SUMMARY.
Objective:
This study considers four hypotheses regarding the impact of extended involuntary outpatient commitment orders on services utilization.
Method:
All Victorian Psychiatric Case Register (VPCR) patients who had extended (180+ day) outpatient commitment orders in the nine year study period and a matched treatment compliant comparison group with extended periods of outpatient care (N = 1182), both with at least two years of post-episode experience, were evaluated. Pre/post episode utilization was compared via paired t tests with individuals as their own controls. Logistic and OLS regression as well as repeated measures ANOVA via the GLM SPSS program and post hoc t tests were used to evaluate between group and across time differences.
Results:
Extended episodes of care for both groups were associated with reduced use of hospitalization and increases in outpatient services. Extended orders did not promote voluntary participation in the post-period. Outpatient services during the extended episode for those on orders were raised to the level experienced by the treatment compliant comparison group and maintained at that level via subsequent renewal of orders throughout the patients’ careers. OLS regression results indicate that approximately six community care service days were required for those on orders to achieve a one-day reduction in hospital utilization following the extended episode.
Conclusion:
Outpatient commitment for those on extended orders in the Victorian context enables a level of community-based services provision, unexpected in the absence of this delivery system, which provides an alternative to hospitalization.
Keywords: Outpatient commitment, Victorian Psychiatric Case Register (VPCR), OLS regression, mental health
Involuntary outpatient commitment provisions are explicitly written into mental health laws in Australia, the United Kingdom, New Zealand, and 41 states and the District of Columbia in the United States (1–5). Though varying in their provisions, outpatient commitment orders require individuals (refusing care and believed potentially dangerous/gravely disabled due to a mental disorder) to accept community treatment or hospital release conditioned on treatment compliance (6). Such compliance may extend to requiring people to live in a particular apartment, take prescribed medications, attend counseling sessions, and abstain from substance utilization (1). Patients who do not comply with the treatment regimen in most jurisdictions may be admitted to a psychiatric hospital for involuntary care. In effect, the patient’s status becomes one of conditional discharge from a psychiatric hospital whether or not they have been in the hospital (in some jurisdictions, orders may be issued without taking the individual to the hospital). This study looks at nine years of experience with the use of outpatient commitment in Victoria, Australia (see Table 1). It considers the claimed effectiveness of extended orders–outpatient commitments lasting longer than 180 days (3,4,7)–and moves beyond existing research by considering the complete patient careers of those put on orders and a matched treatment compliant comparison sample.
TABLE 1.
Victoria’s Outpatient Commitment: Community Treatment Orders
| Outpatient commitment orders require individuals to accept outpatient treatment or hospital release conditioned on treatment compliance. |
| Victoria’s Eligibility Criteria: All of the following must obtain, |
|
| How is outpatient commitment implemented in Victoria? |
|
| Patient Obligations? |
|
| What type of oversight is required? |
|
Outpatient commitment research has produced mixed results. Two major clinical trials in New York and North Carolina randomized small groups of patients (142 and 252 respectively) with mixed diagnoses at various points in their treatment careers to outpatient commitment and no outpatient commitment conditions and followed them for a year (3,8,9). Both studies failed to find significant differences between the randomized groups on any behavioral variables. In a secondary analysis, sacrificing the randomized component of the study, the North Carolina group found less hospital utilization among extended outpatient commitment patients (those with 180+ days on orders during the follow-up year). Four other studies, without comparison samples, are often cited as evidence that outpatient commitment reduces hospital admissions and the duration of hospital stays (10–13). Despite the failure of the controlled trials to show differences attributable to outpatient commitment in the randomized group comparisons, the positive findings from the non-controlled studies and the extended outpatient commitment strategy of the North Carolina group, lead Applebaum (5), in an evaluation of the preponderance of evidence on such orders, to indicate that “… the weight of the evidence and clinical experience now favor efforts to implement reasonable schemes of outpatient commitment …” (p. 350). Following on the claims of the effectiveness of extended orders, advocates have come to see the extended period of such commitment as one such reasonable scheme (14). Given a need to replicate such findings, and a concern about the generalizability of the North Carolina results, further investigation of outpatient commitment and particularly its most promising scheme–180+ day extended orders–seems warranted.
