Description
A 4-year-old girl with no medical history ran into the road and collided with a car. She was knocked over and injured the back of her head. Her consciousness was clear but she vomited twice. CT scan of the head revealed a linear fracture of the occipital bone across the sinus with no intracranial haemorrhage (ICH) (figure 1). Diagnosis was a concussion and skull fracture, and she was admitted for the follow-up. Her vomiting episodes continued for two or three times per day and irritability arose after hospitalisation. Therefore, on hospital day 3, head MRI performed under sedation revealed a high signal intensity on fluid-attenuated inversion recovery (FLAIR) images in the left sigmoid sinus. No flow void was seen. Although we attempted to perform MR venography (MRV), she woke up from anaesthesia. Further anaesthetic additions were deemed risky and the examination was terminated. At this point, we could not be sure of the thrombosis based on the MRI images alone. However, her irritability persisted for 5 days after the onset, so we performed CT venography (CTV) to confirm the thrombosis. CTV revealed an area of decreased blood flow between the left lateral and sigmoid sinuses. No vascular malformation and ICH were observed. A blood test showed no signs of congenital coagulation disorders. Based on these examinations, the patient was diagnosed with cerebral venous sinus thrombosis (CVST) due to intrinsic vascular damage caused by blunt trauma.1 Because of the persistence of irritability over time after the onset, we administered anticoagulation therapy. Her irritability began improving on hospital day 8. On hospital day 32, MRV showed post-treatment symmetrical blood flow of the cerebral veins (figure 2).
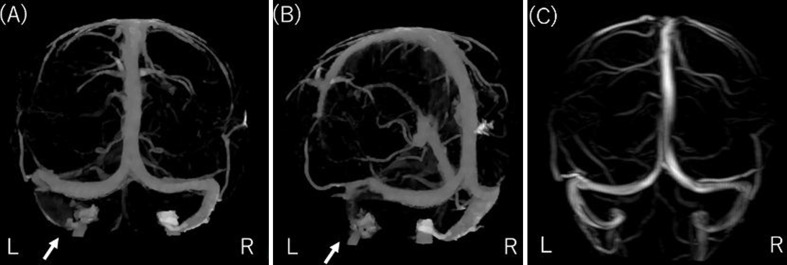
Figure 1.
Head CT on admission. The three-dimensional head CT shows occipital fracture.
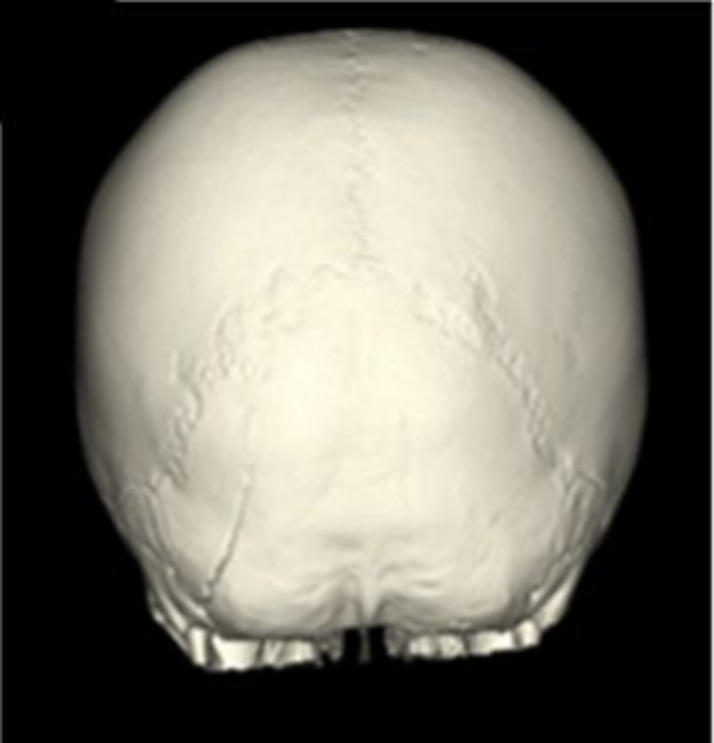
Figure 2.
CT venography on 3 days and MR venography on 32 days after trauma. (A, B) CT venography with hypovolaemia from the left sigmoid to the lateral sinuses 3 days after trauma (arrow). (C) MR venography images after completion of anticoagulation therapy showed no hypovolaemia in the cerebral venous sinus 32 days after trauma.
CVST is very rare in children, with 0.67 cases per 100 000 population.2 Approximately 3%–4% of all cases of paediatric CVST are caused by head injury.3 Clinical symptoms may vary widely, including seizures, disability, headache, vomiting and paralysis. Head CT is likely to be selected as an initial diagnostic tool for head trauma because it is rapid and widely available. The sensitivity of the simple CT scan for CVST is only 20%–43%.4 However, the presence of skull fractures across the sinus and epidural haematoma on CT scan indicates a high risk for CVST. If these findings are recognised and time permits, additional imagining examination, such as CTV and MRV, should be considered. These imaging tools are useful when making a definitive diagnosis.4 Because there are neither specific clinical features nor clear guidelines for diagnosis and of CVST, we believe it important and necessary to consider CVST when a fracture or haematoma around the sinus is observed. Extracaution must be paid to clinical symptoms after a traumatic head injury. However, the effect of anticoagulation treatment for paediatric patients remains unclear.1 In this case, we selected anticoagulation therapy because of the persistence of irritability and absence of ICH. The patient’s mental status subsequently improved and the thrombus disappeared with no complications.
Patient’s perspective.
Father: We were informed and agreed that my daughter had occipital injury, occipital fractures, and cerebral sinus thrombosis, and underwent anticoagulant therapy. We were relieved to confirm disappearance of the thrombosis and improvement in symptoms. After leaving the hospital, she was fine, but her fear of the car remains.
Learning points.
We experienced a case of cerebral venous sinus thrombosis caused by head trauma, which disappeared after anticoagulant therapy.
The differential diagnosis should include the presence of cerebral sinus thrombosis if vomiting persists after head injury.
A search for cerebral sinus thrombosis (CT venography or MR venography) is necessary if fracture or haematoma around the sinus is observed after head injury.
Acknowledgments
The authors would like to thanks Enago (www.enago.jp) for the English language review.
Footnotes
Contributors: KO wrote the manuscript. KN assisted in the preparation of the manuscript. All authors have critically reviewed the manuscript and approved the final version of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Parental/guardian consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Hersh DS, Shimony N, Groves ML, et al. Pediatric cerebral venous sinus thrombosis or compression in the setting of skull fractures from blunt head trauma. J Neurosurg Pediatr 2018;21:258–69. 10.3171/2017.9.PEDS17311 [DOI] [PubMed] [Google Scholar]
- 2.deVeber G, Andrew M, Adams C, et al. Cerebral sinovenous thrombosis in children. N Engl J Med 2001;345:417–23. 10.1056/NEJM200108093450604 [DOI] [PubMed] [Google Scholar]
- 3.Awad A-W, Bhardwaj R. Acute posttraumatic pediatric cerebral venous thrombosis: case report and review of literature. Surg Neurol Int 2014;5:53. 10.4103/2152-7806.130908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li J, Wei L, Xu B, et al. Risk factors and early diagnosis of cerebral venous sinus occlusion secondary to traumatic brain injury. Neurol India 2015;63:881–8. 10.4103/0028-3886.170067 [DOI] [PubMed] [Google Scholar]