good compression at the fracture site. Non-weight bearing for a period of 4 weeks post-fixation followed by gradual weight bearing is the recommended post-operative protocol. The outcomes of surgical fixation are very good and there is no risk of growth arrest as the child is usually closer to skeletal maturity [39–41].
Triplane Fractures
This fracture was first described by Marmor in 1970 and later Lynn coined the term triplane fracture in 1972 [42]. This fracture is hence named as ‘Marmor-Lynn’ fracture. Marmor described the fracture as consisting of three major fragments: (1) the anterolateral part of the distal tibial epiphysis, (2) the remaining medial and posterior portions of the epiphysis with an attached posterior metaphyseal fragment and (3) the tibial metaphysis. Triplane fractures represent 5–10% of pediatric intraarticular ankle fractures [42]. Approximately 50% of the triplane fractures can have associated fibular fracture.
The triplanar geometric configuration is formed by fracture line in the coronal plane through the posterior metaphysis, in the sagittal plane through the epiphysis, and in the transverse plane through the physis. Cooperman et al. reported that the two-part configuration is the most common and recommended that a CT scan is needed to evaluate these fractures [43]. In the two-part fracture, the lateral type is common in which the coronal fragment is posterolateral and a rare medial type with a posteromedial coronal fragment is also reported by Denton and Fischer (Fig. 8b, c) [44]. Von Laer described two types of triplane fractures with many sub-types in each. Essentially Type I triplane fractures are two-part fractures and Type II triplane fractures are three-part fractures [33]. Shin et al. described three different types of intra-malleolar two-part triplane fractures including one completely extra-articular variant (Fig. 8d–f) [35]. Van Laarhoven et al. described a classification with eight configurations which included a rare four-part triplane fracture with a double metaphyseal spike (Fig. 8k) [45]. Rapariz et al. presented a similar classification with six different types which included three different types of three-part fractures and one four-part fracture (Fig. 8g–j) [46]. These classification systems have poor inter-observer reliability and hence not used commonly in day-to-day clinical practice [16].
Though there is controversy on the routine need of CT scans for evaluation of triplane injuries [14–16, 47], we feel that CT scan is mandatory in these fractures both for quantifying the displacement as well as planning the screws which primarily depends on the number and location of fragments (Fig. 9). The primary aims of treatment are to restore congruency of ankle joint, with no step or gap and achieve stable fragment fixation for early mobilization.
Fig. 9.
a, b, c AP, mortise and lateral views of the ankle in a 14-year-old boy showing an undisplaced triplane fracture (3-part); d, e, f coronal, sagittal and axial CT sections of the same patient showing a three-part triplane fracture with intra-articular displacement > 5 mm; g, h AP & lateral views of the C-arm images after closed reduction and percutaneous screw fixation showing good reduction of the fracture; i, j AP & Lateral X-rays done at 6 weeks follow-up showing good healing of the fracture, k, l AP & Lateral X-rays done at 18 months follow-up shows completion of physeal closure without any growth arrest or deformity
We recommend that the following factors should be elucidated in the assessment of triplane fractures rather than focusing on the classification:
Whether the fracture is Intra-articular or extra-articular?
What is the articular step-off/displacement in intra-articular fractures?
Both of these questions can be effectively answered with a CT scan rather than a plain radiograph and hence our practice is to routinely get CT scan in all triplane fractures.
The extra-articular type of triplane fractures are amenable for non-operative treatment and does not need perfect anatomical reduction [33, 34, 37].
All undisplaced fractures (< 2 mm displacement on CT scan) can be treated non-operatively in a long leg cast followed by a repeat X-ray after a week to look for displacement. Weinberg in 2005 reported the rate of loss of reduction following conservative treatment to be less than 10% and concluded that surgical fixation would not be needed in all the cases [48].
