Abstract
Background.
The current study examined if fluctuation in in-the-moment impulsivity was more pronounced for adults with, versus without, a childhood history of ADHD and if ADHD group moderated the association between fluctuation in impulsivity and alcohol use behaviors.
Methods.
Two hundred and eleven adult drinkers (52% ADHD) completed a 10-day, 6 times/day, momentary assessment of state impulsivity. Self-reported trait impulsivity, alcohol problems, and frequency of 5+ drinks in the past 12 months were also assessed.
Results.
The ADHD group had more variability in three domains of state impulsivity (negative urgency, positive urgency, sensation seeking) compared to the nonADHD group. After including global trait impulsivity, the ADHD and nonADHD groups only differed on state sensation seeking. Fluctuation in two domains of state impulsivity were related to frequency of 5+ drinks (lack of planning: ADHD RR=3.60, p<0.001, nonADHD RR=0.90, p=0.81; negative urgency: ADHD RR=4.32, p=0.01, nonADHD RR=0.49, p=0.24) and number of different alcohol problems (lack of planning: ADHD RR=4.87, p<0.001, nonADHD RR=0.58, p=0.29; negative urgency: ADHD RR=4.96, p=0.01, nonADHD RR=0.24, p=0.04) for participants with a history of ADHD but were not related (or related to fewer problems) for those without childhood ADHD. Higher variability in positive urgency was related to more alcohol problems for the participants with childhood ADHD but not the nonADHD participants (ADHD RR=3.00, p=0.03, nonADHD RR=0.50, p=0.25).
Conclusions.
Findings highlight the importance of assessing fluctuation in several domains of impulsivity and may elucidate important treatment targets for alcohol problems for adults with ADHD histories.
Keywords: attention-deficit/hyperactivity disorder, alcohol, impulsivity, ecological momentary assessment
1. Introduction
Childhood attention-deficit/hyperactivity disorder (ADHD) predicts increased heavy episodic alcohol use (Barkley et al., 2008; Hechtman and Weiss, 1986; Molina et al., 2007), and alcohol use disorder (Charach et al., 2011; Lee et al., 2011). Research is needed to understand vulnerability to alcohol problems for this population beyond simplistic models of psychiatric comorbidity (Molina and Pelham, 2014). In the current study, we contribute to existing literature by examining variability in 5 domains of impulsivity (negative urgency: acting rashly in response to negative mood; positive urgency: acting rashly in response to positive mood; lack of perseverance: tendency to not finish tasks or distractability; lack of planning: acting without thinking; and sensation seeking: desire to seek out new or thrilling experiences; e.g, Whiteside and Lynam, 2001; Cyders and Smith, 2008), in real time, and how this variability may differentially relate to heavy alcohol use and problems for adults with childhood ADHD compared to adults without a history of childhood ADHD.
1.1. Trait Impulsivity, Alcohol Use, and ADHD
A large body of research demonstrates that higher trait impulsivity predicts alcohol use and problems (de Wit, 2009; Dick et al., 2010). Individuals with a history of childhood ADHD may engage in heavy alcohol use in part due to elevated trait impulsivity (Elkins et al., 2007; Howard et al., 2015; Molina et al., 2012; Rooney et al., 2012, Rooney et al., 2015). Our prior research has shown that two domains of impulsivity, trait positive and negative urgency, account for the association between childhood ADHD and alcohol problems in adulthood ~15 years later (Pedersen et al., 2016).
1.2. State Impulsivity, Alcohol Use, and ADHD
Many definitions of impulsigenic traits (e.g., negative urgency) actually contain situational components, highlighting the importance of examining fluctuation in impulsive behavior as opposed to global trait levels that aggregate across contexts. Variability in impulsive behavior (increases and decreases) within individuals may be an important index of inhibitory processes that are missed in trait level assessments and which may relate to substance use above and beyond the risk posed by trait levels. Consistent with this possibility, research has shown that self-reported, “trait-like,” measures of affective instability are only modestly correlated with ecological momentary assessment (EMA) measurements of variability in affect (Solhan et al., 2009).
Research has begun to demonstrate the importance of assessing fluctuations in impulsivity in the real world via self-report (Ansell et al., 2015; Tomko et al., 2014; Tomko et al., 2015) and behavioral task performance (McCarthy et al., 2018). Momentary levels of impulsivity have been shown to vary within individuals both across and within days (Tomko et al., 2014). Additionally, individuals with borderline personality disorder have been shown to have more variability in impulsivity than individuals without this disorder (Tomko et al., 2014). Increased emotion dysregulation among individuals with ADHD (Sobanski et al., 2010) may contribute to increased variability in positive and negative urgency as mood shifts increase fluctuation in impulsivity.
Research has begun to demonstrate the importance of examining fluctuations in risk factors for alcohol use in individuals with ADHD. For example, in a small sample of adult smokers with ADHD, hyperactivity-impulsivity symptoms momentarily increased prior to smoking in frustrating situations (Mitchell et al., 2014). A separate EMA study of adults with ADHD found that transdermal nicotine administration momentarily reduced negative mood and impulsivity for both abstinent smokers and nonsmokers (Gehricke et al., 2009). Importantly, EMA research on ADHD populations has been confined to small samples, utilized DSM criteria instead of behaviors likely to vary daily, or has focused on children.
1.3. Current Study
In the current study we hypothesized that adults with ADHD histories ( “ADHD”) would have more variability across 10 days in positive and negative urgency than adults without ADHD histories (“nonADHD”). We did not have a priori hypotheses about variability in the other 3 impulsivity domains. Second, we hypothesized that elevated variability in impulsivity, particularly in positive and negative urgency, would be more strongly related to alcohol use/problems for those with compared to without a history of ADHD. We examined these aims in a well-powered study (estimated power = .80 to detect small effects between the ADHD/nonADHD groups, d = .40, with our sample size: G*Power3, Faul et al., 2007, 2009) over and above corresponding impulsivity domains assessed with traditional trait-based measures (UPPS-P) as well as mean level of EMA-measured impulsivity.
2. Material and methods
2.1. Participants
Participants were 211 adult drinkers (n = 109 with childhood ADHD; 10 currently medicated; 38 currently endorsing ADHD symptoms at diagnostic threshold); n = 102 without childhood ADHD). The sample was 75% male (Mage = 27.9; range 21-35 years, SD = 4.06). Participants were recruited into the study either from the community (n = 124: posted fliers, Craigslist advertisements) or from the Pittsburgh ADHD Longitudinal Study (n = 87: PALS). The majority of participants identified as White/European American (67.3%), 31.8% identified as Black/African American, and 0.9% identified as Asian or another race. Participants were required to be between 21 and 36 years old. Participants in the current study completed an alcohol administration (data to be published elsewhere) and therefore were required to have consumed alcohol at least once in the past month (Mpast 30 day frequency = 5.75 days, SD = 1.41; Mpast 30 day quantity = 3.53 drinks, SD = 2.53) and to have consumed at least the equivalent amount of alcohol in the past six months as would be given during the laboratory alcohol administration (target BrAC of .08%). Additionally, participants were excluded if they were currently (or had ever) abstaining from alcohol due to fear of having a problem, had ever received treatment for an alcohol or substance use disorder, had significant medical or mental illness (e.g., psychotic disorders), were pregnant or breastfeeding, weighed over 250 pounds, or were taking medication for which alcohol use is contraindicated. During enrollment, participants with and without childhood ADHD were matched on self-reported past 30 day drinking behavior to reduce differences in acute tolerance that could affect alcohol response. A similar matching strategy for alcohol use was used across Black and White drinkers.
