Abstract
Breast cancer remains the most common cause of morbidity and mortality by cancer in females worldwide, even though it is largely preventable through population screening. Despite notable progress in the last years in the EU, breast cancer screening programs still maintain wide variations among countries and socio-economic groups. This statistical review aimed to investigate the breast cancer-related health gaps in Romanian women compared to the average EU female population after 10 years of accession (2007-2016). We evaluated breast cancer-related deaths, age-standardized mortality rates and contribution of breast cancer to life expectancy. Trends and percentage changes were compared between Romania and EU-27 for breast cancer, all cancer and all causes of mortality. We found a higher increase of breast cancer deaths in Romania, an increasing trend of mortality (opposite to EU) and a contribution to life expectancy at birth that increased gradually from 0.45 to 0 48 years. All these health gaps compared to EU are aggravated by the fact that no population screening for breast cancer is organized in the country. The opportunities for organizing such a program are consistent, but they should be increased in the future, in order to control the health gap between Romania and EU.
Keywords: breast cancer deaths, age-standardized mortality, breast cancer screening, gaps in health status, breast cancer life expectancy
1. Introduction
Breast cancer remains the most common cause of morbidity and mortality by cancer in females worldwide (1,2). During the last decade (2005-2015), the number of cases of breast cancer increased by 35% worldwide, and approximately one-fifth of this increase was due to an increase in incidence rates (2). Notably, the breast cancer incidence (age standardized rate) decreased only in countries with a high social development index (SDI), while it increased in all the other countries (2). In regard to mortality, the worldwide number of deaths increased by 21%, but the age-standardized death rate declined globally by 6% (3). The decline in mortality was seen especially in high SDI and high middle SDI countries (3-6).
Worldwide, 2,088,849 new cases and 626,679 deaths due to breast cancer were estimated as occurring in 2018 by the International Agency for Research on Cancer and World Health Organization, with this disease accounting for 24% of all new cases of cancer and 15% of all cancer-related deaths in females (7). In Europe, for the same year, same source, 522,513 new cases and 137,707 deaths due to breast cancer were estimated to occur in females, these representing 26.4% of all cancers and 16% of cancer-related deaths in this region (7). Thus, in 2018, Europe possessed 23% of all breast cancer cases in the world and 21% of deaths, although it has only 10% of the world female population.
Despite its extensive impact on public health worldwide, breast cancer is largely preventable through healthy lifestyle, specific high-risk strategies for non-modifiable risks and early detection (8-11). Breast cancer screening through mammography is largely recommended worldwide, and contributions of 20-40% to a reduction in mortality were revealed by different studies (10,12-16).
In the European Union (EU), high quality population screening through mammography in women aged 50-69 years has been recognized as a priority for action (together with screening for cervix and colon cancer) since 2003(17). Two assessments of the implementation for this recommendation have been performed. The first (2008) revealed that 11 countries had population-based screening programs for cancer screening (18). The second assessment found a notable progress in improving access to breast cancer screening, with 79% of the eligible women covered by invitation to screening and 49% covered by examination (19). However, wide variations in access to screening for breast cancer, as well as in incidence and mortality for this disease still persist in the EU, and generally, women in more socio-economically deprived areas have lower access to screening, lower breast cancer incidence, but higher mortality rates (19-22).
This statistical review aimed to investigate the breast cancer-related health gaps in Romanian women compared to the average EU female population after 10 years of accession. We focused on breast cancer mortality indicators: Breast cancer deaths, age standardized mortality rates, life expectancy at birth and contribution of breast cancer to life expectancy.
2. Statistical collection methods
The study interval was 2007-2016, 2007 being the year of accession of Romania to the EU. The study populations were represented by the female population of Romania and EU 27 (the 27 EU countries excluding the UK since 2020), respectively.
Breast cancer-related deaths were considered following the code C50 of the International Classification of Diseases Revision 10 (ICD-10), which is used in the country at present (23). They were analyzed as percentage change compared to deaths from 2007 for both Romania and EU. We also compared changes in breast cancer deaths with changes in deaths for all cancer (C00-C97) and all causes of deaths (A00-Y89, excluding S00-T98) (24).
The annual standardized mortality rates were compared as trend and percentage change over 10 years among the two populations. For understanding the breast cancer situation, we followed also the deaths for all causes and all cancer-related deaths.
