Abstract
Background:
Stimulant medications are commonly prescribed for the treatment of attention-deficit/hyperactivity disorder; however, they also have high potential for diversion and misuse. We estimated national stimulant dispensing trends from 2014 to 2019 and differences in dispensing by age, sex, state, prescriber specialty, payor type, patient copay, and stimulant type.
Methods:
We calculated rates of stimulant dispensing using IQVIA National Prescription Audit (NPA) New to Brand, NPA Regional, and NPA Extended Insights data, which provide dispensing estimates from approximately 49,900 pharmacies representing 92 % of prescriptions dispensed in the United States. Average annual percent change (AAPC) from 2014 to 2019 was analyzed using Joinpoint regression.
Results:
From 2014 to 2019, the national annual rate of stimulant dispensing increased significantly from 5.6 to 6.1 prescriptions per 100 persons. Rates differed by prescription stimulant type, with increases occurring among both amphetamine-type stimulants and long-acting stimulants. Rates among females (AAPC = 3.6 %; P = 0.001) and adults aged 20–39 years (AAPC=6.7 %; P = 0.002), 40–59 years (AAPC=9.7 %; P < 0.001), and ≥60 years (AAPC = 6.9 %; P = 0.001) increased significantly during the study period. Stimulant dispensing rates varied substantially across states, ranging from 1.0 per 100 in Hawaii to 13.6 per 100 in Alabama.
Conclusions:
National stimulant dispensing rates increased from 2014 to 2019, driven by notable increases among females and adults aged ≥20 years. These trends should be considered when prescribing stimulants given growing concerns over prescription stimulant diversion, misuse, and related health harms.
Keywords: Prescription stimulants, Stimulant dispensing, Amphetamines, Methylphenidates
1. Introduction
Stimulant medications are commonly prescribed for the treatment of attention-deficit/hyperactivity disorder (ADHD). It is estimated that 9.4 % of children aged 2–17 years (Danielson et al., 2018) and 4.4 % of adults (Kessler et al., 2006) have ever been diagnosed with ADHD. Stimulant medications prescribed for ADHD include amphetamines (e. g., Adderall) and derivatives of amphetamine (e.g., Vyvanse) and methylphenidate (e.g., Ritalin and Concerta) and derivatives of methylphenidate (e.g., Focalin). In addition to their use for ADHD, some prescription stimulants are approved for the treatment of narcolepsy and short-term adjunct treatment of weight loss (U.S. National Library of Medicine, 2020b).
An estimated 16 million (6.6 %) U.S. adults (Compton et al., 2018) and 2.8 million (3.5 %) children (Zuvekas and Vitiello, 2012) use stimulants annually. Stimulant prescriptions for children age 0–17 years may exhibit seasonal fluctuations that reflect school attendance patterns, while prescriptions for adults have not shown such effects (Cascade et al., 2008). Stimulant use is higher among young adults than other adult age groups; approximately 13.0 % of adults aged 18–29 years used prescription stimulants in the past year compared to 6.7 % among adults aged 30–49 years and 3.5 % among those aged ≥50 years (Compton et al., 2018).
Prescription stimulants are also misused due to their central nervous system stimulant and euphoric effects (Compton et al., 2018), and their perceived cognitive enhancing effects. Nearly all prescription stimulants are classified as Schedule II controlled substances due to their high potential for misuse (U.S. Department of Justice Drug Enforcement Administration, 2020), which is defined as using a prescription stimulant drug in any way not indicated by one’s doctor, including using a stimulant that has been prescribed to someone else (i.e., diversion) or using a stimulant in greater amounts, more often, or longer than what has been prescribed (Substance Abuse and Mental Health Services Administration, 2019). In 2018, more than 5 million Americans reported past-year misuse, with the highest proportion of misuse reported among young adults aged 18–25 years (Substance Abuse and Mental Health Services Administration, 2019). Among this age group, 6.5 % of persons reported past-year misuse, compared to only 1.5 % of persons aged 12–17 years and 1.2 % of persons aged ≥26 years (Substance Abuse and Mental Health Services Administration, 2019). Some research estimates an even higher rate of stimulant medication misuse among college students specifically (17 %) (Benson et al., 2015). In addition, approximately half (52 %) of all 10–18 year-olds have engaged in prescription stimulant diversion in their lifetime, either by obtaining prescription stimulants from others or giving their prescription stimulants to someone else (Lasopa et al., 2015).
There are multiple potential health risks or consequences associated with prescription stimulant misuse. The misuse of stimulants is associated with a range of physical and psychological sequelae, including cardiovascular dysfunction, psychosis and other mental disorders, and overdose (U.S. National Library of Medicine, 2020a). An increased risk of developing diseases of the basal ganglia and cerebellum has also been observed in adult ADHD patients treated with prescription stimulants (Curtin et al., 2018). A chief concern of prolonged misuse is the potential for development of a stimulant use disorder (Han et al., 2017). A nationally-representative longitudinal study that followed individuals to age 35 found that adults who reported stimulant misuse in adolescence had lower educational attainment and more symptoms of substance use disorder than those who never used prescription stimulants and those who used prescription stimulants medically (McCabe et al., 2017). Another key health concern is the potential for negative interaction effects with other drugs or overdose, as people engaging in misuse are less likely to be aware of drug contraindications and appropriate use (Clemow and Walker, 2014). Furthermore, adolescents with ADHD who diverted their prescription stimulants have reported higher odds of experiencing peer victimization, including actual or threats of physical harm as well as relational harm through manipulating interpersonal relationships (Epstein-Ngo et al., 2016).
Despite the potential for diversion and misuse and associated health harms, little is known about current controlled substance stimulant dispensing trends. Recent analyses suggest that age, sex, and U.S. state of residence play a role in stimulant prescribing patterns (Burcu et al., 2016; Piper et al., 2018; Safer, 2016; Tseregounis et al., 2019), with stimulant sales to adults surpassing those of children, and adult women receiving more prescription stimulants than adult men (Burcu et al., 2016; Safer, 2016). Previous analyses have been limited to specific populations (Burcu et al., 2016; Tseregounis et al., 2019) or do not include the most recent available data on prescription stimulant dispensing trends (Burcu et al., 2016; Safer, 2016), limiting the development of informed policies, programs, and practices to prevent stimulant misuse and diversion. In this analysis, we estimated national stimulant dispensing trends from 2014 to 2019 and differences in dispensing by age, sex, state, prescriber specialty, payor type, patient copay, and stimulant type.
