Sir,
We would like to share a case series of four morbidly obese patients with traumatic rib fractures requiring respiratory support in the intensive care unit (ICU) and they received erector spinae plane (ESP) block[1] as analgesic adjunct. They were males with median age (interquartile range, IQR), 56 (42–61) years and median body mass index, BMI (IQR) 35.2 (33.0–36.9) kg/m2. They had sustained polytrauma [Table 1] secondary to motor vehicle accidents with multilevel rib fractures and other injuries. They also had multiple comorbidities, required oxygen therapy with non-invasive ventilatory (NIV) support, therefore, being closely monitored in ICU. They received multimodal analgesia regime—intravenous patient-controlled analgesia (PCA) morphine, regular doses of paracetamol, tramadol plus nonsteroidal anti inflammatory drugs (NSAIDs) or coxib since hospital admission. Despite the above analgesic regime, they still experienced severes pain. The median pain scores using numerical rating scale (NRS) were 6.5/10 (IQR 5.25–7.75) at rest and 9/10 (IQR 7.25–10) during movement. The mean daily morphine consumption prior to block was 48 mg (±8 mg). ESP block was given on day 2 of ICU admission because of unsatisfactory pain control, poor cough effort with difficulty to perform chest physiotherapy and requiring NIV support.
Table 1.
Case description
| Case | Demographic and comorbidities | Major injuries sustained | Site of ESP block* | Analgesic medication prior to ESP block & the block timing | Respiratory support and the best daily partial pressure of oxygen (P02) level in ICU | Pain score and 24 hours morphine consumption | |
|---|---|---|---|---|---|---|---|
| A | 38 years old, male; underlying DM, morbid obesity; ASA III | Multiple ribs fractures (Left 1st-7th, 10th-11th, right 1st rib) with bilateral lung contusion, left hemothorax (on chest drain), minimal bilateral pneumothorax and left vertebrae transverse process C7 & T1 fracture | Left | Oral paracetamol 1 g QID, Celebrex 200 mg BD, Cap tramadol 50 mg TDS, PCA morphine; ESP block was given on D2 | D1: HFM 02 and subsequently put on NIV-CPAP, baseline P02 level 84 mmHg on HFM; D2: NIV-CPAP P02 level 150 mmHg; D3: VM 50%, P02 level 110 mmHg; D4: VM30%, P02 level 105 mmHg; D5: NP02, P02 level 110 mmHg D6: NP02, P02 level 115 mmHg; ESP catheter was removed; D7: NP02, P02 level 105 mmHg |
D1: 7(R)/10(M), 58 mg; D2: 7(R)/10(M) pre-block, 2(R)/4(M) post block, 36 mg; D3: 2(R)/4(M), 32 mg; D4: 2(R)/3(M), 26 mg; D5: 2(R)/3(M), 20 mg; D6: 2(R)/4(M), 22 mg; D7: 2(R)/3(M), 16 mg; |
|
| B | 62 years old, male; underlying major depression, DM, morbid obesity; ASA III | Left hemothorax with multiple ribs and sternal - anterior left 1st rib, anterior left 6th rib, and posterior left 3rd to 7th ribs (on chest drain); Left distal 3rd clavicle fracture, sternum body fracture; Grade 1 spleen injury; Right distal 3rd tibia fibula fracture; Acute kidney injury secondary to rhabdomyolysis | Left | Intravenous paracetamol 1 g QID, intravenous tramadol 50 mg TDS, one day trial of Dexmedetomidine infusion (max dose 0.6 mcg/kg/hour); patient was initially on PCA Fentanyl (200 meg usage within 4 hours, not effective) then changed to PCA morphine; ESP block was given on D2 | D1: HFM 02 and subsequently put on NIV-BiPAP, baseline P02 level 80 mmHg on HFM; D2: NIV-BiPAP, P02 level 164 mmHg; D3: VM40%, P02 level 135 mmHg; D4: VM40%, P02 level 110 mmHg; D5: NP02, P02 level 95 mmHg D6: NP02, P02 level 112 mmHg; ESP catheter was removed; D7: NP02, P02 level 120 mmHg; PCA morphine was discontinued; D8: NP02 |
