Abstract
Background
As America’s third highest opioid prescribers, orthopedic surgeons have contributed to the opioid abuse crisis. This study evaluated opioid use after primary total joint replacement. We hypothesized that patients who underwent total hip arthroplasty (THA) use fewer opioids than patients who underwent total knee arthroplasty (TKA) and that both groups use fewer opioids than prescribed.
Methods
A prospective study of 110 patients undergoing primary THA or TKA by surgeons at an academic center during 2018 was performed. All were prescribed oxycodone 5 mg, 84 tablets, without refills. Demographics, medical history, and operative details were collected. Pain medication consumption and patient-reported outcomes were collected at 2 and 6 weeks postoperatively. Analysis of variance was performed on patient and surgical variables.
Results
Sixty-one patients scheduled for THA and 49 for TKA were included. THA patients consumed significantly fewer opioids than TKA patients at 2 weeks (28.1 tablets vs 48.4, P = .0003) and 6 weeks (33.1 vs 59.3, P = .0004). Linear regression showed opioid use decreased with age at both time points (P = .0002). A preoperative mental health disorder was associated with higher usage at 2 weeks (58.3 vs 31.4, P < .0001) and 6 weeks (64.7 vs 39.2, P = .006). Higher consumption at 2 weeks was correlated with worse outcome scores at all time points.
Conclusions
TKA patients required more pain medication than THA patients, and both groups received more opioids than necessary. In addition, younger patients and those with a preexisting mental health disorder required more pain medication. These data provide guidance on prescribing pain medication to help limit excess opioid distribution.
Keywords: Total joint arthroplasty, Opioid, Prescribing
Introduction
Total hip and knee arthroplasties are common surgeries in orthopedics with more than 300,000 hip replacements and 600,000 knee replacements performed each year in the United States [1]. Proper postoperative pain control leads to improved function, outcome measures, and patient satisfaction with lower hospital costs [[2], [3], [4], [5], [6], [7], [8]]. Inadequate pain control after total joint replacement has been associated with poor results including increased health-care costs, development of chronic pain, and worse functional outcomes [9,10].
In the United States, opioids have been a cornerstone of pain control, but they come with significant side effects and risks. Recent studies have shown that nearly all patients receive more pain medication than they require after elective surgery [[11], [12], [13]] placing excess opioid medication in circulation in households and communities, thereby increasing the potential for abuse and diversion. Consequently, opioid prescribing guidelines have become an increasingly important topic in orthopedic research. It seems logical that the amount of pain medication required on average depends on the type of surgery as well as both patient and surgical characteristics. The goal of this study was to quantify the average amount of pain medication consumed after discharge after total hip arthroplasty (THA) and total knee arthroplasty (TKA), to compare usage between postoperative THA and TKA, and to identify relationships between patient characteristics, postoperative outcome measures, and actual opioid consumption. We hypothesized that total hip replacement patients would consume fewer tablets than total knee replacement patients and that, overall, we prescribe more tablets than necessary for most patients.
Material and methods
After obtaining institutional review board approval, patients scheduled for THA or TKA at an academic hospital consented for this study. Inclusion criteria included patient age of 18 years or older scheduled for primary THA or TKA from one of 5 fellowship-trained surgeons during the year 2018. Exclusion criteria included prior replacement to the operative joint or patients under a pain contract with a chronic pain management physician. Preoperative surveys were conducted to collect comorbidities, medication use, education level, insurance status, Hip disability and Osteoarthritis Outcome Score (HOOS), Knee disability and Osteoarthritis Outcome Score (KOOS), and Global Physical and Mental Score. HOOS and KOOS are patient-reported numeric surveys with sections that assess function, pain, and its impact on quality of life and activities of daily living. The Global Physical and Mental Health scores are sections of the Patient-Reported Outcomes Measurement and Information System, also patient-reported scores that assess overall physical and mental health. Intraoperative records were reviewed to record blood loss, tourniquet time, approach used for THA, and type of TKA implant (cruciate retaining or posterior stabilized). In addition to standard postoperative rehabilitation protocols, all patients were given a single prescription for oxycodone 5 mg totaling 84 tablets, a 1-week supply if 2 tablets were taken every 4 hours. Our practice has been not to provide refills, shifting the burden of monitoring opioid consumption to the patient. We chose 84 tablets based on our anecdotal experience and the fact that most of our patients live hours away. If needed, the only way to provide refills was to provide patients with a paper prescription (State laws prevented e-prescribing or phoned-in opioid prescribing at the time this study was conducted.). All patients received a 30 day prescription for either celecoxib or meloxicam. Patients were permitted to supplement with acetaminophen as needed. At the 2- and 6-week postoperative follow-up visits, patients were surveyed for HOOS, KOOS, and Global Mental and Physical Scores and asked to provide the number of tablets remaining from their oxycodone prescription based on their own record keeping.