All fractures with articular displacement > 2 mm are considered as displaced fractures and warrants perfect anatomical reduction and fixation [37, 40, 49]. Ertl et al. in their series had reported poor functional outcomes in the long-term when the residual gap was more than 2 mm. The importance of 2 mm cut-off was re-emphasized in the recent publication by Lurie et al. in which they showed significantly worse outcome in patients who had > 2.5 mm fracture gap in the CT scan and treated non-operatively [40]. The need for open reduction should be judiciously decided on a case-to-case basis considering the fact that experience and surgical expertise of the operating surgeon plays a significant role in achieving a closed reduction or assisted closed reduction. Use of percutaneous K wires and Steinmann pins as joysticks comes in handy for achieving assisted reduction of the displaced fragments [39]. Excellent outcomes have been reported with both open reduction and closed reduction and percutaneous fixation [39, 49, 50]. We personally prefer assisted reduction and percutaneous screw fixation with an intra-operative arthrogram whenever feasible. We have a low threshold for open reduction especially when the articular reduction is dubious or not perfect.
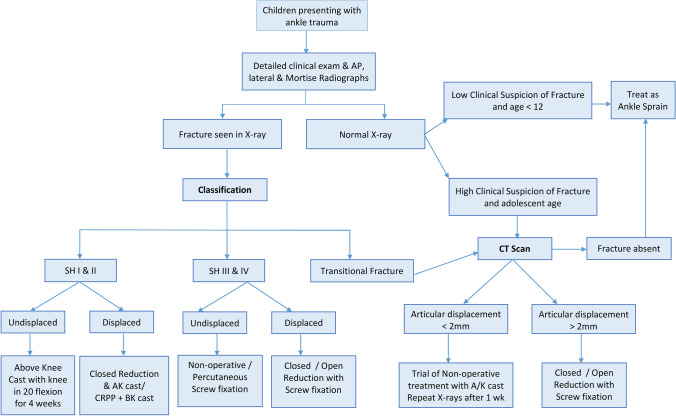
We present a simple algorithm for guiding treatment in children presenting with ankle fractures, based on the existing evidence and our clinical experience (Fig. 10). This algorithm may not include a certain rare form of injuries; however, the principles of treatment remains the same. The type of treatment is essentially decided by whether the fracture is intra or extra-articular and the amount of displacement of the fragments.
Fig. 10.
Treatment algorithm for children presenting with ankle trauma
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard statement
This article does not contain any studies with human or animal subjects performed by any of the authors.
Informed Consent
For this type of study informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
K. Venkatadass, Email: venkatpedortho@gmail.com
G. Sangeet, Email: drsangeetgangadharan@gmail.com
V. Durga Prasad, Email: durga.valleri@gmail.com.
S. Rajasekaran, Email: sr@gangahospital.com
References
- 1.Bible JE, Smith BG. Ankle fractures in children and adolescents. Techniques in Orthopaedics. 2009;24(3):211–219. [Google Scholar]
- 2.Su AW, Larson AN. Pediatric ankle fractures. Foot and Ankle Clinics. 2015;20(4):705–719. doi: 10.1016/j.fcl.2015.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wuerz TH, Gurd DP. Pediatric physeal ankle fracture. Journal of American Academy of Orthopaedic Surgeons. 2013;21(4):234–244. doi: 10.5435/JAAOS-21-04-234. [DOI] [PubMed] [Google Scholar]
- 4.Ogden JA. Injury to the growth mechanisms of the immature skeleton. Skeletal Radiology. 1981;6(4):237–253. doi: 10.1007/BF00347197. [DOI] [PubMed] [Google Scholar]
- 5.Cox G, Thambapillay S, Templeton PA. Compartment syndrome with an isolated Salter Harris II fracture of the distal tibia. Journal of Orthopaedic Trauma. 2008;22(2):148–150. doi: 10.1097/BOT.0b013e31815c11c6. [DOI] [PubMed] [Google Scholar]
- 6.Yeap JS, Fazir M, Ezlan S, Kareem BA, Harwant S. Compartment syndrome of the calf and foot following a displaced Salter–Harris type II fracture of the distal tibia: a review of the literature and a case report. Medical Journal of Malaysia. 2001;56(C):66–69. [PubMed] [Google Scholar]