2. Material and methods
2.1. Data sources
We used IQVIA National Prescription Audit (NPA) New to Brand, NPA Regional, and NPA Extended Insights data, which provide dispensing estimates from approximately 48,900 of the 58,000 pharmacies in the United States, representing 92 % of all prescriptions dispensed in the U.S. Data were weighted to provide national estimates. Data on controlled substance stimulants were extracted by product name and further classified based on amphetamine-type (e.g., Adderall, Vyvanse) or methylphenidate-type (e.g., Ritalin, Concerta, and Focalin) substances, in addition to short-acting formulations (in which effectiveness peaks 2–3 hours after ingestion and lasts for 4–6 hours) or long-acting/extended-release formulations (in which effectiveness peaks 4–7 hours after ingestion and lasts for close to 12 hours; Supplemental Table 1) (Berman et al., 2009).
Census population estimates were obtained from the U.S. Census Bureau to calculate rates and included annual population estimates by age, sex, and state of residence, as well as monthly population estimates for the total U.S. population (U.S. Census Bureau, 2020). The three-month average population estimate for each quarter was calculated to use as the population-based denominator in quarterly analyses. Age-specific monthly population estimates were unavailable, so the annual age-based population was used instead for calculating age-specific quarterly rates. Additionally, age- and sex-specific annual population estimates were unavailable for 2019, so 2018 population estimates were used in their place to calculate 2019 age- and sex-specific rates.
2.2. Data analysis
National rates per 100 persons were calculated annually from 2014 to 2019 and by age group, sex, and stimulant product type. Quarterly rates from 2014 to 2019 were also calculated for the total U.S. population and by stimulant product type to examine seasonal changes in prescribing. Average annual percent change (AAPC) and average quarterly percent change (AQPC) were analyzed using Joinpoint regression (National Cancer Institute, Bethesda, MD). This approach analyzes trends across time using joinpoint models, in which several different lines are connected together at “joinpoints” to determine if and when significant changes in trends occur (Kim et al., 2000). Monte Carlo permutations (4499 permutations) are used to test significance of the models (Kim et al., 2000).
Controlled substance stimulant dispensing for 2019 was also calculated by each payor type (Medicaid, Medicare Part D, third party commercial health insurance, or cash/self-pay), patient copay, and prescriber specialty. State- and region-specific controlled substance stimulant dispensing rates per 100 persons were calculated for 2018 and 2019.
All rates were calculated using SAS v9.4. Chi square tests were run to conduct pairwise comparisons of 2019 rates by age range and sex, to compare 2018 and 2019 rates for the states and regions with the highest rates, and to compare regional differences for 2019 rates (only significant chi square results are presented in the text). P-values <0.05 were considered statistically significant.
CDC’s National Center for Injury Prevention and Control determined that the research was conducted with existing data without individual identifiers; thus, the activity is research not involving human subjects, and Institutional Review Board approval was not required.
3. Results
From 2014 to 2019, the national annual rate of stimulant dispensing increased significantly from 5.6 to 6.1 prescriptions per 100 persons (AAPC = 1.5 %; 95 % CI 0.5–2.5) (Table 1). Rates differed by prescription stimulant type, with increases occurring among both amphetamine-type stimulants (from 4.2 to 4.8 per 100; AAPC = 2.6 %; 95 % CI 0.4–4.7) and long-acting stimulants (from 5.4 to 5.9 per 100; AAPC = 1.6 %; 95 % CI 0.6–2.7). While quarterly rates remained relatively stable overall (AQPC = 0.4 %, 95 % CI 0.2–0.6), a seasonality effect in stimulant dispensing was observed in children <20 years; for children aged 0–9 years, rates were highest in the fourth quarter of each year and remained steady during the remaining quarters, while for children aged 10–19 years, rates peaked in the first quarter of the year and then dropped during the third quarter (Fig. 1).
Table 1.
Overall controlled substance stimulant dispensing trends – United States, 2014–2019.
| Data source: IQVIA National Prescription Audit (NPA) New to Brand. | ||||||||
|---|---|---|---|---|---|---|---|---|
| Annual ratesa | ||||||||
| 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | AAPCb | 95 % CI | |
| Total | 5.6 | 5.8 | 5.9 | 5.8 | 6.0 | 6.1 | 1.5 | (0.5, 2.5) |
| Age | ||||||||
| 0–9 | 7.3 | 6.9 | 6.6 | 6.1 | 6.0 | 5.8 | −4.7 | (−3.6, −12.0) |
| 10–19 | 19.5 | 19.6 | 19.0 | 18.0 | 18.8 | 18.4 | −1.4 | (−2.9, 0.1) |
| 20–39 | 4.5 | 5.1 | 5.7 | 5.8 | 6.1 | 6.4 | 6.7 | (4.2, 9.3) |
| 40–59 | 2.4 | 2.8 | 3.1 | 3.3 | 3.6 | 3.8 | 9.7 | (7.5, 12.0) |
| 60+ | 0.6 | 0.6 | 0.7 | 0.7 | 0.8 | 0.8 | 6.9 | (5.2, 8.6) |
| Sex | ||||||||
| Female | 4.2 | 4.5 | 4.7 | 4.7 | 5.0 | 5.1 | 3.6 | (2.4, 4.8) |
| Male | 6.8 | 6.9 | 6.9 | 6.6 | 6.9 | 6.9 | 0.1 | (−1.0, 1.2) |
| Product Type | ||||||||
| Amphetamine | 4.2 | 4.5 | 4.8 | 4.8 | 4.9 | 4.8 | 2.6 | (0.4, 4.7) |
| Methylphenidate | 1.3 | 1.1 | 1.0 | 0.9 | 1.0 | 1.1 | −2.8 | (−9.9, 4.9) |
| Product Release | ||||||||
| Short-acting | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | −6.8 | (−11.1, −2.3) |
| Long-acting | 5.4 | 5.5 | 5.7 | 5.5 | 5.8 | 5.9 | 1.6 | (0.6, 2.7) |
Bold typeface denotes statistical significance at P < 0.05.