In Victoria, Australia, the public mental health system covers 4.7 million inhabitants mandating a prescribed strategy of care emphasizing the desirability of community over inpatient treatment and care in the “least restrictive environment” (16–18). Since 1986 Victoria has relied on both the extensive use of outpatient commitment (to insure participation in prescribed care by patients believed unable to voluntarily accept needed treatment) and the aggressive and comprehensive out-reach treatment approach employed in the Program In Assertive Community Treatment Model (PACT) (17). Mental health workers are expected to be in contact with the patient with a frequency dictated by the patient’s condition and need for treatment. Given extended observation of different treatment teams (i.e., participation in home visits, counseling sessions, regular staff meetings involving the passing of care from one outpatient team shift to another, staffings involving extensive discussions of how, why and when an outpatient commitment should be employed, and watching several decisions to authorize such an order), it would appear that orders are initiated when team members cannot engage the patient in the services deemed necessary to ensure effective care–e.g., the patient, continuing to evidence disturbed behavior, does not attend counseling sessions or is absent when the team member visits so medication compliance cannot be adequately monitored. The objective of issuing orders is to prevent hospitalization by re-enabling contact with the patient with a frequency the team believes is necessary to insure compliance with prescribed treatment. Outpatient commitment can therefore be considered a successful alternative to hospitalization if it brings the level of service contact to that indicative of compliance with prescribed treatment.
Given previous research and the Victorian treatment objectives, the following four hypotheses are evaluated herein:
Extended outpatient commitment allows for relatively less use of inpatient treatment and will be accompanied by an increase in community care utilization (3).
Compliance post orders will be reflected in increases in voluntary care utilization (15).
Outpatient commitment will enable the level of service provision to approximate that observed in a treatment compliant group.
METHODS
Sample
This retrospective study compares the service utilization of individuals placed on extended outpatient commitments, with a comparison group not placed on orders that experienced a psychiatric hospitalization and a voluntary extended period of community treatment, a treatment compliant sample. To the extent possible the groups are matched on variables influencing the probability of experiencing inpatient care episodes (19)–i.e., diagnosis, and gender and age (within 5 years). While the match is identical on diagnosis, it was not perfect on the latter two variables though all possibilities were exhausted.
The Victorian Psychiatric Case Register (VPCR) provides a record of all clinical contacts and their character occurring within the State. With approval of their ethics committee, the Victorian Department of Human Services approved our access to the register data. All patients having ever experienced an outpatient commitment between 12/11/90 and 30/6/00 (a period when in- and outpatient mental health service utilization and outpatient commitment could be reliably mapped using the VPCR) were identified along with a matched comparison sample (N = 7,826 pairs). In order to insure that we had information on the patient’s entire pre-episode career and adequate post-episode follow-up (two years), we selected only those pairs (N = 2073 pairs) whose first contacts with the mental health system were on or later than 12/11/90 and who had first community care episode end dates prior to 30/6/98. Of these pairs, 1794 had complete outpatient commitment information–i.e., 86.5% of the sample; 591 pairs included both a patient with a 180+ day order and a matched comparison group member with a 180+ day community care episode (other pairs had patients with orders of shorter duration or no matched comparison with an extended care episode). The 591 pairs (N = 1182) constituted our evaluation sample.
Units of Analysis
In documenting the treatment career experience, all treatment contacts were organized into episodes of care: each hospitalization (from day of admission to day of discharge) was considered a separate inpatient episode; each continuous period of community provision without a break in service ≥ 90 days, a community care episode (20). A service break followed by re-initiation of care was considered the start of a new community care episode. All occasions of community service are reported as community treatment days; multiple occasions of community service on the same day count as one community treatment day.
