Abstract
Background
Sufficient analgesia is an obligation, but oligoanalgesia (NRS> 3) is frequently observed prehospitally. Potent analgesics may cause severe adverse events. Thus, analgesia in the helicopter emergency medical service (HEMS) setting is challenging. Adequacy, efficacy and administration safety of potent analgesics pertaining to injured patients in HEMS were analysed.
Methods
Observational study evaluating data from 14 year-round physician-staffed helicopter bases in Austria in a 12-year timeframe.
Results
Overall, 47,985 (34.3%) patients received analgesics, 26,059 of whom were adult patients, injured and not mechanically ventilated on site. Main drugs administered were opioids (n=20,051; 76.9%), esketamine (n=9082; 34.9%), metamizole (n=798; 3.1%) and NSAIDs (n=483; 1.9%). Monotherapy with opioids or esketamine was the most common regimen (n=21,743; 83.4%), while opioids together with esketamine (n= 3591; 13.8%) or metamizole (n=369; 1.4%) were the most common combinations. Females received opioids less frequently than did males (n=6038; 74.5% vs. n=14,013; 78.1%; p< 0.001). Pain relief was often sufficient (> 95%), but females more often had moderate to severe pain on arrival in hospital (n=34; 5.0% vs. n=59; 3.2%; p=0.043). Administration of potent analgesics was safe, as indicated by MEES, SpO2 and respiratory rates. On 10% of all missions, clinical patient assessment was deemed sufficient by HEMS physicians and monitoring was spared.
Conclusions
Opioids and esketamine alone or in combination were the analgesics of choice in physician-staffed HEMS in Austria. Analgesia was often sufficient, but females more than males suffered from oligoanalgesia on hospital arrival. Administration safety was high, justifying liberal use of potent analgesics in physician-staffed HEMS.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13049-021-00839-9.
Introduction
Providing sufficient analgesia in the challenging prehospital emergency setting is an ethical obligation and of clinical relevance [1]. Potent analgesics, able to relieve intense pain, can result in severe adverse events (e.g. respiratory or circulatory depression, hallucination or agitation). Thus, their liberal use is limited [2, 3]. In the special stetting of helicopter emergency medical services (HEMS) severely injured patients needing analgesia are frequent. Physicians must be aware that the handling of severe side-effects during HEMS operations is difficult in a hostile environment with limited in-cabin space. Adequacy, efficacy and safety of prehospital analgesia administered by HEMS have been addressed before, often with reports on high rates of oligoanalgesia [4–8]. The aim of this study was to assess analgesia in patients treated by HEMS physicians over a 12-year timeframe in Austria. Dosages and analgesic regimens were examined, as were adequacy and safety of administration.
Materials and methods
This retrospective study was approved by the Ethics Committee of the Medical University of Innsbruck (AN2015–0068 347/4.13393/5.20) and was registered with Clinical Trials (NCT03760302). In Austria the ÖAMTC (Austrian Automobile, Motorcycle and Touring Club) runs 17 year-round helicopter bases. The HEMS team consists of a pilot, a physician (advanced life support (ALS)-certified with several years of clinical practice, most commonly in anaesthesiology and intensive care medicine) and an emergency medical technician with basic life support and mountain rescue skills. After completing a rescue mission, emergency physicians transfer data from their handwritten medical report to a standardized digital database intended for medical documentation and billing purposes. Analysis of this database was performed for a 12-year timeframe from 01/01/2006 to 31/12/2017. Two helicopter bases were excluded for reasons of data protection restrictions, and one helicopter program was launched in May 2020. Consequently, this analysis drew on nationwide data from 14 year-round helicopter bases. The flow chart for the study is outlined in Fig. A1.
Data obtained included date, time, helicopter base, type of accident or emergency, sex, age in groups, injury pattern, severity and region of injuries, medication and interventions performed by the emergency team. With regard to emergency classifications, mountain accidents were analysed separately.
The largest group of other accidents included work, road traffic and home and leisure accidents. Pain was scaled as no pain, mild pain (Numeric Rating Scale (NRS) ≤3), and moderate to severe pain (NRS > 3). With regard to analgesics, opioids mainly included fentanyl, piritramide, morphine and also seldomly tramadol, nalbuphine, sufentanil and remifentanil. NSAIDs administered included aspirin, mefenamic acid, diclofenac and ketoprofen.
Age documentation was performed in 5- to 10-year scales. With regard to expected weight and required dosages, patients at least 15 years of age were enrolled in the study. When medication dosage was missing or not given accurately, only the type of medication was analysed. Severity and progress of the patient’s condition were evaluated using NACA (National Advisory Committee for Aeronautics) scoring and the voluntarily documented MEES (Mainz Emergency Evaluation Score including four categories for Glasgow Coma Scale, heart and breathing rate, cardiac rhythm, pain, blood pressure and peripheral oxygen saturation (SpO2)) [9, 10].
Data are presented as median and interquartile range or count and percentage, as appropriate. The Chi-square test was performed to detect group differences in frequencies, and the Mann-Whitney U test for group differences in continuous data. Data were stored with Excel 2019 (Microsoft, Seattle, WA, USA) and processed with RStudio version 1.2.5001 (RStudio, Inc., Boston, MA, USA).