2.2. Study Design
Study procedures were approved by the University of Pittsburgh’s Institutional Review Board. Following participation in a laboratory protocol that also included completion of questionnaires (e.g., trait impulsivity), the majority of our participants started the EMA protocol on the following Friday (n=14 had a delayed start date due to extenuating circumstances: e.g., travel schedule). Participants used their personal smartphone or a study smartphone. All participants were provided in-person instruction on how to complete the prompts (e.g., wait until done driving). Prompts were sent via text by an automated pre-programmed computer system. The first assessment was sent via text 15 minutes after self-reported expected wake time and the last assessment was sent to participants 15 minutes prior to reported expected bedtime. The rest of the day was then split into 4 equal segments spanning the 2 hrs after self-reported wake time to 2 hrs prior to self-reported bedtime. Within each of these segments prompts were randomly sent resulting in four additional assessments. Participants had 10 minutes to complete the prompt and received a reminder text five minutes after the first prompt was sent. They could earn up to $110.00 for completing at least 80% of the assessments. Participants who completed less than 80% of the EMA prompts received corresponding compensation (e.g., 60% completion received $66.00/60% of $110.00). On average participants completed 67% (~40 of the 60 total prompts sent) of the assessments across the 10-day period.
2.3. ADHD History
Childhood ADHD (ADHD = 1, nonADHD = 0).
Participants recruited from the community (n = 58 ADHD, n = 66 nonADHD) completed a phone screen of DSM-IV ADHD symptoms from childhood and a parallel informant report was obtained over the phone. For the ADHD group, participants and the informant each separately endorsed at least 6 out of 18 symptoms of ADHD occurring prior to age 12 (2 reported symptoms below this threshold but indicated a positive history of ADHD diagnosis in childhood). Community participants without ADHD were enrolled if both the participant and informant endorsed fewer than 6 ADHD symptoms. ADHD group participants recruited from the PALS were diagnosed in childhood. A nonADHD demographically similar comparision sample was later recuited into PALS (see (Molina et al., 2017) for additional details of PALS).
2.4. Measures obtained during the laboratory visit
Demographics.
Participants reported their sex (male = 1, female = 0), race, and age. These demographic variables were included as covariates in analyses.
Trait Impulsivity.
Five impulsivity facets were assessed using the 59-item UPPS-P impulsive behavior scale (Cyders et al., 2007; Whiteside and Lynam, 2001): lack of planning (11 items: α = .90; e.g., “My thinking is usually careful and purposeful”), sensation seeking (12 items: α = .87; e.g., “I generally seek new and exciting experiences and sensations”), negative urgency (12 items: α = .92; e.g., “In the heat of an argument, I will often say things that I later regret”), positive urgency (14 items: α = .95; e.g., “When I am really excited, I tend not to think of the consequences of my actions”), and lack of perseverance (10 items: α =.85; e.g., “I generally like to see things through to the end”). Response options ranged from 1 (agree strongly) to 4 (disagree strongly). Responses were coded so that higher numbers meant higher impulsivity.
Frequency of 5+ drinks per occasion.
Alcohol use in the past 12 months1 was assessed with the Substance Use Questionnaire (Molina and Pelham, 2003) which includes questions about alcohol use adapted from existing measures (Jessor et al., 1989; National Household Study on Drug Abuse, 1992). The outcome for the current study was frequency of drinking 5+ drinks per occasion. The scale of this item ranged from 0: not at all to 11: several times a day (range 0-11; M = 3.28, SD = 2.61; a response of “3” = 8-11 times).
Alcohol problems.
A modified version of the Young Adult Alcohol Problems Screening Test (YAAPST): (Hurlburt and Sher, 1992) was used to assess alcohol problems in adulthood. This 36-item questionnaire (response options: 0 = none or not in the past year to 3 = more than 5 times) assesses how frequently problems occurred while drinking or as a result of drinking within the past year. The YAAPST has good reliability (e.g., (Hurlburt and Sher, 1992)). For the current study, the number of different problems reported in the past year1 (range 0-22; M = 4.31; SD = 4.45) was analyzed.
2.5. Measures obtained during EMA
State Impulsivity.
We adapted 19 items from the UPPS-P to assess lack of planning (3 items; α = .87), sensation seeking (4 items; α = .81), negative urgency (4 items; α = .83), positive urgency (4 items; α = .91), and lack of perseverance (4 items; α = .81). Participants were asked to report on their experiences since the last EMA prompt (the morning report would include the time since the bedtime assessment). Response options ranged from 1 (agree strongly) to 4 (disagree strongly). Responses were recoded so that higher numbers meant higher impulsivity. Items were selected for their adaptability to assessment of current state. Items that were global (e.g., I have a reserved and cautious attitude toward life) were excluded. Questions were also selected based on likelihood of occurrence or change in 2-3 hour period and were then modified to assess “state” behavior and experiences. For example, the original “I have trouble controlling my impulses” was modified to “Since the last assessment I had trouble controlling my impulses.”
2.6. Analytic Plan
Analyses were conducted using generalized linear models in R 3.3.4 (Team, 2018) with the package MASS for negative binomial models (Venables and Ripley, 2002). The EMA protocol produced up to 60 data points across 10 days. To improve the reliability of the estimates of variability, we only included in analyses the data from participants who completed at least 10% of their prompts (i.e., one days’ worth). This resulted in excluding data for eight participants (5 from the ADHD group, 3 from the nonADHD group) from the analyses (final n = 203).
We first tested whether or not childhood ADHD was associated with increased variability in impulsivity. We computed a within-person standard deviation (SD) across all momentary assessments of each facet of impulsivity across the 10-day study period, and we regressed this variable for each facet of impulsivity on ADHD group. Cases with extreme variability (>.80, which was larger then the 95%ile for all SD) were Windsorized.
Because only a few studies have examined within-person variability in impulsivity, we chose to focus the current study on a straightforward measure of variability. We made this decision since no research has compared models of variability in momentary reports of impulsivity and because a recent meta-analysis on affective instability that demonstrated that more complex approaches (e.g., mean-squared successive difference) did not outperform a more straightforward standard deviation calculation when examining negative affect instability (Dejonckheere et al., 2019; Jahng et al., 2018; Tomko et al., 2014).
