Abstract
Background and Aims:
Subcostal transversus abdominis plane (TAP) block is usually done under ultrasound guidance in laparoscopic cholecystectomy. Laparoscopic-guided subcostal TAP block is an alternate technique where ultrasound is not available. Our primary objective was to compare the success rate of ultrasound and laparoscopic approaches to the subcostal TAP block. The secondary objectives were to assess the duration of postoperative analgesia and morphine consumption postoperatively for 24 h.
Methods:
Eighty patients undergoing laparoscopic cholecystectomy were randomly divided into two groups with patients receiving ultrasound-guided (group U) or laparoscopy-guided (group L) subcostal TAP block at the end of surgery. The success rate was assessed by a sensory blockade of T7 and T8 dermatomes 30 min after extubation. The duration of analgesia was taken as time from block administration to the visual analogue scale of ≥3. Morphine was administered in patient-controlled analgesia (PCA) pump with a bolus of 1 mg and a lock-out interval of 10 min. The total morphine consumption was recorded. The statistical analysis was performed with student t-test and Chi-square test.
Results:
The success rate of group U (100%) was higher than group L (88%) but it was not statistically significant (P = 0.054). The duration of postoperative analgesia was significantly prolonged in group U (867.24 ± 135.83 min) than group L (751.31 ± 311.22 min) (P = 0.033). Morphine consumption was also less in group U (4.72 ± 0.94 mg) than group L (5.57 ± 2.53 mg) (P = 0.049). There was no significant difference in the VAS scores after 4 h postoperatively.
Conclusion:
Laparoscopy-guided subcostal TAP block is a suitable alternative to ultrasound-guided block and can be utilised in places where an ultrasound machine is not available.
Key words: Laparoscopic cholecystectomy, patient-controlled analgesia, ropivacaine, transversus abdominis plane block, ultrasound
INTRODUCTION
Although laparoscopic cholecystectomy (LC) is described as a surgery that is minimally invasive, it is still associated with moderate to severe pain especially in the first 24 h of surgery.[1] Nerve blocks have been advocated as part of a multimodal analgesia regime to reduce the consumption of analgesics and also to provide better pain relief facilitating enhanced recovery after surgery.[2] The use of ultrasound for the transversus abdominis plane (TAP) block has allowed direct visualisation of the spread of local anaesthetics (LA) and increasing the success rate. But ultrasound may not be available in all hospitals performing laparoscopy, especially in developing countries. Also, not all anaesthesiologists are trained in the use of ultrasound. Laparoscopy can be utilised as a guide to performing subcostal TAP block where ultrasound or technical expertise to operate it is not available.[3]
There are only very few studies available regarding the use of laparoscopy-guided subcostal TAP block and no study is available regarding its comparison with the ultrasound-guided subcostal TAP block to the best of our knowledge. The aim of this prospective, randomised and observer-blinded study was to compare the success rate of laparoscopy-guided (LG) subcostal TAP block with ultrasound-guided (UG) subcostal TAP block in LC surgeries performed unilaterally on the right side. The secondary objectives were to compare the duration of postoperative analgesia, visual analogue scale (VAS) scores and consumption of morphine in patient-controlled analgesia (PCA) pump for the first 24 h.
METHODS
This prospective, randomised study was done on 80 patients undergoing LC from February 1, 2019, to September 30, 2019. This study was started after obtaining institutional ethical committee approval and was registered prospectively with clinical trials registry India (CTRI/2019/01/017255). Patients in the age group of 18–70 years, weighing from 60 to 100 kg and American Society of Anaesthesiologists physical status I and II scheduled for LC were included in the study. Patients with known cardiac, liver, or renal diseases, pregnant patients, and patients with coagulation abnormalities were excluded from the study. The informed written consent was obtained from all patients and we followed the ethical guidelines of the declaration of Helsinki.
The patients were randomly divided into two groups of 40 each by computer-generated random numbers and kept in sequentially numbered, opaque and closed envelopes: group U received UG subcostal TAP block and group L received LG subcostal TAP block. The randomisation was done at the start of the study, and envelopes were opened in sequential order. The pain was assessed by a VAS score of 1–10 at rest, and the patients were explained preoperatively about the same.