Results
Demographics and general emergency characteristics
A total of 176,056 HEMS operations were analysed. Primary missions made up 139,831. Of these, analgesics were administered in 47,985 (34.3%) cases. Exclusion of patients under 15 years of age, uninjured or mechanically ventilated on site resulted in 26,059 patients for further analysis (Fig. A1). Sex was analysed separately, resulting in 17,950 males and 8103 females. General emergency characteristics are depicted in Table 1.
Table 1.
General emergency characteristics
| Adults (≥ 15 yrs)n= 26,059*n (%) | ||
|---|---|---|
| Male n= 17,950 (68.9) | Female n= 8103 (31.1) | |
| Age (years) | ||
| 15–19 | 1679 (9.4) | 793 (9.8) |
| 20–39 | 5916 (33.0) | 1940 (23.9) |
| 40–59 | 6788 (37.8) | 2912 (35.9) |
| 60–79 | 3180 (17.7) | 1799 (22.2) |
| > 80 | 387 (2.2) | 659 (8.1) |
| Emergency classification | ||
| Accident (mountain) | 5063 (28.2) | 3265 (40.3) |
| Accident (other) | 12,444 (69.3) | 4531 (55.9) |
| Other | 443 (2.5) | 306 (3.8) |
| Analgesics used | ||
| Opioids | 14,013 (78.1) | 6038 (74.5) |
| Esketamine | 6144 (34.2) | 2938 (36.3) |
| Metamizole | 516 (2.9) | 282 (3.5) |
| NSAIDs+ | 323 (1.8) | 160 (2.0) |
| NACA Score as median (IQR) | 4 (3–4) | 3 (3–4) |
| Injury localizations per patient | ||
| 1 | 9776 (54.5) | 5089 (62.8) |
| 2–3 | 7072 (39.4) | 2645 (32.6) |
| > 3 | 1065 (5.9) | 356 (4.4) |
| Injury localizations | ||
| Head | 4901 (27.3) | 1858 (23.0) |
| Spine | 4228 (23.6) | 1729 (21.3) |
| Chest | 4423 (24.6) | 1403 (17.3) |
| Abdomen | 1537 (8.6) | 546 (6.7) |
| Pelvis | 1023 (5.7) | 411 (5.1) |
| Upper limb | 7022 (39.1) | 2479 (30.6) |
| Lower limb | 8011 (44.6) | 4367 (53.9) |
| Injury types | ||
| Fracture | 12,791 (71.3) | 6054 (74.7) |
| Contusion | 5930 (33.0) | 2424 (29.9) |
| Soft tissue | 6026 (33.6) | 1933 (23.9) |
| Traumatic brain injury | 2871 (16.0) | 1065 (13.1) |
| Internal organs | 1125 (6.3) | 379 (4.7) |
| Neurovascular | 1055 (5.9) | 251 (3.1) |
* sex unknown in n=6 cases; + Non-steroidal anti-inflammatory drugs
The adult age group most affected by frequency was the 40- to 59-year-olds. General injury localizations as well as number of affected body regions per patient are depicted in Table 1. With respect to injury severity, the median National Advisory Committee for Aeronautics (NACA) score was 4 (3–4) for males and 3 (3–4) for females, with a total of 12,239 (47.0%) patients suffering potentially life-threatening injuries as classified by a NACA score ≥ 4.
Analgesics commonly used
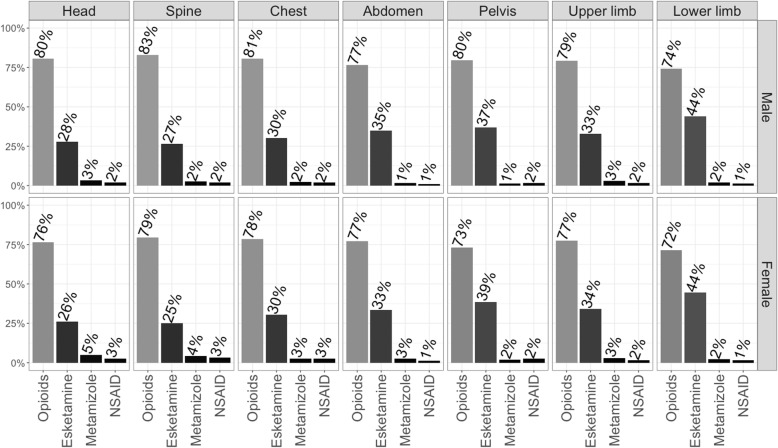
Analgesics commonly used are presented as frequencies and median dosages in Table 2. Figure 1 presents analgesics administered dependent on injury localization, and Table 3 shows analgesic regimens in terms of number of analgesic substance classes administered and commonly used combinations.
Table 2.