Our second aim was to test whether or not variability in impulsivity was associated with heavy alcohol use and problems and if this differed as a function of ADHD history. Because alcohol outcomes are typically not normally distributed, we tested a sequence of models to determine which distribution best fit each outcome. We chose a negative binomial distribution based on parsimony and model fit using multiple indicators (Akaike Information Criteria and Bayesian Information Criteria values, as well as the Vuong test for non-nested models).
We regressed heavy alcohol use and problems on ADHD group and variability in each facet of impulsivity and their associated interactions after accounting for sex, age, race, recruitment method (PALS or community), and global self-report of trait impulsivity. Separate models were run for each domain of impulsivity. We compared these results to models controlling for average levels of EMA-reported impulsivity facets across the 10 days (EMA average impulsivity); findings were nearly identical in magnitude, sign and significance. Because prior research has suggested that significance tests are unreliable indicators of the presence of an interaction when the outcome is nonlinear (such as in a logistic or count outcome) (Ai and Norton, 2003), we used −2 log-likelihood differences as an indicator to determine whether including an interaction term improved fit. We then probed models where an interaction term appeared to improve fit, and estimated predicted counts/probabilities of alcohol outcomes at the mean of the covariates across representative levels of both variables involved in the interaction (King et al., 2000). All predictors and covariates (save ADHD group) were centered prior to testing interactions.
3. Results
3.1. Descriptive Results.
EMA reports of impulsivity averaged from 1.80 (for positive urgency) to 2.88 (sensation seeking), with a range of 1 – 4. ADHD group participants had higher average EMA reported negative urgency (t(198) = −3.54, p = 0.0005, 95% CI [−0.42, −0.12], MADHD = 1.65, MnonADHD = 1.38), positive urgency (t(195) = −3.43, p = 0.0007, 95% CI [−0.38, −0.10], MADHD = 1.53, MnonADHD = 1.29), and sensation seeking (t(201) = −3.59, p = 0.0004, 95% CI [−0.48, −0.14], MADHD = 1.89, MnonADHD = 1.58) compared to nonADHD group participants. Within-person SDs averaged .23 (positive urgency) to .36 (lack of planning). To illustrate, a typical participant reported an average of 1.8 for positive urgency across their EMA responses (roughly, Disagree), and 68% of their reports ranged from 1.56 to 2.04 across assessments. A highly variable participant’s scores might range from 1 (Strongly Disagree) to 3 (Agree) across assessments. Variability in all facets of impulsivity were positively correlated with both global self-report of trait impulsivity and with EMA averages of impulsivity (see Table 1).
Table 1.
Association between Variability and EMA Average and Self-reported Trait of Each Impulsivity Facet.
| EMA Variability | |||||
|---|---|---|---|---|---|
| NU | PU | SS | LP | LPer | |
| EMA Average Level | 0.50*** | 0.53*** | 0.39*** | 0.44*** | 0.33*** |
| Trait Self-report | 0.47*** | 0.46*** | 0.33*** | 0.15* | 0.21* |
Note:
Pearson correlations significant at p < .05
Significant at p < .001.
EMA Variability = Mean of the standard deviations of each impulsivity domain across the ecological momentary assessment (EMA) protocol. NU = negative urgency, PU = positive urgency, SS = sensation seeking, LP = Lack of Planning, LPer = Lack of Perseverance.
3.2. Association between ADHD and Variability in EMA-assessed Impulsivity
ADHD group participants had higher variability in negative urgency, positive urgency, and sensation seeking compared to nonADHD participants without accounting for covariates and trait impulsivity (see Table 2). While ADHD group significantly predicted variability in impulsivity facets controlling for demographic covariates (i.e., sex, age, race, recruitment method), these effects were not robust to the addition of global trait impulsivity to the models. ADHD only predicted variability in sensation seeking after controlling for global trait impulsivity (β = 0.14, p = 0.03). Sex was the only covariate associated with variability in sensation seeking (b = .18, p = 0.03); male participants reported more than female participants.
Table 2.
Mean level of EMA Variability in Impulsivity Facets for Adults with and without a history of ADHD.
| nonADHD | ADHD | t | df | p | |
|---|---|---|---|---|---|
| Negative Urgency | 0.256 | 0.321 | −3.06 | 199 | .003 |
| Positive Urgency | 0.205 | 0.279 | −2.79 | 196 | .006 |
| Sensation Seeking | 0.281 | 0.345 | −2.63 | 197 | .009 |
| Lack of Planning | 0.361 | 0.408 | −1.74 | 201 | .084 |
| Lack of Perseverance | 0.330 | 0.364 | −1.61 | 197 | .109 |
Note: All significant mean level differences at p < .05 between ADHD and nonADHD are in bold.
3.3. ADHD X Impulsivity Variability and Alcohol Use Behaviors
Our second aim was focused on examining how variability in impulsivity domains related to frequency of 5+ drinks and alcohol problems as a function of ADHD history. The interaction between variability in lack of planning and ADHD group was significant for both frequency of 5+ drinks/occasion and alcohol problems (see Table 3). Specifically, at the mean of the covariates, variability in lack of planning was associated with a higher frequency of 5+ drinks/occasion for participants with a history of ADHD, but not for those without (ADHD RR = 3.60, p < 0.001, nonADHD RR = 0.90, p = 0.81; See Figure 1). A similar pattern was found for the interaction between variability in lack of planning and ADHD history in relation to alcohol problems (ADHD RR = 4.87, p < 0.001, nonADHD RR = 0.58, p = 0.29; See Figure 2).
Table 3.
Interaction between Variability in Lack of Planning and ADHD in Relation to Frequency of 5+ drinks/occasion and Number of Alcohol Problems
| Frequency of 5+ drinks | Number of Alcohol Problems | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| b | SE | p value | RR | 95% CI | b | SE | p value | RR | 95% CI | |
| ADHD | −0.37 | 0.12 | 0.002 | 0.69 | [0.54, 0.88] | −0.26 | 0.15 | 0.075 | 0.77 | [0.57, 1.04] |
| Rec. Source | −0.18 | 0.15 | 0.221 | 0.84 | [0.63, 1.12] | −0.32 | 0.18 | 0.073 | 0.73 | [0.50, 1.04] |
| Sex | 0.38 | 0.15 | 0.012 | 1.46 | [1.09, 1.96] | −0.13 | 0.18 | 0.460 | 0.88 | [0.62, 1.25] |
| Age | −0.02 | 0.02 | 0.136 | 0.98 | [0.95, 1.01] | −0.06 | 0.02 | 0.002 | 0.94 | [0.91, 0.98] |
| Race | 0.04 | 0.13 | 0.744 | 1.04 | [0.80, 1.36] | 0.05 | 0.16 | 0.733 | 1.06 | [0.77, 1.45] |
| Trait LP | 0.23 | 0.11 | 0.042 | 1.26 | [0.99, 1.59] | 0.50 | 0.14 | 0.0003 | 1.64 | [1.24, 2.18] |
| SD LP | −0.10 | 0.43 | 0.810 | 0.90 | [0.39, 2.10] | −0.55 | 0.52 | 0.293 | 0.58 | [0.20, 1.65] |
| SD LP X ADHD | 1.38 | 0.60 | 0.020 | 3.99 | [1.20, 13.41] | 2.13 | 0.72 | 0.003 | 8.45 | [1.95, 36.77] |
Note: Rec. Source= recruited from community (0) or PALS (1). SD LP= variability in Lack of Planning. Trait LP = self-report of lack of planning assessed with the UPPS-P. ADHD = 1, nonADHD = 0. SD LP main effect results should be interpreted as the estimate for the nonADHD group as a function of this group being coded as 0 in analyses. Bold values indicate a significant effect at p < .05.
