Abstract
Purpose
We investigated occupational dose to the lens of the eye for CT-assisting personnel for diagnostic purposes using a radio-photoluminescent glass dosimeter (RPLD) and evaluate compliance with the new equivalent dose limit for the lens of the eye (20 mSv/year). Further, we proposed the implementation of “multiple protective measures” and estimated its effect.
Method
An eye lens dosimeter clip was developed specifically to attach RPLDs inside radiation safety glasses in an L-shape. Using a total of six RPLDs attached to the radiation safety glasses, the 3-mm dose-equivalent (Hp(3)) to the lens of the eye for medical staff (n = 11; 6 intensive care physicians, 2 pediatricians, 3 radiological technologists) who assisted patients during CT scan for “diagnostic” purpose (n = 91) was measured. We evaluated the dose reduction efficiencies with radiation safety glasses and bag-valve-mask extension tube. We also estimated the protection efficiency with radiation protection curtain introduced in front of the staff's face via the phantom experiment.
Results
Without wearing radiation safety glasses, Hp(3) to the lens of the eye was greatest for intensive care physicians (0.49 mSv/procedure; allowing 40 procedures to be performed annually), followed by pediatricians (0.30 mSv/procedure; 66 procedures annually) and radiological technologists (0.28 mSv/procedure; 71 procedures annually). Use of each type of protective tools: radiation safety glasses (0.07-mm-Pb), bag-valve-mask extension tube (20 cm) and radiation protective curtain (0.25-mm-Pb), reduced Hp(3) to the lens of the eye by 51%, 31% and 61%, respectively.
Conclusion
Intensive care physicians perform most assisted ventilations with the bag-valve-mask during “diagnostic” CT scans, and may exceed the equivalent dose limit for the lens of the eye if radiation safety glasses are not worn. If “multiple protective measures” are implemented, compliance with the equivalent dose limit for the lens of the eye should be achievable without placing significant burdens on physicians or medical institutions.
Keywords: Occupational dose to the lens of the eye, CT-assisting personnel for diagnostic CT scan, Radio-photoluminescent glass dosimeter, Multiple protective measures, Industrial health management
Occupational dose to the lens of the eye; CT-assisting personnel for diagnostic CT scan; Radio-photoluminescent glass dosimeter; Multiple protective measures; Industrial health management
1. Introduction
The threshold dose for radiation-induced cataract has been thought to be 5 Gy for acute exposure and 8 Gy for hyperfractionated or prolonged exposure [1]. However, numerous epidemiological studies have shown that the threshold dose may significantly decrease [2, 3, 4]. The International Commission on Radiological Protection (ICRP) in 2011 in the Seoul Statement therefore lowered the threshold dose of cataract to 0.5 Gy and recommended a new equivalent dose limit for the lens of the eye, to specify occupational exposure in planned exposure situations, “For occupational exposure in planned exposure situations the Commission now recommends an equivalent dose limit for the lens of the eye of 20 mSv in a year, averaged over defined periods of 5 years, with no single year exceeding 50 mSv” [5]. Since this recommendation, increased interest has been shown in cataracts and occupational dose to the lens of the eye for medical staff in Japan.
Many reports have shown that occupational dose to the lens of the eye is significant among physicians involved in clinical radiation care over many hours, such as interventional radiology (IR) of the neurovascular system [6, 7, 8, 9], cardiovascular system [8, 10] or tumor [8, 9, 11], and endoscopic retrograde cholangiopancreatography (ERCP) [8, 12, 13, 14]. The risk of radiation-induced cataracts is widely recognized. However, relatively little is known about occupational doses to the lens of the eye in CT-assisting personnel. CT has become commonly used in recent years for “treatment” purposes, such as tissue biopsy and drainage. Several reports have examined occupational dose to the lens of the eye in physicians performing these procedures [15, 16, 17, 18, 19, 20, 21, 22, 23] (Table 1), and special protective equipment and their effects in dose reduction [22, 24, 25, 26]. However, while reports have already investigated nurses assisting pediatric patients in the CT room during CT scans for “diagnostic” purposes [27] or in phantom experiments [28, 29], no reports have described direct measurement in medical staff assisting adult patients undergoing high-dose imaging procedures.
Table 1.
Occupational dose to the lens of the eye during CT fluoroscopy for “treatment” purposes: literature review.
| Author (year of publication) [reference number] | Measurement target | Type of dosimeter | Measurement position | Dose |
|---|---|---|---|---|
| Silverman et al. (1999) [15] | Phantom | Ionization chamber | Neck | 2.6 μC/kg (10 mR) (scattered X-ray 100 cm from the beam) |
| Daly et al. (1999) [16] | Operator | Film badge | Outside protective apron (neck) | 0.1–0.3 mSv/month |
| Mellenberg et al. (1999) [17] | Phantom | Ionization chamber | Outside protective apron (collar) | 0.24 ± 0.14 mR/sec |
| Outside protective apron (body) | 1.13 ± 0.49 mR/sec | |||
| Paulson et al. (2001) [18] | Operator | OSLD | Outside protective apron (Lens of the eye) | 0.007–0.048 mSv/procedure |
| Joemai et al. (2009) [19] | Operator | EPD Mk II | Outside protective apron | IR: 14 μSv/procedure |
| AR: 5 μSv/procedure | ||||
| RT: 1 μSv/procedure | ||||
| Heusch et al. (2014) [20] | Operator | EDD-30 | Side of protective glasses | 3.3 μSv/procedure (range, 0.03–218.9 μSv/procedure) |
| Gyekye et al. (2016) [21] | Phantom | MCNPX | Eye | 4.5 ± 1.3 μGy/procedure (with protective equipment) |
| 4.8 ± 1.3 μGy/procedure (without protective equipment) | ||||
| Sarmento et al. (2018) [22] | Operator | TLD | Outside protective apron (body) | 0.06 mSv/procedure |
| Pravata et al. (2018) [23] | Operator | EDD-30 | Outside protective apron (body) | 8.2 μGy/procedure (DLP: 124 mGy・cm) |
OSLD, optically stimulated luminescence dosimeter.
EPD MkII, electronic personal dosimeter (Siemens Environmental Systems, Munich, Germany).
EDD-30, educational direct dosimeter (Unfors Instruments, Billdal, Sweden).
MCNPX, Monte Carlo N-Particle eXtended.
IR, interventional radiologist.
AR, assisting radiologist.
RT, radiologic technologist.
In this study, our first objective was to develop a dosimeter that can measure the occupational dose to the lens of the eye for CT-assisting personnel in a single procedure using a radio-photoluminescent glass dosimeter (RPLD) (GD-352M; Chiyoda Technol Co., Tokyo, Japan). Our second objective was to investigate occupational dose to the lens of the eye for CT-assisting personnel during “diagnostic” CT using this dosimeter, and to evaluate compliance with the new equivalent dose limit for the lens of the eye. Finally, our third objective was to propose implementation of “multiple protective measures” that do not physically burden the CT-assisting personnel, especially intensive care physicians, and do not financially burden the medical institution through superfluous radiation protective measures, and to estimate the effects of this proposal.
2. Material and methods
2.1. Participants for occupational dose measurement
The 3-mm dose-equivalent (Hp(3)) inside and outside the radiation safety glasses was measured for 11 medical staff as an assessment of the equivalent dose to the lens of the eye. A total of 91 “diagnostic” CT scans that needed special assistance for a patient in the CT room performed at our hospital between June 2017 and May 2018 were analyzed (Table 2).
Table 2.