Commonly used analgesics in HEMS operations presented as frequencies and median dosage (IQR)
| Adults (≥ 15 yrs)n= 26,059* | ||
|---|---|---|
| Male n= 17,950 | Female n= 8103 | |
| Fentanyl | ||
| n (%) total | 8439 (47.0) | 3289 (40.6) |
| n (%) with dosage | 4267 (50.6) | 1706 (51.9) |
| Dosage (mg) | 0.20 (0.15–0.25) | 0.20 (0.10–0.25) |
| Piritramide | ||
| n (%) total | 5244 (29.2) | 2559 (31.6) |
| n (%) with dosage | 2549 (48.6) | 1420 (55.5) |
| Dosage (mg) | 7.50 (7.50–15.00) | 7.50 (7.50–10.00) |
| Morphine | ||
| n (%) total | 384 (2.1) | 195 (2.4) |
| n (%) with dosage | 112 (29.2) | 63 (32.3) |
| Dosage (mg) | 10.00 (5.00–10.00) | 5.00 (5.00–10.00) |
| Esketamine | ||
| n (%) total | 6144 (34.2) | 2938 (36.3) |
| n (%) with dosage | 2076 (33.8) | 1123 (38.2) |
| Dosage (mg) | 25.0 (20.0–50.0) | 25.0 (15.0–40.0) |
* sex unknown in n= 6 cases
Fig. 1.
Analgesics commonly used in injured patients in dependency on injury localization. NSAID: Non-steroidal anti-inflammatory drug
Table 3.
Analgesic therapy regimen for injured patients in HEMS operations
| Adults (≥ 15 yrs)n= 26,059* | ||
|---|---|---|
| Male n= 17,950 | Female n= 8103 | |
| Analgesic substance classes | ||
| Monotherapy | 14,938 (83.2) | 6805 (84.0) |
| Dual therapy | 2972 (16.6) | 1278 (15.8) |
| Triple therapy | 40 (0.2) | 19 (0.2) |
| Common combinations | ||
| Opioids only | 11,056 (61.6) | 4781 (59.0) |
| Esketamine only | 3539 (19.7) | 1818 (22.4) |
| Opioids + esketamine | 2520 (14.0) | 1071 (13.2) |
| Opioids + metamizole | 260 (1.4) | 109 (1.3) |
| Metamizole only | 199 (1.1) | 133 (1.6) |
| NSAIDs+ only | 141 (0.8) | 72 (0.9) |
| Opioids + NSAIDs+ | 136 (0.8) | 57 (0.7) |
* sex unknown in n= 6 cases; + Non-steroidal anti-inflammatory drugs
In males, opioids were administered in 78.1%, esketamine in 34.2%; in females, opioids were administered in 74.5% (p< 0.001), esketamine in 36.3% (p= 0.002) of all cases (Table 1). Sorted by frequency of administration, opioids included mainly fentanyl, piritramide and morphine (Table 2). Opioids were given in a high percentage of patients regardless of injury localization (Fig. 1). Additional or alternative administration of esketamine was performed less often for head or spine injuries and was more pronounced in pelvic and lower limb injuries. Regarding analgesic combination therapies, 83.2% of male and 84.0% of female patients received one, 16.6 and 15.8% two and merely 0.2% of female and male patients were given three different substance classes (Table 3). While approximately 81% of patients (regardless of sex) received opioids or esketamine only, the most common combinations were opioids with esketamine (males: 14.0%; females: 13.2%), opioids with metamizole (1.4%; 1.3%) and opioids with NSAIDs (0.8%; 0.7%). Median doses were 0.2 mg of fentanyl, 7.5 mg of piritramide, 5 mg or 10 mg of morphine and 25 mg or 30 mg of esketamine.
Adequacy and administration safety of potent analgesics
The following analysis was performed on patients with complete datasets, including documentation on site and on arrival in hospital, leaving 2330 patients for analysis of respiratory items of MEES documentation and 2517 patients for analysis of pain scores.
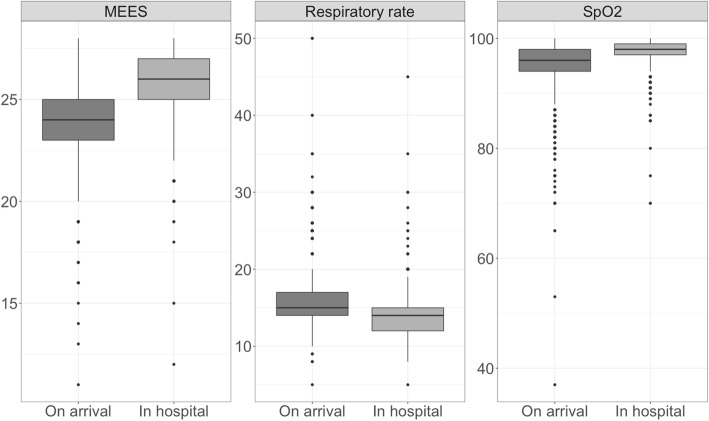
Figure 2 illustrates differences in MEES, respiratory rates and SpO2 in injured adults between the time when the emergency physician arrives on site and the time when the patient is handed over to the hospital. MEES increased from 24 (23–25) to 26 (25–27) (p< 0.001). Respiratory rates decreased from 15 (14–17) to 14 (12–15) (p< 0.001). Oxygen saturation improved from 96 (94–98) to 98 (97–99) (p< 0.001). Additional mechanical ventilation requirements during transport were present in only 45 (0.2%) patients.