We consider the legal conditions under which treatment contacts occurred, reporting statistics separately for voluntary, involuntary, and combined total service utilization. Comparisons are based on yearly numbers of inpatient hospitalizations, hospital days, and/or community treatment days, thus adjusting for the period that the patient is at known risk for hospitalization or community service. A patient’s career risk period is the date of first system contact to ninety days following the last system contact. If a patient left the area or died, this information can only be known by a ninety-day lapse in contact. Risk prior to the initial extended episode is measured from the patient’s first date of system contact to the start date of the extended episode. Rates per year never reflect more treatment experiences than the patient actually had.
Analyses (Employing the SPSS Statistical Package (21))
Hypotheses 1 and 2: Reduced use of hospital and increased post-period voluntary compliance. Using paired t tests, patients were considered within groups as their own comparisons. Patient experiences before the start of their first 180+ day episode were compared to their experiences after episodes’ end. We assumed that the “before” experience would be significantly altered in the post-episode period and that the post-episode period experience would demonstrate whether treatment compliance could be voluntarily maintained (18).
Hypothesis 3: Substitution of community care for inpatient. Logistic and OLS Multiple Regression analyses were completed to respectively evaluate whether the interaction effect of extended outpatient commitment and the receipt of community care significantly contributed to avoiding post-period hospitalization or reducing post-period inpatient days. Three groups of predictors were included in each model: 180+ day episode duration, and duration of the follow up period, as controls for exposure; age, gender, never married, under 65 and living on pension, as previously demonstrated independent influences on hospital utilization; inpatient utilization per year prior to the 1st 180+ day episode, as a severity adjustment (22); and, community care days per year following the start of the episode, group membership and the interaction of the later two variables, the interventions.
Hypothesis 4: Outpatient commitment will enable service contact to approximate that observed in a treatment compliant group. In making between group and across time comparisons we used the GLM program to consider overall differences in utilization of community services and to address two post hoc comparisons: community treatment utilization differences between groups during the extended episode and during vs. post-episode for the group on orders.
RESULTS
The sample’s ICD-9CM primary diagnoses are: schizophrenia (N = 1050, 88.8%), major affective disorder (N = 60, 5.1%), and other conditions (N = 72, 6.1%). Though matched on diagnosis, age within five years, and gender there were differences between groups on the latter two variables (see Table 2). While no statistical differences were found in the duration of the follow up periods for the two groups, the time of their involvement with the system prior to their initial extended episode, the duration of that episode, their career hospitalizations, and the extent of community involvement prior to each of their admissions, did differ. The first finding allows us to make post-period between group comparisons with greater confidence regarding intervention exposure effect comparability; the latter differences are taken into account in the statistical models and by making our comparisons based on yearly utilization. Further, the treatment compliant status of the comparison group seems to be validated in that this group voluntarily participated in community treatment for an average period of 392 days. While it is difficult to define treatment compliance, such participation among those meeting hospitalization criteria seems a reasonable test.
TABLE 2.
Demographics and Design Relevant Patient Career Statistics
| Characteristic | Comparison | Outpatient Commitment | Total |
|---|---|---|---|
| N (%)/M (sd) | N (%)/M (sd) | N (%)/t,df,p | |
| Total Sample | 591 (50%) | 591 (50%) | 1182 (100%) |
| Gender | |||
| Male | 415 (70.2%) | 350 (59.2%) | 765 (64.7%) |
| Female | 176 (29.8%) | 241 (40.8%) | 417 (35.3%) |
| Age at First Date | 26.59 (11.10) | 34.01 (16.01) | 30.31 (14.26) |
| Marital Status | |||
| Divorced | 32 (5.4%) | 49 (8.3%) | 81 (6.9%) |
| Defacto Cohabiting Partner | 28 (4.7%) | 27 (4.6%) | 55 (4.7%) |