- 7.Haumont T, Gauchard GC, Zabee L, Arnoux J-M, Journeau P, Lascombes P. Extensor retinaculum syndrome after distal tibial fractures: anatomical basis. Surgical and Radiologic Anatomy. 2007;29(4):303–311. doi: 10.1007/s00276-007-0215-3. [DOI] [PubMed] [Google Scholar]
- 8.Mubarak SJ. Extensor retinaculum syndrome of the ankle after injury to the distal tibial physis. The Journal of Bone and Joint Surgery. British Volume. 2002;84(1):11–14. doi: 10.1302/0301-620x.84b1.11800. [DOI] [PubMed] [Google Scholar]
- 9.King J, Diefendorf D, Apthorp J, Negrete VF, Carlson M. Analysis of 429 fractures in 189 battered children. Journal of Pediatric Orthopedics. 1988;8(5):585–589. [PubMed] [Google Scholar]
- 10.Stiell IG, Greenberg GH, McKnight RD, Nair RC, McDowell I, Worthington JR. A study to develop clinical decision rules for the use of radiography in acute ankle injuries. Annals of Emergency Medicine. 1992;21(4):384–390. doi: 10.1016/s0196-0644(05)82656-3. [DOI] [PubMed] [Google Scholar]
- 11.Letts RM. The hidden adolescent ankle fracture. Journal of Pediatric Orthopedics. 1982;2(2):161–164. doi: 10.1097/01241398-198202020-00007. [DOI] [PubMed] [Google Scholar]
- 12.Sung KH, Kwon S-S, Moon SJ, Lee SY. Radiographic evaluation of the normal ankle joint in children and adolescent. The Journal of Orthopaedic Science. 2018;23(4):658–664. doi: 10.1016/j.jos.2018.03.003. [DOI] [PubMed] [Google Scholar]
- 13.Bozic KJ, Jaramillo D, DiCanzio J, Zurakowski D, Kasser JR. Radiographic appearance of the normal distal tibiofibular syndesmosis in children. Journal of Pediatric Orthopedics. 1999;19(1):14–21. [PubMed] [Google Scholar]
- 14.Liporace FA, Yoon RS, Kubiak EN, Parisi DM, Koval KJ, Feldman DS, et al. Does adding computed tomography change the diagnosis and treatment of Tillaux and triplane pediatric ankle fractures? Orthopedics. 2012;35(2):e208–212. doi: 10.3928/01477447-20120123-11. [DOI] [PubMed] [Google Scholar]
- 15.Schneidmueller D, Sander AL, Wertenbroek M, Wutzler S, Kraus R, Marzi I, et al. Triplane fractures: do we need cross-sectional imaging? European Journal of Trauma and Emergency Surgery. 2014;40(1):37–43. doi: 10.1007/s00068-013-0338-7. [DOI] [PubMed] [Google Scholar]
- 16.Eismann EA, Stephan ZA, Mehlman CT, Denning J, Mehlman T, Parikh SN, et al. Pediatric triplane ankle fractures: impact of radiographs and computed tomography on fracture classification and treatment planning. Journal of Bone and Joint Surgery: American Volume. 2015;97(12):995–1002. doi: 10.2106/JBJS.N.01208. [DOI] [PubMed] [Google Scholar]
- 17.Brown SD, Kasser JR, Zurakowski D, Jaramillo D. Analysis of 51 tibial triplane fractures using CT with multiplanar reconstruction. American Journal of Roentgenology. 2004;183(5):1489–1495. doi: 10.2214/ajr.183.5.1831489. [DOI] [PubMed] [Google Scholar]
- 18.Boutis K, Narayanan UG, Dong FFT, Mackenzie H, Yan H, Chew D, et al. Magnetic resonance imaging of clinically suspected Salter–Harris I fracture of the distal fibula. Injury. 2010;41(8):852–856. doi: 10.1016/j.injury.2010.04.015. [DOI] [PubMed] [Google Scholar]
- 19.Boutis K, Plint A, Stimec J, Miller E, Babyn P, Schuh S, et al. Radiograph-negative lateral ankle injuries in children: occult growth plate fracture or sprain? JAMA Pediatrics. 2016;170(1):e154114. doi: 10.1001/jamapediatrics.2015.4114. [DOI] [PubMed] [Google Scholar]
- 20.Barmada A, Gaynor T, Mubarak SJ. Premature physeal closure following distal tibia physeal fractures. Journal of Pediatric Orthopedics. 2003;23(6):7. doi: 10.1097/00004694-200311000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Leary JT, Handling M, Talerico M, Yong L, Bowe JA. Physeal fractures of the distal tibia: predictive factors of premature physeal closure and growth arrest. Journal of Pediatric Orthopedics. 2009;29(4):356–361. doi: 10.1097/BPO.0b013e3181a6bfe8. [DOI] [PubMed] [Google Scholar]