Fig. 2.
MEES, respiratory rate and SpO2 of injured patients receiving medical analgesia on arrival of emergency physician compared to at handover in hospital. Only patients with complete data were included (n= 2330). Due to missing differences, a gender independent presentation was chosen
At the same time, documented pain decreased with respect to the two observed timepoints (Fig. 3). Regarding gender differences, no significant difference was detected in patients with moderate to severe pain on arrival of the emergency physician (male: 87.1% vs. female: 89.4%; p= 0.137), but after treatment and on arrival at hospital females more often suffered from moderate to severe pain (male: 3.2% vs. female: 5%; p= 0.043). The fraction suffering no or mild pain increased significantly.
Fig. 3.
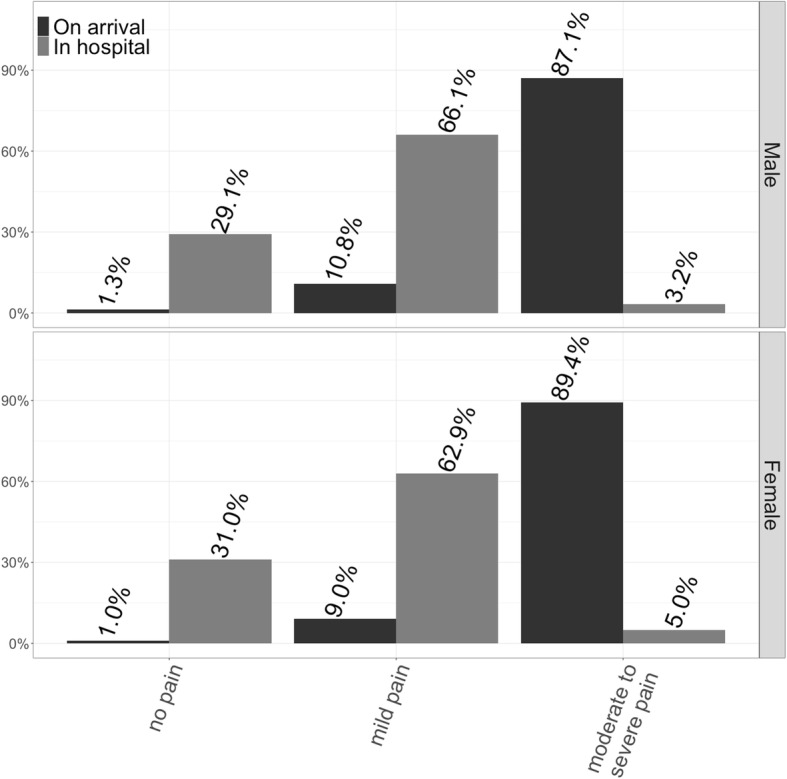
Pain level of injured patients receiving medical analgesia on arrival of emergency physician compared to at handover in hospital. Only patients with complete data regarding level of pain were considered (n= 1840 male adults; n= 677 female adults)
We identified 2723 missions (10%) conducted without technical monitoring such as pulse oximetry, ECG or blood pressure. The majority of patients were male (n=1724; 63.3%), younger (15-39a: n=1160; 42.6%), orientated (n=1877; 91.9%) and with moderate to severe pain (n=2393; 87.9%) from fractures (n=2199; 80.8%) to the upper or lower limb (n=2466; 90.6%). Regarding emergency classifications, 2023 (74.3%) cases were mountain accidents and 1877 (68.9%) occurred between December and May. Opioids were administered to 2071 (76.1%) patients and esketamine to 913 (33.5%). Median dosages were 0.2 mg fentanyl, 7.5 mg piritramide and 25 mg esketamine.
Discussion
This study focuses on emergency patients > 15 years of age, nearly half of whom received analgesic therapy in a potentially life-threatening condition (NACA > 3). Injuries were predominantly fractures, with the upper or lower extremities most often affected. Main substances administered were opioids (fentanyl > piritramide > morphine) followed by esketamine, metamizole and NSAIDs. With analgesic monotherapy being the most common regimen, males proportionally received opioids more often than did females. Following opioids or esketamine only, opioids with esketamine or opioids with metamizole were the most common combination therapies. As shown by the development of MEES, respiratory rates, oxygen saturation and the non-necessity of mechanical ventilation during transport, application of potent analgesics was very safe in the described setting. A total of 10% of the analysed HEMS operations were performed without technical monitoring which could be due to various reasons like short transportation time, cold weather and winter clothes, technical rescue operations or even patient’s medical condition. Regarding pain relief, a higher fraction of females still had moderate to severe pain on hospital arrival. In total, pain levels decreased significantly, and administration seemed safe, thus justifying the liberal use of potent analgesics in HEMS.
This study presents a large retrospective analysis of a nationwide registry covering 14 physician-staffed helicopter bases in Austria over a 12-year timeframe. To date, only few studies of this size have been published on prehospital analgesia in HEMS.