Patient information by site of CT scans for diagnostic purpose (n = 91 procedures, June 2017–May 2018).
| CT imaging site | n | Age [y] |
Body weight [kg] |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Head | 35 | 41.9 ± 32.7 | 40.4 ± 24.7 |
| Head, neck | 3 | 78.3 ± 1.9 | 54.4 ± 1.9 |
| Chest | 5 | 33.6 ± 25.6 | 46.4 ± 22.6 |
| Chest to abdomen | 22 | 70.5 ± 15.1 | 56.5 ± 9.4 |
| Abdomen | 4 | 55.5 ± 33.0 | 55.5 ± 16.8 |
| Head, chest | 4 | 57.0 ± 16.5 | 62.2 ± 11.0 |
| Head, Chest to abdomen | 14 | 63.9 ± 21.1 | 60.5 ± 7.8 |
| CTA | 4 | 76.3 ± 4.5 | 62.7 ± 5.9 |
CTA, computed tomography angiography.
SD, standard deviation.
2.2. CT imaging method and CT dose index
Multi-slice CT systems (Aquilion ONE or Aquilion PRIME; Canon Medical Systems, Nasu, Japan) were used in this study. For image generation, auto-exposure control, and iterative reconstruction were applied. For optimization of the imaging dose, from the 1,203 CT imaging cases at our hospital seen between January 1 and June 30, 2018, median values for CTDIvol and DLP per major site were individually determined and compared with the Japan Diagnostic Reference Levels for 2015 (Japan DRLs 2015) [30].
2.3. Method for measuring occupational dose to the lens of the eye
CT-assisting personnel wore radiation protective clothing (MSA-25L, 0.25-mm-Pb; Maeda Co., Tokyo, Japan) and radiation safety glasses (Panorama shield ® ultra-light 0.07-mm-Pb; Toray, Tokyo, Japan), and the Hp(3) to the lens of the eye was obtained from the air kerma value measured by GD-352M (Figure 1) affixed inside and outside the radiation safety glasses. GD-352M complies with the IEC62387 requirements to the dosimetry system with passive detectors, offering stable dose linearity from a low dose range (not more than ± 5.0% within a range from 0.01 mGy to 50 mGy) [31, 32]. We confirmed that the coefficient of variation did not exceed 3.0% before commencing this study.
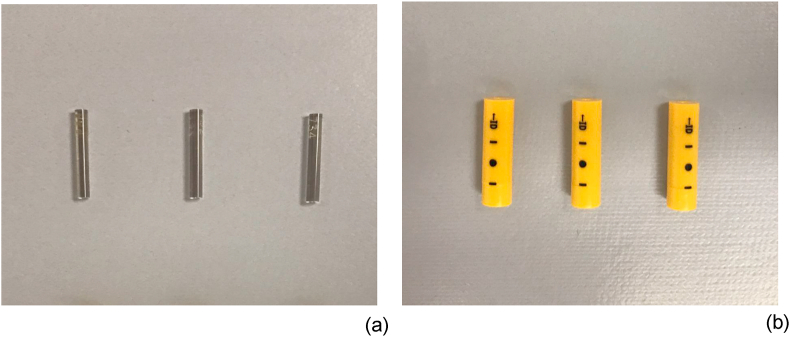
Figure 1.
Radio-photoluminescent glass dosimeter (GD-352M). (a) The dosimeter tip is cylindrical, measuring 1.5 mm in diameter and 12.0 mm in length. (b) The tip is used in a plastic case laminated with a 0.75-mm Sn filter.
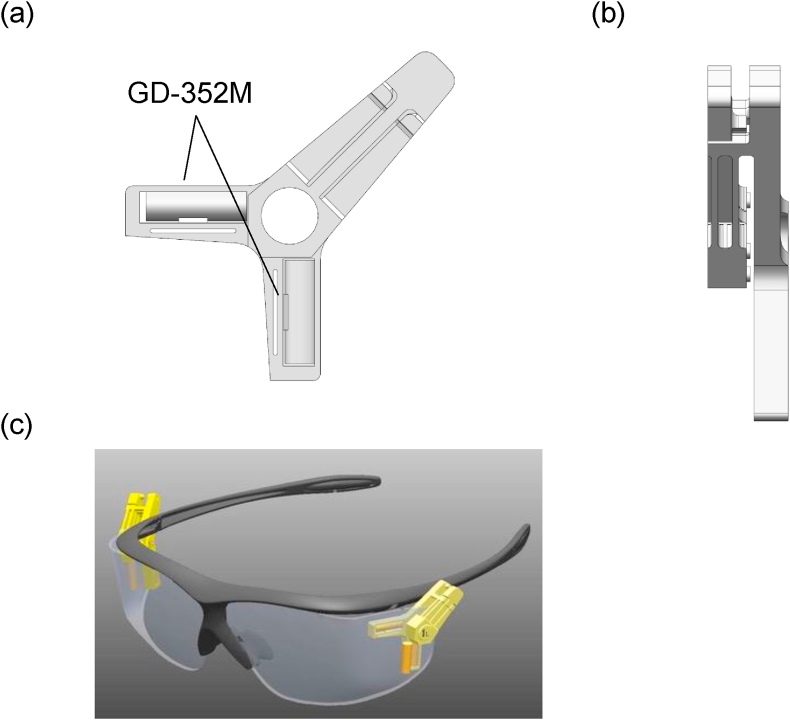
The GD-352M, to compensate for excessive energy response due to the high effective atomic number of the detector material, contains a Sn filter to absorb low-energy photon. However, because using this Sn filter creates a directional dependence of sensitivity [31], an eye lens dosimeter clip made with polyphenylene sulfide resin was manufactured such that two GD-352M RPLDs were placed in an L-shape, vertically and horizontally in relation to the ground, thereby offsetting the directional dependence and having the GD-352M does not hamper the user as well (Figure 2a, b). Using this eye lens dosimeter clip, a total of six GD-352M were attached to the inside and outside of the radiation safety glasses (Figure 2c).
Figure 2.
Diagram of the eye lens dosimeter clip. A polyphenylene sulfide resin clip was shaped such that the long axes of the two GD-352M were fixed perpendicular to each other inside the radiation safety glasses. (a) Anteroposterior view and (b) lateral view of the eye lens dosimeter clip. (c) Two eye lens dosimeter clips (left and right sides) were attached to the inside of the radiation safety glasses, and two GD-352M (left and right sides) were attached to the outside of the radiation safety glasses.
Imaging settings of the CT (tube voltage, tube current), CT dose indices CTDIvol and DLP, position of the CT-assisting personnel, method of assistance, and method of radiation protection were recorded per CT scan.
2.4. Conversion of Hp(3) to the lens of the eye from air kerma value obtained from RPLD
X-ray tube position of the CT scanner was fixed at 0° and tube voltage was set at 120 kVp. Using the wireless X-ray output analyzer (Piranha Model 657; RTI, Mölndal, Sweden) placed at the isocenter of the CT gantry, the aluminum half-value layer (Al-HVL) was measured. Next, the X-ray spectrum was calculated using an approximate expression by Tucker et al. [33], and the effective energy was determined from the obtained Al-HVL using the interaction cross-section data of photons and matter by Hubbell et al. [34]. Mean effective energy was set as 56.47 keV (Table 3). Finally, the “air kerma to 3-mm dose-equivalent conversion coefficient K (Hp(3)/air kerma),” which corresponds to the mean effective energy, was taken from previous reports [35]. Conversion coefficient K was determined to be 1.650.
Table 3.
X-ray effective energy during CT scan at a tube voltage of 120 kVp.
| CT equipment | FOV | Effective energy [keV] |
|---|---|---|
| 80-MDCT | S-size (24 cm) | 55.74 |
| L-size (40 cm) | 57.97 | |
| 320-MDCT | S-size (24 cm) | 54.87 |
| L-size (40 cm) | 57.30 | |
| Mean ± SD | 56.47 ± 1.23 | |
FOV, field of view.
80-MDCT, 80 multidetector-row CT.