Continuous variables were reported using mean and standard deviation and analyzed using regression analysis. Pill consumption was compared between groups using independent Student t-tests or one-way analysis of variance. One-way analysis of variance was used to evaluate for significant differences in opioid consumption based on demographic and surgical characteristics. Statistical analysis was conducted using the program JMP 14.1 (SAS Institute Inc., Cary, NC). A P value of 0.05 or less was considered statistically significant.
Results
Sixty-one patients scheduled for THA and 49 for TKA participated in the study. Overall mean age was 64.8 ± 10.7 years (range, 35.5-84.0). Sixty (54.5%) of the 110 patients were female. The demographic breakdown of each operative group can be found in Table 1. Eight patients (7.3%) did not fill their opioid prescription, 5 in the THA group, and 3 in the TKA group. One of these 8 patients was on opioids preoperatively. At the 2-week follow-up, THA patients had consumed 28.1 tablets while TKA patients consumed 48.4 tablets, a statistically significant difference (P = .0003). By 6 weeks, THA patients consumed a mean of 33.1 tablets, significantly fewer than the 59.3 tablets TKA patients consumed (P = .0004). These differences are summarized in Table 2. At 2 weeks, THA patients had a pain level of 2.2 on a 0-10 scale, while TKA patients had a pain level of 3.6 (P = .001). At 6 weeks, THA patients had pain level of 1.2, while TKA patients had pain scores of 2.7 (P < .0001). Presence of preoperative opioid, NSAID, benzodiazepine, or anticonvulsant medications had no correlation with postoperative opioid consumption amounts. However, NSAID use in the first 6 weeks after surgery did correlate with higher consumption of opioid during that time. Insurance status, education level, surgeon, approach for THA (P values of 0.44 at 2 weeks and 0.801 at 6 weeks), tourniquet time, and type of TKA implant (P values of 0.404 at 2 weeks and 0.412 at 6 weeks) had no correlation with opioid consumption (Table 3).
Table 1.
Demographics of patients in the study.
| THA | TKA | Total | ||
|---|---|---|---|---|
| Age | Average | 63.3 | 66.8 | 64.8 |
| Range | 35.5-83.6 | 42.2-84.0 | 35.5-84.0 | |
| Gender | Male | 32 | 31 | 63 |
| Female | 29 | 18 | 47 | |
| Insurance | Medicaid | 6 | 4 | 10 |
| Medicare | 27 | 27 | 54 | |
| Private | 28 | 18 | 46 |
Table 2.
Number of pills used and pain score on a 0-10 scale at the 2- and 6-wk postoperative time points.
| THA | TKA | P value | Combined | |
|---|---|---|---|---|
| Pills used | ||||
| 2 wks | 28.1 | 48.4 | .0003 | 37.0 |
| 6 wks | 33.1 | 59.3 | .0004 | 43.6 |
| Pain score | ||||
| 2 wks | 2.2 | 3.6 | .001 | 2.8 |
| 6 wks | 1.2 | 2.7 | <.0001 | 1.9 |
Displayed for THA and TKA patients (with P value calculated using a Student t-test) along with average for all patients combined.
Table 3.