Demographics and general emergency characteristics
Current publications on analgesia in HEMS originate in the combat setting, in particular with the U.S. armed forces in Afghanistan [11–14]. Affected patients were primarily young male soldiers who suffered acute trauma due to blast or penetrating injuries. Civilian HEMS operations report data from Europe [3–6, 15, 16] and also Australia [8]. The data analysed show that 34.3% of patients received analgesic therapy. This compares with the figures reported for HEMS operations in Victoria, Australia (89%) [8], Germany (79%) [4], Switzerland (57–84%) [15, 17]. Regarding ground-based EMS, two studies from Europe reported a percentage of 48% of all patients [2, 3], whereas merely 3% of all trauma patients in a South African study received any kind of analgesic medication [18]. As shown in other studies conducted in Austria, a high density of HEMS in combination with a mountainous landscape often prompts airborne rescue of merely mildly or even non-injured patients [19, 20]. This can also be seen from our data, where a total of 44.6% of all HEMS operations were classified as NACA ≤ 3. This may explain the rather small percentage of patients receiving analgesia in this study.
Analgesics commonly used
Analgesia administered during EMS may vary depending on type (HEMS/ EMS) and staffing (e.g. paramedic vs. physician) including the training level of the providers (anaesthesiologist vs. general practitioner, specialist vs. trainee, BLS vs. ALS provider, clinical experience). In systems with a large volume of emergency operations staffed at most with BLS/ILS providers, administration of i.v. analgesics is limited [18]. Nitrous oxide can be an option, but is mainly used in some English-speaking countries [18]. Another inhalational analgesic is low-dose methoxyflurane [21, 22]. Despite its undeniable advantages, as in quick, easy and safe administration also by non-physicians, its distribution seems very limited up to date (e.g. Australia, Italy). Moreover, as also confirmed in this study, opioids and ketamine/ esketamine predominate in the prehospital management of moderate to severe pain [2–5, 11–14]. Whether racemic ketamine or its S-enantiomer esketamine is preferred depends mainly on country-specific regulations. When comparing the two, consideration of different dosing requirements is important. As shown in a study on analgesia in HEMS in Switzerland, ketamine was preferably used by anaesthetists [17]. The high proportion of Austrian emergency physicians also being anaesthetists also explains the rather high rate of esketamine use in this study. In detail, the presented data were able to show high use of opioids over all injury localizations and the predominant use of esketamine in injuries affecting the upper and lower limbs including the pelvis. Fortunately, the administration of these potent analgesics is not limited to physicians, at least in some countries. Albeit median doses are somewhat higher in this physician-staffed service, paramedics can effectively and safely administer opioids and ketamine [8, 23–27]. Furthermore, dose differences are not only present inter- but also intra-professionally as demonstrated by a study from a physician-staffed EMS in Germany, which showed differences in pain treatment between surgeons and anaesthesiologists, particularly regarding opioids [28]. Ketamine has been described as being safe and effective alone – even as effective as an alternative opioid – and also as being able to reduce opioid requirements when used in combination with opioids [26, 29, 30]. After opioids or esketamine administered alone, the by far most commonly administered combination therapy in the presented study was an opioid with esketamine, followed by a combination of an opioid with metamizole.
Adequacy and application safety of potent analgesics for injured patients during HEMS operations
Moderate to severe pain is a frequent finding in the prehospital care of emergency patients [8, 17, 31]. So is the rate of inadequate pain treatment, also described as oligoanalgesia (18–58%) [4–6, 24].
While the absence of analgesic administration as well as a higher NACA Score and NRS on site have unsurprisingly been described as risk factors for insufficient pain management, the same is unexpectedly also true of treatment by a female physician [6]. Although perceived oligoanalgesia rates were the same, emergency physicians improved quality of analgesia by providing a substantially higher NRS reduction than did paramedics in a study from Switzerland [2]. As higher doses of fentanyl administered in a paramedic setting have been shown to relieve pain better [23], the observed benefits might be due to deliberately increased dosages in physician-staffed settings, as also seen in this study. Ketamine has been shown to be safe, when administered alone or in combination with opioids, with no loss of consciousness, oxygen desaturation or clinically significant emergence reactions occurring [7, 27, 30]. Ketamine alone seems to have fewer side-effects than morphine alone, but the combination of both has more side-effects than morphine alone [32]. Albeit a commonly used combination therapy, the administration of ketamine with morphine has also not been recommended because of uncertainties regarding safety [32, 33]. Adverse events due to analgesic medications are not easy to discriminate in an emergency and sometimes austere situation. With regard to potent analgesics as in opioids or esketamine, the most feared and clinically important side-effect is certainly a possible respiratory depression. Comparison of the need for additional mechanical ventilation during transport as well as clinical scores (MEES), surrogates for sufficient respiration (SpO2, respiratory rate) and levels of pain on arrival of the emergency physician and at the time of handover in hospital led us to conclude that the analgesics administered in this study were safe and adequate. The percentage of patients suffering from moderate to severe pain unmistakably decreased from over 87% to under 5%, further justifying liberal use of potent analgesics. Interestingly, while no gender differences were recorded with respect to initially moderate to severe pain, females more often still suffered from moderate to severe pain on arrival in hospital. Documented injury severity was lower in females and, while median analgesic dosages were comparable, decreased opioid but increased esketamine administration was recorded in female adults. Reasons for this difference cannot be derived from the presented data, but this finding stands in contrast to the existing literature, where largely no gender difference or even a female predominance in pain relief is described [2, 4–6, 18].