The general anaesthesia was standardised in both groups. The patients were premedicated with alprazolam 0.5 mg orally on the night before surgery and 2 h before surgery. Fentanyl 2 μg/kg was used as an intraoperative analgesic. The patients were induced with propofol 2 mg/kg and cisatracurium 1.5 mg/kg was used as a muscle relaxant. The endotracheal intubation was performed, and anaesthesia was maintained with N2O:O2 in a ratio of 2:1 with sevoflurane titrated from 1% to 2%. An orogastric tube was inserted in all cases to avoid gastric distension and removed postoperatively. At the end of the surgery, the anaesthesiologist involved in patient care opened the envelope and either administered the subcostal TAP block on the right side in group U or advised the surgeon to perform it in group L. They took no further part in the study. The patients were shifted to post anaesthetic care unit (PACU) and observed there for 24 h. The anaesthesiologist in PACU, who was blinded to the group involved, monitored the patient and documented the study parameters. The patient was also blinded to the group allotted. All the blocks in group U were performed by a single experienced anaesthesiologist. The LG subcostal TAP block was performed by a single experienced surgeon.
An ultrasonogram (USG) machine (Logiq V2, GE Medical Systems, Jiangsu, China), with a 5–13MHz linear probe was used for the group U patients. The probe was placed immediately below the costal margin near the midline. 100 mm, 20G Stimuplex (B Braun) needle was targeted in the fascial plane between the posterior rectus sheath and the transversus abdominis muscle and the correct placement of the needle was confirmed by hydrodissection. 20 mL of 0.2% ropivacaine with 8 mg dexamethasone was administered in group U.[4] The correct plane of infiltration in the LG subcostal TAP block was identified by visualising the lifting of fibres of transversus abdominis muscle (Doyle's bulge) seen intra-peritoneally by hydrodissection and has been depicted in Figure 1.[3] Group L patients also received 20 mL of 0.2% ropivacaine and 8 mg dexamethasone. All the patients received paracetamol 1 g at the end of surgery and every 6 h intravenously for 24 h. The patients did not receive any other additional analgesics. Ondansetron 4 mg was given intravenously during induction and repeated after 12 h. The patients were extubated after completing blocks and shifted to PACU for observation.
Figure 1.
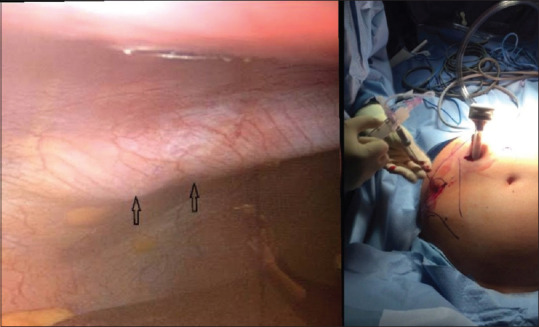
Doyle's bulge of laparoscopic-guided (LG) subcostal transversus abdominis plane block
The patients were monitored with a pulse oximeter, electrocardiograph and non-invasive blood pressure monitor. All the patients were administered PCA with morphine. The bolus dose was fixed at 1 mg with a lockout interval of 10 min and a baseline infusion of 0.1 mg/h. The patients were instructed to use a bolus dose when VAS ≥3. The outcomes measured were success rate, duration of postoperative analgesia and morphine consumption in 24 h. The sensory blockade of T7 and T8 on the right side was assessed 30 min after extubation. The block was considered as successful if there was a sensory blockade. The duration of postoperative analgesia was considered as the time from block completion to the first bolus requirement of morphine. The total morphine consumption in the first 24 h postoperatively was also documented. The patients were observed for the development of any new complications during the period.
The sample size estimation was based on an initial pilot study involving 30 patients with the success rate as the primary endpoint of the study. The study revealed a success rate of 100% with group U and 74% with group L. To detect a 20% difference in success rate with 80% power at the 5% significant level, 35 patients were required in each group. Hence, we recruited 40 patients in each group for the study to compensate for possible dropouts. The data from the pilot study were not included in the final analysis. The data were entered in the MS-Excel spreadsheet (2016) and were analysed using the statistical package for social sciences version 25 (trial version). The descriptive statistics including proportions, measures of central tendency and measures of dispersion were used to describe the data. Further, Student's t-test was used to compare means between the groups and the Chi-square test was used to compare proportions. A P value of <0.05 was considered to be statistically significant.