Breakdown of pill usage.
| Variable | Number of patients | Pills used at 2 wks | Pills used at 6 wks | |
|---|---|---|---|---|
| Hip approach | Direct anterior | 23 | 28.1 | 33.1 |
| Posterior | 38 | 28.1 | 31.9 | |
| Knee implant | CR knee | 18 | 48.4 | 59.3 |
| PS knee | 30 | 48.1 | 59.3 | |
| Insurance type | Medicaid | 10 | 36.3 | 43.0 |
| Medicare | 54 | 37.0 | 43.1 | |
| Private | 46 | 37.0 | 43.6 | |
| Gender | Female | 60 | 37.0 | 43.1 |
| Male | 50 | 37.0 | 43.6 | |
| Education level | College experience | 41 | 37.0 | 43.6 |
| High school graduate | 26 | 37.4 | 45.1 | |
| Less than high school | 5 | 59.0 | 73.2 | |
| Age | 70+ | 41 | 37.0 | 43.1 |
| 60-69 | 33 | 35.5 | 42.9 | |
| 50-59 | 28 | 37.0 | 43.6 | |
| <50 | 8 | 37.6 | 38.7 |
CR, cruciate retaining; PS, posterior stabilized.
Preoperative psychiatric diagnosis such as anxiety or depression was significantly associated with increased opioid consumption at all time points. At 2 weeks, patients with a psychiatric history had consumed 58.3 pills vs 31.4 pills (P < .0001). At 6 weeks, the difference was 64.7 vs 39.2 pills consumed (P = .006). In all patients, linear regression analysis showed the use of postoperative opioids decreased significantly with increasing age at 2 (Figure 1) and 6 weeks (P = .002 at both time points) (Figure 2).
Figure 1.
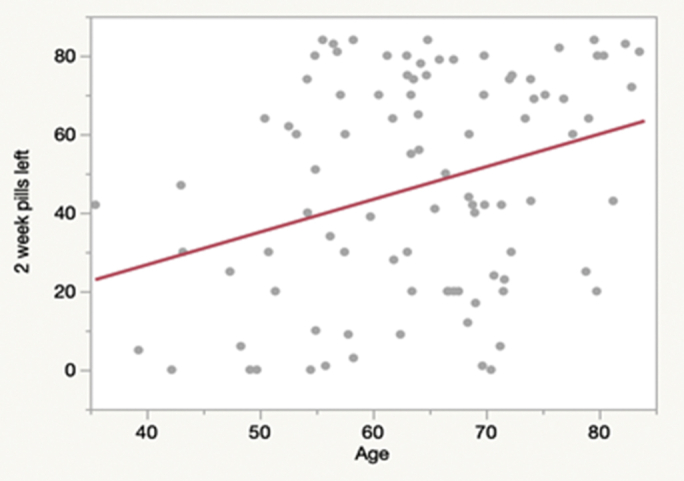
Bivariate fit of pills remaining by age at 2 wk.
Figure 2.
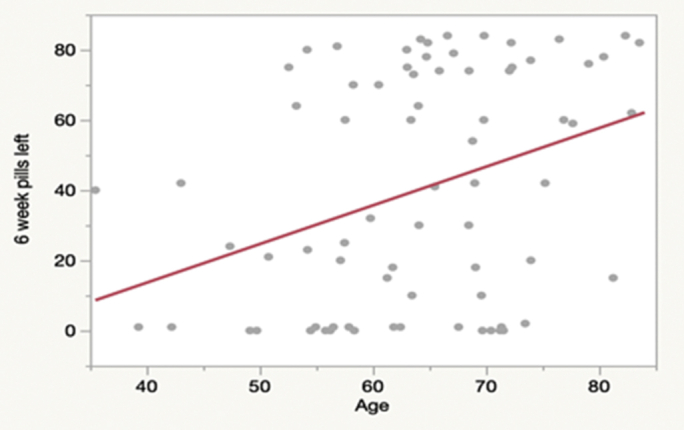
Bivariate fit of pills remaining by age at 6 wk.
Higher consumption in the first 2 weeks postoperatively was associated with worse HOOS Quality of Life (P = .044) and Global Physical Score (P = .0003) at 2 weeks and worse KOOS pain (P = .041), KOOS Activities of Daily Living (ADL) (P = .012), Global Physical Score (P = .001), and Global Mental Score (P = .022) at 6 weeks. Higher consumption at 6 weeks predicted worse HOOS ADL scores at 6 weeks (P = .045).