Not previously described is the fact that 10% of the described HEMS missions were conducted without any technical monitoring despite the overwhelming use of opioids and esketamine. These special cases were particularly young, orientated men involved in mountain accidents mainly in winter and suffering from severe pain from fractures to the upper or lower limbs. Obviously, this practice is not uncommon and emergency physicians were not discouraged from administering these potent analgesics in order to relieve severe pain despite the non-availability or cold-related failure of adequate technical monitoring equipment.
Limitations
Although handwritten report forms were primarily documented prospectively and transferred to the digital database in a timely manner and by the emergency physician himself, poor documentation quality is not uncommon in emergency prehospital settings [23, 34]. Errors occurring during data transfer might have additionally contributed to this problem. Accurate documentation has been proposed as a quality indicator of physician staffed emergency medical service [35] but the mean proportion of completely documented cases often remains low, as seen in a recent Nordic study on HEMS [36]. Comparing to proportions of 25–91% reported by them, merely 9–10% of all cases in this study were completely documented, including MEES, SpO2-values, respiratory rates and pain levels from initial on-site evaluation and hospital admission. A reporting bias can therefore not be excluded. Furthermore, pain levels were documented with an NRS-guided scale and not with exact numerical documentation. Detailed analysis of pain reduction (e.g. NRS reduction) was therefore not possible. Furthermore, data analysis in general was conducted retrospectively.
Conclusion
Opioids and esketamine were frequently administered in physician-staffed HEMS. Analgesia was largely sufficient, with females more often suffering from oligoanalgesia (NRS> 3) on hospital arrival. Administration safety was high, justifying liberal use of potent analgesics in physician-staffed HEMS.
Supplementary Information
Additional file 1 Figure A1. Consort Flowchart.
Acknowledgements
We acknowledge all physicians of the ÖAMTC CFV (ÖAMTC Christophorus Flugrettungsverein) for collecting data while treating patients, Markus Luger, MD for suggesting this analysis, Mary Heaney Margreiter (http://margreiter-translation.com/e_contact.html) for language editing.
Patient and public involvement
Patients and/or the public were not involved in the design, conduct of this study, or the reporting of this research.
Authors’ contributions
CR, SW, VW, PP and MS contributed to conception and design. CR and MS contributed to analysis. CR, and MS contributed to data acquisition. CR and MS drafted the manuscript. All authors critically revised the manuscript, contributed to interpretation, gave final approval and agreed to be accountable for all aspects of the work ensuring integrity and accuracy.
Funding
This work was not supported by any grants.
Availability of data and materials
No data are available. Participant data from the ÖAMTC CFV. All data are deidentified. The data set was delivered containing only serial numbers for each participant. Protocol and statistical analysis plans are available.
Ethics approval and consent to participate
The Ethics Committee of the Medical University of Innsbruck approved the study (AN2015–0068 347/4.13393/5.20) and it was registered with Clinical Trials (NCT03760302).
Consent for publication
Not required.
Competing interests
None of the authors has competing interests regarding this manuscript.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Christopher Rugg, Email: christopher.rugg@tirol-kliniken.at.
Simon Woyke, Email: simon.woyke@tirol-kliniken.at.
Wolfgang Voelckel, Email: wolfgang.voelckel@auva.at.
Peter Paal, Email: peter.paal@icloud.com.
Mathias Ströhle, Email: mathias.stroehle@tirol-kliniken.at.
References
- 1.McManus JG, Sallee DR. Pain Management in the Prehospital Environment. Pain Manag Prehospital Environ. 2005;23:415–431. doi: 10.1016/j.emc.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 2.Kiavialaitis G, Müller S, Braun J, Rössler J, Spahn D, Stein P, et al. Clinical practice of pre-hospital analgesia: an observational study of 20,978 missions in Switzerland. Am J Emerg Med. 2019;19:0735–6757. doi: 10.1016/j.ajem.2019.10.033. [DOI] [PubMed] [Google Scholar]
- 3.Scholten AC, Berben SAA, Westmaas AH, van Grunsven PM, de Vaal ET, Rood PPM, et al. Pain management in trauma patients in (pre)hospital based emergency care: current practice versus new guideline. Injury Netherlands. 2015;46:798–806. doi: 10.1016/j.injury.2014.10.045. [DOI] [PubMed] [Google Scholar]
