Abstract
Several types of contraception methods exist, and among these are hormonal and non-hormonal intrauterine devices (IUDs). Cases have been reported of fractured IUD pieces and retention of copper fragments upon attempted removal in office. These findings suggest the importance of careful removal of an IUD by providers. A 38-year-old Caucasian woman, gravida 2, para 2, presented for a colposcopy and endometrial biopsy (EMB). She had had a copper IUD (ParaGard) placed 10 years prior. She now requested to have it removed. After completion of the colposcopy and EMB, the provider located the IUD strings for removal. During careful removal of the IUD, a piece was broken off and remained in the uterine cavity. Upon visual inspection of the removed IUD, the right wing was missing and presumed to be still in the patient. Transabdominal and transvaginal ultrasound (TVUS) confirmed presence of a portion of the IUD in the uterine wall near the cervix. The patient was scheduled for surgical removal of the IUD by robot-assisted total laparoscopic hysterectomy with bilateral salpingectomy. This case highlights the importance of thorough evaluation of an IUD upon removal. Practitioners who work with IUD insertion and removal should remain informed about this rare complication. Risk of fracture during IUD removal should be better communicated between physicians and patients. This case study underlines the importance of careful IUD planning, from insertion to removal. Further research considering improved stepwise removal should be considered.
Keywords: Gynecology, Fractured, Intrauterine device, Copper, Removal, Case report
Highlights
-
•
Fracture of an intrauterine device (IUD) upon removal is a very rare complication, with a prevalence rate of 1–2%.
-
•
Risk of fracture during IUD removal should be better communicated between physicians and patients.
-
•
Our patient's IUD fracture prompted a hysterectomy to safely remove the device.
-
•
Malposition of an IUD may interfere with effectiveness and complicate removal.
1. Introduction
Several types of contraception methods exist, and among these are hormonal and non-hormonal intrauterine devices (IUDs). The non-hormonal, copper-based ParaGard IUD is approved for up to 10 years [1]. Mechanism of action is the prevention of fertilization via the spermicidal nature of the copper IUD2. In addition, the ParaGard is the most effective form of emergency contraception [1]. Risks for this form of contraception exist; however, the overall adverse event risk is low [2]. Cases have been reported of fractured IUD pieces and retention of copper fragments upon attempted removal in office [3,4]. These findings suggest the importance of careful removal of IUD by providers, especially if copper is included due to its inflammatory properties [3]. Treatment for retained IUD consists of hysteroscopy or laparoscopy in office before consideration to admit for surgical removal [5]. This case study reviews the treatment course of a retained and broken IUD after attempted removal in office.
2. Case Presentation
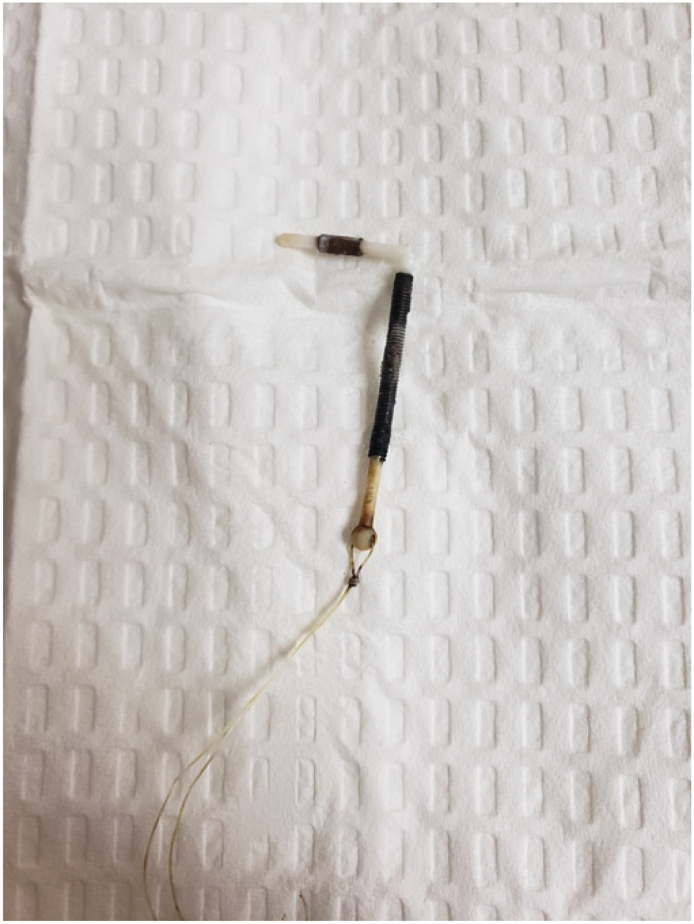
A 38-year-old Caucasian woman, gravida 2, para 2, presented for a colposcopy and endometrial biopsy (EMB) as follow-up for a previous abnormal pap smear. She had had the copper IUD (ParaGard) device placed 10 years prior. She now requested to have it removed. Past medical history included abnormal pap smear showing atypical squamous cells of undetermined significance (ASCUS), positive HPV findings, dysmenorrhea, irregular periods, intermenstrual bleeding and menorrhagia. She had a family history significant for breast cancer and deep venous thrombosis (DVT). Past surgical history was significant for loop electrosurgical excision procedures (LEEP) for cervical intraepithelial neoplasia 2 (CIN 2). The patient appeared well, with normal vital signs. On physical exam, her vaginal canal and cervix were normal, and the IUD strings were visible. After completion of the colposcopy and EMB, the provider located the strings for removal of the IUD. During careful removal of the IUD, a piece was broken off and remained in the uterine cavity. Upon visual inspection of the removed IUD (Fig. 1), the right wing was missing and presumed to be still in the patient. At this time, she was in no acute distress. The patient was diagnosed with retained specified foreign body and scheduled for an ultrasound scan to locate the missing IUD fragment.