320-MDCT, 320 multidetector-row CT.
SD, standard deviation.
2.5. Analysis of the reduction in occupational dose to the lens of the eye with radiation protective equipment
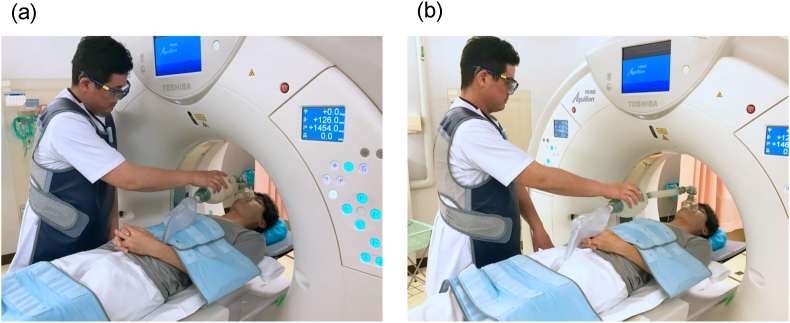
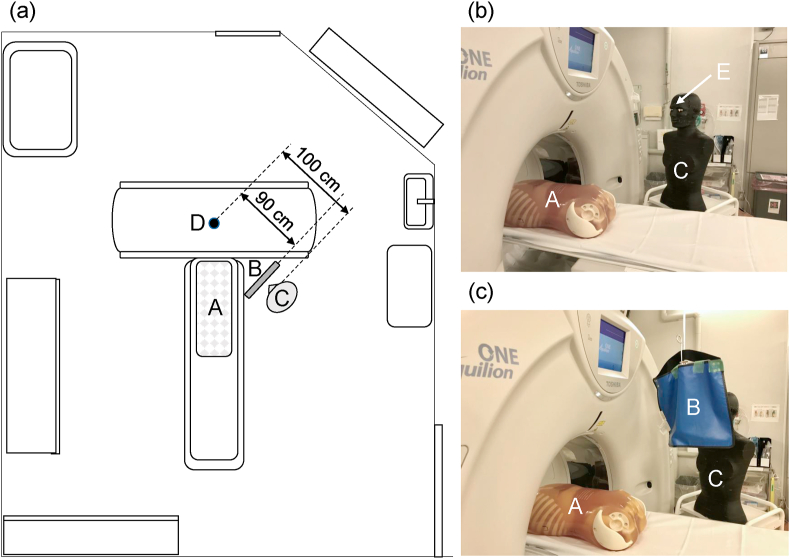
From the Hp(3) dose ratio of outside to inside the radiation safety glasses (outside/inside) measured for CT-assisting personnel, the dose reduction efficiency with radiation safety glasses was determined. After each Hp(3) was normalized to the corresponding DLP, the dose reduction efficiency with the bag-valve-mask extension tube was determined from the median dose ratio using the bag-valve-mask extension tube compared to not using the extension tube (with/without) (Figure 3). Furthermore, using a CT scanner at 120 kVp of tube voltage, the dose reduction efficiency with the radiation protective curtain was experimentally determined. A radiation protective curtain (39 × 43 cm, 0.25-mm Pb-equivalent thickness) was installed at the position 10 cm away from the face of the phantom (Alderson RANDO phantom, Radiology Support Device Inc., California, US) and the Hp(3) was analyzed with the GD-352M that had been affixed at the forehead of the phantom. The height of GD-352M was adjusted at 160 cm from the ground the eye level of the average Japanese male (Figure 4).
Figure 3.
Use of a bag-valve-mask extension tube (approximately 20 cm). (a) Without extension tube. (b) With extension tube.
Figure 4.
Experiment setting for obtaining dose reduction efficiency with the radiation-protective curtain. (a) Geometry arrangement for measurements. (b) Without radiation protective curtain. (c)With radiation protective curtain. A: Body phantom instead of patient (PBU-60, Kyoto Kagaku Co., Kyoto, Japan). B: Radiation protective curtain (39 × 43 cm, 0.25-mm Pb-equivalent thickness, 90 cm from the CT isocenter, with the upper edge of the curtain at a height of 185 cm from the ground). C: Body phantom instead of CT-assisting personnel (Alderson RANDO phantom). D: Isocenter of CT gantry. E: GD-352M affixed at the forehead of the phantom (100 cm from the CT isocenter, at a height of 160 cm from the ground).
2.6. Statistics
Occupational doses, CT imaging settings, and CT dose indices were compared between different standing positions of the assisting personnel and between professions of the personnel using Kruskal-Wallis one-way analysis of variance (ANOVA). When statistical significance was observed with one-way ANOVA, the difference between standing positions of each CT-assisting personnel and between professions of these personnel was evaluated using Dunn's test (with Bonferroni correction). Values of P < 0.05 were considered statistically significant.
2.7. Ethics
This study was approved by the ethics committee at our university (approval number: R1-054) and was conducted in compliance with the tenets of the Declaration of Helsinki.
3. Results
3.1. Optimization of CT settings
Comparing the CT dose index at our hospital with the Japan DRLs 2015, nearly all CT dose indices (median) were lower than the Japan DRLs 2015, demonstrating sufficient optimization (Table 4).
Table 4.
Comparison between CT dose indices at our hospital (n = 1,203 procedures, January 1− June 30, 2018) and diagnostic reference levels.
| Examinations | n | Body weight [kg] |
CTDIvol [mGy] |
DLP [mGy·cm] |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Median [range] | 25th−75th percentiles | Japan DRLs∗ | Mean ± SD | Median [range] | 25th−75th percentiles | Japan DRLs∗ | ||
|
Adult | ||||||||||
| Routine brain | 219 | 56.1 ± 13 | 54.7 ± 14.4 | 52.8 [32.4–136.3] | 47.1–58.4 | 85 | 936.3 ± 277.3 | 865.1 [528.7–2319.8] | 775.1–1,000.4 | 1,350 |
| Routine chest | 294 | 56.6 ± 12.7 | 11.1 ± 4.1 | 10.6 [3.8–34.4] | 8.4–13.2 | 15 | 414.5 ± 137.1 | 405.2 [138.3–1205.0] | 318.4–491.6 | 550 |
| Chest to pelvis | 234 | 57.1 ± 12.6 | 13.4 ± 5.1 | 12.3 [5.7–29.5] | 9.8–16.0 | 18 | 967.1 ± 389.0 | 894.7 [392.2–2252.2] | 691.0–1,157.0 | 1,300 |
| Abdomen to pelvis | 82 | 54.9 ± 11.6 | 18.6 ± 8.9 | 17.8 [7.4–50.3] | 10.4–24.5 | 20 | 898.3 ± 400.2 | 876.9 [349.1–1934.4] | 507.3–1,196.0 | 1,000 |
| Liver, multi-phase | 54 | 59.8 ± 12.0 | 18.5 ± 5.1 | 18.4 [8.3–32.1] | 15.2–21.7 | 15 | 2,254.1 ± 728.8 | 2,196.6 [991.5–3891.4] | 1,767.2–2,507.9 | 1,800 |
| Coronary CTA | 50 | 61.5 ± 13.6 | 68.0 ± 33.3 | 64.5 [10.6–191.8] | 47.2–91.4 | 90 | 1,411.4 ± 614.9 | 1,356.8 [400.6–4537.8] | 400.6–1,691.7 | 1,400 |
|
Child (age, years) | ||||||||||
| Head (0) | 47 | 3.9 ± 2.4 | 21.6 ± 9.3 | 20.2 [1.3–47.0] | 14.9–26.5 | 38 | 394.7 ± 198.4 | 379.1 [21.5–1,011.4] | 246.4–464.2 | 500 |
| Head (1–5) | 58 | 12.8 ± 5.4 | 32.0 ± 10.8 | 30.1 [9.1–82.2] | 24.7–40.9 | 47 | 684.7 ± 256.7 | 669.6 [300.6–2,316.4] | 520.0–832.7 | 660 |
| Head (6–10) | 47 | 23.1 ± 7.2 | 40.1 ± 13.6 | 36.9 [20.3–95.2] | 32.9–44.8 | 60 | 799.5 ± 243.3 | 763.5 [361.0–1,498.0] | 667.2–924.8 | 850 |
| Chest (0) | 18 | 3.5 ± 0.9 | 6.5 ± 2.9 | 6.5 [2.2–11.1] | 4.6–8.5 | 11 | 121.6 ± 79.5 | 110.6 [26.9–348.8] | 57.8–151.6 | 210 |
| Chest (1–5) | 25 | 13.2 ± 3.8 | 7.9 ± 5.3 | 5.1 [2.7–23.0] | 4.6–9.5 | 14 | 209.7 ± 151.6 | 174.2 [68.6–646.2] | 82.4–230.7 | 300 |
| Chest (6–10) | 19 | 19.1 ± 5.2 | 9.7 ± 5.5 | 8.8 [3.3–21.5] | 5.1–12.8 | 15 | 275.0 ± 159.3 | 212.7 [86.8–629.8] | 136.5–408.6 | 410 |
| Abdomen (0) | 17 | 5.1 ± 2.7 | 5.7 ± 3.1 | 5.3 [1.1–11.1] | 4.2–8.4 | 11 | 137.3 ± 87.8 | 104.1 [23.5–300.0] | 62.2–207.0 | 220 |
| Abdomen (1–5) | 19 | 13.8 ± 2.4 | 9.8 ± 3.7 | 9.5 [4.2–17.9] | 8.1–10.8 | 16 | 313.5 ± 122.7 | 311.7 [96.0–602.7] | 217.1–363.9 | 400 |
| Abdomen (6–10) | 20 | 22.7 ± 5.3 | 8.8 ± 4.6 | 6.7 [4.1–19.0] | 5.5–14.0 | 17 | 337.5 ± 154.7 | 250.1 [166.5–611.4] | 237.4–550.3 | 530 |
CTDIvol, computed tomography dose index (volume).