Figure 1:
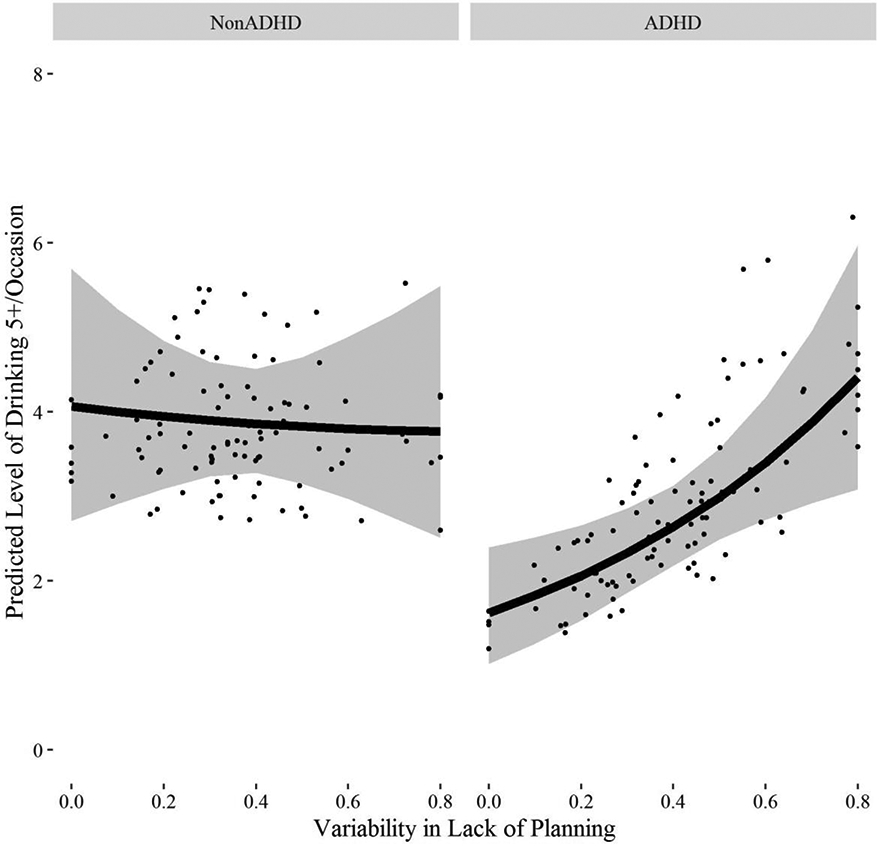
Illustration of the interaction between childhood ADHD and variability in lack of planning in relation to the frequency of 5+ drinks/occasion. Effects of childhood ADHD and nonADHD are presented separately.
Figure 2:
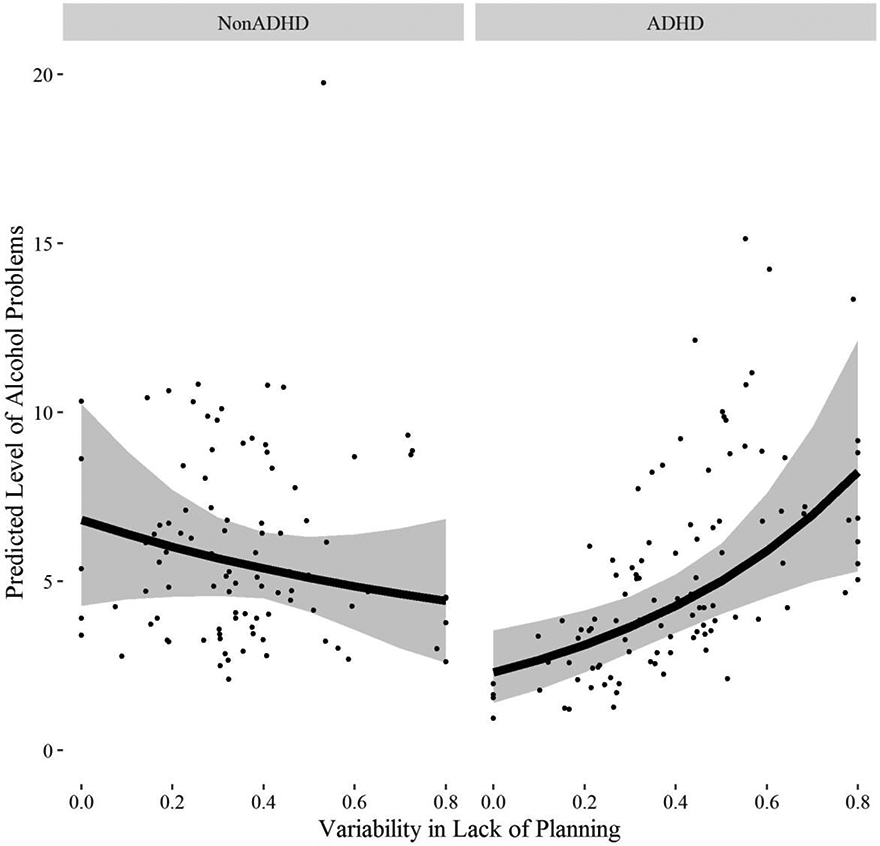
Illustration of the interaction between childhood ADHD and variability in lack of planning in relation to the number of alcohol problems. Effects of childhood ADHD and nonADHD are presented separately.
ADHD group also moderated the association between negative urgency and frequency of 5+ drinks/occasion and alcohol problems (see Table 4). For participants with an ADHD history, variability in negative urgency was associated with an increased number of drinking 5+ drinks/occasion, but not for those without (ADHD RR = 4.32, p = 0.01, nonADHD RR = 0.49, p = 0.24; See Figure 3). There was a similar pattern of findings for the effects of variability in negative urgency on alcohol problems for those with an ADHD history, while the opposite effect was found for those without (ADHD RR = 4.96, p = 0.01, nonADHD RR = 0.24, p = 0.04; See Figure 4).
Table 4.