Per 100 persons.
Average annual percent change in rates from 2014 to 2019; calculated using Joinpoint regression.
Fig. 1.
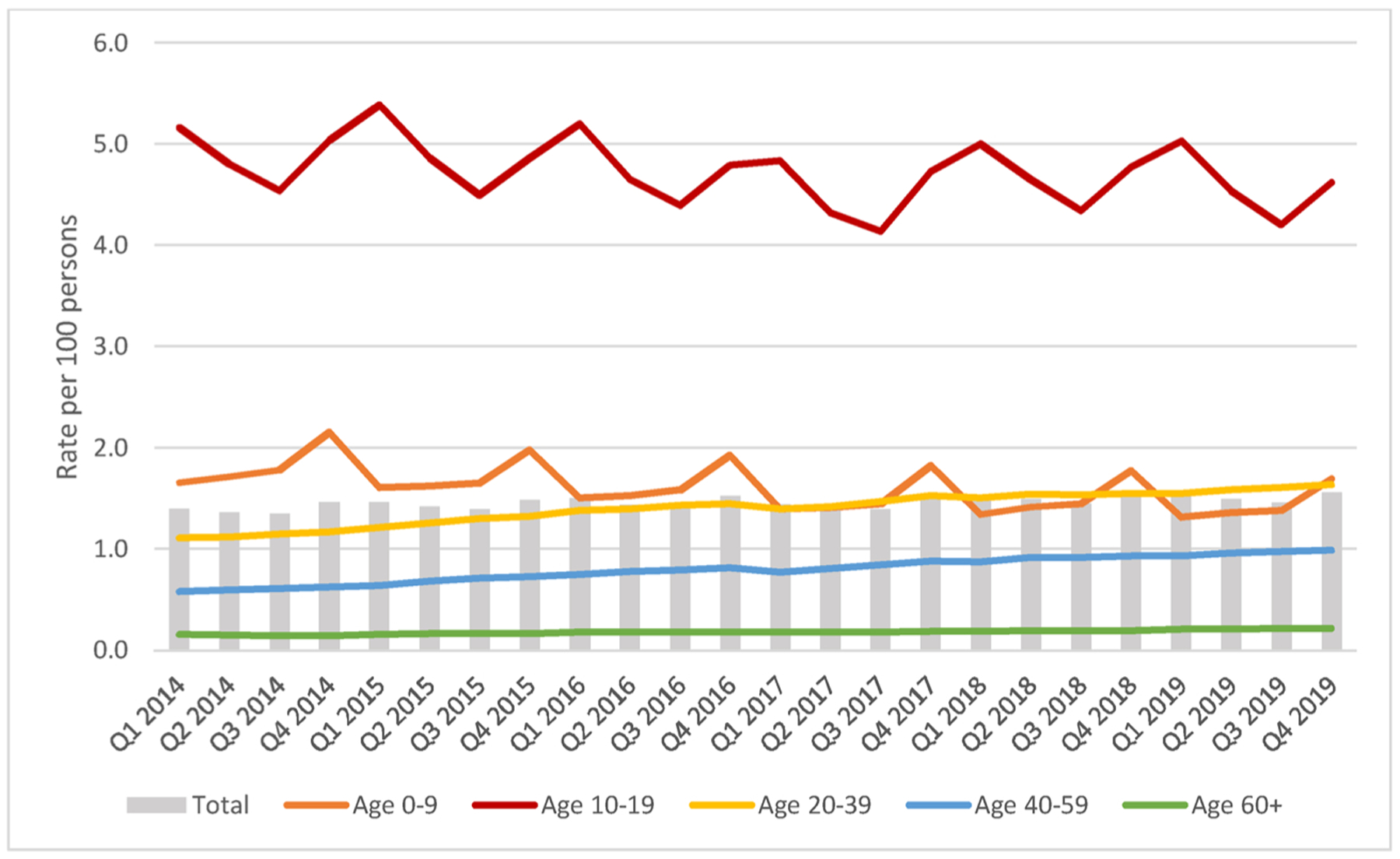
Quarterly controlled substance stimulant dispensing trends overall and by age group (per 100 persons) – United States, 2014–2019.
Data source: IQVIA National Prescription Audit (NPA) New to Brand.
Prescription stimulant dispensing rates increased significantly for females (AAPC = 3.6 %; 95 % CI 2.4–4.8), but not for males (AAPC = 0.1; 95 % CI −1.0–1.2), during the study period (Table 1). Children aged 0–9 years experienced a significant decrease in rates (AAPC = −4.7 %; 95 % CI −3.6–−12.0) from 2014 to 2019, while rates increased significantly among adults aged 20–39 years (AAPC = 6.7 %; 95 % CI 4.2–9.3), 40–59 years (AAPC = 9.7 %; 95 % CI 7.5–12.0), and ≥60 years (AAPC = 6.9 %; 95 % CI 5.2–8.6) (Table 1). Rates were highest among males aged 10–19 years; in 2019, one in four males aged 10–19 years was dispensed a prescription stimulant, compared to one in eight females (Table 2). Sex was a modifier for age-related trends in 2019; among children younger than 20, rates of stimulant dispensing were higher among males (8.2 and 24.6 per 100 for males aged 0–9 and 10–19 years, respectively) than females (3.2 and 11.9 per 100 for females aged 0–9 and 10–19 years, respectively; P < 0.001) in 2019, but for adults age ≥20 years, rates were higher among females (6.8, 4.8, and 1.0 per 100 for females aged 20–39, 40–59, and ≥60 years, respectively) than males (5.9, 2.9, and 0.7 per 100 for males aged 20–39, 40–59, and ≥60 years, respectively; P < 0.001) (Table 2).
Table 2.