Discussion
The opioid epidemic has forced a closer look at prescribing habits so as not to contribute to the already escalating problem of addiction and diversion. Greater regulation of opioid prescribing and the logistical burden of getting a paper prescription refill into the hands of patients who live hours away saw a change in the way we prescribe. Patients instead have been given a single prescription of postoperative opioid and told it cannot be refilled, shifting the responsibility of tracking usage to the patient. Anecdotally, we had observed that some patients deplete their pain pills in less than 2 weeks while others did not fill the prescription at all. More commonly, we had observed that THA patients complained less of pain than TKA patients. The goal of this study was to identify if patients receiving a THA vs a TKA required different amounts of opioids postoperatively and to identify potential risk factors for higher opioid needs in the period following total joint replacement. Our hope was to be able to significantly reduce the amount of postoperative opioids issued to our total joint replacement patients, and to better understand the characteristics that contribute to higher pain levels and pain medication consumption in some patients than others.
We saw a significant difference between the 2 surgeries, with THA patients requiring 33.1 pills vs the 59.3 required by TKA patients in the first 2 weeks postoperatively. Numerous retrospective studies have shown similar results, with TKA patients being given more and using more pain medication in the postoperative period, as well as being more likely to develop chronic opioid use habits after surgery [[14], [15], [16], [17], [18]]. To our knowledge, this study is the first to directly compare the 2 procedures prospectively with a standardized opioid prescription protocol. The reason behind the difference in pain medication consumption is likely rooted in the painful rehabilitation that occurs after TKA, causing a need for more pain medication in the acute period after surgery.
Studies have identified numerous risk factors for increased opioid use postoperatively including tobacco and alcohol abuse, chronic pain, anxiety, depression, and benzodiazepine use [12,[17], [18], [19]]. While older age is often cited as a risk factor for chronic prescription opioid use in general, several studies have shown that young age in the acute postoperative period is a risk factor for increased opioid requirement after orthopedic surgeries [[20], [21], [22]]. Our study mirrored these results, with opioid use decreasing with increased age at all time points. The reasons are likely multifactorial. Older patients typically have lower demands in their daily lives, causing them to perform fewer painful activities in the postoperative period, prompting less opioid use. Also, opioid-type drugs in older patients have a lower volume of distribution than in younger patients, meaning it takes a smaller dose of drug to reach the same plasma concentration [23,24], thus allowing older patients to reach the same blood level of medication with fewer pills. It is well described that older patients are at greater risk of experiencing the negative effects of opioids, and this study supports a surgeon’s decision to prescribe fewer opioids to the elderly [24].
Of note, the authors recognized a noticeable difference in pill consumption between the education level “less than high school” and other education levels. As seen in Table 1, this group’s consumption at 2 and 6 weeks was 59 and 73.2 pills, respectively, over 20 pills more than all other education groups at both time points. These data were not statistically different, likely because of only 5 patients falling into this group, but we believe it is of note. In a study of over 14,000 patients, Ellis et al. [25] saw a correlation between lower education levels and opioid abuse treatment. While we are not suggesting that patients are abusing opioids, our data show a trend that is supported in current literature. Patients with lower education may be at higher risk of increased opioid use, a topic deserving of future research.
The unique outcome this study evaluated was patient-reported outcomes in the setting of opioid use. The most significant finding was in the relationship between pill consumption in the first 2 weeks and patient-reported outcome scores at the 2- and 6-week time points. After THA, higher opioid consumption in the first 2 weeks was associated with worse HOOS Quality of Life scores at the 2-week time point. After TKA, higher opioid consumption at 2 weeks was significantly correlated with lower KOOS Pain and Activities of Daily Living scores at 6 weeks. For all patients, higher consumption at 2 weeks was associated with worse Global Physical Scores and Global Mental Scores at the 6-week visit. These relationships illustrate a connection between acute postoperative pain, opioid use, and early patient outcomes. While the etiology of these relationships is unclear, surgeons should consider patients with greater opioid use in the first few weeks after surgery to be at higher risk for worse outcomes.
Overall, this study shows that the main risk factors for increased opioid use in our population are younger age, preoperative psychiatric diagnoses, higher pain scores after surgery, and TKA. Excluding postoperative pain scores, the remaining 3 factors are all known before surgery. These patients could be counseled that they are likely to experience more postoperative pain and greater opioid consumption, and surgeons can consider additional interventions to reduce pain and opioid use after surgery.