D1: 8(R)/10(M), 48 mg; D2: 8(R)/9(M) pre-block, 2(R)/4(M) post block, 29 mg; D3: 2(R)/4(M), 25 mg; D4: 2(R)/4(M), 26 mg; D5: 2(R)/4(M), 22 mg; D6: 1 (R)/2(M), 8 mg; D7: 1 (R)/2(M), 5 mg; |
|
| C | 55 years old, male; underlying DM, HPT, IHD; active heavy smoker; ASA III | Right pneumothorax (on chest drain), subcutaneous emphysema. Multiple fractures: comminuted fractures at right scapula, right posterior 2nd rib, right posterior 3rd rib, lateral right 7th, 8th, 9th ribs | Right | Oral paracetamol 1 g QID, Celebrex 200 mg BD, Cap tramadol 50 mg TDS, PCA Morphine; ESP block was performed on D2 | D1: HFM 02 and subsequently put on NIV-BiPAP, Fi02 0.6, baseline P02 level 90 mmHg on HFM; D2: NIV-BiPAP, Fi02 0.5, P02 level 117 mmHg; D3: NIV-BiPAP, Fi02 0.4, P02 level 97 mmHg; D4: VM50%, P02 level 98 mmHg; D5: VM50%, P02 level 99 mmHg; ESP catheter was removed; PCA morphine was discontinued; D6: NP02, P02 level 107 mmHg |
D1: 7(R)/8(M), 38 mg; D2: 6(R)/7(M) pre-block, 2(R)/4(M) post block, 17 mg; D3: 1 (R)/3(M), 16 mg; D4: 1 (R)/3(M), 10 mg; D5: 0(R)/2(M) D6: 0(R)/3(M) |
|
| D | 58 years old, male; underlying DM, HPT; ASA III | Small right pneumothorax, subcutaneous emphysema and bilateral lung contusion. Multiple rib fractures with flail segments -anterior and posterior right 1st rib and 2nd ribs, posterior and lateral segments of right 3rd rib, posterior and lateral segments of right 8th rib; rib fractures - posterior right 4th, posterior 5th, 7th and 9th rib, lateral right 6th rib | Right | Oral paracetamol 1 g QID, Celebrex 200 mg BD, Cap tramadol 50 mg TDS, PCA Morphine; ESP block was performed on D2 | D1: HFM 02 and subsequently put on NIV- BiPAP Fi02 0.5, baseline P02 100 mmHg on HFM; D2: NIV-BiPAP Fi02 0.5, P02 104 mmHg; D3: NIV-BiPAP Fi02 0.4, P02 97 mmHg; D4: VM50%, P02 104 mmHg; D5: NP02, P02 125 mmHg; D6: NP02, P02 98 mmHg; ESP catheter was removed; |
D1: 5(R)/8(M), 48 mg; D2: 5(R)/8(M) pre-block, 2(R)/5(M) post block, 34 mg; D3: 1 (R)/3(M), 28 mg; D4: 1 (R)/3(M), 30 mg; D5: 1 (R)/3(M), 22 mg; D6: 1 (R)/4(M), 16 mg; |
*ESP block with catheter was placed on the most painful site of injury; DM, diabetes mellitus; HPT, hypertension; IHD, ischemic heart disease; ASA, American Society of Anesthesiologists; BD, twice daily; TDS, thrice daily, QID, four times a day; PCA, patient-controlled analgesia; HFM, high flow mask; NIV, non-invasive ventilator; BiPAP, bilevel positive airway pressure; CPAP, continuous positive airway pressure; VM, Venturi mask; NP, nasal prong; D1, Day one ICU admission; D2, Day two ICU admission; D3, Day three ICU admission; D4, Day four ICU admission; D5, Day five ICU admission; D6, Day six ICU admission; D7, Day seven ICU admission; D8, Day eight ICU admission; R, worst pain score at rest; M, worst pain score at slightest movement