| Married (Legally) | 60 (10.2%) | 73 (12.4%) | 133 (11.3%) |
| Never Married | 422 (71.4%) | 339 (57.4%) | 761 (64.4%) |
| Separated | 33 (5.6%) | 59 (10.0%) | 92 (7.8%) |
| Widowed | 5 (0.8%) | 34 (5.8%) | 39 (3.3%) |
| Unknown | 11 (1.9%) | 10 (1.7%) | 21 (1.8%) |
| Duration of 1st 180+ Day Episode | 492 days (sd 382) | 391days (sd 214) | t = 5.56, df 590, p < .000 |
| Duration of Follow-up Period | 904 days (sd 742) | 841 days (sd 667) | t = −1.57, df = 590, p = .115 |
| Days From 1st System Contact To 1st 180+ Day Episode | 374 days (sd 526) | 685 days (sd 612) | t = −9.81, df = 590, p < .000 |
| Average # of Times Community Involved Prior to Admission | 2.52 (sd 1.94) | 4.36 (sd 3.51) | t = −12.1, df = 460, p < .000 |
Hypotheses 1 and 2: Findings indicate a reduced use of hospital, an increase in post-period community care, but no increase in post-period voluntary compliance. Table 3 shows that patients on orders were hospitalized on average 56.3 days per year before the extended episode and only 19.6 days per year after. Their number of community treatment days increased from 27.5 days per year to 41.1 days per year in the respective periods. The comparison sample was hospitalized on average 37.2 days per year before and only 10.4 days per year after. Their number of community treatment days increased from 13.3 days per year to18.8 days per year. The differences are significant at p < .000 as are all before and after comparisons in Table 3 with one noted exception. Increases in voluntary community treatment days were not significant for those on orders. For this group the increases were primarily in the involuntary community treatment day category. For the comparison group community treatment day increases were all in the voluntary category. (The few involuntary community contacts reflect involvement of community-based staff during an involuntary hospitalization to insure continuity of care; involvements decreased across periods due to actual reductions in involuntary hospitalizations.)
TABLE 3.
Service Utilization Before, During, and After First 180 Day Episode (N = 591)
| Outpatient Commitment Group | Comparison Group | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Service Type | Before Start | During | After End | Before Start | During | After End | ||||||
| Hospitalization | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
| Inpatient Days | ||||||||||||
| Involuntary | 47.3 | 55.4 | NA | NA | 17.0 | 32.0 | 25.8 | 33.0 | NA | NA | 5.9 | 14.4 |
| Voluntary | 9.1 | 27.1 | NA | NA | 2.6 | 8.4 | 11.4 | 25.6 | NA | NA | 4.5 | 18.1 |
| Total | 56.3 | 82.5 | NA | NA | 19.6 | 40.4 | 37.2 | 58.6 | NA | NA | 10.4 | 32.5 |
| Number of Admissions | ||||||||||||
| Involuntary | 1.3 | 0.9 | NA | NA | 0.6 | 0.8 | 0.9 | 0.7 | NA | NA | 0.4 | 0.7 |
| Voluntary | 0.3 | 0.6 | NA | NA | 0.1 | 0.4 | 0.5 | 0.8 | NA | NA | 0.3 | 0.5 |
| Total | 1.7 | 1.5 | NA | NA | 0.7 | 1.2 | 1.4 | 1.5 | NA | NA | 0.7 | 1.2 |
| Average Length of Stay in Days | ||||||||||||
| Involuntary | 24.0 | 34.6 | NA | NA | 7.0 | 14.1 | 19.4 | 24.5 | NA | NA | 4.3 | 10.5 |
| Voluntary | 5.9 | 22.6 | NA | NA | 1.8 | 7.0 | 7.3 | 15.7 | NA | NA | 2.6 | 13.4 |
| Community Care Days | ||||||||||||
| Voluntary | 18.3 | 22.2 | .2 | 3.8 | 19.9 | 26.5 | 11.7 | 17.4 | 41.8 | 24.7 | 18.1 | 22.3 |
| Involuntary | 9.2 | 17.9 | 42.3 | 32.7 | 21.2 | 34.4 | 1.5 | 2.9 | .5 | 4.1 | 0.7 | 2.4 |
| Totals | 27.5 | 40.2 | 42.8 | 32.3 | 41.1 | 61.0 | 13.3 | 20.2 | 42.0 | 24.6 | 18.8 | 24.7 |
Hypothesis 3: There was a significant substitution of outpatient care for inpatient care. Table 4 shows the results of the logistic and OLS regressions predicting, respectively, post-period hospitalization and post-period utilization of inpatient days. The logistic model is significant (Chi Sq. 423.265, df 10 p < .000) and demonstrates that when all factors are taken into account each day of community treatment decreases the chance of hospitalization in the post-period for the outpatient commitment group by 3.2% over those in the comparison group. The OLS model is significant (AdjRsq = .101, F = 13.202, df = 10,1089, p < .000). It shows a significant outpatient commitment group by community care service days interaction (b = −.16, se .06, p < .004) such that for the outpatient commitment group (with all other covariates and demographics controlled) one community treatment day is associated with a .16 reduction in inpatient days per year during the period after the episode end; alternatively six community treatment days with a one (.96) day reduction in inpatient utilization.