Interaction between Variability in Negative Urgency and ADHD in Relation to Frequency of 5+ drinks/occasion and Number of Alcohol Problems
| Frequency of 5+ drinks | Number of Alcohol Problems | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| b | SE | p value | RR | 95% CI | b | SE | p value | RR | 95% CI | |
| ADHD | −0.36 | 0.12 | 0.003 | 0.70 | [0.55, 0.89] | −0.32 | 0.14 | 0.024 | 0.72 | [0.55, 0.96] |
| Rec. Source | −0.10 | 0.15 | 0.503 | 0.91 | [0.68, 1.21] | −0.09 | 0.17 | 0.591 | 0.91 | [0.64, 1.30] |
| Sex | 0.40 | 0.15 | 0.008 | 1.49 | [1.11, 2.00] | −0.04 | 0.17 | 0.814 | 0.96 | [0.68, 1.35] |
| Age | −0.02 | 0.02 | 0.111 | 0.98 | [0.95, 1.01] | −0.06 | 0.02 | 0.001 | 0.94 | [0.91, 0.98] |
| Race | 0.04 | 0.13 | 0.767 | 1.04 | [0.80, 1.36] | 0.10 | 0.15 | 0.508 | 1.11 | [0.82, 1.50] |
| Trait NU | 0.17 | 0.10 | 0.100 | 1.19 | [0.97, 1.45] | 0.60 | 0.12 | 0.0001 | 1.82 | [1.44, 2.31] |
| SD NU | −0.71 | 0.60 | 0.236 | 0.49 | [0.16, 1.54] | −1.43 | 0.71 | 0.044 | 0.24 | [0.06, 0.90] |
| SD NU X ADHD | 2.17 | 0.76 | 0.004 | 8.76 | [1.97, 39.41] | 3.03 | 0.90 | 0.0007 | 20.77 | [3.86, 112.14] |
Note: Rec. Source= recruited from community (0) or PALS (1). SD NU = variability in negative urgency. Trait NU = self-report of negative urgency assessed with the UPPS-P. ADHD = 1, nonADHD = 0. SD NU main effect results should be interpreted as a the estimate for the nonADHD group as a function of this group being coded as 0 in analyses. Bold values indicate a significant effect at p < .05.
Figure 3:
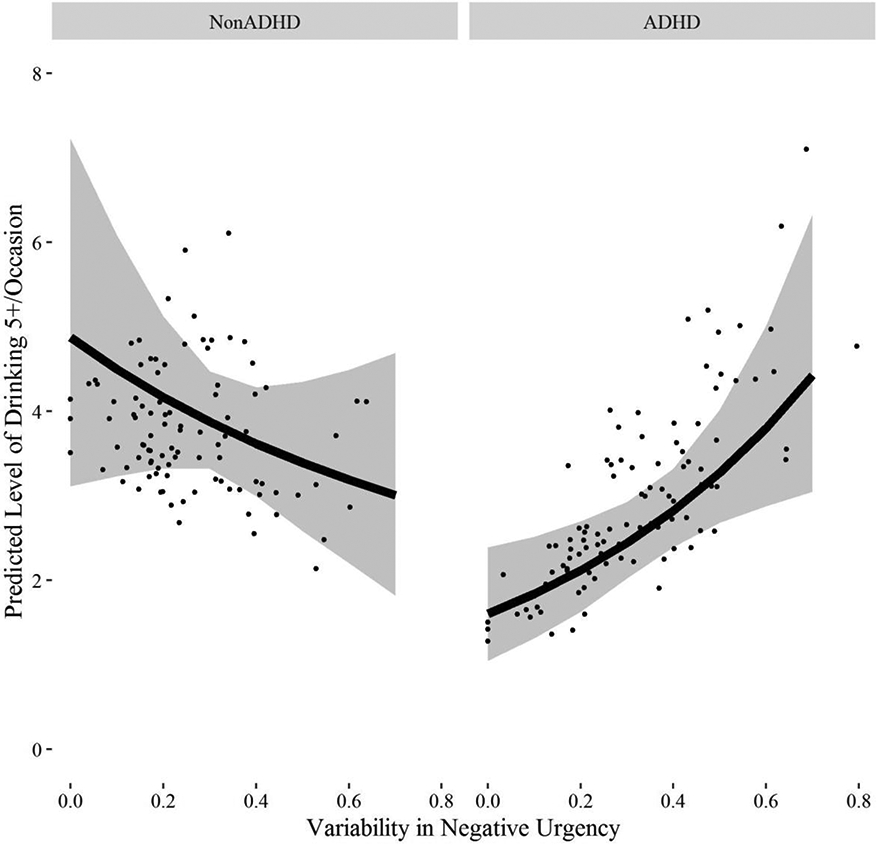
Illustration of the interaction between childhood ADHD and negative urgency in relation to the frequency of 5+ drinks/occasion. Effects of childhood ADHD and nonADHD are presented separately.
Figure 4:
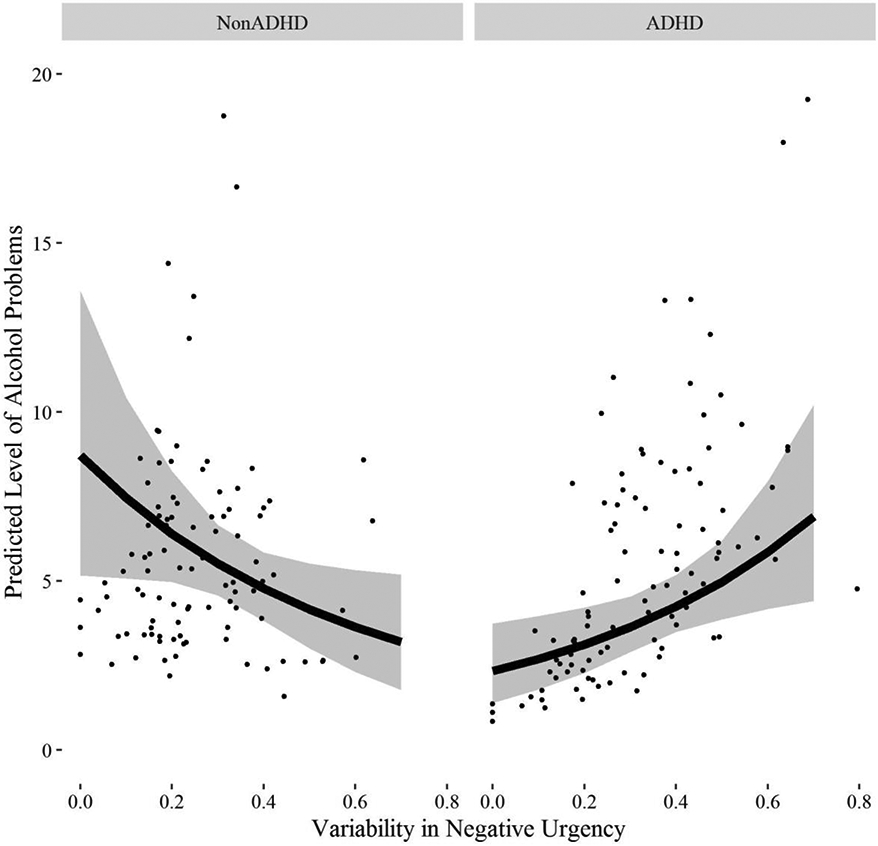
Illustration of the interaction between childhood ADHD and negative urgency in relation to the number of alcohol problems. Effects of childhood ADHD and nonADHD are presented separately.