The blocks were performed using a 10-5 MHz 38 mm linear probe (Sonosite M-Turbo, Bothell, Washington, USA) and an 80 mm, 18-gauge Tuohy epidural needle (Perifix® Filter set, BBraun, Melsungen, Germany) with in-plane needling technique. Patients were placed either in sitting or lateral position, adjusted according to their comfort level as they had multiple injuries and skin wound affecting the positioning. The transverse process of the 3rd or 4th thoracic vertebra was identified. Muscle layers of trapezius, rhomboids major, and erector spinae were identified, and the fascial plane beneath the erector spinae muscle was entered with the Tuohy epidural needle inserted from cranial to caudal direction. The needle placement was confirmed with pumping effect within the fascial plane following hydrodissection and small boluses of local anaesthetic. A total bolus of 40 ml of ropivacaine 0.375% was delivered within the fascial plane and an indwelling Perifix epidural catheter was threaded-in and anchored with 4 cm tip in the fascial plane with transparent film dressing (3M™ Tegaderm™, Maplewood, Minnesota, USA) [Figure 1]. ESP block is a fascial plane block which relies on high volume low concentration local anaesthetic to exert its analgesic efficacy. Luftig et al.[2] recommended a 40 ml local anaesthetic regime for patient above 70 kg in unilateral ESP block. All patients experienced significant pain reduction within 30 min after the block [Figure 1]. A continuous infusion of 8 ml/h ropivacaine 0.2% was run with intermittent bolus of 10 ml ropivacaine 0.2% every 12 h. The intermittent bolus was delivered manually by a trained staff nurse to avoid patient confusion with the PCA morphine device plus no available programmed infusion pump. The median pain scores after ESP block were 2/10 (IQR 2 – 2) at rest and 4/10 (IQR 4.0–4.75) during movement. The pain score remained mild to moderate over the next few days. As patients also had other injuries [Table 1], it would be difficult to achieve zero pain score although other injury sites were not the predominant pain area. Therefore, the mean daily morphine consumption only reduced gradually after ESP block [Table 1]. The median length of ICU stays were 6.5 days (IQR 6–7.75). The median duration of NIV support was 2.5 days (IQR 2–3).
Figure 1.
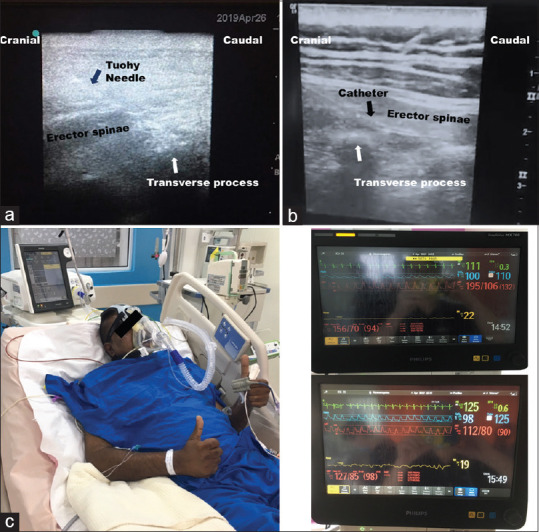
(a) Poor sonoanatomy of the erector spinae plane (ESP) despite optimal adjustment of the ultrasound settings, probe selection and manipulation. The ESP is located deeper (>4 cm). The 18G Tuohy needle is vaguely seen in the trajectory pathway. (b) Sonoanatomy of ESP with catheter in a thin lady (unrelated case), a stark difference of sonoanatomy between a lean and an obese patient. (c) Patient B is on non-invasive ventilator support. Inset – The monitors showed drastic reduction of blood pressure after the ESP block because his pain was alleviated and stress response attenuated
Traumatic rib fractures are very painful. Inadequate pain control would impair breathing, adequate coughing with clearance of pulmonary secretions and compliance with chest physiotherapy. Consequently, patient would be at risk of secondary pulmonary complications, that is, atelectasis, pneumonia, respiratory failure, and the need for respiratory support. Effective analgesia may help to improve a patient's respiratory mechanics and to avoid intubation of the trachea for ventilatory support and therefore may dramatically alter the course of recovery. Multimodal systemic analgesics with intravenous patient-controlled opioid has been the mainstay of pain management and they are usually sufficient for healthy individuals with one to two fractured ribs.[3] However, for more than three to four fractured ribs, studies and experience have reaffirmed that regional techniques like thoracic epidural, thoracic paravertebral, serratus anterior plane, and intercostal blocks provide superior analgesia.