CTA, computed tomography angiography.
DLP, dose-length product.
DRLs, diagnostic reference levels.
Japan Diagnostic Reference Levels 2015 (Japan DRLs 2015).
3.2. Directional dependence of GD-352M in radiation sensitivity
Analysis of the dose ratio (vertical/horizontal) of the two GD-352M positioned orthogonally in vertical and horizontal directions relative to the ground showed that the vertical-to-horizontal dose ratio was virtually 1.0 for both left and right sides (Table 5). As the directional dependence of the GD-352M sensitivity was found to be practically negligible, the dose value of the vertical or horizontal GD-352M that provided the higher dose value was used.
Table 5.
Vertical/horizontal dose ratio of GD-352M inside the radiation safety glasses (n = 91 procedures, June 2017–May 2018).
| Side of radiation safety glasses | Vertical-to-horizontal dose ratio (V/H)∗ |
||
|---|---|---|---|
| Mean ± SD | Median [range] | 95%CI | |
| Right (n = 91) | 1.03 ± 0.03 | 1.00 [0.72–3.33] | 0.97–1.08 |
| Left (n = 91) | 1.00 ± 0.02 | 0.98 [0.49–1.78] | 0.97–1.04 |
SD, standard deviation.
95%CI, 95% confidence interval of mean value.
Vertical-to-horizontal dose ratio of GD-352M placed perpendicular to the ground (vertically) and parallel to the ground (horizontally) inside the radiation safety glasses.
3.3. Bilateral difference in occupational dose to the lens of the eye
Bilateral dose ratios (right/left) for both outside and inside the radiation safety glasses were approximately 1.0, indicating an absence of clear bilateral differences (Table 6). The greater dose value from either the right or left side was used as the Hp(3) to the lens of the eye.
Table 6.
Bilateral dose ratio of GD-352M (n = 91 procedures, June 2017–May 2018).
| Outside/Inside radiation safety glasses | Bilateral dose ratio (right/left)∗ |
||
|---|---|---|---|
| Mean ± SD | Median [range] | 95%CI | |
| Outside (n = 91) | 1.04 ± 0.61 | 0.95 [0.17–4.81] | 0.91–1.16 |
| Inside (n = 91) | 1.02 ± 0.23 | 0.99 [0.49–1.78] | 0.97–1.07 |
95%CI, 95% confidence interval of mean value.
SD, standard deviation.
Dose ratio of GD-352M placed on the right and left sides of the radiation safety glasses.
3.4. Working practice and occupational dose to the lens of the eye for CT-assisting personnel
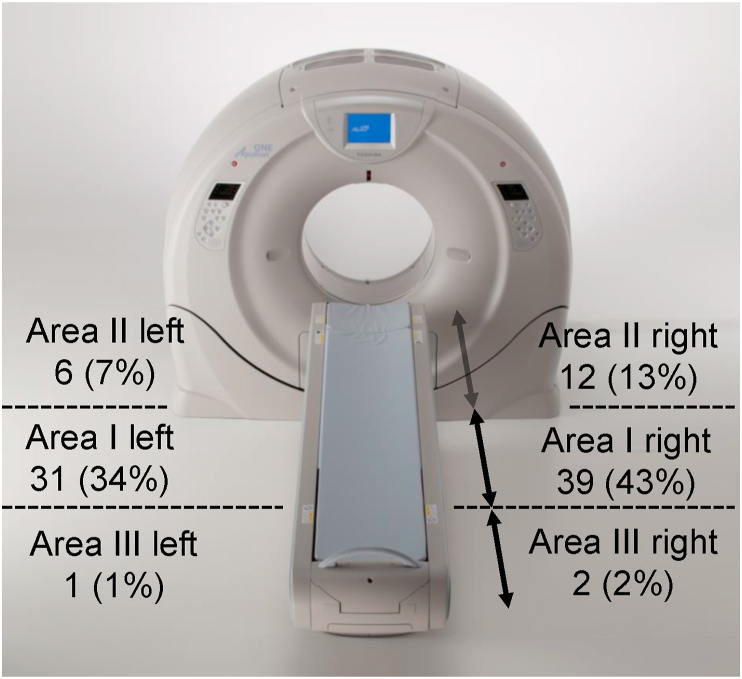
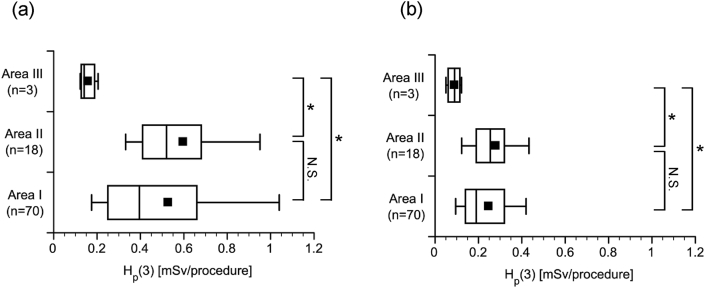
Working practices for CT-assisting personnel are shown in Table 7. Assistance was mostly performed in Area I and Area II near the CT gantry ((31 + 39 + 6 + 12)/91, 97%) (Figure 5). Working in Area I and Area II, compared with Area III (distant from the CT gantry), resulted in significantly higher Hp(3) both outside (Figure 6a) and inside (Figure 6b) the radiation safety glasses.
Table 7.
