Abstract
Study Objectives:
The 2019 coronavirus disease (COVID-19) has become a global health and economic crisis. Recent evidence from small samples suggest that it has increased mood and sleep disturbances, including insomnia, around the world. This study aimed to estimate the effect of COVID-19 on insomnia levels worldwide and in the United States during the acute phase of the pandemic.
Methods:
We analyzed search query data recorded between January 2004 and May 2020 from Google Trends and Google Keyword Planner for the search term “insomnia”.
Results:
The number of search queries for insomnia has increased over the past decade and is greater than the number of search queries for other major sleep disorders. The COVID-19 pandemic increased search queries for insomnia both worldwide and in the United States, with the number in the United States increasing by 58% during the first 5 months of 2020 compared with the same months from the previous 3 years. There is a robust diurnal pattern in insomnia search queries in the United States, with the number of queries peaking around 3 am and the overall pattern remaining stable during the pandemic.
Conclusions:
These results highlight the impact the COVID-19 pandemic has had on sleep health and the urgent need for making effective interventions accessible. Future studies will be needed to determine whether the increase in insomnia symptoms will persist and lead to higher rates of chronic insomnia in the population.
Citation:
Zitting K-M, Lammers-van der Holst HM, Yuan RK, Wang W, Quan SF, Duffy JF. Google Trends reveals increases in internet searches for insomnia during the coronavirus disease 2019 (COVID-19) global pandemic. J Clin Sleep Med. 2021;17(2):177–184.
Keywords: insomnia, COVID-19, Google Trends, sleep, sleep disorder
BRIEF SUMMARY
Current Knowledge/Study Rationale: The 2019 coronavirus disease (COVID-19) pandemic has been reported to increase mood and sleep disturbances around the world, but the magnitude of the impact is not known. We studied the effect of COVID-19 on insomnia by analyzing Google search query data for the search term “insomnia”.
Study Impact: Our study suggests that there was an increase in difficulty sleeping, both in the United States and globally, in response to the initial phase of the COVID-19 pandemic. Searches for information on insomnia showed both diurnal (peaking at 3 am) and weekly (lower on weekends) trends and overall were significantly higher in April and May 2020 than in the previous years.
INTRODUCTION
The current 2019 coronavirus disease (COVID-19) pandemic is one of the most significant global health challenges of our era, affecting most aspects of life, including sleep. Emerging evidence suggests that the pandemic has led to increases in mood and sleep disturbances in health care workers1,2 and patients undergoing cognitive behavioral therapy for insomnia,3 as well as increased risk for insomnia in the general population.4,5 Stress is considered one of the primary triggers for insomnia.6,7 Increased levels of stress from loss of a daily routine, economic uncertainty, and concerns about contracting the virus during the COVID-19 pandemic could have downstream effects on sleep, leading to insomnia.
Exposure to traumatic events such as natural disasters,8-10 terror attacks,11-15 and disease outbreaks16 have been shown to be important precipitants of acute insomnia.17 While acute insomnia is more frequently encountered in those directly exposed to traumatic events, sleep disturbances have also been observed among those indirectly exposed via mass media.11
Insomnia, defined as difficulty initiating sleep, staying asleep, or waking up too early, which is accompanied by daytime impairments/sleepiness,18 is the most common sleep disorder in the world. The prevalence of insomnia symptoms and insomnia disorder is approximately 30% and 10%, respectively, and both are most common in women, older adults, and people with medical or mental illness.19-21 While insomnia symptoms resolve without treatment in the majority of cases, a subset (∼7%) of those experiencing insomnia symptoms will go on to develop a chronic insomnia disorder,22,23 defined as having sleep issues at least 3 nights a week for at least 3 months,18 often requiring treatment.
There are a few studies that have examined insomnia during the COVID-19 pandemic. A cross-sectional, population-based survey study in Greece revealed that 38% of the participants reported insomnia, greater than the estimated prevalence before the COVID-19 pandemic, with women and people living in urban areas more susceptible to sleep difficulties.4 Zhang and colleagues2 found that 36% of medical staff reported insomnia during a COVID-19 outbreak, reporting related factors that included worry about being infected, perceived unhelpfulness of psychological support from news or social media, and extreme uncertainty regarding effective control of the COVID-19 pandemic. In a recent preliminary report, an increase in insomnia was reported among a cohort of patients with obstructive sleep apnea using positive airway pressure therapy after the COVID-19 lockdown in the United States (41% vs 48%).24
Data generated through online internet searches offer a potential source of information for monitoring insomnia in the general population. Google, along with other online search engines, is increasingly used as a source of medical and health information. With an estimated 5.5 billion searches per day,25 it thus provides an excellent platform for monitoring people’s health-seeking behaviors in the form of search queries. Prior studies have shown that the volume of online searching is strongly correlated with disease incidence.26,27 Indeed, search engine data have been successfully utilized for investigating various health conditions, including mental disorders28-30 and sleep,31-33 and to predict the spread of influenza earlier than traditional models used by the Centers for Disease Control and Prevention.34
We therefore aimed to investigate whether internet search queries for the word “insomnia” were increased during the early COVID-19 outbreak by analyzing search queries from Google Trends, a publicly available website that provides data on the frequency of Google searches over specified time ranges and by geographical region (support.google.com/trends). We also aimed to further examine whether these queries show diurnal or weekly patterns and whether there is a relationship between searches and the number of COVID-19–related deaths worldwide and in the United States.