TABLE 4.
Hospitalization and Inpatient Days Post Period Following 1st 180+ Day Community Episode
| A. Hospitalization in the Post Period Logistic Regression Model* | ||||||
|---|---|---|---|---|---|---|
| Variables in the Equation** | ||||||
| B | S.E. | Wald | df | Sig. | Exp(B) | |
| • GROUP = Outpatient Commitment v Comparison | .696 | .289 | 5.797 | 1 | .016 | 2.006 |
| • Community Service days per year after the start of the 1st 180+ Day Episode | .039 | .006 | 41.912 | 1 | .000 | 1.040 |
| • Interaction: Outpatient Commitment Group by Community Service Days After the Start of the 1st 180+ Day Episode | −.032 | .006 | 28.456 | 1 | .000 | .968 |
| *Dependent variable: Hospitalized in the post period (Chi Sq. 423.265, df 10 p < .000). | ||||||
| **Predictor Variables in the Equation: Group, interaction of group by treatment days after the start of the 180+ episode, age, gender, never married, pension income, follow-up period duration, 1st 180+ period duration, inpatient days per year prior to the 1st 180+ episode, treatment days following the start of the 180+ episode. Only the main group and service effects, and the interaction effect are shown. | ||||||
| B. Inpatient Days Per Year in the Post Period OLS Regression Model | |||||
|---|---|---|---|---|---|
| Unstandardized Coefficients | Standardized Coefficients | t | Sig. | ||
| B | Std. Error | Beta | |||
| (Constant) | 7.495 | 4.482 | −1.672 | .095 | |
| • Group: (Outpatient Commitment = 1, Comparison = 0) | 8.411 | 2.906 | .152 | 2.894 | .004 |
| • Community service days per year after the start of the 1st 180+ Day Episode | .223 | .054 | .519 | 4.124 | .000 |
| • Interaction of Outpatient Commitment Group by Community Service Days After the Start of 180 Day Episode | −.161 | .056 | −.424 | 2.893 | .004 |
| *Dependent variable: Total inpatient days per year after the end of the 1st 180 episode; R = .330, Rsq = .101, Adj. Rsq. = .101, F = 13.202, D.f. = 10,1089, p < .000. | |||||
| **Predictor Variables in the Equation: Group, interaction of group by treatment days after the start of the 180+ episode, age, gender, never married, pension income, follow-up period duration, 1st 180+ period duration, inpatient days per year prior to the 1st 180+ episode, treatment days following the start of the 180+ episode. Only the main group and service effects, and the interaction effect are shown. | |||||
Hypothesis 4: Outpatient commitment enabled service contact to approximate that observed in a treatment compliant group. The groups differed in their utilization of outpatient services across the three points in time (F = 106.51, p < .000) as did the subjects within groups (F = 297.22, p < .000). Of most importance, however, is the absence of significant differences between groups in their yearly community service utilization during the extended episode and between the episode and post episode periods for the group on orders (see Figure 1).
FIGURE 1.