Finally, ADHD group moderated the association between positive urgency and alcohol problems (not frequency of 5+ drinks; see Table 5). Individuals with an ADHD history exhibited stronger associations between variability in positive urgency and alcohol problems than those without (ADHD RR = 3.00, p = 0.03, nonADHD RR = 0.50, p = 0.25; See Figure 5). There were no statistically significant interactions between ADHD group and variability in sensation seeking or lack of perseverance and the main effects between variability in these domains and alcohol behaviors were also not significant.
Table 5.
Interaction between Variability in Positive Urgency and ADHD in Relation to Frequency of 5+ drinks/occasion and Number of Alcohol Problems
| Frequency of 5+ drinks | Number of Alcohol Problems | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| b | SE | p value | RR | 95% CI | b | SE | p value | RR | 95% CI | |
| ADHD | −0.34 | 0.12 | 0.005 | 0.71 | [0.56, 0.91] | −0.19 | 0.14 | 0.194 | 0.83 | [0.63, 1.10] |
| Rec. Source | −0.13 | 0.15 | 0.365 | 0.88 | [0.65, 1.17] | −0.24 | 0.18 | 0.172 | 0.79 | [0.55, 1.12] |
| Sex | 0.33 | 0.15 | 0.029 | 1.39 | [1.04, 1.87] | −0.22 | 0.17 | 0.197 | 0.80 | [0.56, 1.13] |
| Age | −0.02 | 0.02 | 0.179 | 0.98 | [0.95, 1.01] | −0.05 | 0.02 | 0.004 | 0.95 | [0.92, 0.99] |
| Race | 0.03 | 0.13 | 0.833 | 1.03 | [0.79, 1.34] | 0.02 | 0.16 | 0.912 | 1.02 | [0.75, 1.39] |
| Trait PU | 0.21 | 0.10 | 0.045 | 1.23 | [1.00, 1.51] | 0.44 | 0.12 | 0.0003 | 1.55 | [1.22, 1.99] |
| SD PU | −0.22 | 0.49 | 0.660 | 0.81 | [0.31, 2.09] | −.69 | 0.60 | 0.252 | 0.50 | [0.15, 1.73] |
| SD PU X ADHD | 0.83 | 0.62 | 0.182 | 2.28 | [0.67, 7.77] | 1.79 | 0.75 | 0.017 | 6.00 | [1.35, 26.3] |
Note: Rec. Source= recruited from community (0) or PALS (1). SD PU = variability in positive urgency. Trait PU = self-report of positive urgency assessed with the UPPS-P. ADHD = 1, nonADHD = 0. SD PU main effect results should be interpreted as a the estimate for the nonADHD group as a function of this group being coded as 0 in analyses. Bold values indicate a significant effect at p < .05.
Figure 5:
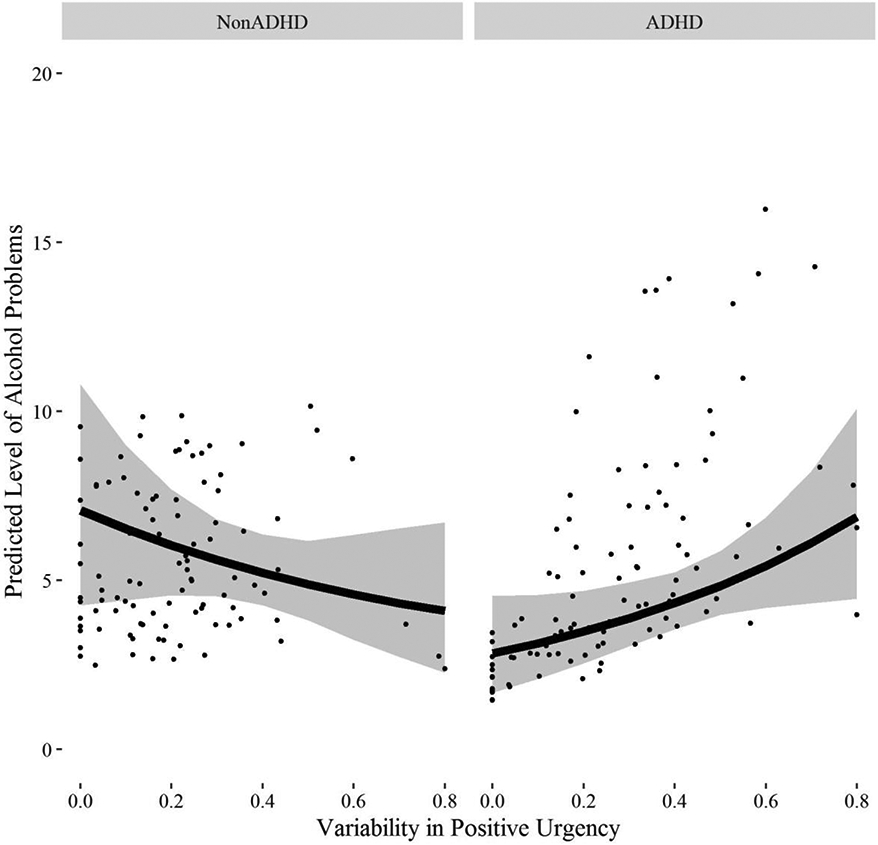
Illustration of the interaction between childhood ADHD and positive urgency in relation to the number of alcohol problems. Effects of childhood ADHD and nonADHD are presented separately.
4. Discussion
These findings are the first to demonstrate the importance of examining fluctuation in multiple domains of impulsivity to understand ADHD-related alcohol risk. Our results showed that multiple domains of impulsivity (negative urgency, positive urgency, sensation seeking) vary more for individuals with a history of ADHD across a 10 day period compared to those without this history. Further, increased variability in lack of planning, negative urgency, and positive urgency were related to alcohol behaviors for the ADHD group but were not related (or related in the opposite direction) for the group without an ADHD history.