Controlled substance stimulant dispensing trends by age and sex – United States, 2014–2019.
| Data Source: IQVIA National Prescription Audit (NPA) New to Brand. | ||||||||
|---|---|---|---|---|---|---|---|---|
| Annual ratesa | ||||||||
| 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | AAPCb | 95 % CI | |
| Total | 5.6 | 5.8 | 5.9 | 5.8 | 6.0 | 6.1 | 1.5 | (0.5, 2.5) |
| Females | 4.2 | 4.5 | 4.7 | 4.7 | 5.0 | 5.1 | 3.6 | (2.4, 4.8) |
| 0–9 | 4.2 | 3.9 | 3.7 | 3.5 | 3.4 | 3.2 | −4.9 | (−5.7, −4.1) |
| 10–19 | 12.2 | 12.5 | 12.2 | 11.6 | 12.1 | 11.9 | −0.9 | (−2.4, 0.6) |
| 20–39 | 4.8 | 5.3 | 6.0 | 6.2 | 6.5 | 6.8 | 7.2 | (4.6, 9.9) |
| 40–59 | 2.9 | 3.3 | 3.8 | 4.1 | 4.5 | 4.8 | 10.2 | (7.8, 12.7) |
| 60+ | 0.6 | 0.7 | 0.8 | 0.8 | 0.9 | 1.0 | 8.4 | (6.4, 10.4) |
| Males | 6.8 | 6.9 | 6.9 | 6.6 | 6.9 | 6.9 | 0.1 | (−1.0, 1.2) |
| 0–9 | 10.3 | 9.7 | 9.2 | 8.6 | 8.4 | 8.2 | −4.6 | (−5.8, −3.5) |
| 10–19 | 26.5 | 26.4 | 25.6 | 24.2 | 25.2 | 24.6 | −1.6 | (−3.1, −0.0) |
| 20–39 | 4.3 | 4.9 | 5.3 | 5.4 | 5.7 | 5.9 | 6.2 | (3.7, 8.8) |
| 40–59 | 1.9 | 2.1 | 2.4 | 2.5 | 2.7 | 2.9 | 8.9 | (6.9, 11.0) |
| 60+ | 0.5 | 0.6 | 0.6 | 0.6 | 0.6 | 0.7 | 4.7 | (2.9, 6.5) |
Bold typeface denotes statistical significance at P < 0.05.
Per 100 persons.
Average annual percent change in rates from 2014 to 2019; calculated using Joinpoint regression.
Stimulant dispensing rates varied substantially across states, ranging from 1.0 per 100 in Hawaii to 13.6 per 100 in Alabama in 2019 (Fig. 2, Supplemental Table 2). Many states saw increases in stimulant dispensing rates from 2018 to 2019, with the largest rate increases occurring in Rhode Island (8.2–9.4 per 100; P < 0.001), Vermont (10.5–11.6 per 100; P < 0.001), Massachusetts (7.5–8.6 per 100; P < 0.001), Virginia (5.7–6.8 per 100; P < 0.001), and Maine (10.4–11.4 per 100; P < 0.001) (Supplemental Table 2). Stimulant dispensing rates were three times higher in the South (7.6 per 100) than in the West (2.8 per 100) in 2019 (P < 0.001) (Supplemental Table 2).
Fig. 2.
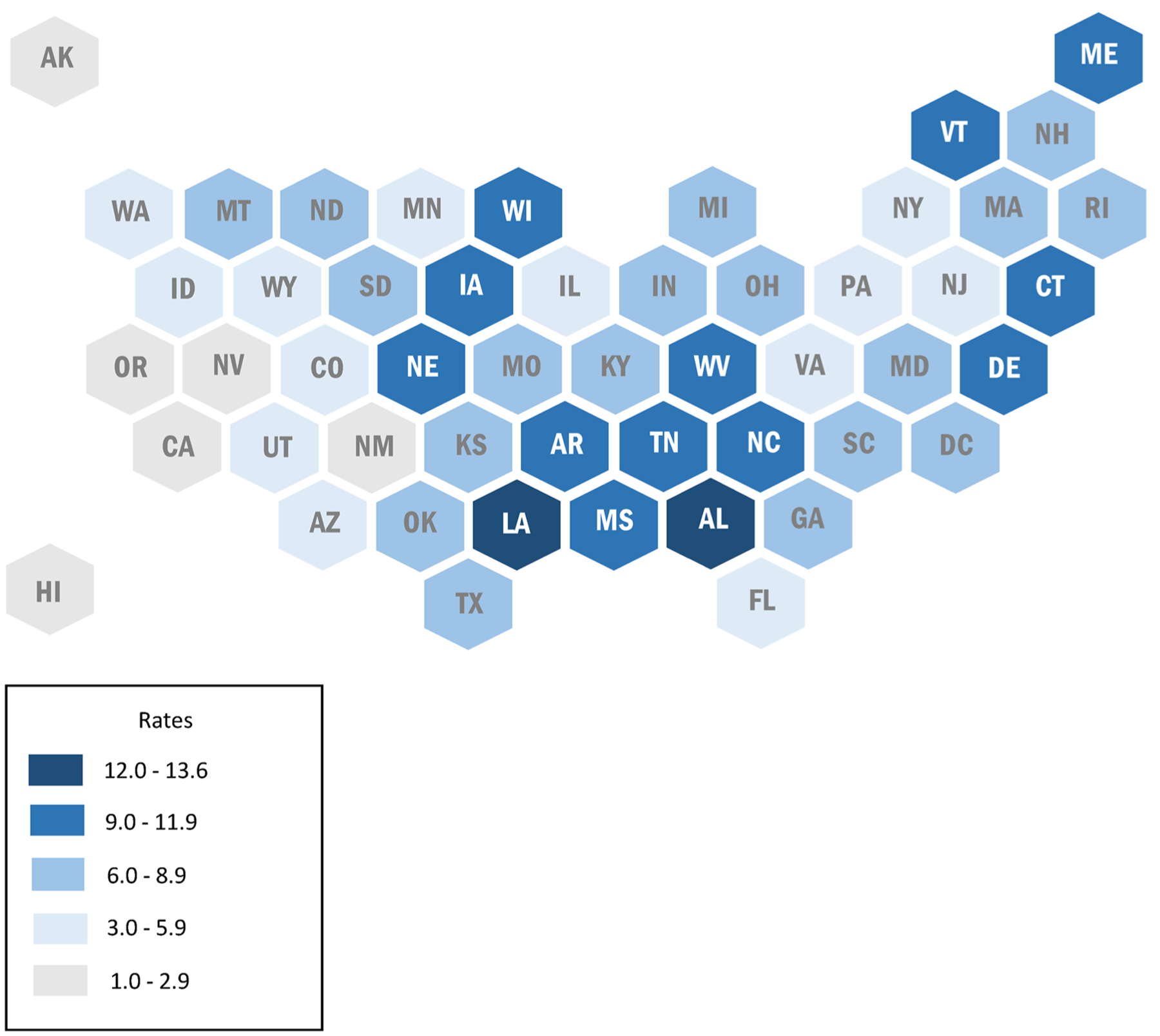
Stimulant dispensing rates per 100 persons by U.S. state, 2019.