Working practice for CT-assisting personnel by profession (n = 91 procedures, June 2017–May 2018).
| Working practice | Intensive care physician (n = 6) | Pediatrician (n = 2) | Radiological technologist (n = 3) | Total [procedure] |
|---|---|---|---|---|
| Assisted ventilation with bag-valve-mask | 65 | 0 | 0 | 65 |
| Head holding | 0 | 5 | 7 | 12 |
| Observation | 7 | 1 | 6 | 14 |
| Total [procedure] | 72 | 6 | 13 | 91 |
Figure 5.
Standing positions of CT-assisting personnel and number of assists (n = 91, June 2017–May 2018). Area I is on the side of the bed near the CT gantry. Area II is on the other side of the bed and near the CT gantry. Area III is on the side of the bed away from the CT gantry. The number of personnel (number of times, %) in each position is listed.
Figure 6.
The 3-mm dose-equivalent (Hp(3)) to the lens of the eye by standing position of the CT-assisting personnel during CT (n = 91, June 2017–May 2018). Hp(3) to the lens of the eye of the assisting personnel per CT procedure (a) outside the radiation safety glasses and (b) inside the radiation safety glasses. ANOVA (Kruskal-Wallis) resulted in: (a) P = 0.010 and (b) P = 0.017. ∗ Pairs with P < 0.05 according to multiple comparison using Dunn's test (with Bonferroni correction) are shown. N.S., no statistical significance.
No significant differences in Hp(3) were seen between professions for both outside (P = 0.094, Kruskal-Wallis, Table 8) and inside (P = 0.108, Kruskal-Wallis, Table 8) the radiation safety glasses.
Table 8.
Occupational doses to the lens of the eye, CT imaging settings, and CT dose indices by profession of CT-assisting personnel (n = 91 procedures, June 2017–May 2018).
| Profession | Intensive care physician (n = 6, 72 procedures) |
Pediatrician (n = 2, 6 procedures) |
Radiological technologist (n = 3, 13 procedures) |
ANOVA∗ (P value) | Total (n = 11, 91 procedures) |
||||
|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Median [range] | Mean ± SD | Median [range] | Mean ± SD | Median [range] | Mean ± SD | Median [range] | ||
|
Analysis point | |||||||||
| Outside radiation safety glasses (Hp(3)) [mSv] | 0.55 ± 0.39 | 0.49 [0.12–2.49] | 0.53 ± 0.42 | 0.30 [0.15–1.18] | 0.41 ± 0.41 | 0.28 [0.07–1.64] | 0.094 | 0.53 ± 0.39 | 0.43 [0.07–2.49] |
| Inside radiation safety glasses (Hp(3)) [mSv] | 0.26 ± 0.15 | 0.23 [0.05–1.05] | 0.23 ± 0.15 | 0.14 [0.09–0.46] | 0.19 ± 0.15 | 0.15 [0.06–0.65] | 0.108 | 0.25 ± 0.15 | 0.21 [0.05–1.05] |
|
CT imaging setting, CT dose index | |||||||||
| Tube voltage [kVp] | 120 ± 3 | 120 [100–135] | 107 ± 9 | 100 [100–120] | 117 ± 7 | 120 [100–120] | <0.001 | 120 ± 6 | 120 [100–135] |
| Tube current [mA] | 4,131.2 ± 2,522.4 | 3,847.5 [968.0–13,196.0] | 720.8 ± 741.6 | 339.0 [211.3–2,148.0] | 1,650.0 ± 1,253.8 | 1177 .0 [116.0–5,178.0] | <0.001 | 3,532.2 ± 2,570.1 | 3,373.0 [67.0–13,196.0] |
| CTDIvol [mGy] | 44.5 ± 24.7 | 48.6 [8.8–119.9] | 23.6 ± 14.4 | 21.0 [2.2–42.5] | 51.8 ± 25.4 | 45.3 [10.9–100.0] | 0.650 | 41.5 ± 25.0 | 44.0 [2.2–119.9] |
| DLP [mGy・cm] | 1,802.2 ± 947.7 | 1,561.0 [280.4–4,824.6] | 474.2 ± 367.8 | 360.1 [26.9–1,063.4] | 1,072.0 ± 703.1 | 862.9 [18.1–2,543.8] | <0.001 | 1,577.7 ± 972.5 | 1,462.8 [18.1–4,824.6] |
CTDIvol, volume computed tomography dose index.
DLP, dose-length product.
Hp(3), 3-mm dose-equivalent (personal dose equivalent).
SD, standard deviation.
Homogeneity of the three profession groups was confirmed using the Kruskal-Wallis test.
Considering these results together, the distance from the CT gantry obviously exerts a stronger influence on Hp(3) than mere differences in professions. Actually, both the intensive care physicians and the pediatricians that frequently assist patients (assisted ventilation with bag-valve mask and head holding are always performed in Area I or II) near the CT gantry (Table 7) showed a higher Hp(3) tendency than radiological technologists (Table 8), who often perform observations while away from the CT gantry (Table 7).
3.5. Maximum number of procedures before reaching the annual dose limit
Considering that 20 mSv is the annual dose limit for the lens of the eye, the number of procedures that can be performed on an annual basis before reaching the annual dose limit when radiation safety glasses are not worn (calculated from outside the radiation safety glasses) and worn (calculated from inside the radiation safety glasses) was shown in Table 9. Assisted ventilation with the bag-valve-mask is the most frequently performed procedure (65/91, 71%), and is entirely performed by the intensive care physician (65/65, 100%) (Table 7). If one intensive care physician provided all the assistance without wearing radiation safety glasses, the annual limit could easily be exceeded. Warning individuals to wear radiation safety glasses is clinically important to avoid exceeding the annual dose limit for the lens of the eye.
Table 9.
Maximum number of procedures before reaching the annual dose limit (n = 91 procedures, June 2017–May 2018).
| Practice | Assisted ventilation with bag-valve-mask (n = 65 procedures) |
Head holding (n = 12 procedures) |
Observation (n = 14 procedures) |
|||
|---|---|---|---|---|---|---|
| (Hp(3)) Median [range] [mSv] |
Max number | (Hp(3)) Median [range] [mSv] |
Max number | (Hp(3)) Median [range] [mSv] | Max number | |
|
Analysis point | ||||||
| Outside radiation safety glasses | 0.51 [0.14–2.49] | 39∗ | 0.36 [0.20–1.64] | 55∗ | 0.19 [0.07–1.46] | 105∗ |
| Inside radiation safety glasses | 0.25 [0.08–1.05] | 80∗ | 0.16 [0.12–0.65] | 125∗ | 0.12 [0.05–0.50] | 166∗ |
Hp(3), 3-mm dose-equivalent (personal dose equivalent).
Maximum number not exceeding 20 mSv/year, calculated by 20 [mSv]/Median [mSv] (rounded down to nearest integer).
3.6. Dose reduction efficiency with radiation protective equipment
Radiation safety glasses reduced the Hp(3) to the lens of the eye by 51% (Table 10). Moreover, use of a bag-valve-mask extension tube reduced the doses outside and inside the radiation safety glasses by 43% and 31%, respectively (Table 11). Furthermore, a 0.25-mm Pb-equivalent thickness radiation protective curtain reduced the Hp(3) by 61% (Table 12).
Table 10.
Dose reduction efficiency with radiation safety glasses (n = 91 procedures, June 2017–May 2018).
| Mean ± SD | Median [range] | 95%CI | Dose reduction rate [%] ∗∗ | |
|---|---|---|---|---|
| Hp(3) ratio outside/inside the radiation safety glasses (outside/inside)∗ | 2.06 ± 0.44 | 2.04 [1.07–3.73] | 1.96–2.15 | 51 |
SD, standard deviation; 95%CI, 95% confidence interval.
Ratio of Hp(3) outside the radiation safety glasses (higher value of either left or right) and Hp(3) inside the radiation safety glasses (higher value of either left or right).
(2.04 – 1)/2.04 × 100 [%].
Table 11.