- 4.Helm M, Hossfeld B, Braun B, Werner D, Peter L, Kulla M. Oligoanalgesia in patients with an initial Glasgow coma scale score ≥8 in a physician-staffed helicopter emergency medical service: a multicentric secondary data analysis of >100,000 out-of-hospital emergency missions. Anesth Analg. 2020;130:176–186. doi: 10.1213/ANE.0000000000004334. [DOI] [PubMed] [Google Scholar]
- 5.Albrecht E, Taffe P, Yersin B, Schoettker P, Decosterd I, Hugli O. Undertreatment of acute pain (oligoanalgesia) and medical practice variation in prehospital analgesia of adult trauma patients: a 10 yr retrospective study. Br J Anaesth England. 2013;110:96–106. doi: 10.1093/bja/aes355. [DOI] [PubMed] [Google Scholar]
- 6.Oberholzer N, Kaserer A, Albrecht R, Seifert B, Tissi M, Spahn DR, et al. Factors influencing quality of pain Management in a Physician Staffed Helicopter Emergency Medical Service. Anesth Analg. 2017;125:200–209. doi: 10.1213/ANE.0000000000002016. [DOI] [PubMed] [Google Scholar]
- 7.Bredmose PP, Lockey DJ, Grier G, Watts B, Davies G. Pre-hospital use of ketamine for analgesia and procedural sedation. Emerg Med J EMJ England. 2009;26:62–64. doi: 10.1136/emj.2007.052753. [DOI] [PubMed] [Google Scholar]
- 8.Andrew E, de Wit A, Meadley B, Cox S, Bernard S, Smith K. Characteristics of patients transported by a paramedic-staffed helicopter emergency medical Service in Victoria. Australia Prehosp Emerg Care. 2015;19:416–424. doi: 10.3109/10903127.2014.995846. [DOI] [PubMed] [Google Scholar]
- 9.Alessandrini H, Oberladstätter D, Trimmel H, Jahn B, Baubin M. NACA-Scoringsystem: Eine retro- und prospektive Validitätsanalyse anhand ausgewählter Diagnosegruppen. Notf Rettungsmedizin. 2012;15:42–50. doi: 10.1007/s10049-010-1386-8. [DOI] [Google Scholar]
- 10.Reinhardt T, Hennes H-J. Mainz emergency evaluation score (MEES) Notf Rettungsmedizin. 1999;2:380–381. doi: 10.1007/s100490050164. [DOI] [Google Scholar]
- 11.Mora AG, Ganem VJ, Ervin AT, Maddry JK, Bebarta VS. En Route Use of Analgesics in Nonintubated, Critically Ill Patients Transported by U.S. Air Force Critical Care Air Transport Teams. Mil Med. England. 2016;181:145–151. doi: 10.7205/MILMED-D-15-00194. [DOI] [PubMed] [Google Scholar]
- 12.Shackelford SA, Fowler M, Schultz K, Summers A, Galvagno SM, Gross KR, et al. Prehospital pain medication use by U.S. Forces in Afghanistan. Mil Med. England. 2015;180:304–309. doi: 10.7205/MILMED-D-14-00257. [DOI] [PubMed] [Google Scholar]
- 13.Schauer SG, Mora AG, Maddry JK, Bebarta VS. Multicenter, Prospective Study of Prehospital Administration of Analgesia in the U.S. Combat Theater of Afghanistan. Prehospital Emerg Care Off J Natl Assoc EMS Physicians Natl Assoc State EMS Dir. England; 2017;21:744–749. [DOI] [PubMed]
- 14.Petz LN, Tyner S, Barnard E, Ervin A, Mora A, Clifford J, et al. Prehospital and en route analgesic use in the combat setting: a prospectively designed, multicenter, observational study. Mil Med England. 2015;180:14–18. doi: 10.7205/MILMED-D-14-00383. [DOI] [PubMed] [Google Scholar]
- 15.Pasquier M, Geiser V, De Riedmatten M, Carron PN. Helicopter rescue operations involving winching of an emergency physician. Injury. Netherlands. 2012;43:1377–1380. doi: 10.1016/j.injury.2011.06.196. [DOI] [PubMed] [Google Scholar]
- 16.Samdal M, Haugland HH, Fjeldet C, Rehn M, Sandberg M. Static Rope Evacuation by Helicopter Emergency Medical Services in Rescue Operations in Southeast Norway. Wilderness Environ Med. 2018; [DOI] [PubMed]
- 17.Eidenbenz D, Taffé P, Hugli O, Albrecht E, Pasquier M. A two-year retrospective review of the determinants of pre-hospital analgesia administration by alpine helicopter emergency medical physicians to patients with isolated limb injury. Anaesthesia. 2016;71:779–787. doi: 10.1111/anae.13462. [DOI] [PubMed] [Google Scholar]
- 18.Lourens A, Parker R, Hodkinson P. Prehospital acute traumatic pain assessment and management practices in the Western cape, South Africa: a retrospective review. Int J Emerg Med. 2020;13:21. doi: 10.1186/s12245-020-00278-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ströhle M, Haselbacher M, Rugg C, Walpoth A, Konetschny R, Paal P, et al. Mortality in via ferrata emergencies in Austria from 2008 To 2018. Int J Environ Res Public Health. [DOI] [PMC free article] [PubMed]
- 20.Ströhle M, Beretz I, Rugg C, Woyke S, Rauch S, Paal P. Canyoning accidents in Austria from 2005 To 2018. Int J Environ Res Public Health. [DOI] [PMC free article] [PubMed]