Data Source: IQVIA National Prescription Audit (NPA) Regional.
The vast majority of stimulant medications dispensed in 2019 were paid for through commercial insurance (80.4 % in 2019), followed by Medicaid (17.2 % in 2019), Medicare Part D (1.6 % in 2019), and cash (0.8 % in 2019) (Table 3). Approximately 35 % of stimulant prescriptions dispensed had no copay, approximately one-fifth of prescriptions had copays between $25.01 and $50.00, and approximately 10 % had copays of greater than $50. Together, the three specialties of psychiatry, pediatrics, and primary care physicians accounted for 66.5 % of all controlled substance stimulants dispensed in 2019 (Table 3).
Table 3.
Controlled substance stimulant dispensing by payor, copay, and provider specialty – United States, 2019.
| Data source: IQVIA National Prescription Audit (NPA) Extended Insights. | ||
|---|---|---|
| 2019 | ||
| N | % | |
| Totala | 19,897,611 | 100.0 |
| Payor | ||
| Cash | 157,532 | 0.8 |
| Medicaid | 3,423,007 | 17.2 |
| Commercial | 15,996,704 | 80.4 |
| Medicare Part D | 314,919 | 1.6 |
| Patient Copay | ||
| $0.00 | 7,057,881 | 35.5 |
| $0.01 – $10.00 | 2,050,532 | 10.3 |
| $10.01 – $25.00 | 1,677,361 | 8.4 |
| $25.01 – $50.00 | 4,091,059 | 20.6 |
| $50.01 or higher | 3,506,560 | 17.6 |
| Copay unspecified | 1,514,218 | 7.6 |
| Prescriber Specialty | ||
| Addiction Medicine | 4,489 | <0.1 |
| Emergency Medicine | 19,252 | 0.1 |
| Medical Subspecialties | 95,472 | 0.5 |
| Nurse Practitioner | 3,252,714 | 16.3 |
| Obstetrics/Gynecology | 25,009 | 0.1 |
| Osteopathic Medicine | 1,500,198 | 7.5 |
| Other | 558,059 | 2.8 |
| Pain Medicine | 14,826 | 0.1 |
| Pediatrics | 4,512,312 | 22.7 |
| Physician Assistant | 812,218 | 4.1 |
| Primary Care | 3,562,654 | 17.9 |
| Psychiatry | 5,152,307 | 25.9 |
| Surgery | 16,915 | 0.1 |
Subcategories do not necessarily add up to the total amount due to missing data.
4. Discussion
We analyzed trends in controlled substance stimulant dispensing in the United States from 2014 to 2019. Overall, rates increased during the study period; however, trends varied by age group and sex. Among children aged 0–19 years, rates declined significantly or remained stable, whereas all adults aged ≥20 years experienced significant increases in stimulant dispensing rates. Significant increases were also observed among females, particularly females aged ≥20 years. In addition, we found that stimulant dispensing rates varied greatly by state and region. These trends have important implications for providers who prescribe stimulants, patients who use them, and public health practitioners and policymakers working to develop and implement policies, programs, and practices to prevent stimulant misuse and diversion. The wide variation in stimulant dispensing across state and region also carries implications for future research to identify the clinical, health system, and community factors that contribute to these variations.
A novel finding in our study was the seasonality effect in quarterly stimulant dispensing rates among children younger than 20 years; for children aged 0–9 years, stimulant dispensing rose sharply during the fourth quarter of each year, while for children aged 10–19 years, the lowest numbers of prescription stimulants were dispensed in the third quarter of each year. The pattern for adults did not show the same seasonal effect. It is possible that this reflects changes in prescription dispensing practices while children are out of school for the summer and then returning to the school year. Although prior research is limited, a seasonality effect in stimulant prescribing among children age 0–17 years has been previously documented, while adult prescriptions show no such effect and instead show overall increases across time (Cascade et al., 2008). This may indicate that medications for ADHD are being primarily used during the school year, and raises concerns around the need to re-acclimate to the medication and side effects associated with intermittent dosing (Cascade et al., 2008). Additional research to understand these patterns and the implications for treatment efficacy as well as misuse and diversion is needed.
The approximately doubled rates of controlled substance stimulant dispensing among males compared to females aged 10–19 years is consistent with ADHD diagnosis trends (Visser et al., 2014) and has been observed in other publications (Burcu et al., 2016). However, our analysis, which used nationally representative data from all payors as well as cash payments by patients, found a much higher prescription stimulant dispensing rate among 10–19 year-olds compared to previous research on stimulant dispensing among the commercially insured in Illinois, New Mexico, Oklahoma, and Texas (7.2 per 100 children aged 10–19 years in 2014 versus 19.5 per 100 children aged 10–19 in 2014 in our study) (Burcu et al., 2016). Nevertheless, it is reassuring that annual trends for children aged 0–9 showed significant declines in stimulant dispensing rates in our analysis, suggesting that providers are taking efforts to limit unnecessary prescribing in younger children.