One limitation of this study is the short-term nature of the outcome measures. Patient-reported outcome scores were collected up to 6 weeks postoperatively, so we are unable to investigate the relationship of postoperative opioid consumption with long-term outcomes. Another limitation of the study is the way in which opioid use was tabulated relying solely on self-reported usage. We entrusted patients to log their own usage and did not manually count remaining tablets at their return visits. Also, this study was performed at an academic center in a rural state with a small population and with a greater prevalence of opioid abuse. Therefore, our patients’ postoperative opioid usage may be biased by knowledge of the perils of opioid use and abuse that are not generalizable to the public at large.
Conclusions
This study showed that TKA, younger age, and psychiatric diagnoses are all risk factors for increased postoperative opioid use. Since this study was undertaken, new state laws now permit sending opioid prescriptions electronically, thereby allowing us to prescribe fewer pain pills at discharge and issuing refills when the need is legitimate. Correctly estimating the amount a patient may require for their recovery at discharge remains advantageous as it reduces patient anxiety and administrative burden on staff. This study has changed our prescribing patterns as we now issue fewer pain pills to our THA patients than to our TKA patients. Furthermore, we ask patients how many pills they feel they will need at discharge as the vast majority are committed to minimizing their opioid use given the stigma and national attention paid to the opioid epidemic.
Conflict of Interests
B. A. Lindsey gave a lecture for Hanger Prosthetics, is a paid consultant for Zimmer-Biomet, obtained funding from Stryker, and is in the Research Committee for MSTS.
Acknowledgment
The authors would like to acknowledge Matthew Dietz, MD; Benjamin Frye, MD; and Timothy Murphy, MD, for contributing patients to this study. The authors would also like to acknowledge Gerald R. Hobbs, PhD, for conducting the statistical analysis.
Appendix A. Supplementary data
References
- 1.Singh J.A., Vessely M.B., Harmsen W.S. A population-based study of trends in the use of total hip and total knee arthroplasty, 1969-2008. Mayo Clin Proc. 2010;85(10):898. doi: 10.4065/mcp.2010.0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chelly J.E., Ben-David B., Williams B.A., Kentor M.L. Anesthesia and postoperative analgesia: outcomes following orthopedic surgery. Orthopedics. 2003;26(8 SUPPL):s865. doi: 10.3928/0147-7447-20030802-08. [DOI] [PubMed] [Google Scholar]
- 3.Postoperative pain management techniques in hip and knee arthroplasty. https://www.ncbi.nlm.nih.gov/pubmed/?term=19385585 [PubMed]
- 4.Cheville A., Chen A., Oster G., McGarry L., Narcessian E. A randomized trial of controlled-release oxycodone during inpatient rehabilitation following unilateral total knee arthroplasty. J Bone Joint Surg Am. 2001;83(4):572. doi: 10.2106/00004623-200104000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Peters C.L., Shirley B., Erickson J. The effect of a new multimodal perioperative anesthetic regimen on postoperative pain, side effects, rehabilitation, and length of hospital stay after total joint arthroplasty. J Arthroplasty. 2006;21(6 SUPPL):132. doi: 10.1016/j.arth.2006.04.017. [DOI] [PubMed] [Google Scholar]
- 6.Lamplot J.D., Wagner E.R., Manning D.W. Multimodal pain management in total knee arthroplasty. a prospective randomized controlled trial. J Arthroplasty. 2014;29(2):329. doi: 10.1016/j.arth.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 7.Tali M., Maaroos J. Lower limbs function and pain relationships after unilateral total knee arthroplasty. Int J Rehabil Res. 2010;33(3):264. doi: 10.1097/MRR.0b013e3283352126. [DOI] [PubMed] [Google Scholar]
- 8.Rathmell J.P., Pino C.A., Taylor R., Patrin T., Viani B.A. Intrathecal morphine for postoperative analgesia: a randomized, controlled, dose-ranging study after hip and knee arthroplasty. Anesth Analg. 2003;97(5):1452. doi: 10.1213/01.ANE.0000083374.44039.9E. [DOI] [PubMed] [Google Scholar]