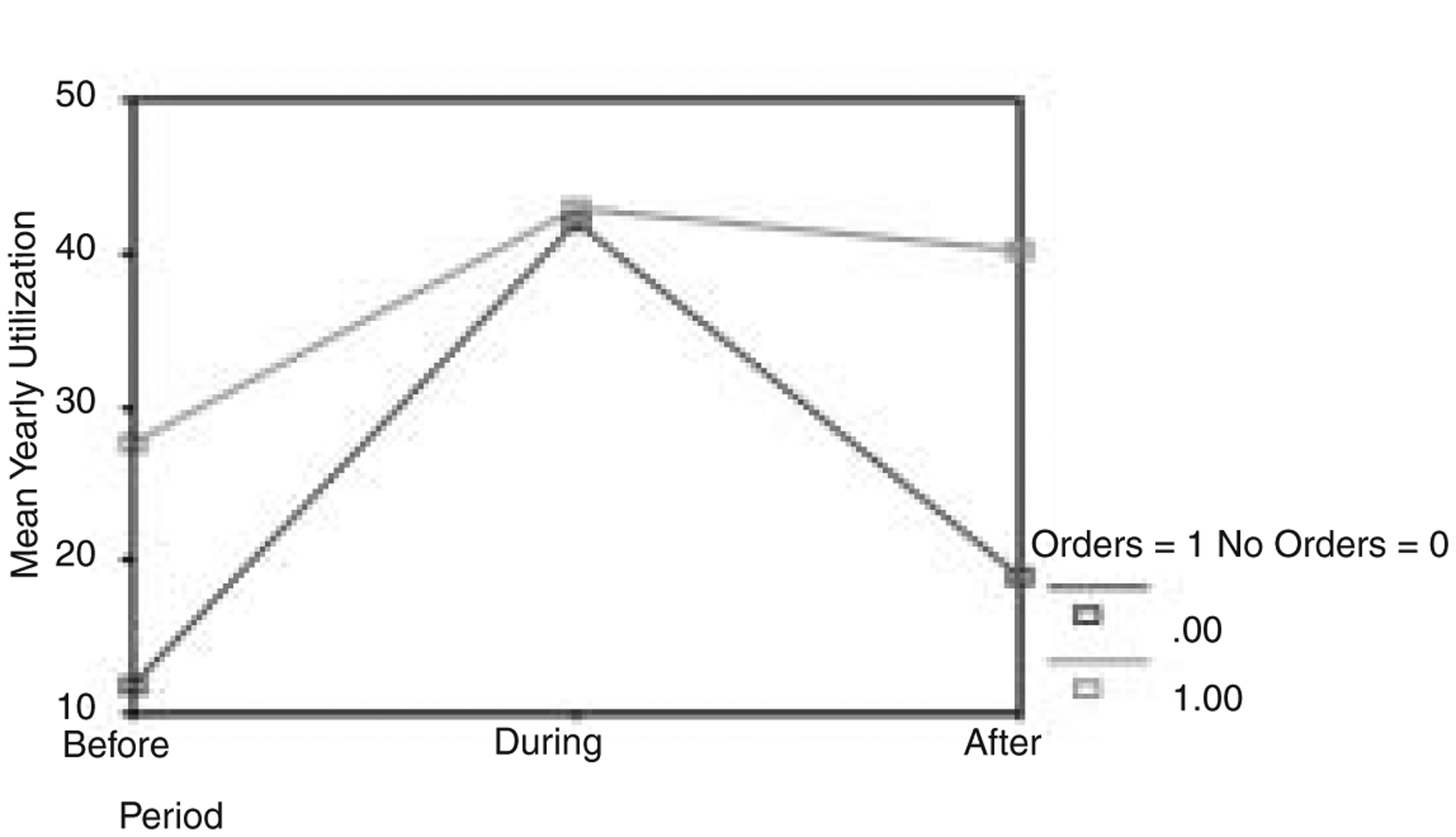
Yearly Service Utilization Before, During, and After Episode
DISCUSSION
Comparisons of the pre/post extended community care episode utilization experiences of both groups show reduced use of hospitalization, approximately a month per year per patient, and dramatic increases in community services, approximately a third more service utilization than in the pre-period. This is, however, only a partial support of the first hypothesis since proportionally the reductions and increases are similar for both groups and might be attributed to deinstitutionalization policy in Victoria or simple regression to the mean. Most important, however, with respect to evaluating the utility of outpatient commitment, is that the equivalent proportional increase in the community services for the group on orders, and perhaps the proportional reduction in the hospitalization, only arises because of the provision of ordered community care.