Higher prevalence of stimulant use among women aged ≥35 years seen in our study has also been observed in previous studies (Burcu et al., 2016; Tseregounis et al., 2019). Additionally, consistent with increasing trends in our study among women aged 20–39 and 40–59 years, a recent report found that ADHD stimulant prescriptions filled increased 344 % from 2003 to 2015 among reproductive-aged women (15–44 years) who were privately insured (Anderson et al., 2018). Given these trends, providers working with reproductive-aged women using prescription stimulants should ensure patients are informed about any possible risks associated with use during pregnancy. ADHD has been historically under-diagnosed and under-treated among adults (Cascade et al., 2008), so the increases in dispensing patterns observed in our study could indicate rising awareness of this issue among patients and prescribers and improved access to needed treatment. With the publication of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) in 2013, the diagnostic criteria for ADHD was updated to include criteria for adults (American Psychiatric Association, 2013). Diagnostic criteria were also updated to reflect that ADHD symptoms must be present prior to age 12, rather than age 7 (American Psychiatric Association, 2013). As these changes coincided with the start date of our analysis period, it is likely that some of the increase observed in stimulant dispensing among adults reflects an increase in diagnoses for ADHD. For example, a study of a cohort of 30 year-olds in Brazil found a 31 % increase in adult ADHD prevalence (from 1.2 % to 2.1 %) when applying the DSM-5 criteria (Vitola et al., 2017). However, other researchers have reported that adults who are prescribed stimulants are less likely than youths to have a clinical diagnosis of ADHD, which could potentially reflect increasing off-label use among adults (Burcu et al., 2016).
There are concerns that increases in prescribing patterns may also play a role in increased prescription stimulant diversion and misuse. For example, in Australia, research found that increased stimulant poisonings were correlated with increased stimulant prescribing rates (Cairns et al., 2016). Some population groups, particularly college students, have experienced recent increases in past-year nonmedical prescription stimulant use that parallel increased trends in medical use (McCabe et al., 2014). Prescribers should be aware of changing stimulant misuse trends in their communities as well as the dispensing trends observed in our analysis when prescribing stimulants. In addition, prescribers can enhance patient education regarding appropriate indications for use, risks of misuse, use disorder, and overdose.
The finding that nearly half of all stimulant prescriptions dispensed in 2019 came from the provider specialties of pediatrics and psychiatry is expected given that ADHD is the primary disorder these medications are used to treat; however, it also highlights key medical specialties to target for enhanced patient and prescribing education. Although primary care physicians did not prescribe stimulants as often as pediatricians or psychiatrists, they did account for nearly 1 in 5 dispensed stimulant prescriptions in 2019. Stimulant prescribing by non-psychiatrists is increasing, as is the issuance of prescription stimulants for conditions other than ADHD (Safer, 2016). Thus, primary care physicians and other specialties such as nurse practitioners, osteopathic physicians, and physician assistants are important specialties to consider in targeting patient and prescribing education tools regarding appropriate use of stimulants and the potential risks of stimulant misuse and diversion. Future research is needed to understand more about how stimulant prescribing differs by provider specialty.
Providers can also make patients aware of the risks associated with diversion, how to keep products stored and disposed of safely, and the dangers of sharing or selling prescription stimulants to others. A systematic review found that stimulant diversion rates vary across populations, but can be as high as 80.0 % (Faraone et al., 2019), with men more than twice as likely as women to divert prescription stimulants (Aldridge et al., 2011). Given the recent finding that 80 % of persons reporting nonmedical prescription stimulant use obtained them from friends and relatives, and that 78.0 % of those friends and relatives obtained their prescriptions from one doctor (Han et al., 2017), enhanced patient education on the risks associated with prescription stimulant diversion is needed (Arria and DuPont, 2018; Clemow and Walker, 2014; Faraone et al., 2019). Patient education is also needed to counter misperceptions about cognitive benefits in the academic setting as a motivator for misuse, particularly among college students. Our analysis found increasing dispensing of amphetamine-type stimulants compared to methylphenidate-type stimulants consistent with current prescribing and use trends (Berman et al., 2009; Piper et al., 2018; Safer, 2016). Amphetamine-type stimulants have a higher potential for misuse in adults (Berman et al., 2009) and have been misused more often by college students in recent years (Teter et al., 2006). Providers should consider these factors and trends when making decisions about which types of products to prescribe to adolescents and young adults and provide appropriate education geared toward patients in academic settings.
In tandem with patient education, additional strategies to prevent stimulant misuse (i.e., using a prescription stimulant drug in any way not indicated by one’s doctor) (Substance Abuse and Mental Health Services Administration, 2019), prescription diversion, and stimulant use disorder include close monitoring of patients who have been prescribed a stimulant (including checking state prescription drug monitoring programs) and screening for substance misuse and substance use disorder prior to and during treatment with stimulants (Arria and DuPont, 2018; Clemow and Walker, 2014; Faraone et al., 2019; Han et al., 2017), as well as prescribing nonstimulant ADHD medications and using evidence-based non-pharmacology treatments in patients that are at risk of substance misuse and use disorder (Clemow and Walker, 2014; Faraone et al., 2019). It is particularly critical for providers to adopt these strategies in light of recent studies which have found associations between prescription stimulant misuse and other substance use disorders, including cocaine use disorder and prescription opioid use disorder (Compton et al., 2018; Han et al., 2017). Furthermore, persons who reported past-year methamphetamine use had higher odds of also reporting prescription stimulant misuse; 21.6 % of adults who reported past-year methamphetamine use also reported past-year prescription stimulant misuse (Jones et al., 2020). This overlap in prescription stimulant misuse and illicit drug use underlies the importance of expanded patient education, screenings, and other interventions described above for patients which are prescribed stimulant medications.