Fig. 1.
ParaGard copper IUD removed from patient. Found to have broken right wing upon inspection.
On follow-up she presented to the clinic for results of her colposcopy and EMB. Colposcopy showed CIN2 and inflammation. EMB findings were benign. An ultrasound scan was performed to locate the presence of the broken IUD in office.
3. Management and Outcome
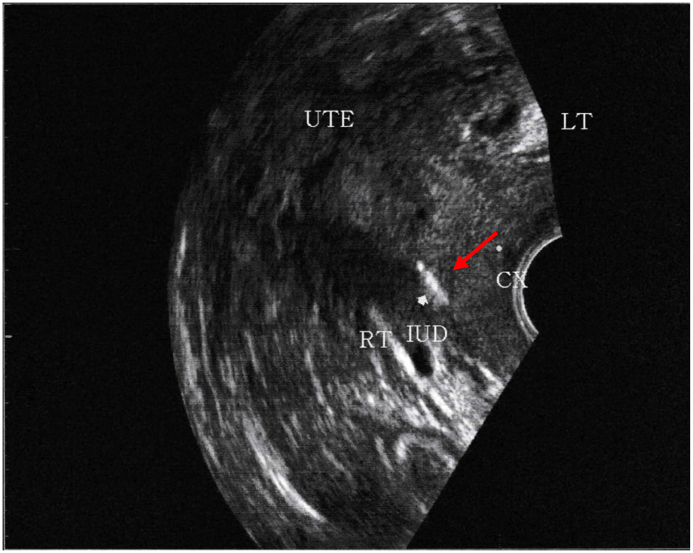
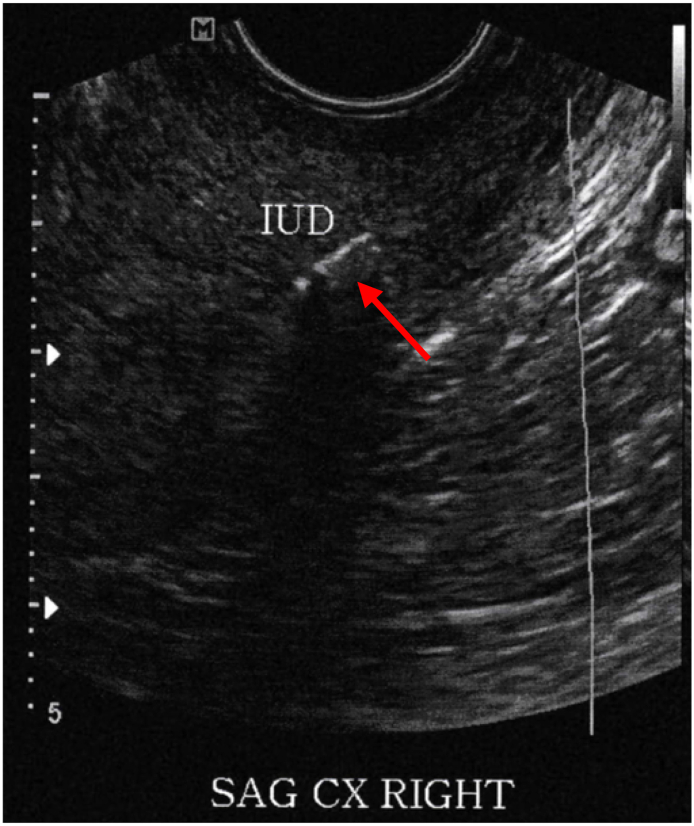
Transabdominal and transvaginal ultrasound (TVUS) confirmed the presence of a portion of the IUD in the uterine wall near the cervix, along with a uterine fibroid (Fig. 2, Fig. 3). The patient was scheduled for surgical removal of the IUD by robot-assisted total laparoscopic hysterectomy with bilateral salpingectomy. This method of IUD removal was chosen by the provider because of the patient's history of bleeding, abnormal pap smears, the location of the retained IUD prior to removal, and presence of fibroids found via ultrasound. During surgery, the uterus was measured to be 9 cm and the ovaries appeared normal. There was endometriosis noted in the posterior cul-de-sac on the uterosacral ligaments bilaterally, which were treated with cautery before hysterectomy. Following the hysterectomy, the uterus was examined, and the portion of the ParaGard IUD was confirmed to be embedded in the wall of the uterine cervix. The procedure was well tolerated by the patient and there were no complications.