RESULTS
Eighty-eight patients were assessed for eligibility, and eight patients were excluded from randomisation due to not meeting inclusion criteria or not willing to participate in the study. The CONsolidated Standards of Reporting Trials (CONSORT) flowchart showing the flow of patients in the study has been depicted in Figure 2. No patients were lost to follow-up. The demographic profile like age, sex, height and weight were similar in both the groups. There was no difference in the ASA physical status and duration of surgery. The results are tabulated in Table 1.
Figure 2.
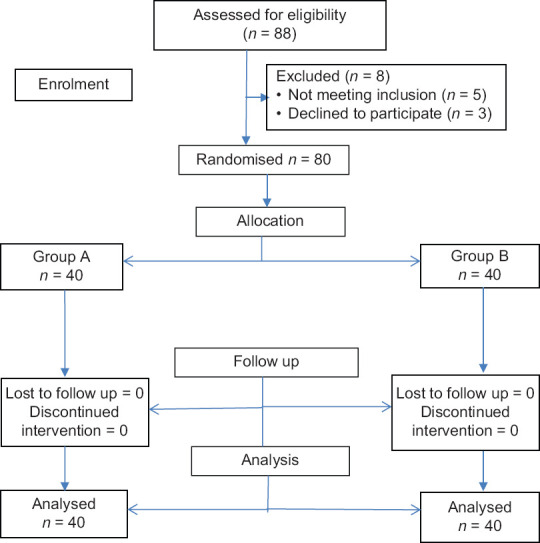
Consolidated Standards of Reporting Trials (CONSORT) flowchart
Table 1.
Demographic characteristics
| Group U | Group L | P | |
|---|---|---|---|
| Gender (male/female) | 12/28 | 15/25 | 0.636* |
| Age (years) | 39.38±8.32 | 38.06±10.06 | 0.506* |
| Height (cm) | 164.47±12.74 | 166.88±14.14 | 0.389* |
| Weight (kg) | 68.55±6.7 | 66.45±7.92 | 0.204* |
| ASA PS I/II | 23/17 | 21/19 | 0.822* |
| Duration of surgery (min) | 52.91±6. 62 | 50.48±5.89 | 0.086* |
Values are in mean±standard deviation (SD) or number of patients. *P not significant; ASA PS -American Society of Anesthesiologists physical status
All the patients in group U had a successful blockade whereas five patients in group L had block failure as assessed by sensory blockade of T7 and T8. But the difference was statistically significant (P-value = 0.054). The data from these five patients were also utilised for final analysis based on intention to treat rather than a per-protocol basis.[5] The duration of postoperative analgesia was 867.24 ± 135.83 min in group U and 751.31 ± 311.22 min in group L (P-value = 0.033) and it was statistically significant. The total consumption of morphine was 4.72 ± 0.94 mg in group U when compared to 5.57 ± 2.53 mg in group L. This was also statistically significant (P-value = 0.049). The results are given in Table 2.
Table 2.
Anaesthetic data
| Group U | Group L | P | |
|---|---|---|---|
| Success rate (%) | 100 | 88 | 0.054* |
| Duration of postoperative analgesia (min) | 867.24±135.83 | 751.31±311.22 | 0.033Ϯ |
| Total morphine consumption (mg) | 4.72±0.94 | 5.57±2.53 | 0.049Ϯ |
Ϯ P significant. Values are in mean±SD or percentage
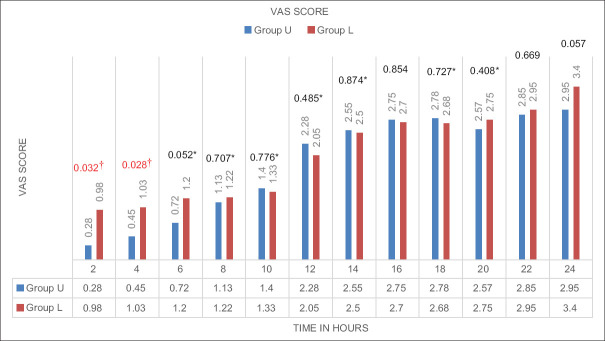
The VAS score was compared between the two groups every 2 h for the first 24 h postoperatively. The VAS score was significantly less in group U than group L for the first 4 h of surgery. There was no statistical significance in the VAS score after 4 h. The graphical representation of the mean VAS score is given in Figure 3. Two patients in group L and one patient in group U had nausea, and it was statistically insignificant. No other complications were observed in both groups.