Our findings using U.S. population data are comparable to those observed in other countries. Data from the United Kingdom also show increasing trends in stimulant dispensing across time, with adolescent males receiving these prescriptions at nearly five times that of adolescent females (Renoux et al., 2016). Data from France indicates that prescription stimulant dispensing occurs more frequently among adults aged 25–49 years compared to other age groups and that this population may be more likely to engage in misuse (Pauly et al., 2018). University students in Australia have also reported prescription stimulant diversion and misuse, although rates may be lower than what has been reported in the U.S. (Lucke et al., 2018). However, some trends observed in this study may be unique to the United States. For example, the seasonality trends observed in this study may not apply to children in other countries, or may follow different seasonal patterns in line with local school schedules. Additionally, while much attention has been given to stimulant overprescribing in children in the U.S., children who represent minority populations may be subject to under prescribing; a recent study found that Aboriginal children in Australia were one-third to two-thirds less likely to have prescription stimulants than their non-Aboriginal counterparts (Ghosh et al., 2015).
This analysis is subject to several limitations. First, we did not have access to more granular data, including race/ethnicity, urbanicity, and average annual income to explore other sociodemographic factors that may influence controlled substance stimulant dispensing. Second, we were unable to link and compare these data with other data sources such as the National Survey on Drug Use and Health to explore whether there is a direct relationship between increased prescription stimulant dispensing and stimulant diversion and misuse in certain population groups. Third, data on dosage and duration were not available for analysis. Fourth, information was not available on prescriptions that were written but not filled or whether the prescription was actually used by the intended recipient. Fifth, we could not capture diversion as a result of obtaining stimulants without a prescription or via forged prescriptions or under false pretenses. Sixth, we were unable to determine the appropriateness of the prescription relative to the medical condition, and severity could not be determined. The dataset did not include information on patient diagnoses, so we could not distinguish whether our observed trends were related to stimulants prescribed for ADHD compared to other conditions. Seventh, 2019 population data by age and gender were unavailable, so 2018 population estimates were used instead. Because these population denominators were so large, we do not expect this to substantially change our findings. Finally, our data were already categorized into specific age groups, and therefore we could not examine certain age categorizations of interest for further examination of trends (e.g., 18–25 year-olds, or college-age students).
National controlled substance stimulant dispensing rates increased from 2014 to 2019, driven by notable increases among females and adults aged ≥20 years. Dispensing rates also varied substantially across states, ranging from 1.0 prescriptions per 100 persons in Hawaii to 13.6 per 100 persons in Alabama in 2019, and across U.S. Census regions. These trends should be considered when prescribing stimulants given growing concerns over prescription stimulant diversion, misuse, and related health harms. Strategies that prescribers can employ that may reduce the risk of prescription stimulant misuse and diversion include close monitoring of patients who have been prescribed a stimulant, checking state prescription drug monitoring programs, and screening for substance misuse and use disorder, prescribing nonstimulant ADHD medications and using evidence-based non-pharmacological treatments when appropriate, and educating patients about the risks and dangers of diversion and misuse.
Supplementary Material
Role of funding source
Nothing declared. This analysis did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Declaration of Competing Interest
The authors have no conflicts of interest to declare.
Appendix A. Supplementary data
Supplementary material related to this article can be found, in the online version, at doi: https://doi.org/10.1016/j.drugalcdep.2020.108297.
References
- Aldridge AP, Kroutil LA, Cowell AJ, Reeves DB, Van Brunt DL, 2011. Medication costs to private insurers of diversion of medications for attention-deficit hyperactivity disorder. PharmacoEcon. 29 (7), 621–635. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association, 2013. Attention deficit/hyperactivity disorder. https://www.psychiatry.org/psychiatrists/practice/dsm/educational-resources/dsm-5-fact-sheets. (Accessed September 2, 2020).
- Anderson KN, Ailes EC, Danielson M, Lind JN, Farr SL, Broussard CS, Tinker SC, 2018. Attention-deficit/hyperactivity disorder medication prescription claims among privately insured women aged 15–44 years - United States, 2003–2015. MMWR Morb. Mortal. Wkly. Rep 67 (2), 66–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arria AM, DuPont RL, 2018. Prescription stimulant use and misuse: implications for responsible prescribing practices. Am. J. Psychiatry 175 (8), 707–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benson K, Flory K, Humphreys KL, Lee SS, 2015. Misuse of stimulant medication among college students: a comprehensive review and meta-analysis. Clin. Child Fam. Psychol. Rev 18 (1), 50–76. [DOI] [PubMed] [Google Scholar]
- Berman SM, Kuczenski R, McCracken JT, London ED, 2009. Potential adverse effects of amphetamine treatment on brain and behavior: a review. Mol. Psychiatry 14 (2), 123–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burcu M, Zito JM, Metcalfe L, Underwood H, Safer DJ, 2016. Trends in stimulant medication use in commercially insured youths and adults, 2010–2014. JAMA Psychiatry 73 (9), 992–993. [DOI] [PubMed] [Google Scholar]
- Cairns R, Daniels B, Wood DA, Brett J, 2016. ADHD medication overdose and misuse: the NSW Poisons Information Centre experience, 2004–2014. Med. J. Aust 204 (4), 154. [DOI] [PubMed] [Google Scholar]
- Cascade E, Kalali AH, Weisler RH, Lenderts S, 2008. Seasonality and the changing adult/child prescription ratios in ADHD therapy. Psychiatry (Edgmont) 5 (1), 23–25. [PMC free article] [PubMed] [Google Scholar]
- Clemow DB, Walker DJ, 2014. The potential for misuse and abuse of medications in ADHD: a review. Postgrad. Med 126 (5), 64–81. [DOI] [PubMed] [Google Scholar]