Fig. 2.
Transabdominal ultrasound confirming the presence of the retained IUD (arrow) by a bright echogenic linear structure in the uterine cavity.
Fig. 3.
TVUS confirming the presence of the retained IUD (arrow) by a bright echogenic linear structure in the uterine cavity.
4. Discussion
Long-active reversible contraceptives are continually being used and are an effective option for preventing pregnancy [6]. Complications from IUDs may include, but are not limited to, cramping, ectopic pregnancy, embedment or fragmentation, expulsion, infertility, pelvic infection, uterine perforation, and vaginal bleeding [7]. Of note, fracture of the IUD is a very rare complication [8], with a prevalence rate of 1–2% [4]. The patient in this case report experienced a rare complication of IUD removal. Some case studies have been published about fractured IUDs, although this may be underreported. As this case study shows, the importance of mechanical complications, such as fracture of the IUD, needs to be emphasized. There are minimal data to describe the long-term risks of leaving a foreign piece of the IUD in the uterus. However, there may be concern about pain, infertility, infection, and bleeding [8]. IUDs can harbor infections with group A Streptococcus (GAS) or Actinomyces [9]. For this reason, careful and timely removal of the fractured IUD is necessary. Likewise, uterine perforation and migration of IUDs during implantation may lead to later fracture of the IUD wings when removed. Risk of perforation can increase with the use of excess force during IUD insertion [10].
Current practice of removing IUDs centers around an in-office procedure. The IUD is removed by securely grasping the strings at the external os and applying traction [7]. If resistance is met, then the removal should stop until the practitioner reassesses [7]. If the IUD is not removed by conventional methods, dilation of the cervix or ultrasound guidance should be considered [11,12]. Ultrasound-guided removal of an IUD is a cost-effective and less invasive than hysteroscopy [11]. Thus, hysteroscopy is usually reserved for removal of the retained IUD after these methods have been tried [13]. With the lack of post-operative complications after IUD removal by hysteroscopy [13,14], this method, as well as ultrasound guidance, might be a more successful and cost-effective first step in removal of any IUD in-patient or out-patient. Our patient in this case required a hysterectomy due to several unique factors. One of these was the location of the retained IUD in the uterine wall, which required a more invasive procedure for proper removal. This case highlights the importance of the IUD complication due to the requirement of a hysterectomy in order to safely remove the retained device.
Increased emphasis should be placed upon patients who may be at an increased risk for IUD misplacement. These include patients whose IUD may be embedded anatomically outside the uterus. In this case report, the patient's IUD was found via TVUS to be embedded in part of the cervix. This malposition of the IUD could have contributed to her history of irregular bleeding and more importantly to the fracture of the IUD upon removal in office. Risk for malposition includes small uterine size, congenital anatomical malformations, uterine forces during menstruation, and misplacement by healthcare providers [15,16]. Research shows that an IUD can be misplaced during years of use in the uterus due to anatomic, provider, or physiologic changes [17] and thus lead to lower rates of pregnancy prevention [15]. Copper IUDs, in particular, have been shown to be more likely to result in contraceptive failure if they are not in the right place [15]. For this reason, routine screening with ultrasound may need to be emphasized during routine care of patients who currently have IUDs. Although research does not yet connect IUD malposition with increased fracture risk, the concern for malposition remains for providers. With an IUD moving beyond the original position placed by the provider, excess force and difficultly may occur upon removing the device later, leading to potential fracture. Strong resistance when a provider pulls to remove the IUD may indicate the IUD is embedded in the uterine wall [12]. Being able to prevent the risk of retained or fractured IUDs is important for providers and patients alike.
In conclusion, this case highlights the importance of thorough evaluation of an IUD upon removal. Practitioners who work with IUD insertion and removal should remain informed about this rare complication. Risk of fracture during IUD removal should be better communicated between physicians and patients. A proper stepwise care plan for the physician is important, including decreasing risk by monitoring for proper IUD positioning. Likewise, careful IUD removal techniques in office can aid in better understanding of this rare complication. For example, facing too much resistance upon attempted removal of the IUD may warrant use of ultrasound guidance. This case study underlines the importance of careful IUD planning, from insertion to removal. Further research considering improved stepwise removal should be considered.