The ADHD group had more fluctuation in 3 of 5 domains of impulsivity prior to accounting for trait level impulsivity. However, only fluctuation in sensation seeking remained significantly higher for the ADHD group compared to those without an ADHD history after accounting for the corresponding impulsivity trait in analyses. Given the association between trait impulsivity and fluctuation in impulsivity it may be the case that higher trait impulsivity is driving the increased fluctuation in impulsivity facets for individuals with a history of ADHD. While the sensation seeking finding was unexpected, this may indicate that individuals with a history of ADHD are more influenced by environmental context in their engagement in thrill seeking behaviors than individuals without a history of ADHD. Prior research has provided tentative support for individuals with childhood ADHD being more influenced by peers (Belendiuk et al., 2016) than those without. Contextual factors, such as risk-taking peers, may result in increased behavioral risk-taking for those with ADHD histories. Conversely, being with friends who are engaged in calm, routine activities may dampen sensation seeking more for this population.
Variability in three impulsivity domains – lack of planning, negative urgency, and positive urgency -- were related to alcohol use behaviors for the ADHD group. Attentional control deficits that characterize individuals with ADHD may partly explain these findings. Weafer and colleagues (2011) found that poor attentional control was associated with increased quantity of alcohol consumed for adults with but not without ADHD. In conjunction with momentary shifts in lack of planning, attentional control deficits may overload the ability to restrain from engaging in behaviors that result in heavy episodic drinking and alcohol problems. Another possibility is that variability is an index of dysregulation that is a separate risk factor. An individual who spends periods of time with reduced and then elevated impulsivity may not be aware that they are in a state of increased likelihood of drinking more alcohol or needing to use protective behavioral strategies to reduce the likelihood of experiencing alcohol problems.
Variability in negative urgency was related to frequency of heavy drinking and alcohol problems for the ADHD group over and above trait negative urgency. Variability in positive urgency was related to alcohol problems (not frequency of 5+ drinks) for the ADHD group only. These results directly extend recent laboratory findings that trait negative urgency was related to higher alcohol craving and higher breath alcohol content in negative (but not neutral) mood conditions (VanderVeen et al., 2016). Adults with a history of ADHD may experience more reactivity to events that increase/decrease mood which could strengthen the connection between variability in urgency and alcohol use behaviors.
While the current study had many strengths including measurement of traditional trait level, average EMA level, and EMA-assessed variability in multiple domains of impulsivity, there are several limitations. First, our assessment of impulsivity utilized self-report; variability in behavioral disinhibition task performance may yield different associations. Second, EMA-measured heavy alcohol use/problems were infrequent during the 10-day protocol so we examined associations with alcohol use behaviors from the prior 12 months. Future research with a heavier drinking sample would allow for inclusion of EMA-measured heavy drinking and problems and can focus on disentangling in-the-moment temporal associations. Third, participants with and without a history of ADHD were matched on recent alcohol use so between group comparisons on alcohol problems and heavy drinking are not generalizabile. Fourth, while we observed some participant differences as a function of recruitment source (i.e., the community recruited sample was younger and had a higher percentage of female and Black/African American participants), and the community sample recruitment was not based on a full diagnostic interview, the sample heterogeneity increased its representativeness (including individuals with and without specialty clinic diagnosis and treatment). Although supplemental analyses (not presented) did not find recruitment source to be a statistically significant moderator of the associations presented, future replication with a complete diagnostic assessment battery would provide a helpful validation of these findings. It would also allow examination of potentially important comorbidities (e.g., depression, conduct disorder) alongside persistence of ADHD into adulthood. Persistent ADHD may coincide with more fluctuations in state impulsivity and examination of these factors may illuminate important subgroups within the heterogeneous population of individuals with ADHD histories. Lastly, although our sample included over 50 females, most participants were male which limits ability to examine possible sex differences.
5. Conclusions
Despite these limitations, the current study points to the possibility that fluctuations in negative urgency, lack of planning, and to a lesser extent positive urgency, are important when considering alcohol risk for individuals with a history of ADHD over and and above elevated impulsigenic “traits.” Treatments focused on reducing fluctuations in impulsive behaviors or alerting people with histories of ADHD to a shift in impulsivity prior to drinking may decrease their risk for negative alcohol outcomes.
Highlights:
Fluctuation in impulsivity may increase risk for alcohol problems
Adults with a history of ADHD experience more fluctuation in impulsivity
Fluctuation in impulsivity relates to alcohol use and problems for those with ADHD
Acknowledgments
Role of funding source. Funding for this study was provided by the National Institute on Alcohol Abuse and Alcoholism (NIAAA): K01AA021135, R37A011873, K21AA000202; the National Institute on Drug Abuse (NIDA) R01 DA012414 and the ABMRF/The Foundation for Alcohol Research.
Footnotes
As a result of a programming error 41 participants reported their frequency of 5+ drinks/occasion and number of alcohol problems in the past 6 months instead of the past 12 months like the majority of the sample. Analyses were conducted dropping these 41 participants from analyses and the pattern of results remained the same.
Conflict of Interest. The authors have no conflicts of interest to declare.
References
- Ai C, Norton EC, 2003. Interaction terms in logit and probit models. Econ. Lett 80, 123–9. [Google Scholar]
- Ansell EB, Laws HB, Roche MJ, Sinha R, 2015. Effects of marijuana use on impulsivity and hostility in daily life. Drug. Alcohol. Depend 148, 136–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barkley RA, Murphy KR, Fischer M, 2008. ADHD in adults: What the science says. The Guilford Press, New York. [Google Scholar]
- Belendiuk KA, Pedersen SL, King KM, Pelham WE, Molina BSG, 2016. Change over time in adolescent and friend alcohol use: Differential associations for youth with and without childhood attention-deficit/hyperactivity disorder (ADHD). Psychol. Addict. Behav 30, 29–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charach A, Yeung E, Climans T, Lillie E, 2011. Childhood attention-deficit/hyperactivity disorder and future substance use disorders: comparative meta-analyses. J. Am. Acad. Child. Adolesc. Psychiatry 50, 9–21 [DOI] [PubMed] [Google Scholar]