- Compton WM, Han B, Blanco C, Johnson K, Jones CM, 2018. Prevalence and correlates of prescription stimulant use, misuse, use disorders, and motivations for misuse among adults in the United States. Am. J. Psychiatry 175 (8), 741–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtin K, Fleckenstein AE, Keeshin BR, Yurgelun-Todd DA, Renshaw PF, Smith KR, Hanson GR, 2018. Increased risk of diseases of the basal ganglia and cerebellum in patients with a history of attention-deficit/hyperactivity disorder. Neuropsychopharmacol 43, 2548–2555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danielson ML, Bitsko RH, Ghandour RM, Holbrook JR, Kogan MD, Blumberg SJ, 2018. Prevalence of parent-reported ADHD diagnosis and associated treatment among U.S. children and adolescents, 2016. J. Clin. Child Adolesc. Psychol 47 (2), 199–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein-Ngo QM, McCabe SE, Veliz PT, Stoddard SA, Austic EA, Boyd CJ, 2016. Diversion of ADHD stimulants and victimization among adolescents. J. Pediatr. Psychol 41 (7), 786–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraone SV, Rostain AL, Montano CB, Mason O, Antshel KM, Newcorn JH, 2019. Systematic review: nonmedical use of prescription stimulants: risk factors, outcomes, and risk reduction strategies. J. Am. Acad. Child Adolesc. Psychiatry 59 (1), 100–112. [DOI] [PubMed] [Google Scholar]
- Ghosh M, Holman CD, Preen DB, 2015. Use of prescription stimulant for attention deficit hyperactivity disorder in aboriginal children and adolescents: a linked data cohort study. BMC Pharmacol. Toxicol 16, 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B, Jones CM, Blanco C, Compton WM, 2017. National trends in and correlates of nonmedical use of prescription stimulants, nonmedical use frequency, and use disorders. J. Clin. Psychiatry 78 (9), e1250–e1258. [DOI] [PubMed] [Google Scholar]
- Jones CM, Compton WM, Mustaquim D, 2020. Patterns and characteristics of methamphetamine use among adults - United States, 2015–2018. MMWR Morb. Mortal. Wkly. Rep 69 (12), 317–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, Faraone SV, Greenhill LL, Howes MJ, Secnik K, Spencer T, Ustun TB, Walters EE, Zaslavsky AM, 2006. The prevalence and correlates of adult ADHD in the United States: results from the national comorbidity survey replication. Am. J. Psychiatry 163 (4), 716–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HJ, Fay MP, Feuer EJ, Midthune DN, 2000. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med 19 (3), 335–351. [DOI] [PubMed] [Google Scholar]
- Lasopa SO, Striley CW, Cottler LB, 2015. Diversion of prescription stimulant drugs among 10–18-year-olds. Curr. Opin. Psychiatry 28 (4), 292–298. [DOI] [PubMed] [Google Scholar]
- Lucke J, Jensen C, Dunn M, Chan G, Forlini C, Kaye S, Partridge B, Farrell M, Racine E, Hall W, 2018. Non-medical prescription stimulant use to improve academic performance among Australian university students: prevalence and correlates of use. BMC Public Health 18 (1), 1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, Teter CJ, Boyd CJ, 2014. Trends in medical use, diversion, and nonmedical use of prescription medications among college students from 2003 to 2013: connecting the dots. Addict. Behav 39 (7), 1176–1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Veliz P, Wilens TE, Schulenberg JE, 2017. Adolescents’ prescription stimulant use and adult functional outcomes: a national prospective study. J. Am. Acad. Child Adolesc. Psychiatry 56 (3), 226–233 e224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pauly V, Frauger E, Lepelley M, Mallaret M, Boucherie Q, Micallef J, 2018. Patterns and profiles of methylphenidate use both in children and adults. Br. J. Clin. Pharmacol 84 (6), 1215–1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper BJ, Ogden CL, Simoyan OM, Chung DY, Caggiano JF, Nichols SD, McCall KL, 2018. Trends in use of prescription stimulants in the United States and Territories, 2006 to 2016. PLoS One 13 (11), e0206100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renoux C, Shin JY, Dell’Aniello S, Fergusson E, Suissa S, 2016. Prescribing trends of attention-deficit hyperactivity disorder (ADHD) medications in UK primary care, 1995–2015. Br. J. Clin. Pharmacol 82 (3), 858–868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safer DJ, 2016. Recent trends in stimulant usage. J. Atten. Disord 20 (6), 471–477. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2019. Key substance use and mental health indicators in the United States: results from the 2018 National Survey on Drug Use and Health. Rockville, MD: https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHNationalFindingsReport2018/NSDUHNationalFindingsReport2018.pdf. (Accessed April 4, 2020). [Google Scholar]
- Teter CJ, McCabe SE, LaGrange K, Cranford JA, Boyd CJ, 2006. Illicit use of specific prescription stimulants among college students: prevalence, motives, and routes of administration. Pharmacotherapy 26 (10), 1501–1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tseregounis IE, Stewart SL, Crawford A, Marshall BDL, Cerda M, Shev AB, Henry SG, 2019. Age- and sex-specific increases in stimulant prescribing rates-California, 2008–2017. J. Atten. Disord, 1087054719883008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau, 2020. U.S. Census Bureau (Accessed April 4, 2020). https://www.census.gov/programs-surveys/popest/data/tables.All.html.
- U.S. Department of Justice Drug Enforcement Administration, 2020. Controlled Substance Schedules (Accessed April 4, 2020). https://www.deadiversion.usdoj.gov/schedules/.
- U.S. National Library of Medicine, 2020a. Adderall (Accessed April 4, 2020). https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=f22635fe-821d-4cde-aa12-419f8b53db81.
- U.S. National Library of Medicine, 2020b. Amphetamine Sulfate (Accessed April 4, 2020). https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=79b9db39-7cdc-5607-f0ce-ac2a2cfd59d5.
- Visser SN, Danielson ML, Bitsko RH, Holbrook JR, Kogan MD, Ghandour RM, Perou R, Blumberg SJ, 2014. Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011. J. Am. Acad. Child Adolesc. Psychiatry 53 (1), 34–46 e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitola ES, Bau CH, Salum GA, Horta BL, Quevedo L, Barros FC, Pinheiro RT, Kieling C, Rohde LA, Grevet EH, 2017. Exploring DSM-5 ADHD criteria beyond young adulthood: phenomenology, psychometric properties and prevalence in a large three-decade birth cohort. Psychol. Med 47 (4), 744–754. [DOI] [PubMed] [Google Scholar]
- Zuvekas SH, Vitiello B, 2012. Stimulant medication use in children: a 12-year perspective. Am. J. Psychiatry 169 (2), 160–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