- 22.Spiegel PG, Cooperman DR, Laros GS. Epiphyseal fractures of the distal ends of the tibia and fibula. A retrospective study of two hundred and thirty-seven cases in children. Journal of Bone and Joint Surgery: American Volume. 1978;60(8):1046–1050. [PubMed] [Google Scholar]
- 23.Blackburn EW, Aronsson DD, Rubright JH, Lisle JW. Ankle fractures in children. Journal of Bone and Joint Surgery. 2012;94(13):1234–1244. doi: 10.2106/JBJS.K.00682. [DOI] [PubMed] [Google Scholar]
- 24.Schurz M, Binder H, Platzer P, Schulz M, Hajdu S, Vécsei V. Physeal injuries of the distal tibia: long-term results in 376 patients. International Orthopaedics. 2010;34(4):547–552. doi: 10.1007/s00264-009-0851-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cai H, Wang Z, Cai H. Surgical indications for distal tibial epiphyseal fractures in children. Orthopedics. 2015;38(3):e189–195. doi: 10.3928/01477447-20150305-55. [DOI] [PubMed] [Google Scholar]
- 26.Rohmiller MT, Gaynor TP, Pawelek J, Mubarak SJ. Salter–Harris I and II fractures of the distal tibia: does mechanism of injury relate to premature physeal closure? Journal of Pediatric Orthopedics. 2006;26(3):7. doi: 10.1097/01.bpo.0000217714.80233.0b. [DOI] [PubMed] [Google Scholar]
- 27.Russo F, Moor MA, Mubarak SJ, Pennock AT. Salter–Harris II fractures of the distal tibia: does surgical management reduce the risk of premature physeal closure? Journal of Pediatric Orthopedics. 2013;33(5):6. doi: 10.1097/BPO.0b013e3182880279. [DOI] [PubMed] [Google Scholar]
- 28.Phan VC, Wroten E, Yngve DA. Foot progression angle after distal tibial physeal fractures. Journal of Pediatric Orthopedics. 2002;22(1):31–35. [PubMed] [Google Scholar]
- 29.Asad WA, Younis MHS, Ahmed AF, Ibrahim T. Open versus closed treatment of distal tibia physeal fractures: a systematic review and meta-analysis. European Journal of Orthopaedic Surgery and Traumatology. 2018;28(3):503–509. doi: 10.1007/s00590-017-2062-1. [DOI] [PubMed] [Google Scholar]
- 30.Seel EH, Noble S, Clarke NMP, Uglow MG. Outcome of distal tibial physeal injuries. Journal of Pediatric Orthopaedics Part B. 2011;20(4):242–248. doi: 10.1097/BPB.0b013e3283467202. [DOI] [PubMed] [Google Scholar]
- 31.Kling TF, Bright RW, Hensinger RN. Distal tibial physeal fractures in children that may require open reduction. Journal of Bone and Joint Surgery. American Volume. 1984;66(5):647–657. [PubMed] [Google Scholar]
- 32.Sugi MT, Tileston K, Krygier JE, Gamble J. Transepiphyseal (Type VII) ankle fracture versus os subfibulare in pediatric ankle injuries. Journal of Pediatric Orthopedics. 2018;38(10):4. doi: 10.1097/BPO.0000000000001246. [DOI] [PubMed] [Google Scholar]
- 33.von Laer L. Classification, diagnosis, and treatment of transitional fractures of the distal part of the tibia. Journal of Bone and Joint Surgery. American Volume. 1985;67(5):687–698. [PubMed] [Google Scholar]
- 34.Feldman DS, Otsuka NY, Hedden DM. Extra-articular triplane fracture of the distal tibial epiphysis. Journal of Pediatric Orthopedics. 1995;15(4):479–481. doi: 10.1097/01241398-199507000-00014. [DOI] [PubMed] [Google Scholar]
- 35.Shin AY, Moran ME, Wenger DR. Intramalleolar triplane fractures of the distal tibial epiphysis. Journal of Pediatric Orthopedics. 1997;17(3):352–355. [PubMed] [Google Scholar]