Acknowledgments
Contributors
All authors contributed to a significant portion of this manuscript
Conflict of Interest
The authors declare that they have no conflict of interest regarding the publication of this case report.
Funding
No funding from an external source supported the publication of this case report
Patient Consent
Obtained
Provenance and Peer Review
This case report was peer reviewed
Contributor Information
Jordan Sarver, Email: js492517@ohio.edu.
Melissa Cregan, Email: mc793917@ohio.edu.
References
- 1.Batur P., Kransdorf L.N., Casey P.M. Emergency contraception. Mayo Clin. Proc. 2016;91(6):802–807. doi: 10.1016/j.mayocp.2016.02.018. [DOI] [PubMed] [Google Scholar]
- 2.Kaneshiro B., Aeby T. Long-term safety, efficacy, and patient acceptability of the intrauterine Copper T-380A contraceptive device. Int. J. Women’s Health. 2010;2:211–220. doi: 10.2147/ijwh.s6914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dubovis M., Rizk N. Retained copper fragments following removal of a copper intrauterine device: two case reports. Case Rep. Womens Health. 2020 doi: 10.1016/j.crwh.2020.e00208. Published online April 24. (e00208) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilson S., Tan G., Baylson M., Schreiber C. Controversies in family planning: how to manage a fractured IUD. Contraception. 2013;88(5):599–603. doi: 10.1016/j.contraception.2013.07.007. [DOI] [PubMed] [Google Scholar]
- 5.Cheung M.-L., Rezai S., Jackman J.M. Retained intrauterine device (IUD): triple case report and review of the literature. Rosa-e-Silva J. Case Rep. Obstet. Gynecol. 2018;2018 doi: 10.1155/2018/9362962. (9362962) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Howard B., Grubb E., Lage M., Tang B. Trends in use of and complications from intrauterine contraceptive devices and tubal ligation or occlusion. Reprod. Health. 2017;14:70. doi: 10.1186/s12978-017-0334-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson B.A. Insertion and removal of intrauterine devices. Am. Fam. Physician. 2005;71(1):95–102. [PubMed] [Google Scholar]
- 8.Wakrim S., Lahlou L. Spontaneously expelled IUD and missing fragments in the uterine cavity. Radiol. Case Rep. 2020;15(9):1654–1656. doi: 10.1016/j.radcr.2020.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yu Wu C., Noska A. Intrauterine device infection causing concomitant streptococcal toxic shock syndrome and pelvic abscess with Actinomyces odontolyticus bacteraemia. BMJ Case Rep. 2016;10 doi: 10.1136/bcr-2015-213236. Published online March. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Neumann D., Graversen J., Pugh S. Intrauterine device embedded in omentum of postpartum patient with a markedly retroverted uterus: a case report. J. Med. Case Rep. 2017;11(299) doi: 10.1186/s13256-017-1480-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Verma U., Astudillo-Dávalos F., Gerkowicz S. Safe and cost-effective ultrasound guided removal of retained intrauterine device: our experience. Contraception. 2015;92(1):77–80. doi: 10.1016/j.contraception.2015.02.008. [DOI] [PubMed] [Google Scholar]
- 12.Prine L., Shah M. Long-acting reversible contraception: difficult insertions and removals. Am. Fam. Physician. 2018;98(5):303–309. [PubMed] [Google Scholar]
- 13.Asto R., Habana M.A. Hysteroscopic-guided removal of retained intrauterine device: experience at an academic tertiary hospital. Gynecol. Minim. Invasive Ther. 2018;7(2):56–60. doi: 10.4103/GMIT.GMIT_11_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prabhakaran S., Chuang A. In office retrieval of intrauterine contraceptive devices with missing strings. Contraception. 2011;83(2):102–106. doi: 10.1016/j.contraception.2010.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wildemeersch D., Hasskamp T., Goldstuck N. Malposition and displacement of intrauterine devices-diagnosis, management, and prevention. Clin. Obstet. Gynecol. Reprod. Med. 2016;2 Published online May 30. [Google Scholar]
- 16.Goldstuck N., Wildemeersch D. Role of uterine forces in intrauterine device embedment, perforation, and expulsion. Int. J. Women’s Health. 2014;6:735–744. doi: 10.2147/IJWH.S63167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goldbach A., Hava S., Patel H., Khan M. IUD embedment in the fallopian tube: an unexpected location for a translocated IUD. Radiol. Case Rep. 2018;13(4):788–792. doi: 10.1016/j.radcr.2018.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]