Life expectancy at birth was compared as trend and percentage change. Contribution of breast cancer to life expectancy was calculated only for Romania.
All the data were extracted from Eurostat database (deaths by different ICD codes, age standardized mortality rates, life expectancy, population by age-group) (24). The contribution of breast cancer to life expectancy was calculated using the abridged life table for five-year age groups (24,25).
Morbidity indicators (incident cases/rates) were not considered due to the fact that routine reporting of morbidity is fragmentary, and the country does not have a national functional registry for breast cancer.
3. Results of the statistical analysis
Country context
Romania experienced a delay in implementing an organized population screening for breast cancer compared to other EU members. The country accessed the EU in 2007 and at that moment, a breast cancer screening was under planning (18). In 2017, a breast cancer screening was under piloting as a small-scale project (19). Some attempts to provide free access to mammography screening for women of eligible age were envisaged, either as service included in the basic health package of services, or in the framework of some projects, but the impact of these measures was very low, once that 79% of the Romanian women report they never had a breast X-ray examination (20).
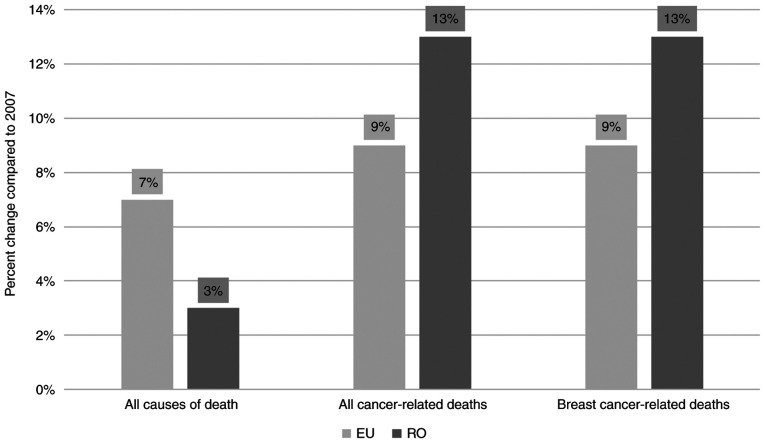
Changes in the number of deaths
In 2007, in the EU 27 female population, there were a registered 2,121,906 deaths of all causes, 468,044 deaths due to all cancers and 77,743 deaths due to breast cancer. In Romania, in the same year, 118,560 deaths from all causes, 18,491 deaths due to all cancers and 3,049 deaths due to breast cancer were registered. After 10 years, the annual deaths from all causes in the EU increased by 7%; meanwhile the number of deaths due to all cancers and the number of deaths due to breast cancer increased by 9% each (Fig. 1). Romania had only 3% increase of the annual deaths of all causes in 2016 compared to 2007, but the deaths due to all cancers and the breast cancer-related deaths increased by 13%, compared to 2007 (Fig. 1).
Figure 1.
Change in annual deaths in 2016, compared to 2007: EU and Romania. EU, European Union; RO, Romania.
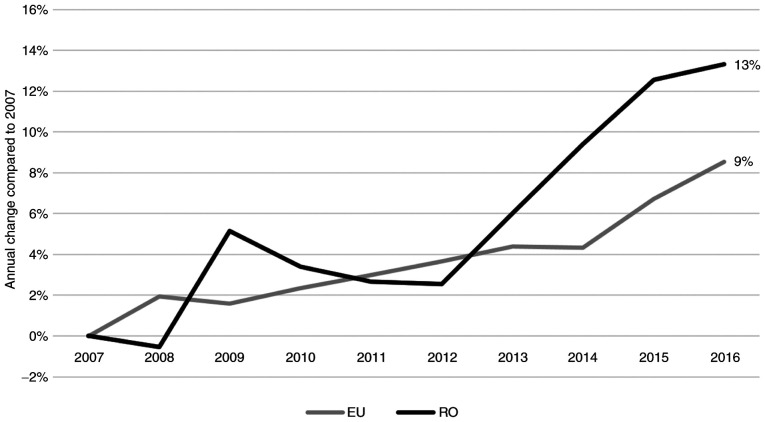
The annual change in breast cancer-related deaths in EU was slightly upward, reaching 9% in 2016; meanwhile in Romania there were higher variations and an obvious worsening after 2012 (Fig. 2).