- 9.Moucha C.S., Weiser M.C., Levin E.J. Current strategies in anesthesia and analgesia for total knee arthroplasty. J Am Acad Orthop Surg. 2016;24(2):60. doi: 10.5435/JAAOS-D-14-00259. [DOI] [PubMed] [Google Scholar]
- 10.Joshi G.P., Ogunnaike B.O. Consequences of inadequate postoperative pain relief and chronic persistent postoperative pain. Anesthesiol Clin North America. 2005;23(1):21. doi: 10.1016/j.atc.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 11.Feinberg A.E., Chesney T.R., Srikandarajah S., Acuna S.A., McLeod R.S. Opioid use after discharge in postoperative patients: a systematic review. Ann Surg. 2018;267(6):1056. doi: 10.1097/SLA.0000000000002591. [DOI] [PubMed] [Google Scholar]
- 12.Howard R., Fry B., Gunaseelan V. Association of opioid prescribing with opioid consumption after surgery in Michigan. JAMA Surg. 2019;154(1):e184234. doi: 10.1001/jamasurg.2018.4234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bicket M.C., White E., Pronovost P.J., Wu C.L., Yaster M., Alexander G.C. Opioid oversupply after joint and spine surgery: a prospective cohort study. Anesth Analg. 2019;128(2):358. doi: 10.1213/ANE.0000000000003364. [DOI] [PubMed] [Google Scholar]
- 14.Roberts K.C., Moser S.E., Collins A.C. Prescribing and consumption of opioids after primary, unilateral total hip and knee arthroplasty in opioid-naive patients. J Arthroplasty. 2020;35(4):960. doi: 10.1016/j.arth.2019.08.036. [DOI] [PubMed] [Google Scholar]
- 15.Goesling J., Moser S.E., Zaidi B. Trends and predictors of opioid use after total knee and total hip arthroplasty. Pain. 2016;157(6):1259. doi: 10.1097/j.pain.0000000000000516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Opioid prescriptions after total joint arthroplasty. https://www.ncbi.nlm.nih.gov/pubmed/30489249 [PubMed]
- 17.Dwyer M.K., Tumpowsky C.M., Hiltz N.L., Lee J.A., Healy W.L., Bedair H.S. Characterization of post-operative opioid use following total joint arthroplasty. J Arthroplasty. 2018;33(3):668. doi: 10.1016/j.arth.2017.10.011. [DOI] [PubMed] [Google Scholar]
- 18.Tran T., Castello J., Taylor S.E. Opioid use and appropriateness of supply after total knee or hip arthroplasty: an Australian perspective. J Am Acad Orthop Surg. 2020;28(23):e980–e989. doi: 10.5435/JAAOS-D-19-00789. [DOI] [PubMed] [Google Scholar]
- 19.Prentice H.A., Inacio M.C.S., Singh A., Namba R.S., Paxton E.W. Preoperative risk factors for opioid utilization after total hip arthroplasty. J Bone Joint Surg Am. 2019;101(18):1670. doi: 10.2106/JBJS.18.01005. [DOI] [PubMed] [Google Scholar]
- 20.Sun E.C., Darnall B.D., Baker L.C., Mackey S. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period.[Erratum appears in JAMA intern med. 2016 sep 1;176(9):1412; PMID: 27533349] JAMA Intern Med. 2016;176(9):1286. doi: 10.1001/jamainternmed.2016.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rao A.G., Chan P.H., Prentice H.A. Risk factors for postoperative opioid use after elective shoulder arthroplasty. J Should Elbow Surg. 2018;27(11):1960. doi: 10.1016/j.jse.2018.04.018. [DOI] [PubMed] [Google Scholar]
- 22.Pugely A.J., Bedard N.A., Kalakoti P. Opioid use following cervical spine surgery: trends and factors associated with long-term use. Spine J. 2018;18(11):1974. doi: 10.1016/j.spinee.2018.03.018. [DOI] [PubMed] [Google Scholar]
- 23.Owen J.A., Sitar D.S., Berger L., Brownell L., Duke P.C., Mitenko P.A. Age-related morphine kinetics. Clin Pharmacol Ther. 1983;34(3):364. doi: 10.1038/clpt.1983.180. [DOI] [PubMed] [Google Scholar]
- 24.Naples J.G., Gellad W.F., Hanlon J.T. The role of opioid analgesics in geriatric pain management. Clin Geriatr Med. 2016;32(4):725. doi: 10.1016/j.cger.2016.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ellis M.S., Kasper Z.A., Cicero T.J. The impact of opioid use disorder on levels of educational attainment: perceived benefits and consequences. Drug Alcohol Depend. 2020;206:107618. doi: 10.1016/j.drugalcdep.2019.107618. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


