Abstract
Ischaemic stroke is a rare manifestation of hypercoagulability induced by underlying malignancy. It is proposed that paraneoplastic non-bacterial thrombotic endocarditis (NBTE) is the most common cause, predisposing to the formation of friable valvular lesions composed of platelets and fibrin that embolize commonly. Pancreas, gallbladder, stomach, colon and gynaecological malignancies have all been associated with NBTE. We describe a female patient who presented to our facility with syncope and limb weakness. Magnetic resonance imaging of the brain revealed ischaemic strokes in both the anterior and posterior circulation. Further investigation revealed a pelvic mass that was biopsy proven to be ovarian malignancy. Prognosis is heavily reliant on disease stage, thus diagnostic clues suggesting the possibility of underlying malignancy in the presentation of stroke should prompt a thorough investigation to exclude malignancy.
INTRODUCTION
Ischaemic stroke is an uncommon presenting sign of malignancy. Most ischaemic strokes have a detectable medical cause such as cardio-embolism, large vessel atherosclerotic disease or small vessel disease [1]. However, unrecognised thrombophilia including occult malignancy is an important aetiology to consider in stroke presentations, particularly when the infarct exceeds the supply territory of a single vessel and other causes have been excluded [2, 3]. Subtle clues in the absence of a clear aetiology, such as raised D-dimer, thrombocytopenia, elevated tumour markers and characteristic cerebral infarction imaging patterns [3], suggest further investigation to exclude malignancy which is warranted, particularly as early detection remains an essential driver of improved prognosis. We describe a case of multifocal stroke as the first presenting sign of an underlying ovarian malignancy in a 64-year-old female.
CASE REPORT
A 64-year-old female presented to the emergency department after an episode of syncope and sudden onset right hemiplegia. One week prior, she had experienced a syncopal episode that resulted in a minor car accident without serious injury. On further history, the patient reported having experienced several pre-syncopal events, discoordination and episodic loss of fine motor skills in the previous 2 weeks. There was no associated history of fevers or weight loss and there were no significant risk factors for bacterial endocarditis such as intravenous drug use, implantable cardiac devices, rheumatic fever or dental decay.
The patient had a history of achondroplasia/metaphyseal dysplasia and a family history of multiple sclerosis. There was no history of hypertension, dyslipidaemia, diabetes mellitus or prior vascular disease.
On examination, tone was increased in the right upper and lower limbs and muscular power in the right limbs was reduced to movement against gravity. There was reduced sensation to pinprick and fine touch on the right side of the body. Knee and elbow reflexes were brisker on the right than the left and the right plantar reflex was upgoing.
The cardiovascular, respiratory and gastrointestinal examinations were normal except for very prominent splinter haemorrhages (Fig. 1).
Figure 1.

Impressive splinter haemorrhages of both hands at the time of presentation.
Initial investigations were as follows: haemoglobin 137 g/L, WCC 9.3 × 109, neutrophils 8.0 × 109, platelet count 147 × 109, D-dimer 18.5 (NR < 0.5), troponin 1621 ng/L (NR < 11), PT 12.3 secs (NR 10.0–14.0), APTT 29 secs (NR 26–36), creatinine 48 umol/L and eGFR > 90.
The patient was admitted for further investigation. MRI brain demonstrated multiple sites of ischaemic change in both the anterior and posterior circulation (Fig. 2). A cardiac embolic source was considered and TTE demonstrated a small hypoechoic focus 6 mm ×3 mm on the aortic annulus reported as representing either thrombus or atheroma. Further serological testing ruled out autoimmune and inflammatory conditions. A CT aortogram + coronary angiogram to exclude dissection or coronary artery disease given the rise in troponin noted an incidental pelvic mass (Fig. 3) thought to be arising from the adnexa. A confirmatory pelvic ultrasound reported a lesion arising from the right ovary with complex and vascular structure. CA 125 was >1500 (normal ref < 100). The patient was transferred to a tertiary centre with specialist onco-gynaecological and general surgical services for biopsy, which confirmed stage III high-grade serous ovarian cancer.
Figure 2.
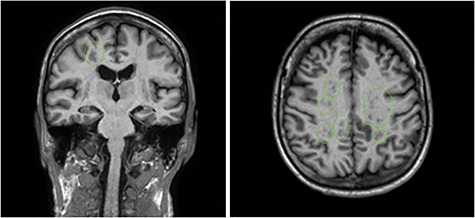
MRI brain demonstrating multifocal infarctions in both the anterior and posterior circulation, consistent with a cardioembolic source.
Figure 3.