Figure 3.
Comparison of visual analogue scale (VAS). Values are in mean with P value at the top. *P-value not significant. †P-value significant
DISCUSSION
The objective of our study was to compare the subcostal TAP block performed with the aid of ultrasound with laparoscopy guided technique. We were able to achieve a 100% success rate with the use of ultrasound for the subcostal TAP block. The success rate with the laparoscopic technique was 88%. The duration of postoperative analgesia was significantly prolonged in group U with more reduction in morphine consumption than group L.
LC offers major benefits to the patient such as minimised incision size and trauma with reduced postoperative discomfort, shortened recovery rates and a lower incidence of postoperative wound infections. These factors all contribute to shorter in-patient stay and reduced perioperative morbidity. The cause of pain following LC varies from trocar site incisional pain which is somatic in nature to deep visceral pain as well as referred somatic pain. The tissue trauma occurring during resection of the gall bladder is the single most important factor in determining the severity of pain.[6] But moderate to severe pain in the immediate postoperative period following LC can delay discharge and offset the benefits of laparoscopy.[7]
The subcostal approach to the TAP block has been documented to be effective for upper abdominal surgeries as it blocks the anterior cutaneous branches of the intercostal nerves (T7-T10).[8] Several studies have established the role of ultrasound-guided subcostal TAP block in providing better pain scores and diminishing morphine consumption in LC.[9,10,11] But to perform a UG subcostal TAP block requires an additional skill for anaesthesiologists and not all of them are trained in performing UG nerve blockade. Ultrasound, being an expensive machine, may not be available in all hospitals performing laparoscopy. The use of laparoscopy in performing subcostal TAP block is grossly underutilised and few studies have documented the efficacy of LG subcostal TAP block.[3,12,13] LG TAP block has been proven to be effective in providing postoperative pain relief for other laparoscopic surgeries like colorectal surgery,[14] gynaecological laparoscopy,[15] and robotic-assisted gynaecologic surgery.[16]
The success rate was 100% in group U and 88% in group L. The five failures encountered in the laparoscopic technique may be due to direct non-visualisation of the point of deposition and spread of LA. There were no studies available analysing the success rate of both types of block. Keir et al. did a systematic review of 10 studies and concluded that though TAP block was effective in reducing pain scores and consumption of opioids, it was not superior to local port site infiltration with LA.[1] Siriwardana et al. compared local infiltration with LG TAP block in LC surgeries. They observed that LG TAP block did not provide any additional pain relief in comparison to local infiltration and even commented it can worsen the pain scores. They attributed that the main reason for negative findings in their study was the administration of LA in an inappropriate plane and inexperience of the surgeon performing the block. They concluded that prior training of surgeons in performing laparoscopy guided TAP block might have increased the success rate.[17] However, we were able to achieve a higher success rate by prior training of the surgeon for LG subcostal TAP block before starting the study.