Outpatient commitment is a way of delivering services to a population that for one or another reason cannot or will not consistently accept such service voluntarily. It would appear that the role of the outpatient commitment during the extended episode is to raise the level of outpatient service to that provided to the treatment compliant comparison sample. We observed no difference in the total amount of community services used in both groups during the extended episode–the comparison group received them voluntarily, the committed group under orders. Extended orders from their initiation represent a change in the way of packaging services for a patient and the process is continued via renewals following the initial episode’s end throughout the patient’s career. Long-term service participation under orders does not presage a shift to voluntary participation.
Outpatient commitment provided an alternative to hospitalization during the episode when no hospitalization occurred as well as in the post-period. In the post-period our regression analyses demonstrate that it is the combination of community services enabled by outpatient commitment that facilitate the reduction of hospital utilization in the population on extended orders. In the outpatient commitment group this results in the substitution of approximately six outpatient community treatment days for each reduced inpatient day per year in the period after the end of the 1st extended episode. Thus, extended outpatient commitment enables community services to become an alternative to hospitalization, without it there would be limited service participation for the group on orders.
Neither extended outpatient commitment alone nor community services alone accounted for the reduced inpatient day use effect in the post-period–quite the opposite. As in other studies (1), both are associated with increased inpatient utilization because such services are frequently initiated around the crises preceding an inpatient care episode and accompany the transition from hospital back to community. We believe that the use of such findings to argue against the use of extended orders fails to appreciate the role of the outpatient commitment in community care efforts.
Outpatient commitment is perhaps best conceived as a delivery mechanism rather than a treatment in and of itself. It is probably only as good as the treatment that accompanies it. Given that the alternative to hospitalization effect is accomplished through the additional use of involuntary community care in the follow-up period, it is difficult for many to identify the involuntary commitment as a success. Yet, the patients on orders are complex cases whose services needs are probably more extensive than the treatment compliant matched controls at the outset (1). Witness that prior to each hospitalization the community involvement with the patients on orders is almost twice that of the comparison group.
Our findings speak only to the use of extended 180+ day episodes of care in combination with community services offered in Victoria, Australia. They do not address demonstrable psychosocial outcomes experienced by individuals participating in such treatment regimens. The results and conclusions reported herein might be considered stronger from an evidence standpoint had they been derived from comparisons of randomly assigned groups, yet the RCT vehicle would not have offered a nine-year representation of a population’s real world experience. We did use a matched comparison design with patients acting as their own controls in the within and between group analyses. Moreover, though our findings apply only to the Australian context, it is notable that outpatient commitment has become a major issue in Western psychiatry and this study represents a report on the most extensive experience with its utilization.
This paper offers several new perspectives on outpatient commitment: It considers outpatient commitment as a delivery system. It focuses on the interaction of outpatient commitment with services provided and questions previous approaches that criticize the use of outpatient commitment on the basis of its associations with increased service utilization. In conclusion, outpatient commitment for those on extended orders in the Victorian context enables a level of community-based services provision, unexpected in the absence of this delivery system, which provides an alternative to hospitalization.
Footnotes
Presented as the keynote address at The Ninth Doris Siegel Memorial Colloquium, International Social Health Care: Policy Program and Studies, held at the Mount Sinai Medical Center, New York, NY, May 20, 2004.
Contributor Information
Steven P. Segal, Mental Health and Social Welfare Research Group, School of Social Welfare, University of California, Berkeley, Berkeley, CA 94720-7400..
Philip Burgess, The University of Queensland, Mental Health Services Research, Queensland Centre for Mental Health Research, The Park–Centre for Mental Health, Wacol, Queensland, Australia..