- Cyders MA, Smith GT, Spillane NS, Fischer S, Annus AM, Peterson C, 2007. Integration of impulsivity and positive mood to predict risky behavior: development and validation of a measure of positive urgency. Psychol. Assess 19, 107–118. [DOI] [PubMed] [Google Scholar]
- de Wit H, 2009. Impulsivity as a determinant and consequence of drug use: a review of underlying processes. Addict. Biol 14, 22–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dejonckheere E, Mestdagh M, Houben M, Rutten I, Sels L, Kuppens P, Tuerlinckx F, 2019. Complex affect dynamics add limited information to the prediction of psychological well-being. Nature human behaviour. [DOI] [PubMed] [Google Scholar]
- Dick DM, Smith G, Olausson P, Mitchell SH, Leeman RF, O'Malley SS, Sher K, 2010. Understanding the construct of impulsivity and its relationship to alcohol use disorders. Addict. Biol 15, 217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkins IJ, Mcgue M, Iacono WG, 2007. Prospective effects of attention-deficit/hyperactivity disorder, conduct disorder, and sex on adolescent substance use and abuse. Archives of General Psychiatry. 64, 1145–1152. [DOI] [PubMed] [Google Scholar]
- Gehricke JG, Hong N, Whalen CK, Steinhoff K, Wigal TL, 2009. Effects of transdermal nicotine on symptoms, moods, and cardiovascular activity in the everyday lives of smokers and nonsmokers with attention-deficit/hyperactivity disorder. Psychol. Addict. Behav 23, 644–655. [DOI] [PubMed] [Google Scholar]
- Hechtman L, Weiss G, 1986. Controlled prospective fifteen year follow-up of hyperactives as adults: Non-medical drug and alcohol use and anti-social behaviour. Can. J. Psychiatry 31, 557–567. [DOI] [PubMed] [Google Scholar]
- Howard AL, Molina BS, Swanson JM, Hinshaw SP, Belendiuk KA, Harty SC, Arnold LE, Abikoff HB, Hechtman L, Stehli A, Greenhill LL, Newcorn JH, Wigal T, 2015. Developmental progression to early adult binge drinking and marijuana use from worsening versus stable trajectories of adolescent ADHD and delinquency. Addict. 110, 784–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurlburt SC, Sher KJ, 1992. Assessing alcohol problems in college students. J. Am. Coll. Health 41, 49–58. [DOI] [PubMed] [Google Scholar]
- Jahng S, Wood PK, Trull TJ, 2008. Analysis of affective instability in ecological momentary assessment: Indices using successive difference and group comparison via multilevel modeling. Psychol. Methods 13, 354–375. [DOI] [PubMed] [Google Scholar]
- Jessor R, Donovan JE, Costa FM, 1989. Health behavior questionnaire. Boulder, CO: Institute of Behavioral Science, University of Colorado. [Google Scholar]
- King G, Tomz M, Wittenberg J, 2000. Making the most of statistical analyses: Improving interpretation and presentation. Am. J. Pol. Sci 44, 341–355. [Google Scholar]
- Lee SS, Humphreys KL, Flory K, Liu R, Glass K, 2011. Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: a meta-analytic review. Clin. Psychol. Rev 31, 328–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy DE, Minami H, Bold KW, Yeh VM, Chapman G, 2018. Momentary assessment of impulsive choice and impulsive action: Reliability, stability, and correlates. Addict. Behav 83, 130–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell JT, Dennis MF, English JS, Dennis PA, Brightwood A, Beckham JC, Kollins SH, 2014. Ecological Momentary Assessment of Antecedents and Consequences of Smoking in Adults with Attention-Deficit/Hyperactivity Disorder. Subst. Use. Misuse 49, 1446–1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BSG, Pelham WE, 2003. Childhood predictors of adolescent substance use in a longitudinal study of children with ADHD. J. Abnorm. Psychol 112, 497–507. [DOI] [PubMed] [Google Scholar]
- Molina BSG, Pelham WE, 2014. Attention-deficit/hyperactivity disorder and risk of substance use disorder: developmental considerations, potential pathways, and opportunities for research. Annu Rev. Clin. Psychol 10, 607–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BSG, Pelham WE, Cheong J, Marshal MP, Gnagy EM, Curran PJ, 2012. Childhood attention-deficit/hyperactivity disorder (ADHD) and growth in adolescent alcohol use: the roles of functional impairments, ADHD symptom persistence, and parental knowledge. J. Abnorm. Psychol 121, 922–935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BSG, Pelham WE, Gnagy EM, Thompson AL, Marshal MP, 2007. Attention-deficit/hyperactivity disorder risk for heavy drinking and alcohol use disorder is age specific. Alcohol. Clin. Exp. Res 31, 643–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BSG, Sibley MH, Pedersen SL, Pelham WE, 2017. The Pittsburgh ADHD Longitudinal Study (PALS), Oxford University Press; New York. [Google Scholar]
- National Household Study on Drug Abuse. Substance Abuse and Mental Health Services Administration; 1992.
- Pedersen SL, Walther CA, Harty SC, Gnagy EM, Pelham WE, Molina BS, 2016. The indirect effects of childhood attention deficit hyperactivity disorder on alcohol problems in adulthood through unique facets of impulsivity. Addict. 111, 1582–1589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rooney M, Chronis-Tuscano A, Yoon Y, 2012. Substance Use in College Students With ADHD. J. Atten. Disord 16, 221–234. [DOI] [PubMed] [Google Scholar]
- Rooney M, Chronis-Tuscano AM, Huggins S, 2015. Disinhibition mediates the relationship between ADHD and problematic alcohol use in college students. J. Atten. Disord 19, 313–327. [DOI] [PubMed] [Google Scholar]
- Rosen PJ, Factor PI, 2015. Emotional Impulsivity and Emotional and Behavioral Difficulties Among Children With ADHD: An Ecological Momentary Assessment Study. J. Atten. Disord 19, 779–793. [DOI] [PubMed] [Google Scholar]
- Sobanski E, Banaschewski T, Asherson P, Buitelaar J, Chen W, Franke B, Holtmann M, Krumm B, Sergeant J, Sonuga-Barke E, Stringaris A, 2010. Emotional lability in children and adolescents with attention deficit/hyperactivity disorder (ADHD): clinical correlates and familial prevalence. J. Child. Psychol. Psychiatry 51, 915–923. [DOI] [PubMed] [Google Scholar]
- Solhan MB, Trull TJ, Jahng S, Wood PK, 2009. Clinical assessment of affective instability: comparing EMA indices, questionnaire reports, and retrospective recall. Psychol. Assess 21, 425–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Team, R.C., 2018. R: A language and environment for statistical computing, R Foundation for Statistical Computing; Vienna, Austria. [Google Scholar]
- Tomko RL, Lane SP, Pronove LM, Treloar HR, Brown WC, Solhan MB, Wood PK, Trull TJ, 2015. Undifferentiated negative affect and impulsivity in borderline personality and depressive disorders: A momentary perspective. J. Abnorm. Psychol 124, 740–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomko RL, Solhan MB, Carpenter RW, Brown WC, Jahng S, Wood PK, Trull TJ, 2014. Measuring impulsivity in daily life: the momentary impulsivity scale. Psychol. Assess 26, 339–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderVeen JD, Plawecki MH, Millward JB, Hays J, Kareken DA, O'Connor S, Cyders MA, 2016. Negative urgency, mood induction, and alcohol seeking behaviors. Drug. Alcohol. Depend 165, 151–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venables WN, Ripley BD, 2002. Modern Applied Statistics with S, fourth ed. Springer-Verlag, New York, pp. 498. [Google Scholar]
- Weafer J, Milich R, Fillmore MT, 2011. Behavioral components of impulsivity predict alcohol consumption in adults with ADHD and healthy controls. Drug. Alcohol. Depend 113, 139–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR, 2001. The Five Factor Model and impulsivity: using a structural model of personality to understand impulsivity. Pers. Individ. Dif 30, 669–689. [Google Scholar]