The duration of postoperative analgesia in group U was 14.4 h and 12.51 h in group L. Baral et al. performed bilateral UG subcostal TAP block with 10 mL of 0.25% bupivacaine on either side. The first requirement of rescue analgesic was 3.20 ± 0.84 h which was very less compared to our study. This may be due to the low volume of LA used on one side which might have been inadequate and also no adjuvant was used. Also, they used only paracetamol 1 g at induction and it was not given postoperatively. But we used paracetamol 6th hourly as part of the multimodal regime.[8] Khan et al. compared the UG posterior TAP block with the subcostal approach with 63 patients in each group. Both groups received 20 mL of 0.375% bupivacaine bilaterally and multimodal analgesia with tramadol, ketorolac and paracetamol. They reported that 30% of patients in the posterior TAP block group required additional analgesic and no patient in subcostal TAP block required additional analgesic for 24 h. The longer duration of action of the subcostal TAP block may be due to the multitude of drugs used as compared to only paracetamol in our study.[11]
The VAS score was reduced in the first 4 h of surgery in group U than group L. The score was less than 3 in both the groups. Peng et al. performed a meta-analysis of seven trials and concluded that pain intensity at rest and movement is significantly less at different time points in the postoperative period in patients receiving TAP block.[9] Altıparmak et al. used a numerical rating scale of one to ten in comparing oblique UG subcostal TAP block with erector spinae plane (ESP) block for LC. They found that NRS was less than three in the oblique UG subcostal TAP block though it was higher than in the ESP group. This pain scoring was similar to our study.[6] Vindal et al. compared LG TAP block with port-site infiltration and found VAS score at rest was similar in both the groups except for reduced VAS score at discharge and one week postoperatively in the block group. VAS score at coughing was also reduced at all times in the LG TAP block.[3] The total consumption of morphine was significantly less in group U than group L. Peng et al. in their meta-analysis concluded that TAP block reduced the consumption of opioids and thereby its associated adverse effects.[9] Altıparmak et al. and Baral et al. were able to demonstrate reduced consumption of tramadol and pethidine respectively following UG subcostal TAP block.[6,8] Rajanbabu et al. compared postoperative pain scores and analgesic consumption between bilateral TAP block under direct laparoscopic vision with 15 mL of 0.1% ropivacaine on each side and routine port site infiltration with 30 mL of 0.1% ropivacaine following robotic-assisted gynaecologic surgery. They found significantly reduced pain scores and analgesic consumption for 24 h postoperatively.[16]
We included five cases of block failure from group L in the final analysis. This might be the reason for the prolonged duration of postoperative analgesia, reduced consumption of morphine and reduced VAS score in the first 4 h postoperatively in group U. The incidence of nausea can be attributed to the use of PCA morphine as well as N2O administered during general anaesthesia. We did not encounter any other complications in both the groups emphasizing the safety profile of the subcostal TAP block irrespective of the guidance technique used.
Our study has a few limitations. First, we did not perform a bilateral block as may be needed to manage referred pain from pneumoperitoneum. Since we assumed that surgical resection remains the most common cause of pain, we felt a unilateral block is adequate as part of multimodal analgesia. Second, we did not study the VAS score at movement, which could have given additional data.
CONCLUSION
We conclude that laparoscopic-guided subcostal TAP block is as effective as ultrasound-guided subcostal TAP block with lesser success rate and may be used as a part of multimodal analgesia in places where ultrasound and its technical expertise are not available. Both the techniques are safer and devoid of any serious complications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Keir A, Rhodes L, Kayal A, Khan OA. Does a transversus abdominis plane (TAP) local anaesthetic block improve pain control in patients undergoing laparoscopic cholecystectomy? A best evidence topic. Int J Surg. 2013;11:792–4. doi: 10.1016/j.ijsu.2013.05.039. [DOI] [PubMed] [Google Scholar]