Dose reduction efficiency with bag-valve-mask extension tube (n = 65 procedures).
| Practice | Without extension tube (n = 3 procedures) |
With extension tube (n = 62 procedures) |
Dose reduction rate∗ [%] | ||
|---|---|---|---|---|---|
| Hp(3) |
Hp(3)/DLP |
Hp(3) |
Hp(3)/DLP |
||
| Median [range] [mSv] |
Median [range] (a) [mSv·mGy−1·cm−1 ·10−4] | Median [range] [mSv] |
Median [range] (b) [mSv·mGy−1·cm−1·10−4] | ||
|
Analysis point | |||||
| Outside radiation safety glasses | 1.79 [0.69–2.49] | 5.16 [3.59–11.8] | 0.50 [0.14–1.13] | 2.92 [0.88–7.62] | 43 |
| Inside radiation safety glasses | 0.56 [0.26–1.05] | 2.18 [1.37–3.69] | 0.23 [0.08–0.56] | 1.51 [0.55–3.24] | 31 |
Hp(3), 3-mm dose-equivalent (personal dose equivalent).
DLP, dose-length product.
Dose reduction rate estimated as: {1 - (b)/(a)} × 100 [%].
Table 12.
Dose reduction efficiency with radiation protective curtain (n = 5).
| Practice | None (n = 5) |
Radiation protective curtain (0.25-mm-Pb)∗ (n = 5) |
Dose reduction rate∗∗∗ [%] |
|---|---|---|---|
| Hp (3) (a) |
Hp (3) (b) |
||
| Mean ± SD [mSv] | Mean ± SD [mSv] | ||
|
Analysis point | |||
| Eye level of the CT assisting personnel∗∗ | 0.31 ± 0.04 | 0.12 ± 0.03 | 61 |
Hp(3), 3-mm dose-equivalent (personal dose equivalent).
SD, standard deviation.
39 × 43 cm, installed at 90 cm from isocenter of the CT gantry, upper edge at a height of 185 cm from the ground.
Forehead of the Alderson RANDO phantom, 100 cm from isocenter of the CT gantry, at a height of 160 cm from the ground.
Dose reduction rate estimated as: {1 - (b)/(a)} × 100 [%].
3.7. Case illustration: a case of high occupational dose to the lens of the eye from a single instance of assisting in CT scans
Assistance in CT imaging was performed for an 80-year-old man who developed a complication of retroperitoneal abscess after surgery for left renal pelvis cancer. Since bleeding continued, plain CT and multiphase contrast-enhanced CT were conducted to determine the cause. An intensive care physician performed assisted ventilation using a bag-valve-mask without an extension tube and worked in Area I right near the CT gantry (Figure 5) during the scan. In this case, multiple CT scans were required, resulting in a DLP of 4,824.6 mGy⋅cm, which was higher than usual (Table 8). Hp(3) to the lens of the eye for the CT-assisting personnel was therefore extremely high, at 2.49 mSv and 1.05 mSv outside and inside the radiation safety glasses, respectively.
4. Discussion
The personal dose equivalent to the lens of the eye of medical staff has traditionally been monitored by a personal dosimeter installed outside the lead apron. However, after the ICRP issued a recommendation to reduce the annual equivalent dose limit for the lens of the eye from 150 mSv to 20 mSv in 2011 [5], the need to manage the dose more strictly than ever has increased, and it has become necessary to measure the dose near the eyes, considering the shielding efficiency obtained using radiation safety glasses.
However, in Japan, the only two dosimeters that can currently be used are DOSIRIS™ (Institute for Radiological Protection and Nuclear Safety: IRSN, France) and Vision™ (Landauer, Glenwood, IL). Typically, these dosimeters measure cumulative dose in 1 month and do not offer sufficient sensitivity to evaluate dose per procedure when assisting patients in a CT scan. For this reason, we constructed an eye lens dosimeter clip and applied the GD-352M dosimeter that complies with the IEC62387 requirements [32] with sufficient sensitivity and accuracy. In this study, CT-assisting personnel wearing radiation safety glasses placed two GD-352M dosimeters in an L shape under the radiation safety glasses. As a result, it was clarified that the radiation sensitivity of GD-352M was not affected by the direction. This was probably because the directions of the primarily scattered x-rays were different from the two directions of GD-352M, that is, the direction vertically or horizontally to the ground. It was also found that the field of view was not obstructed. In addition, Hp(3) considering the shielding effect of radiation safety glasses could be obtained for each case of assisting patients. Therefore, in order to measure Hp (3) in single case of assistance, it would be sufficient to install one GD-352M vertically or horizontally to the ground inside the radiation safety glasses.
Our results proved that intensive care physicians, who are frequently exposed to radiation during CT for “diagnostic” purposes, had an Hp(3) of 0.49 mSv/procedure (median) without radiation safety glasses (Table 8). Our data was about the same as the value of Hp(3) previously reported for the CT-assistance personnel during “diagnostic” CT scans [28, 29]. Furthermore, our data showed a significantly greater Hp(3) than the previously reported doses to the lens of the eye for the operator during CT fluoroscopy for “treatment” purposes (Table 1). Pravata et al. reported that the DLP value was 124 mGy・cm for “treatment” CT scans [23], whereas standard setting was about several hundred ~ mGy・cm for “diagnostic” CT scans for adult patients according to our hospital's data (Table 4). CT for “diagnostic” purposes requires a larger number of photons to be injected into the subject than CT fluoroscopy for “treatment” purposes, given the need to obtain high-resolution imaging. This was considered one of the reasons for the higher occupational dose compared to other CT-assisting personnel. Intensive care physicians thus require appropriate training on protective measures suitable to the high occupational dose to the lens of the eye.
In this study, radiation safety glasses showed a 51% dose reduction, which was almost the same as previously reported for the protective glasses with 0.07-mm Pb-equivalent thickness (51.3%–60.0%) [7, 10, 13, 28, 36, 37, 38]. Increasing the lead content of radiation safety glasses (e.g. 0.5 or 0.75-mm Pb-equivalent) can improve the shielding effect, but it will be heavier. It is important to note that if radiation safety glasses are no longer worn simply because they are heavy, they will result in no contribution to radiation protection. When analyzing dose reduction efficiency using dosimeters installed outside and inside the radiation safety glasses, a high level of uncertainty remains, due to the radiation scattered from the glasses themselves [36] and the head of the personnel as well, posture of medical staff, position relative to the X-ray source, and the equipment model [37, 38, 39]. Although uncertainties in dose reduction efficiency cannot be entirely ignored, it would be preferable for medical staff who are likely to exceed the annual dose limit for the lens of the eye to monitor inside the radiation safety glasses (when used) rather than outside the lead apron.
When considering the radiation protection of CT-assisting personnel, the three areas of the fundamentals of industrial health management [40] are important (Table 13). Following these fundamentals, if “multiple protective measures” can be implemented with the combination of bag-valve-mask extension tube and radiation safety glasses, reducing Hp(3) to the lens of the eye by 66% (calculated by a simple multiplication, (1 – 0.31) × (1 – 0.51) × 100 = 34%) would be theoretically possible without placing any significant burden on either medical staff or the medical institution.
Table 13.
Three areas of industrial health management for CT-assisting personnel.
| Three areas of industrial health management | Specific measures |
|---|---|
| I Working environment management | Measurement of scattered radiation, radiation shielding, use of protective boards (curtain), optimization of CT imaging settings in comparison with DRLs |
| II Working management | Examination of CT-assistance procedures, use of personal protective equipment (radiation safety glasses, neck guards, protective clothing), use of bag-valve-mask extension tube |
| III Health management | Health checkup before employment (before assignment), regular health checkup (general examination; specialized tests for blood, lens of the eye, skin, etc.), health diagnosis at abnormal radiation exposure, follow-up after leaving work |
DRLs, diagnostic reference levels.
