Abstract
This cohort study compares family caregiver hours provided to those with vs without dementia during the last 10 years of life.
Family caregivers of people with dementia (eg, spouses, children, and other unpaid caregivers) provide high levels of care1 and experience substantial caregiver strain at the end of life,2 yet little is known about the trajectory of care as the end of life approaches and how individual family members contribute to total care. We compared the hours of care that family caregivers provide to those with and without dementia during the last 10 years of life.
Methods
We sampled all decedents in the nationally representative Health and Retirement Study, including interview waves 2006 to 2016, who were 75 years or older at the time of death (n = 5266) and excluded those with significant missing data (n = 1317). Data analysis was conducted between October 2019 and March 2020. We determined each family caregiver’s annual care hours using the decedent’s self-reported hours of help received with self-care and household activities in the preceding month. We estimated caregiving hours between interviews using a weighted average of hours from each interview and assigned annual prorated hours based on the time from interview to death.3 We used a clinically validated algorithm4 to determine dementia status in the interview before death and then stratified results based on marital status. The study was approved by the Mount Sinai School of Medicine institutional review board with a waiver of informed consent due to the retrospective nature of the study.
Results
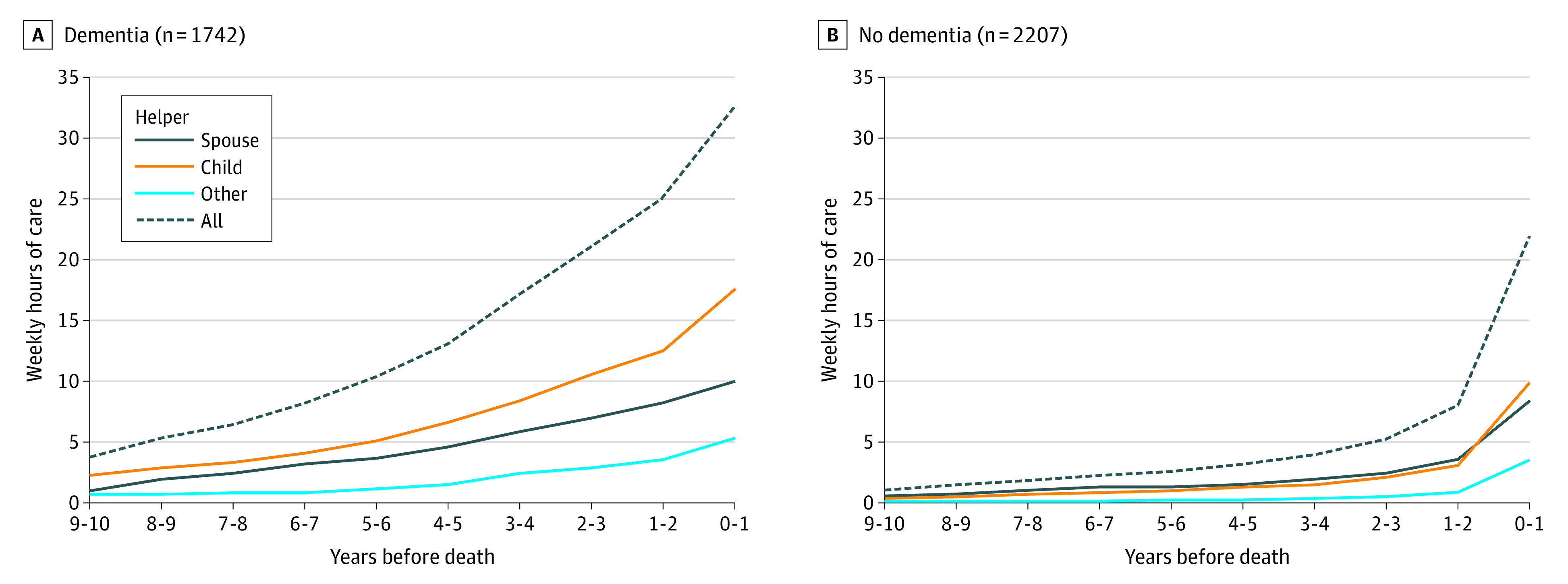
Family caregivers of people with dementia provided 3 times as many total hours of care over the last 10 years of life compared with caregivers of those without dementia (Figure). While care hours provided to those with dementia increased steadily in each of the last 10 years (mean annual increase, 17%; range 18%-41%), care hours provided to those without dementia remained low and then nearly tripled in the last year of life (mean [SD] of 8 [23] hours of care per week 1-2 years before death and 22 [35] hours in the last year of life). Adult children of those with dementia provided a larger portion of total care hours (50%) compared with those without dementia (41%). In the last year of life, adult children of those with dementia provided a mean (SD) of 17 (34) hours of care per week, while children of those without dementia provided a mean (SD) of 10 (22) hours. Among those married at the interview before death, spousal caregivers provided most of the care hours over all 10 years before death in the dementia and nondementia groups (81% and 77% of total care hours, respectively).
Figure. Weekly Caregiving Hours in the Last 10 Years of Life by Dementia Status and Caregiver Type.
Discussion
Our study highlights the high levels of caregiving provided to those with dementia by their family caregivers in general and by adult children in particular. All married individuals relied primarily on spouses to provide care. However, adult children provided the bulk of care for family members with dementia, who were on average older and more likely to be widowed; substantial caregiving responsibilities for this population often began at least 10 years before death.
The survey data did not assess the total time caregivers spent with family members; some time reported as caregiving may have replaced time spent in social engagement before needs arose, and our results may therefore overstate the time spent providing care. However, this limitation is unlikely to explain the many hours spent caregiving for individuals with dementia. Moreover, sustained caregiving responsibilities for individuals with dementia likely have financial implications beyond the time spent providing care. Caregivers may work fewer hours, miss opportunities for advancement, or fail to enter or stay in the workforce5; indirect costs of caregiving affect financial security and retirement savings and may even affect opportunities for the next generation. Because of the higher prevalence of dementia among those with lower socioeconomic status, the intergenerational effect of caregiving is particularly concerning for those already struggling to achieve equity. Existing programs that provide short-term, episodic support for caregivers (eg, the US Family Medical Leave Act and paid family leave) do not match the long-term, progressive care needs of those with dementia.
References:
- 1.Kasper JD, Freedman VA, Spillman BC, Wolff JL. The disproportionate impact of dementia on family and unpaid caregiving to older adults. Health Aff (Millwood). 2015;34(10):1642-1649. doi: 10.1377/hlthaff.2015.0536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vick JB, Ornstein KA, Szanton SL, Dy SM, Wolff JL. Does caregiving strain increase as patients with and without dementia approach the end of life? J Pain Symptom Manage. 2019;57(2):199-208.e2. doi: 10.1016/j.jpainsymman.2018.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kelley AS, McGarry K, Gorges R, Skinner JS. The burden of health care costs for patients with dementia in the last 5 years of life. Ann Intern Med. 2015;163(10):729-736. doi: 10.7326/M15-0381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Plassman BL, Langa KM, Fisher GG, et al. . Prevalence of dementia in the United States: the aging, demographics, and memory study. Neuroepidemiology. 2007;29(1-2):125-132. doi: 10.1159/000109998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Van Houtven CH, Coe NB, Skira MM. The effect of informal care on work and wages. J Health Econ. 2013;32(1):240-252. doi: 10.1016/j.jhealeco.2012.10.006 [DOI] [PubMed] [Google Scholar]