Figure 2.
Trend of annual change in breast cancer-related deaths compared to 2007. EU and Romania. EU, European Union; RO, Romania.
Changes in the age-standardized mortality rate
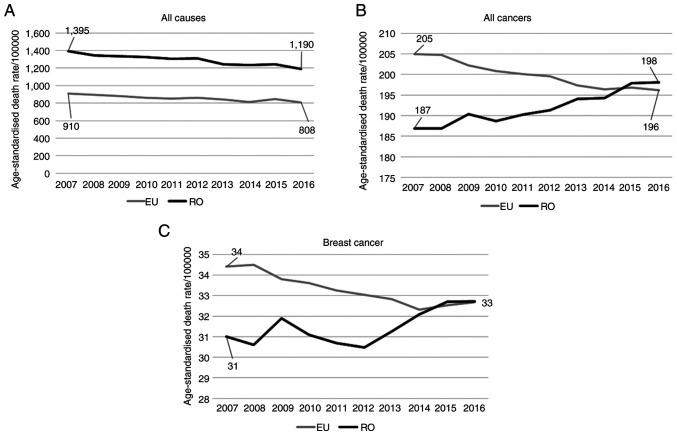
The age-standardized mortality rates for all causes had similar, slightly decreasing and almost parallel trends in the EU and Romania, with Romania starting the beginning of the interval with a much higher value compared to the EU (1,395 deaths/100,000 inhabitants, compared to 910 in the EU) (Fig. 3A). At the end of the study interval, the mortality in Romania decreased by 15% while mortality in the EU decreased by 11%. In 2016, mortality due to all causes in Romania was 47% higher compared to the EU.
Figure 3.
(A) Age standardized mortality rates, 2007-2016, Romania vs. EU for all causes. (B) Age standardized mortality rates, 2007-2016, Romania vs. EU for all cancers. (C) Age standardized mortality rates, 2007-2016, Romania vs. EU for breast cancer. EU, European Union; RO, Romania.
The mortality of all cancers had divergent trends in Romania and EU (Fig. 3B). Romania started at the beginning of the study period with a 9% lower mortality of all cancers compared to EU, but it had an increasing trend, while the mortality due to all cancers in the EU decreased progressively in the interval. Overall, the all cancer mortality rate in Romania increased by 6% and that of EU decreased by 4%. In 2016, the mortality in Romania was 1% higher compared to the EU.
Breast cancer-related mortality had also divergent trends, with a constant decline in the EU, but an irregular, increasing course for Romania (Fig. 3C). In 2007, the mortality in Romania was 9% lower compared than the EU, but in 2016, all the advantage that Romania apparently had at the beginning of the interval was lost, both populations reaching the same mortality rate. Overall, we found an increase of 6% in Romania and a decrease by 5% in EU. The increasing trend of breast cancer mortality in Romania has been underlined also in the precedent decade (26). It is assumed that it will continue in the future and this will widen the health gap compared to the EU.
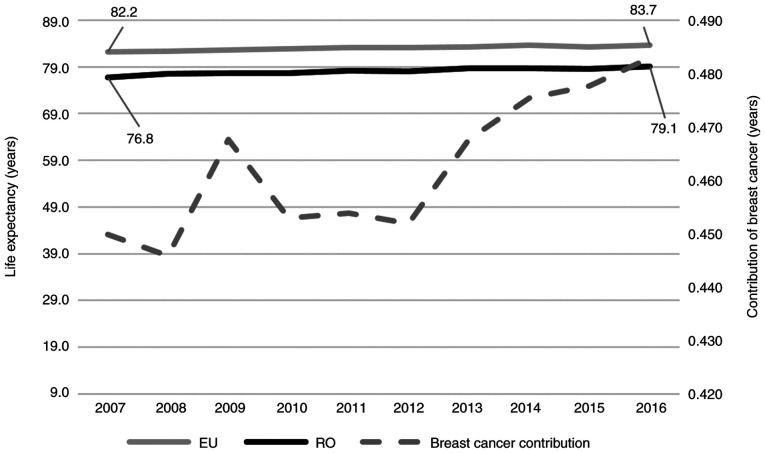
Changes in life expectancy at birth
In 2007, Romanian females had one of the lowest life expectancies at birth of 76.8 years among all EU members, with 5.4 year gap compared to the EU average. A slight increasing trend was found for both Romania and EU, with a small reduction in the gap (Fig. 4). Thus, at the end of the interval, life expectancy at birth increased by 3 and 2% in Romania and the EU, respectively, and the gap reached 4.8 years.