- 2.Venkatraman R, Abhinaya RJ, Sakthivel A, Sivarajan G. Efficacy of ultrasound-guided transversus abdominis plane block for postoperative analgesia in patients undergoing inguinal hernia repair. Local Reg Anesth. 2016;9:7–12. doi: 10.2147/LRA.S93673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vindal A, Sarda H, Lal P. Laparoscopically guided transversus abdominis plane block offers better pain relief after laparoscopic cholecystectomy: Results of a triple blind randomized controlled trial. Surg Endosc. 2020 doi: 10.1007/s00464-020-07558-9. doi: 10.1007/s00464-020-07558-9. [DOI] [PubMed] [Google Scholar]
- 4.Elsharkawy H, Bendtsen TF. Ultrasound-guided transversus abdominis plane and quadratus lumborum blocks. [Last accessed on 2020 Sep 28]. Available from: https://www.nysora.com/regional-anesthesia-for-specific-surgical-procedures/abdomen/ultrasound-guided-transversusabdominis-plane-quadratus-lumborum-blocks/
- 5.Shah PB. Intention-to-treat and per-protocol analysis. CMAJ. 2011;183:696. doi: 10.1503/cmaj.111-2033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Altıparmak B, Korkmaz Toker M, Uysal AI, Kuşçu Y, Gümüş Demirbilek S. Ultrasound-guided erector spinae plane block versus oblique subcostal transversus abdominis plane block for postoperative analgesia of adult patients undergoing laparoscopic cholecystectomy: Randomized, controlled trial. J Clin Anesth. 2019;57:31–6. doi: 10.1016/j.jclinane.2019.03.012. [DOI] [PubMed] [Google Scholar]
- 7.Buvanendran A, Kroin JS. Multimodal analgesia for controlling acute postoperative pain. Curr Opin Anaesthesiol. 2009;22:588–93. doi: 10.1097/ACO.0b013e328330373a. [DOI] [PubMed] [Google Scholar]
- 8.Baral BK, Poudel PR. Comparison of analgesic efficacy of ultrasound guided subcostal transversus abdominis plane block with port site infiltration following laparoscopic cholecystectomy. J Nepal Health Res Counc. 2018;16:457–61. [PubMed] [Google Scholar]
- 9.Peng K, Ji FH, Liu HY, Wu SR. Ultrasound-guided transversus abdominis plane block for analgesia in laparoscopic cholecystectomy: A systematic review and meta-analysis. Med Princ Pract. 2016;25:237–46. doi: 10.1159/000444688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Breazu CM, Ciobanu L, Hadade A, Bartos A, Mitre C, Mircea PA, et al. The efficacy of oblique subcostal transversus abdominis plane block in laparoscopic cholecystectomy - A prospective, placebo controlled study. Rom J Anaesth Intensive Care. 2016;17:67–73. doi: 10.21454/rjaic.7518.231.obq. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khan KK, Khan RI. Analgesic effect of bilateral subcostal tap block after laparoscopic cholecystectomy. J Ayub Med Coll Abbottabad. 2018;30:12–5. [PubMed] [Google Scholar]
- 12.Elamin G, Waters PS, Hamid H, O'Keeffe HM, Waldron RM, Duggan MS. Efficacy of a laparoscopically delivered transversus abdominis plane block technique during elective laparoscopic cholecystectomy: A prospective, double-blind randomized trial. J Am Coll Surg. 2015;221:335–44. doi: 10.1016/j.jamcollsurg.2015.03.030. [DOI] [PubMed] [Google Scholar]
- 13.Tihan D, Totoz T, Tokocin M, Ercan G, Calikoglu TK, Vartanoglu T, et al. Efficacy of laparoscopic transversus abdominis plane block for elective laparoscopic cholecystectomy in elderly patients. Bosn J Basic Med Sci. 2016;16:139–44. doi: 10.17305/bjbms.2015.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Favuzza J, Delaney CP. Laparoscopic-guided transversus abdominis plane block for colorectal surgery. Dis Colon Rectum. 2013;56:389–91. doi: 10.1097/DCR.0b013e318280549b. [DOI] [PubMed] [Google Scholar]
- 15.El sharkwy IA, Noureldin EH, Mohamed EA, Mohamed AA. Laparoscopic-guided transversus abdominis plane block versus trocar site local anesthetic infiltration in gynecologic laparoscopy. Gynecol Surg. 2018;15 doi: 10.1186/s10397-018-1047-3. [Google Scholar]
- 16.Rajanbabu A, Puthenveettil N, Appukuttan A, Asok A. Efficacy of laparoscopic-guided transversus abdominis plane block for patients undergoing robotic-assisted gynaecologic surgery: A randomised control trial. Indian J Anaesth. 2019;63:841–6. doi: 10.4103/ija.IJA_471_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Siriwardana RC, Kumarage SK, Gunathilake BM, Thilakarathne SB, Wijesinghe JS. Local infiltration versus laparoscopic guided transverse abdominis plane block in laparoscopic cholecystectomy: Double-blinded randomized control trial. Surg Endosc. 2019;33:179–83. doi: 10.1007/s00464-018-6291-0. [DOI] [PubMed] [Google Scholar]