Nonetheless, when an increase is seen in unforeseen cases irradiated with a high dose, as shown in the case illustration, a radiation protective curtain (Figure 4) or so (e.g. Ceiling-mounted transparent barrier) should be installed in the CT examination room. Using these three types of protection as part of the “multiple protective measures,” an 87% (calculated by a simple multiplication, (1 – 0.31) × (1 – 0.51) × (1 – 0.61) × 100 = 13%) reduction in Hp(3) to the lens of the eye can be expected. However, installing a ceiling-mounted radiation protective curtain is not necessarily easy, due to the structural limitations of CT examination rooms, the high cost of installation, and the obstacle created to patient assistance.
5. Conclusions
We could measure the Hp(3) to the lens of the eye of the CT-assisting personnel in a single procedure using GD-352M attached to the dosimeter clip developed. We also found that median Hp(3) to the lens of the eye for intensive care physicians, who frequently perform assisted ventilation with a bag-valve-mask, was 0.49 mSv/procedure without wearing radiation safety glasses, indicating that the equivalent dose to the lens of the eye may exceed 20 mSv annually. However, following the fundamentals of industrial health, implementing “multiple protective measures” could achieve full compliance with the equivalent dose limit for the lens of the eye (average annual limit, 20 mSv/year over 5 years).
Declarations
Author contribution statement
T. Moritake, K. Nagamoto: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
K. Nakagami, K. Morota, S. Matsuzaki: Performed the experiments; Analyzed and interpreted the data.
S. Nihei, M. Kamochi: Performed the experiments Investigation; Contributed reagents, materials, analysis tools or data.
N. Kunugita: Contributed reagents, materials, analysis tools or data.
Funding statement
S. Nihei was supported by JSPS KAKENHI Grant Number JP18K09959. M. Kamochi was supported by JSPS KAKENHI Grant Number JP19K10498. T. Moritake was supported by JSPS KAKENHI Grant Number JP18H03376. N. Kunugita was supported by Japanese Ministry of Health, Labour and Welfare (Grant Number: 180501-1).
Data availability statement
Data included in article/supplementary material/referenced in article.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- 1.ICRP Publication 41: NONSTOCHASTIC effects of ionizing radiation. Ann. ICRP. 1984;14(3):1–33. [PubMed] [Google Scholar]
- 2.Nakashima E., Neriishi K., Minamoto A. A reanalysis of atomic-bomb cataract data, 2000-2002: a threshold analysis. Health Phys. 2006;90(2):154–160. doi: 10.1097/01.hp.0000175442.03596.63. [DOI] [PubMed] [Google Scholar]
- 3.Neriishi K., Nakashima E., Minamoto A., Fujiwara S., Akahoshi M., Mishima H.K., Kitaoka T., Shore R.E. Postoperative cataract cases among atomic bomb survivors: radiation dose response and threshold. Radiat. Res. 2007;168(4):404–408. doi: 10.1667/RR0928.1. [DOI] [PubMed] [Google Scholar]
- 4.Worgul B.V., Kundiyev Y.I., Sergiyenko N.M., Chumak V.V., Vitte P.M., Medvedovsky C., Bakhanova E.V., Junk A.K., Kyrychenko O.Y., Musijachenko N.V., Shylo S.A., Vitte O.P., Xu S., Xue X., Shore R.E. Cataracts among Chernobyl clean-up workers: implications regarding permissible eye exposures. Radiat. Res. 2007;167(2):233–243. doi: 10.1667/rr0298.1. [DOI] [PubMed] [Google Scholar]
- 5.ICRP ICRP statement on tissue reactions/early and late effects of radiation in normal tissues and organs – threshold doses for tissue reactions in a radiation protection context. Ann. ICRP. 2012;41(1-2):1–322. doi: 10.1016/j.icrp.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 6.Moritake T., Matsumaru Y., Takigawa T., Nishizawa K., Matsumura A., Tsuboi K. Dose measurement on both patients and operators during neurointerventional procedures using photoluminescence glass dosimeters. AJNR Am. J. Neuroradiol. 2008;29(10):1910–1917. doi: 10.3174/ajnr.A1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kato M., Chida K., Ishida T., Toyoshima H., Yoshida Y., Yoshioka S., Moroi J., Kinoshita T. Occupational radiation exposure of the eye in neurovascular interventional physician. Radiat. Protect. Dosim. 2019;185(2):151–156. doi: 10.1093/rpd/ncy285. [DOI] [PubMed] [Google Scholar]
- 8.Vanhavere F., Carinou E., Domienik J., Donadille L., Ginjaume M., Gualdrini G., Koukorava C., Krim S., Nikodemova D., Ruiz-Lopez N., Sans-Merce M., Struelens L. Measurements of eye lens doses in interventional radiology and cardiology: final results of the ORAMED project. Radiat. Meas. 2011;46(11):1243–1247. doi: 10.1093/rpd/ncq508. [DOI] [PubMed] [Google Scholar]
- 9.Wong J.H.D., Anem L.E.A., Tan S., Tan S.K., Ng K.H. Eye lens dose of medical personnel involved in fluoroscopy and interventional procedures at a Malaysian Hospital. Phys. Med. 2019;68:47–51. doi: 10.1016/j.ejmp.2019.11.007. [DOI] [PubMed] [Google Scholar]
- 10.Haga Y., Chida K., Kaga Y., Sota M., Meguro T., Zuguchi M. Occupational eye dose in interventional cardiology procedures. Sci. Rep. 2017;7(1):569. doi: 10.1038/s41598-017-00556-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O'Connor U., Walsh C., Gallagher A., Dowling A., Guiney M., Ryan J.M., McEniff N., O'Reilly G. Occupational radiation dose to eyes from interventional radiology procedures in light of the new eye lens dose limit from the International Commission on Radiological Protection. Br. J. Radiol. 2015;88(1049):20140627. doi: 10.1259/bjr.20140627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O'Connor U., Gallagher A., Malone L., O'Reilly G. Occupational radiation dose to eyes from endoscopic retrograde cholangiopancreatography procedures in light of the revised eye lens dose limit from the International Commission on Radiological Protection. Br. J. Radiol. 2013;86(1022):20120289. doi: 10.1259/bjr.20120289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matsubara K., Takei Y., Mori H., Kobayashi I., Noto K., Igarashi T., Suzuki S., Akahane K. A multicenter study of radiation doses to the eye lenses of medical staff performing non-vascular imaging and interventional radiology procedures in Japan. Phys. Med. 2020;74:83–91. doi: 10.1016/j.ejmp.2020.05.004. [DOI] [PubMed] [Google Scholar]
- 14.Lee B., Kim M.S., Eum D., Min K.T. The radiation environment of anaesthesiologists in the endoscopic retrograde cholangiopancreatography room. Sci. Rep. 2019;9(1):9124. doi: 10.1038/s41598-019-45610-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Silverman S.G., Tuncali K., Adams D.F., Nawfel R.D., Zou K.H., Judy P.F. CT fluoroscopy-guided abdominal interventions: techniques, results, and radiation exposure. Radiology. 1999;212(3):673–681. doi: 10.1148/radiology.212.3.r99se36673. [DOI] [PubMed] [Google Scholar]