Figure 4.
Life expectancy at birth, trends for 2007-2016, Romania vs. EU. EU, European Union; RO, Romania.
The contribution of breast cancer to the reduction in life expectancy at birth reached 0.45 years in 2007 and increased slowly to 0.48 years in 2016.
4. Discussion
At present, the access to breast screening mammography in Romanian women is fragmentary, often imposing out-of-pocket payment for the investigation. No population screening has been organized to date, despite some attempts to include mammography screening in the national health programs or to some pilot projects that have been implemented, in conformity of Order of the Health Minister and of the president of the National Health Insurance House no 574/269/2008 regarding the implementing norms for the national health programs (27-36). Therefore, a small section of the female population in Romania regularly undergoes clinical and imaging examinations, in the context of which in Romania breast cancer is the first cause of cancer-related death in females, with a long gap to colon or lung cancer.
The situation in Romania is not particular, as evidence suggests that access to organized screening programs for breast cancer is more restricted in Eastern Europe, compared to the rest of the continent, despite the fact that organized mammography screening reduces the mortality due to breast cancer (20,37,38). Moreover, countries from Eastern Europe have more limited capacities for organizing population screening and usually lack the high-quality data for measuring the occurrence of breast cancer (38).
In Romania, breast cancer represents the main cause of cancer-related mortality in females, presenting an increased number over the years and a constant proportion of 16% of all cancer-related deaths. The mortality model is worsening, and this increased the health gap compared to the EU female population. All of these facts represent urgent reasons for acting for planning and implementing an organized, population-based screening.
As an EU member, Romania has been concerned in the last decade about the need for implementing a population-based breast cancer screening. Opportunities for developing such a program have been prioritized in the Partnership Agreement with EU for 2014-2020(39). Under this framework, an important project for developing breast cancer screening is planned: ‘Operational Program Human Capital (project no. 120799) (40). Increasing the institutional capacity and professional competencies of health system specialists is needed in order to implement the National Breast Cancer Screening Program. In its first phase, this project aims to build capacity in the country by creating a reference center for regional breast cancer screening programs, by developing a national standardized methodology for prevention, early detection, diagnosis and early treatment of breast cancer, in accordance with European guidelines, and by providing training for the medical workforce (40). Increase in awareness of the general population and vulnerable groups for attending the breast cancer screening is also a priority objective, in the context in which information campaigns for screening programs lacking in Romania are up to date (38). The second phase of the project is under preparation and there is expected to provide breast screening in four regions of the country, targeting a minimum of 30,000 women aged 50-69 years, with a focus on vulnerable groups: Operational Program Human Capital Applicants Guideline ‘Be responsible for your health-regional programs for prevention, early detection, diagnosis and early treatment for breast cancer-phase 2’ (41).
This project is essential in the existing country context and there is expected that, after its successful implementation (planned to end in 2023), breast screening will be provided throughout the country. However, about three million women aged 50-69 years live in Romania at present according to Eurostat database (24). If we consider only this age-group for mammography screening, and only one examination every three years for each woman, which is below the European Guideline, the project will cover around 1% of the eligible population. This means that more efforts and resources should be concentrated to organize a population breast cancer screening in Romania in the next years, in order to speed up the process of ensuring proper access for all eligible women, on ethical premises, and also to slow the upward trend of breast cancer-related mortality.
5. Conclusions
Breast cancer represents an important public health issue in Romania, through the trend in the increasing number of deaths and mortality in the last decade and through its contribution to lower life expectancy. The absence of an organized population screening in the country will aggravate the gap in breast cancer mortality between Romania and the EU in the near future.
Romania has concrete and consistent opportunities to develop a population screening for breast cancer in the upcoming years. These opportunities seem to be relevant, but far from sufficient for covering the eligible population on short-term basis. More efforts and resources should be concentrated in the next years in order to ensure universal access to breast screening for eligible women, and to control the gap in health status between Romania and the EU.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and analyzed during the current study are available from Eurostat and the National Institute of Statistics, Bucharest, Romania, on reasonable request.