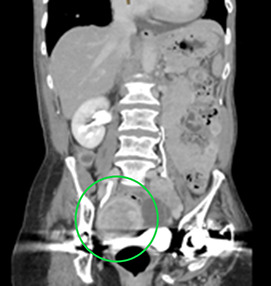
CT aortogram demonstrating a suspicious lesion arising from the right adnexa. Ultrasound confirmed a complex, vascular lesion arising from the right ovary and later biopsy proven as high-grade serous ovarian cancer.
DISCUSSION
This case demonstrates ovarian malignancy as an uncommon cause of multifocal embolic stroke. Although rare, it remains important to consider that stroke may be the preceding event to the diagnosis of malignancy [5]. There are a number of case reports in the literature and a wider retrospective review of 5106 stroke patients demonstrated that 24 of the cohort had occult malignancy [8]. This reinforces the importance of a thorough investigation to exclude the diagnosis if malignancy is suspected.
Ovarian cancer has been reported in the literature to have a propensity to manifest with ischaemic stroke, and is one of the more common malignancies associated with this type of presentation [3]. The pathophysiological basis is proposed to relate to systemic changes associated with the paraneoplastic disruption of normal clotting, endothelial disruption and platelet activation [3, 4]. Normal clotting is disturbed through hypercoagulability and disseminated intravascular coagulation, representing the complex interplay of tumour produced procoagulants and inflammatory cytokines on the clotting process [5]. Endothelial disruption may damage valvular surfaces causing them to become thrombogenic [3], resulting in non-bacterial thrombotic endocarditis (NBTE) which may cause subsequent systemic embolization. NBTE has been reported as a manifestation of numerous malignancies, such as pancreas, stomach, colon, liver, gallbladder and ovarian [3]. Clinically, this is seen as valvular lesions composed of platelets and fibrin [6].
Case series reporting these principal mechanisms in stroke related to occult malignancy [5] have amalgamated diagnostic clues which point the clinician towards the diagnosis. These include elevated D-dimer, thrombocytopenia, thrombophilia or raised tumour markers [3–6]. In addition, diffusion-weighted imaging demonstrates a typical uniform multifocal ischaemic stroke that is widely distributed across vascular territories [7]. Our patient’s laboratory and imaging results further validated these observations having raised D-dimer, tumour markers, thrombocytopenia and characteristic imaging features supportive of NBTE.
CONCLUSION
Although an uncommon presentation malignancy should be considered as an underlying aetiology for ischaemic stroke, particularly in the absence of an identifiable cause and when the stroke exceeds a single vessel territory of supply, early diagnosis is important as cancer progression affects prognosis. It is a reminder of the importance of a multidisciplinary approach across medical and surgical specialities in the diagnosis and subsequent treatment of malignancy as the presenting clues may be subtle.
CONFLICT OF INTEREST STATEMENT
None declared.
References
- 1. Guercini F, Acciarresi M, Agnelli GPM. Cryptogenic stroke: time to determine aetiology. J Thrombosis Haemostasis 2008;6:549–54. [DOI] [PubMed] [Google Scholar]
- 2. Goedee S, Naber A, Rovers JM, Roks G. Ischaemic stroke as initial presentation of systemic malignancy. Case Rep 2014;2014:bcr2013202122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Borowski A, Ghodsizad A, Gams E. Stroke as a first manifestation of ovarian cancer. J Neuro-oncol 2005;71:267–9. [DOI] [PubMed] [Google Scholar]
- 4. Schwarzbach CJ, Schaefer A, Ebert A, Held V, Bolognese M, Kablau M, et al. Stroke and cancer: the importance of cancer-associated hypercoagulation as a possible stroke etiology. Stroke 2012;43:3029–34. [DOI] [PubMed] [Google Scholar]
- 5. Chen W, He Y, Su Y. Multifocal cerebral infarction as the first manifestation of occult malignancy: case series of trousseau's syndrome and literature review. Brain Circ 2018;4:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Oueida Z, Scola M. Ovarian clear cell carcinoma presenting as non-bacterial thrombotic endocarditis and systemic embolization. World J Oncol 2011;2:270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Singhal AB, Topcuoglu MA, Buonanno FS. Acute ischemic stroke patterns in infective and nonbacterial thrombotic endocarditis: a diffusion-weighted magnetic resonance imaging study. Stroke 2002;33:1267–73. [DOI] [PubMed] [Google Scholar]
- 8. Taccone FS, Jeangette SM, Blecic SA. First-ever stroke as initial presentation of systemic cancer. J Stroke Cerebrovasc Dis 2008;17:169–74. [DOI] [PubMed] [Google Scholar]