- 36.Horn BD, Crisci K, Krug M, Pizzutillo PD, MacEwen GD. Radiologic evaluation of juvenile tillaux fractures of the distal tibia. Journal of Pediatric Orthopedics. 2001;21(2):162–164. [PubMed] [Google Scholar]
- 37.Crawford AH. Triplane and Tillaux fractures: is a 2 mm residual gap acceptable? Journal of Pediatric Orthopedics. 2012;32(1):S69–73. doi: 10.1097/BPO.0b013e31824b25a1. [DOI] [PubMed] [Google Scholar]
- 38.Tiefenboeck TM, Binder H, Joestl J, Tiefenboeck MM, Boesmueller S, Krestan C, et al. Displaced juvenile tillaux fractures: surgical treatment and outcome. Wiener Klinische Wochenschrift. 2017;129(5–6):169–175. doi: 10.1007/s00508-016-1059-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Choudhry IK, Wall EJ, Eismann EA, Crawford AH, Wilson L. Functional outcome analysis of triplane and tillaux fractures after closed reduction and percutaneous fixation. Journal of Pediatric Orthopedics. 2014;34(2):139–143. doi: 10.1097/BPO.0000000000000085. [DOI] [PubMed] [Google Scholar]
- 40.Lurie B, Van Rysselberghe N, Pennock AT, Upasani VV. Functional outcomes of tillaux and triplane fractures with 2 to 5 millimeters of intra-articular gap. Journal of Bone and Joint Surgery. 2020;102(8):679–686. doi: 10.2106/JBJS.19.01170. [DOI] [PubMed] [Google Scholar]
- 41.Kaya A, Altay T, Ozturk H, Karapinar L. Open reduction and internal fixation in displaced juvenile tillaux fractures. Injury. 2007;38(2):201–205. doi: 10.1016/j.injury.2006.07.033. [DOI] [PubMed] [Google Scholar]
- 42.Schnetzler KA, Hoernschemeyer D. The pediatric triplane ankle fracture. Journal of American Academy of Orthopaedic Surgeons. 2007;15(12):738–747. doi: 10.5435/00124635-200712000-00007. [DOI] [PubMed] [Google Scholar]
- 43.Cooperman DR, Spiegel PG, Laros GS. Tibial fractures involving the ankle in children. The so-called triplane epiphyseal fracture. Journal of Bone and Joint Surgery. American Volume. 1978;60(8):1040–1046. [PubMed] [Google Scholar]
- 44.Denton JR, Fischer SJ. The medial triplane fracture: report of an unusual injury. Journal of Trauma. 1981;21(11):991–995. [PubMed] [Google Scholar]
- 45.van Laarhoven CJ, Severijnen RS, van der Werken C. Triplane fractures of the distal tibia. The Journal of Foot and Ankle Surgery. 1995;34(6):556–559. doi: 10.1016/S1067-2516(09)80077-X. [DOI] [PubMed] [Google Scholar]
- 46.Rapariz JM, Ocete G, González-Herranz P, López-Mondejar JA, Domenech J, Burgos J, et al. Distal tibial triplane fractures: long-term follow-up. Journal of Pediatric Orthopedics. 1996;16(1):113–118. doi: 10.1097/00004694-199601000-00023. [DOI] [PubMed] [Google Scholar]
- 47.Nenopoulos A, Beslikas T, Gigis I, Sayegh F, Christoforidis I, Hatzokos I. The role of CT in diagnosis and treatment of distal tibial fractures with intra-articular involvement in children. Injury. 2015;46(11):2177–2180. doi: 10.1016/j.injury.2015.07.017. [DOI] [PubMed] [Google Scholar]
- 48.Weinberg AM, Jablonski M, Castellani C, Koske C, Mayr J, Kasten P. Transitional fractures of the distal tibia. Injury. 2005;36(11):1371–1378. doi: 10.1016/j.injury.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 49.Kim JR, Song KH, Song KJ, Lee HS. Treatment outcomes of triplane and Tillaux fractures of the ankle in adolescence. Clinics in Orthopedic Surgery. 2010;2(1):34–38. doi: 10.4055/cios.2010.2.1.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zelenty W, Yoon RS, Shabtai L, Choi P, Martin B, Horn D, et al. Percutaneous versus open reduction and fixation for Tillaux and triplane fractures: a multicenter cohort comparison study. Journal of Pediatric Orthopaedics Part B. 2018;27(6):551–555. doi: 10.1097/BPB.0000000000000522. [DOI] [PubMed] [Google Scholar]