- 16.Daly B., Krebs T.L., Wong-You-Cheong J.J., Wang S.S. Percutaneous abdominal and pelvic interventional procedures using CT fluoroscopy guidance. AJR. Am. J. Roentgenol. 1999;173(3):637–644. doi: 10.2214/ajr.173.3.10470894. [DOI] [PubMed] [Google Scholar]
- 17.Mellenberg D.E., Sato Y., Thompson B.H., Warnock N.G. Personnel exposure rates during simulated biopsies with a real-time CT scanner. Acad. Radiol. 1999;6(11):687–690. doi: 10.1016/S1076-6332(99)80118-4. [DOI] [PubMed] [Google Scholar]
- 18.Paulson E.K., Sheafor D.H., Enterline D.S., McAdams H.P., Yoshizumi T.T. CT fluoroscopy-guided interventional procedures: techniques and radiation dose to radiologists. Radiology. 2001;220(1):161–167. doi: 10.1148/radiology.220.1.r01jl29161. [DOI] [PubMed] [Google Scholar]
- 19.Joemai R.M., Zweers D., Obermann W.R., Geleijns J. Assessment of patient and occupational dose in established and new applications of MDCT fluoroscopy. AJR Am. J. Roentgenol. 2009;192(4):881–886. doi: 10.2214/AJR.08.1765. [DOI] [PubMed] [Google Scholar]
- 20.Heusch P., Kröpil P., Buchbender C., Aissa J., Lanzman R.S., Heusner T.A., Ewen K., Antoch G., Fürst G. Radiation exposure of the radiologist’s eye lens during CT-guided interventions. Acta Radiol. 2014;55(1):86–90. doi: 10.1177/0284185113493222. [DOI] [PubMed] [Google Scholar]
- 21.Gyekye P., Becker F., Mensah S., Emi-Reynolds G. Optimisation of scatter radiation to staff during CT-fluoroscopy: Monte Carlo studies. Radiat. Protect. Dosim. 2016;170(1-4):393–397. doi: 10.1093/rpd/ncw135. [DOI] [PubMed] [Google Scholar]
- 22.Sarmento S., Pereira J.S., Sousa M.J., Cunha L.T., Dias A.G., Pereira M.F., Oliveira A.D., Cardoso J.V., Santos L.M., Santos J.A.M., Alves J.G. The use of needle holders in CTF guided biopsies as a dose reduction tool. J. Appl. Clin. Med. Phys. 2018;19(1):250–258. doi: 10.1002/acm2.12234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pravata E., Presilla S., Roccatagliata L., Cianfoni A. Operator radiation doses during CT-guided spine procedures. Clin. Neurol. Neurosurg. 2018;173:105–109. doi: 10.1016/j.clineuro.2018.08.015. [DOI] [PubMed] [Google Scholar]
- 24.Kato R., Katada K., Anno H., Suzuki S., Ida Y., Koga S. Radiation dosimetry at CT fluoroscopy: physician's hand dose and development of needle holders. Radiology. 1996;201(2):576–578. doi: 10.1148/radiology.201.2.8888264. [DOI] [PubMed] [Google Scholar]
- 25.Stoeckelhuber B.M., Leibecke T., Schulz E., Melchert U.H., Bergmann-Koester C.U., Helmberger T., Gellissen J. Radiation dose to the radiologist's hand during continuous CT fluoroscopy-guided interventions. Cardiovasc. Intervent. Radiol. 2005;28(5):589–594. doi: 10.1007/s00270-005-0104-2. [DOI] [PubMed] [Google Scholar]
- 26.Neeman Z., Dromi S.A., Sarin S., Wood B.J. CT fluoroscopy shielding: decreases in scattered radiation for the patient and operator. J. Vasc. Intervent. Radiol. 2006;17(12):1999–2004. doi: 10.1097/01.RVI.0000244847.63204.5F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Al-Haj A.N., Lobriguito A.M., Lagarde C.S. Occupational doses during the injection of contrast media in paediatric CT procedures. Radiat. Protect. Dosim. 2003;103(2):169–172. doi: 10.1093/oxfordjournals.rpd.a006129. [DOI] [PubMed] [Google Scholar]
- 28.Miyajima R., Fujibuchi T., Miyachi Y., Tateishi S., Uno Y., Amakawa K., Ohura H., Orita S. Effective techniques to reduce radiation exposure to medical staff during assist of X-ray computed tomography examination. Nihon Housyasen Gizyutsu Gakkai Zasshi. 2018;74(4):326–334. doi: 10.6009/jjrt.2018_JSRT_74.4.326. [DOI] [PubMed] [Google Scholar]
- 29.Sookpeng S., Martin C.J., Kadman B. Eye lens radiation doses to miscentering patients and health-care staff from head computed tomography. J. Radiol. Nurs. 2019;38(3):193–199. [Google Scholar]
- 30.J-RIME . 2015. Diagnostic Reference Levels Based on Latest Surveys in Japan:Japan DRLs 2015.http://www.radher.jp/J-RIME/report/DRLhoukokusyoEng.pdf [Google Scholar]
- 31.Silva E.H., Knezevic Z., Struelens L., Covens P., Ueno S., Vanhavere F., Buls N. Energy and angular dependence of radiophotoluminescent glass dosemeters for eye lens dosimetry. Radiat. Protect. Dosim. 2016;170(1-4):208–212. doi: 10.1093/rpd/ncw104. [DOI] [PubMed] [Google Scholar]
- 32.Silva E.H., Struelens L., Covens P., Ueno S., Koguchi Y., Vanhavere F., Buls N. Optimization of a radiophotoluminescent glass dosemeter for occupational eye lens dosimetry in interventional radiology/cardiology. Radiat. Protect. Dosim. 2018;182(2):177–183. doi: 10.1093/rpd/ncy046. [DOI] [PubMed] [Google Scholar]
- 33.Tucker D.M., Barnes G.T., Chakraborty D.P. Semiempirical model for generating tungsten target x-ray spectra. Med. Phys. 1991;18(2):211–218. doi: 10.1118/1.596709. [DOI] [PubMed] [Google Scholar]
- 34.Hubbell J.H., Seltzer S.M. National Institute of Standards and Technology; 1995. Tables of X-Ray Mass Attenuation Coefficients and Mass Energy-Absorption Coefficients from 1 keV to 20 MeV for Elements Z = 1 to 92 and 48 Additional Substances of Dosimetric Interest. Physical Reference Data (NISTIR 5632) [Google Scholar]
- 35.Daures J., Gouriou J., Bordy J.M. CEA-R-6235 Saclay; 2009. Conversion Coefficients from Air Kerma to Personal Dose Equivalent Hp(3) for Eye-Lens Dosimetry. [Google Scholar]
- 36.Tanaka T., Matsubara K., Fukuda A., Kobayashi S. Estimation of Ηp(3) to the eye lens of interventional radiologists - relation between the eye lens dose and radiologist’s height. Radiat. Protect. Dosim. 2019;187(4):409–417. doi: 10.1093/rpd/ncz181. [DOI] [PubMed] [Google Scholar]
- 37.van Rooijen B.D., de Haan M.W., Das M., Arnoldussen C.W., de Graaf R., van Zwam W.H., Backes W.H., Jeukens C.R. Efficacy of radiation safety glasses in interventional radiology. Cardiovasc. Intervent. Radiol. 2014;37(5):1149–1155. doi: 10.1007/s00270-013-0766-0. [DOI] [PubMed] [Google Scholar]
- 38.Mao L., Liu T., Caracappa P.F., Lin H., Gao Y., Dauer L.T., Xu X.G. Influences of operator head posture and protective eyewear on eye lens doses in interventional radiology: a Monte Carlo Study. Med. Phys. 2019;46(6):2744–2751. doi: 10.1002/mp.13528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rivett C., Dixon M., Matthews L., Rowles N. An assessment of the dose reduction of commercially available lead protective glasses for interventional radiology staff. Radiat. Protect. Dosim. 2016;172(4):443–452. doi: 10.1093/rpd/ncv540. [DOI] [PubMed] [Google Scholar]
- 40.Koshi S. A basic framework of working environment control for occupational health in Japan. Ind. Health. 1996;34(3):149–165. doi: 10.2486/indhealth.34.149. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data included in article/supplementary material/referenced in article.