METHODS
Data collection and analysis
Google Trends data
Google Trends (https://trends.google.com/trends/) is a publicly available web-based tool owned by Google, LLC (Mountain View, CA), that provides access to a representative random sample of all Google search requests (queries). The data are anonymized and grouped together, which allows users to analyze interest in a specific search term or topic over time and/or across geographical locations. Absolute search volume is not provided; all search query data are indexed data presented as relative popularity on a scale from 0 to 100, with each individual data point divided by the total number of searches of the selected time range and region (support.google.com/trends), and the highest value scaled to 100. If the compare function is used for comparing interest between 2 or more topics, the resulting search query numbers are normalized to all searches across the selected topics.
In order to investigate people’s interest in insomnia before and during the COVID-19 pandemic, we examined the number of search queries for the word “insomnia” and other sleep disorders from the United States as well as worldwide between 1 January 2004 (earliest date Google Trends data are available) and 31 May 2020. More specifically, we downloaded, in Universal Standard Time the following: (1) monthly search query data for the search terms “insomnia,” “sleep apnea,” “restless legs,” and “narcolepsy” from 1 January 2014 through 31 December 2019 using Google Trends’ compare function; (2) daily search query data for the search term “insomnia” between 1 January 2020 and 31 May 2020; (3) daily and weekly search query data for the search term “insomnia” between 1 January 2017 and 31 May 2020. Because the daily data from Google Trends are only available in segments of approximately 8 months, we downloaded the daily data in segments and normalized it to the weekly data (which were available for the entire period) to make it comparable across the entire time period. These data were then rescaled back to the original 0–100 scale such that the highest value became 100. For the day of the week (Sunday–Saturday) analysis, we excluded data from approximately the first week of each year in order to align the weekdays between the years and ensure that each day of the week was evenly represented across years. In addition, we downloaded the daily search query data for the search term “cancer” between 1 January 2020 and 31 May 2020 as a control for people’s medically related search habits during the acute phase of the COVID-19 pandemic.
We also downloaded the hourly and weekly search query data for the search term “insomnia” between 1 January 2017 through 31 May 2020 from each of the 50 states in the United States using the freely available pytrends script for Python (https://pypi.org/project/pytrends/). Due to a problem on the Google Trends interface, we were unable to download the hourly data between 1 and 14 March 2020 for most states. All data were converted from Universal Standard Time to local time and corrected for daylight savings time shifts. For those states that span 2 time zones, we used the time zone of the majority of the land area in the state. Because the hourly data from Google Trends are only available in 1-week segments, we normalized the hourly data to the weekly data to make it comparable across the entire time period. These data were normalized against the absolute number of search queries by month data from Google Ads Keyword Planner (Google LLC, Mountain View, CA) to calculate the number of “insomnia” search queries per hour for each state.
Google Keyword planner data
In order to investigate the changes in the absolute number of Google search queries for “insomnia,” we downloaded the monthly search query data for the keyword “insomnia” between January 2017 and May 2020 for the entire United States and for each of the 50 states from Google Keyword Planner (https://ads.google.com/intl/en_eg/home/tools/keyword-planner/) using the historical metrics function. In addition to calculating the absolute number of “insomnia” search queries per hour by combining the Google Ads Keyword Planner data with Google Trends data, we calculated the number of search queries per population of each state by dividing the number of Google search queries per state with state population estimates from the US Census Bureau (https://www.census.gov/).
COVID-19–related deaths
In order to examine the impact of COVID-19 on the number Google search queries for “insomnia,” we correlated the number of COVID-19–related deaths to the number of daily “insomnia” search queries from 1 January 2020 in the United States and worldwide. The 2 datasets for the number of daily deaths from COVID-19 in the United States and worldwide were downloaded from the freely available COVID-19 Data Repository maintained by the Center for Systems Science and Engineering at Johns Hopkins University (https://github.com/CSSEGISandData/COVID-19). Because the first recorded COVID-19–related deaths occurred on 22 January (worldwide) and 29 February (United States), all data points before these dates were deleted in the datasets used for the piecewise regression analysis. We chose to use death data rather than infection data due to the lack of accurate infection data available early in the pandemic.
All datasets were downloaded between 17 June and 9 July 2020. Only English search terms were included in the analysis. To explore the acute effects of the COVID-19 pandemic on searches for “insomnia,” we selected the time period of 1 January 2020 through 31 May 2020 (date of data freeze) to focus on and compare against the same months from the previous 3 years (2017–2019).