[3,4] Regional techniques are particularly useful in elderly patients, patients with multiple rib fractures, and in patients with severe pain or compromised pulmonary function.[3] However, epidural analgesia and paravertebral block may not be feasible in the presence of anti-coagulation, multisystem trauma, haemodynamic instability, or in patients unable to be optimally positioned.[3] ESP block was the most feasible regional technique in our case series because patients were obese. The quality of the ESP sonoanatomy was already below average and located deeper (>4 cm) [Figure 1] despite optimal adjustment of the ultrasound settings (knob), probe selection, and probe manipulation. The paravertebral space which is anatomically located deeper than ESP could not be properly visualised during scout scan, therefore we did not attempt paravertebral blocks. A literature review showed that there are three case reports[5,6,7] and one retrospective cohort study[8] about the use of ESP block for pain relief in rib fractures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We thank Dr Siew Gee Ho for helping us to trace the clinical progress and outcome of the above-mentioned cases.
REFERENCES
- 1.Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block. A novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41:621–7. doi: 10.1097/AAP.0000000000000451. [DOI] [PubMed] [Google Scholar]
- 2.Luftig J, Mantuani D, Herring AA, Dixon B, Clattenburg E, Nagdev A. The authors reply to the optimal dose and volume of local anesthetic for erector spinae plane blockade for posterior rib fractures. Am J Emerg Med. 2018;36:1103–4. doi: 10.1016/j.ajem.2018.03.051. [DOI] [PubMed] [Google Scholar]
- 3.Thiruvenkatarajan V, Cruz Eng H, Adhikary SD. An update on regional analgesia for rib fractures. Curr Opin Anesthesiol. 2018;31:601–7. doi: 10.1097/ACO.0000000000000637. [DOI] [PubMed] [Google Scholar]
- 4.Beard L, Hillermann C, Beard E, Millerchip S, Sachdeva R, Gao Smith F, et al. Multicenter longitudinal cross-sectional study comparing effectiveness of serratus anterior plane, paravertebral and thoracic epidural for the analgesia of multiple rib fractures. Reg Anesth Pain Med. 2020;45:351–6. doi: 10.1136/rapm-2019-101119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hamilton DL, Manickam B. Erector spinae plane block for pain relief in rib fractures. Br J Anaesth. 2017;118:474–5. doi: 10.1093/bja/aex013. [DOI] [PubMed] [Google Scholar]
- 6.Luftig J, Mantuani D, Herring AA, Dixon B, Clattenburg E, Nagdev A. Successful emergency pain control for posterior rib fractures with ultrasound-guided erector spinae plane block. Am J Emerg Med. 2018;36:1391–6. doi: 10.1016/j.ajem.2017.12.060. [DOI] [PubMed] [Google Scholar]
- 7.Nandhakumar A, Nair A, Bharath VK, Kalingarayar S, Ramaswamy BP, Dhatchinamoorthi D. Erector spinae plane block may aid weaning from mechanical ventilation in patients with multiple rib fractures: Case report of two cases. Indian J Anaesth. 2018;62:139–41. doi: 10.4103/ija.IJA_599_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adhikary SD, Liu WM, Fuller E, Cruz-Eng H, Chin KJ. The effect of erector spinae plane block on respiratory and analgesic outcomes in multiple rib fractures: A retrospective cohort study. Anaesthesia. 2019;74:585–93. doi: 10.1111/anae.14579. [DOI] [PubMed] [Google Scholar]