- 21.Marinangeli F, Reggiardo G, Sblendido A, Soldi A, Farina A. Prospective, multicentre trial of Methoxyflurane for acute trauma-related pain in helicopter emergency medical systems and hostile environments: METEORA protocol. Adv Ther. 2018;35:2081–2092. doi: 10.1007/s12325-018-0816-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xia AD, Dickerson SL, Watson A, Nokela M, Colman S, Szende A. Evaluation of pain relief treatment and timelines in emergency care in six European countries and Australia. Open Access Emerg Med. 2019;11:229–240. doi: 10.2147/OAEM.S214396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Friesgaard KD, Kirkegaard H, Rasmussen C-H, Giebner M, Christensen EF, Nikolajsen L. Prehospital intravenous fentanyl administered by ambulance personnel: a cluster-randomised comparison of two treatment protocols. Scand J Trauma Resusc Emerg Med. 2019;27:11. doi: 10.1186/s13049-019-0588-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Friesgaard KD, Nikolajsen L, Giebner M, Rasmussen C-H, Riddervold IS, Kirkegaard H, et al. Efficacy and safety of intravenous fentanyl administered by ambulance personnel. Acta Anaesthesiol Scand. England. 2016;60:537–543. doi: 10.1111/aas.12662. [DOI] [PubMed] [Google Scholar]
- 25.McQueen C, Crombie N, Cormack S, Wheaton S. Prehospital use of ketamine for analgesia and procedural sedation by critical care paramedics in the UK: a note of caution? Emerg med J EMJ. England. 2014;31:1029. doi: 10.1136/emermed-2014-204022. [DOI] [PubMed] [Google Scholar]
- 26.Jennings PA, Cameron P, Bernard S. Ketamine as an analgesic in the pre-hospital setting: a systematic review. Acta Anaesthesiol Scand England. 2011;55:638–643. doi: 10.1111/j.1399-6576.2011.02446.x. [DOI] [PubMed] [Google Scholar]
- 27.Losvik OK, Murad MK, Skjerve E, Husum H. Ketamine for prehospital trauma analgesia in a low-resource rural trauma system: a retrospective comparative study of ketamine and opioid analgesia in a ten-year cohort in Iraq. Scand J Trauma Resusc Emerg Med. 2015;23:94. doi: 10.1186/s13049-015-0176-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schaller SJ, Kappler FP, Hofberger C, Sattler J, Wagner R, Schneider G, et al. Differences in pain treatment between surgeons and anaesthesiologists in a physician staffed prehospital emergency medical service: a retrospective cohort analysis. BMC Anesthesiol. 2019;19:18. doi: 10.1186/s12871-019-0683-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bansal A, Miller M, Ferguson I, Burns B. Ketamine as a Prehospital analgesic: a systematic review. Prehospital Disaster Med United States. 2020;35:314–321. doi: 10.1017/S1049023X20000448. [DOI] [PubMed] [Google Scholar]
- 30.Johansson P, Kongstad P, Johansson A. The effect of combined treatment with morphine sulphate and low-dose ketamine in a prehospital setting. Scand J Trauma Resusc Emerg Med. 2009;17:61. doi: 10.1186/1757-7241-17-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Friesgaard KD, Riddervold IS, Kirkegaard H, Christensen EF, Nikolajsen L. Acute pain in the prehospital setting: a register-based study of 41.241 patients. Scand J Trauma Resusc Emerg Med. 2018;26:53. [DOI] [PMC free article] [PubMed]
- 32.Yousefifard M, Askarian-Amiri S, Rafiei Alavi SN, Sadeghi M, Saberian P, Baratloo A, et al. The efficacy of ketamine Administration in Prehospital Pain Management of trauma patients; a systematic review and meta-analysis. Arch Acad Emerg Med. 2020;8:e1. [PMC free article] [PubMed] [Google Scholar]
- 33.Sobieraj DM, Baker WL, Martinez BK, Miao B, Hernandez AV, Coleman CI, et al. Comparative Effectiveness of Analgesics To Reduce Acute Pain in the Prehospital Setting. Rockville (MD): Agency for Healthcare Research and Quality (US); 2019. [PubMed]
- 34.Browne LR, Studnek JR, Shah MI, Brousseau DC, Guse CE, Lerner EB. Prehospital opioid Administration in the Emergency Care of injured children. Prehosp Emerg Care. 2016;20:59–65. doi: 10.3109/10903127.2015.1056897. [DOI] [PubMed] [Google Scholar]
- 35.Haugland H, Rehn M, Klepstad P, Krüger A. Developing quality indicators for physician-staffed emergency medical services: a consensus process. Scand J Trauma Resusc Emerg Med [Internet]. 2017 [cited 2020 Dec 8];25. Available from: http://sjtrem.biomedcentral.com/articles/10.1186/s13049-017-0362-4 [DOI] [PMC free article] [PubMed]
- 36.Haugland H, Olkinuora A, Rognås L, Ohlen D, Krüger A. Testing quality indicators and proposing benchmarks for physician-staffed emergency medical services: a prospective Nordic multicentre study. BMJ Open. 2019;9:e030626. doi: 10.1136/bmjopen-2019-030626. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1 Figure A1. Consort Flowchart.
Data Availability Statement
No data are available. Participant data from the ÖAMTC CFV. All data are deidentified. The data set was delivered containing only serial numbers for each participant. Protocol and statistical analysis plans are available.