Authors' contributions
FF, REB and CSP collected and analyzed the data regarding the breast cancer mortality in Romania compared with the EU. FF, REB, CSP, TAG and OM made substantial contribution to the conception of the work and interpretation of data; in addition, they drafted the manuscript and were major contributors in writing the manuscript. SV and AN made substantial contributed to the design of the work, further drafts and comments. FF and REB performed statistical analysis and study description. All authors read and approved the final version of the manuscript.
Ethics approval and consent to participate
Not required due to the statistical analysis nature of the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Azamjah N, Soltan-Zadeh Y, Zayeri F. Global trend of breast cancer mortality rate: A 25-year study. Asian Pac J Cancer Prev. 2019;20:2015–2020. doi: 10.31557/APJCP.2019.20.7.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, Brenner H, Dicker DJ, Chimed-Orchir O, Dandona R, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: A systematic analysis for the global burden of disease study. JAMA Oncol. 2017;3:524–548. doi: 10.1001/jamaoncol.2016.5688. Global Burden of Disease Cancer Collaboration. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1545–1602. doi: 10.1016/S0140-6736(16)31678-6. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ying W, Yi Z, Zhen Z, Qian H, Dingli S, Dai Z, Huafeng K, Zhijun D. Global burden of breast cancer and attributable risk factors in 195 countries and territories, from 1990 to 2017: Results from the Global Burden of Disease Study 2017. J Hematol Oncol. 2019;12(140) doi: 10.1186/s13045-019-0828-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Longfei L, Lei Y, Yuling L, Fang Y, Hui Li, Jian N. Incidence and death in 29 cancer groups in 2017 and trend analysis from 1990 to 2017 from the Global Burden of Disease Study. J Hematol Oncol. 2019;12(96) doi: 10.1186/s13045-019-0783-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharma R. Breast cancer incidence, mortality and mortality-to-incidence ratio (MIR) are associated with human development, 1990-2016: Evidence from Global burden of disease study 2016. Breast Cancer. 2019;26:428–445. doi: 10.1007/s12282-018-00941-4. [DOI] [PubMed] [Google Scholar]
- 7. International Agency for Research on Cancer and World Health Organization. Global Cancer Observatory. Cancer today. Available from: https://gco.iarc.fr// (accessed on 23 Oct, 2020). [Google Scholar]
- 8.Lacey JV Jr, Kreimer AR, Buys SS, Marcus PM, Chang SC, Leitzmann MF, Hoover RN, Prorok PC, Berg CD, Hartge P. Breast cancer epidemiology according to recognized breast cancer risk factors in the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial Cohort. BMC Cancer. 2009;9(84) doi: 10.1186/1471-2407-9-84. Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial Project Team. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marmot MG, Altman DG, Cameron DA, Dewar JA, Thompson SG, Wilcox M. The benefits and harms of breast cancer screening: An independent review. Br J Cancer. 2013;108:2205–2240. doi: 10.1038/bjc.2013.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. International Agency for Research on Cancer: IARC Handbooks of Cancer Prevention. Volume 15: Breast Cancer Screening. IARC Press, Lyon, 2015. [Google Scholar]
- 11.Dimitrova N, Saz PZE, Bramesfeld A, Ulutürk A, Bocchi G, López-Alcalde J, Pylkkanen L, Neamțiu L, Ambrosio M, Deandrea S, Lerda D. European guidelines for breast cancer screening and diagnosis-the European Breast Guidelines. EUR 28360 EN doi:10.2788/503032. 2016. [Google Scholar]
- 12.The benefits and harms of breast cancer screening: An independent review. Lancet. 2012;380:1778–1786. doi: 10.1016/S0140-6736(12)61611-0. Independent UK Panel on Breast Cancer Screening. [DOI] [PubMed] [Google Scholar]