REFERENCES
- 1.Preston NJ, Kisely S, Xiao J: Assessing the outcome of compulsory psychiatric treatment in the community: Epidemiological study in Western Australia. British Journal of Medicine 524:1244–1246, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Torrey EF, Kaplan RJ: A national survey of the use of outpatient commitment. Psychiatric Services 46: 778–784, 1995 [DOI] [PubMed] [Google Scholar]
- 3.Swartz MS, Swanson JW, Hiday VA et al. : Can involuntary commitment reduce hospital recidivism? Findings from a randomized trial with severely mentally ill individuals. American Journal of Psychiatry 12: 1968–1974, 1999 [DOI] [PubMed] [Google Scholar]
- 4.Swartz MS, Swanson JW, Hiday VA et al. : A randomized controlled trial of outpatient civil commitment in North Carolina. Psychiatric Services 52(3): 325–329, 2001 [DOI] [PubMed] [Google Scholar]
- 5.Appelbaum P: Thinking carefully about outpatient commitment. Psychiatric Services 52(3): 347–351, 2001 [DOI] [PubMed] [Google Scholar]
- 6.Allen M, Smith VF: Opening Pandora’s Box: The practical and legal dangers of involuntary outpatient commitment. Psychiatric Services 52(3): 342–347, 2001 [DOI] [PubMed] [Google Scholar]
- 7.Torrey EF, Zdanowicz MT: Outpatient commitment: What, why, and for whom. Psychiatric Services 52(3): 337–341, 2001 [DOI] [PubMed] [Google Scholar]
- 8.Policy Research Associates Final Report: Research Study of the New York City Involuntary Outpatient Commitment Pilot Program, (at Bellevue Hospital). Policy Research Associates; (www.prainc.com/IOPT/opttoc.ht), 1998 [Google Scholar]
- 9.Steadman HJ, Gounts K, Dennis D et al. : Assessing the New York City Involuntary Outpatient Commitment Pilot Program. Psychiatric Services 52(3): 330–337, 2001 [DOI] [PubMed] [Google Scholar]
- 10.Fernandez GA, Nygard S: Impact of involuntary outpatient commitment on the revolving door syndrome in North Carolina. Hospital and Community Psychiatry 41: 1001–1004, 1990 [DOI] [PubMed] [Google Scholar]
- 11.Zanni G, deVeau L: Inpatient stays before and after outpatient commitment in Washington, DC Hospital and Community Psychiatry 37: 941–942, 1986 [DOI] [PubMed] [Google Scholar]
- 12.Munetz MR, Grande T, Kleist J et al. : The Effectiveness of Outpatient Civil Commitment. Psychiatric Services 47: 1251–1253, 1996 [DOI] [PubMed] [Google Scholar]
- 13.Rohland B: The role of outpatient commitment in the management of persons with schizophrenia. Iowa Consortium for Mental Health Services, Training, and Research, 1998 [Google Scholar]
- 14.Torrey EF, Zdanowicz MT: Study shows that long-term assisted treatment reduces violence and hospital utilization. Catalyst 2(3): 1–2, 2000 [Google Scholar]
- 15.Van Putten DA, Santiago JP, Bergen MR: Involuntary commitment in Arizona: A retrospective study. Hospital and Community Psychiatry 39:205–502, 1988 [DOI] [PubMed] [Google Scholar]
- 16.Commonwealth of Australia: National Mental Health Report 1996, Canberra, ACT: Commonwealth Department of Health and Family Services, 1998 [Google Scholar]
- 17.Commonwealth of Australia: National Mental Health Report 1997. Canberra, ACT: Commonwealth Department of Health and Family Services, 1999 [Google Scholar]
- 18.Mental Health Branch National Standards for Mental Health Services. Canberra, ACT: Commonwealth Department of Health and Family Services, 1997 [Google Scholar]
- 19.Robins L, Regeir D (Eds.): Psychiatric Disorders in America: The Epidemiological Catchment Area Study. New York: The Free Press, 1991 [Google Scholar]
- 20.Tansella M, Micciolo R, Biggeri A et al. : Episodes of care for first-ever psychiatric patients: A long term case-register evaluation in a mainly urban area. British Journal of Psychiatry 167, 220–227, 1995 [DOI] [PubMed] [Google Scholar]
- 21.SPSS for Windows, Release 11.0.1, 2001
- 22.Schinnar AP, Rothbard AB, Kanter R: Adding state counts of the severely and persistently mentally ill. Administration and Policy in Mental Health 19(1): 3–12, 1991 [Google Scholar]