- 13.Monticciolo DL. Current guidelines and gaps in breast cancer screening. J Am Coll Radiol. 2020;17:1269–1275. doi: 10.1016/j.jacr.2020.05.002. [DOI] [PubMed] [Google Scholar]
- 14.Beau AB, Andersen PK, Vejborg I, Lynge E. Limitations in the effect of screening on breast cancer mortality. J Clin Oncol. 2018;36:2988–2994. doi: 10.1200/JCO.2018.78.0270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Olsen AH, Lynge E, Njor SH, Merethe K, Marit W, Tonje B, Eiliv L. Breast cancer mortality in Norway after the introduction of mammography screening. Int J Cancer. 2013;132:208–214. doi: 10.1002/ijc.27609. [DOI] [PubMed] [Google Scholar]
- 16.Peintinger F. National breast screening programs across Europe. Breast Care (Basel) 2019;14:354–358. doi: 10.1159/000503715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Off J Eur Union. 2003;327:34–38. European Council. Council recommendation of 2 December 2003 on cancer screening (2003/878/EC) [Google Scholar]
- 18.Von Karsa L, Anttila A, Ronco GL, Ponti A, Malila N, Arbyn M, Segnan N, Castillo-Beltran M, Boniol M, Ferlay J, et al. Cancer screening in the European Union. Report on the implementation of the Council Recommendation on cancer screening. First report. Brussels: European Commission; 2008. https://eur-lex.europa.eu/legal-content/en/ALL/?uri=CELEX%3A52008DC0882. [Google Scholar]
- 19.Ponti A, Anttila A, Ronco G, Senore C. Cancer Screening in the European Union. Report on the implementation of Council Recommendation on Cancer Screening. Brussels: European Commission; 2017. https://screening.iarc.fr/EUreport.php. [Google Scholar]
- 20.Smith D, Thomson K, Bambra C, Todd A. The breast cancer paradox: A systematic review of the association between area-level deprivation and breast cancer screening uptake in Europe. Cancer Epidemiol. 2019;60:77–85. doi: 10.1016/j.canep.2019.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Levi F, Lucchini E, Negri C, Vecchia L. Trends in mortality from major cancers in the European Union, including acceding countries, in 2004. Cancer. 2004;101:2843–2850. doi: 10.1002/cncr.20666. [DOI] [PubMed] [Google Scholar]
- 22.Deandrea S, Molina-Barceló A, Uluturk A, Moreno J, Neamtiu L, Peiró-Pérez R, Saz-Parkinson Z, Lopez-Alcalde J, Lerda D, Salas D. Presence, characteristics and equity of access to breast cancer screening programmes in 27 European countries in 2010 and 2014. Results from an international survey. Prev Med. 2016;91:250–263. doi: 10.1016/j.ypmed.2016.08.021. [DOI] [PubMed] [Google Scholar]
- 23. World Health Organization. International Statistical Classification of Diseases and Related Health Problems. 10th Revision. Volume 2. Instruction manual, 1-174, 2010. [Google Scholar]
- 24. Eurostat database. Population and social condition. Health status. https://ec.europa.eu/eurostat/data/database// (accessed on 23 Oct, 20). [Google Scholar]
- 25. Chiang Chin Long: Life Table and mortality analysis. World Health Organization Geneva. 1978. https://apps.who.int/iris/bitstream/handle/10665/62916/15736_eng.pdf. [Google Scholar]
- 26.Tereanu C, Baili P, Berrino F, Micheli A, Furtunescu FL, Minca DG, Sant M. Recent trends of cancer mortality in Romanian adults: Mortality is still increasing, although young adults do better than the middle-aged and elderly population. Eur J Cancer Prev. 2013;22:199–209. doi: 10.1097/CEJ.0b013e3283581d90. [DOI] [PubMed] [Google Scholar]
- 27.Bohîlțea RE, Turcan G, Cîrstoiu MM, Ionescu C, Nemescu D, Turcan N, Vladareanu R. Clinical implementation of ultrasound gynecological examination report (software REGU) based on international consensuses of tumor study groups. Filodiritto editore-proceedings. 5th Romanian congress of the Romanian society of ultrasound in obstetrics And Gynecology: 99-104, 2017. [Google Scholar]
- 28.Badea M, Baros A, Bohiltea RE, Julea IE, Furtunescu F, Istrate-Ofiteru AM, Iovan L, Cirstoiu MM, Burcin MR, Turcan N, et al. Modern interdisciplinary monitoring of cervical cancer risk. Rom J Morphol Embryol. 2019;60:469–478. [PubMed] [Google Scholar]
- 29.Tataru AL, Furau G, Afilon J, Ionescu C, Dimitriu M, Bratu OG, Tit DM, Bungau S, Furau C. The situation of cervical cancers in the context of female genital cancer clustering and burden of disease in Arad County, Romania. J Clin Med. 2019;8(96) doi: 10.3390/jcm8010096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Iorga RA, Bratu OG, Marcu RD, Constantin T, Mischianu DLD, Socea B, Gaman MA, Diaconu CC. Venous thromboembolism in cancer patients: Still looking for answers (Review) Exp Ther Med. 2019;18:5026–5032. doi: 10.3892/etm.2019.8019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miricescu D, Diaconu CC, Stefani C, Stanescu AMA, Totan A, Rusu IR, Bratu OG, Spinu D, Greabu M. The serine/threonine protein kinase (Akt)/protein kinase B (PkB) signaling pathway in breast cancer. J Mind Med Sci. 2020;7:34–39. [Google Scholar]
- 32.Ionescu CA, Matei A, Navolan D, Dimitriu M, Bohîltea R, Neacsu A, Ilinca C, Ples L. Correlation of ultrasound features and the risk of ovarian malignancy algorithm score for different histopathological subtypes of benign adnexal masses. Medicine. 2018;97(e11762) doi: 10.1097/MD.0000000000011762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bohîlțea RE, Ancăr V, Cîrstoiu M, Rădoi V, Bohiltea LC, Furtunescu F. Project for the National program of early diagnosis of endometrial cancer part I. J Med Life. 2015;8:305–314. [PMC free article] [PubMed] [Google Scholar]
- 34.Bohîlțea RE, Ancăr V, Rădoi V, Furtunescu F, Bohiltea LC. Project for the National program of early diagnosis of endometrial cancer part II. J Med Life. 2015;8:423–431. [PMC free article] [PubMed] [Google Scholar]
- 35.Bohîlțea RE, Furtunescu F, Dosius M, Cîrstoiu M, Radoi V, Baros A, Bohiltea LC. Evaluation of endometrial cancer epidemiology in Romania. J Med Life. 2015;8:218–225. [PMC free article] [PubMed] [Google Scholar]
- 36.Bohîlțea RE, Sajin M, Furtunescu F, Bohiltea LC, Mihart A, Baros A, Anca AF. Clinical and pathological correlations in endometrial pathology. J Med Life. 2015;8:552–562. [PMC free article] [PubMed] [Google Scholar]
- 37.Zielonke N, Gini A, Jansen EEL, Anttila A, Segnan N, Ponti A, Veerus P, de Koning HJ, van Ravesteyn NT, Heijnsdijka EAM. Evidence for reducing cancer-specific mortality due to screening for breast cancer in Europe: A systematic review. Eur J Cancer. 2020;127:191–206. doi: 10.1016/j.ejca.2019.12.010. EU-TOPIA consortium. [DOI] [PubMed] [Google Scholar]
- 38.Altobelli E, Rapacchietta L, Angeletti PM, Barbante L, Profeta FV, Fagnano R. Breast cancer screening programmes across the WHO European Region: Differences among countries based on national income level. Int J Environ Res Public Health. 2017;14(452) doi: 10.3390/ijerph14040452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Partnership Agreement Romania 2014RO16M8PA001.1.2. https://www.fonduri-ue.ro/acord-parteneriat#varianta-%C3%AEn-englez%C4%83. [Google Scholar]
- 40. Oncologic Institute ‘Prof Dr I Chiricuta’ Cluj Napoca. Project 120799 ‘Increasing the institutional capacity and professional competencies of health system specialists in order to implement the National Breast Cancer Screening Program. http://www.iocn.ro/Noutati/-Publicatii-proiect-POCU-Etapa-I-Cresterea-capacitatii-institutionale-si-a-competentelor-profesionale-ale-specialistilor-din-sistemul-de-sanatate-in-scopul-implementarii-Programului-National-de-screening-pentru-cancerul-de-san-120799-eID967.html. [Google Scholar]
- 41. Ministry of the European Funds. Project Fische ‘Breast cancer screening-stage 2’. https://www.fonduri-structurale.ro/fisa-proiect/2/programul-operational-capital-uman/275/pocu-4-9-screening-cancer-de-san-etapa-ii. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from Eurostat and the National Institute of Statistics, Bucharest, Romania, on reasonable request.