Statistical analyses
Statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC). We used mixed-model analysis to analyze the data and post hoc least-square-means tests to compare between groups. Logarithmic transformation was used when data were not normally distributed. Model diagnostics were performed to check the fit of the data. Piecewise mixed models were used to study the relationships between the number of “insomnia” search queries and the number of COVID-19–related deaths. Peak time for the hourly “insomnia” search queries was calculated as a circular mean across the daily maximum values for each state. In addition, a cosine curve was fitted to the nonflat part of the curve (12 hours of the 24 hours, from 8 pm to 8 am) to estimate peak phase. Briefly, Cosinor analysis fits a sinusoid to an observed time series and estimates the amplitude (magnitude of one-half of the daily variation from peak to trough) and phase (timing of the peak). We fit a model with a period of 24 hours and estimated the peak phase and tested the null hypothesis that the amplitude of the fitted curve was zero (ie, no 24-hour rhythmicity could be detected).35 The critical significance level was set at α = .05. The Bonferroni method was used to adjust for multiple comparisons where necessary and the adjusted P values are reported. Data presented in Figures 1, 2, 4A and S1 (366.9KB, pdf) are means while data presented in Figures 3 and 4B are means ± SEM.
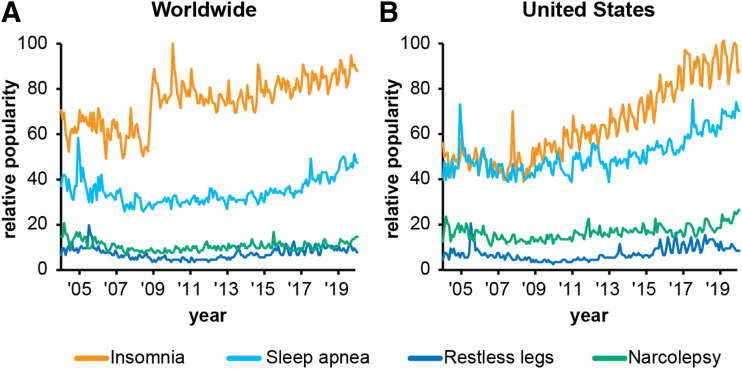
Figure 1. Google search queries for the sleep-related terms between 2004 and 2019.
Google search queries worldwide (A) and in the United States (B) for the search terms “insomnia,” “sleep apnea,” “restless legs,” and “narcolepsy” between 2004 and 2019. There were significantly more search queries for “insomnia” compared to the other 3 sleep disorders worldwide (P < .0001 for all comparisons, log-transformed data) and in the United States (P < .0001 for all comparisons, log-transformed data). There was also a significant increase in search interest for “insomnia” starting from 2009 worldwide (P < .0001 for all comparisons) and from 2011 in the United States (P = .0015 for 2004 vs 2011; P < .0001 for all other comparisons).
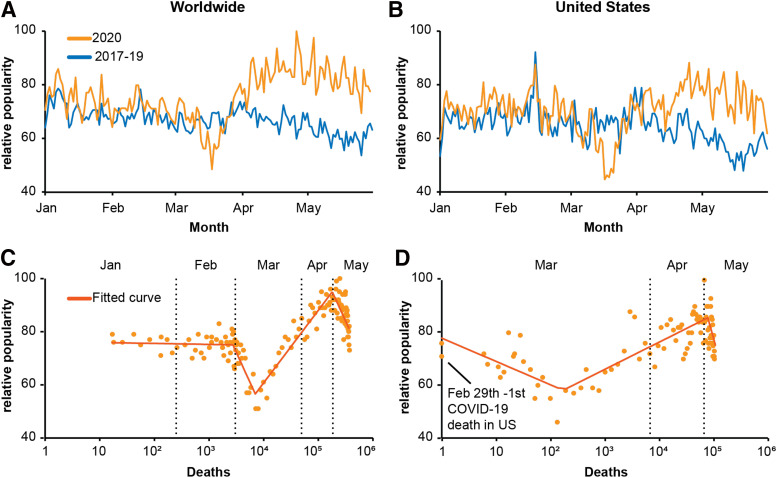
Figure 2. Search interest in insomnia and cumulative number of COVID-19 deaths.
Daily search queries for the search term “insomnia” worldwide (A) and in the United States (B) during the first 5 months (January through May 2020) of the COVID-19 pandemic compared with the same 5 months of 2017–2019. There was a significant increase in search interest for “insomnia” in April and May of 2020 compared with the same months in previous years, both worldwide (A) (P < .0001) and in the United States (B) (P < .0001). This increase in search interest for “insomnia” coincides with the increase in the cumulative number of COVID-19–related deaths (logarithmic scale) both worldwide (17 March–22 April; P < .0001) (C) and in the United States (17 March–7 May; P < .0001) (D). COVID-19 = 2019 coronavirus disease.
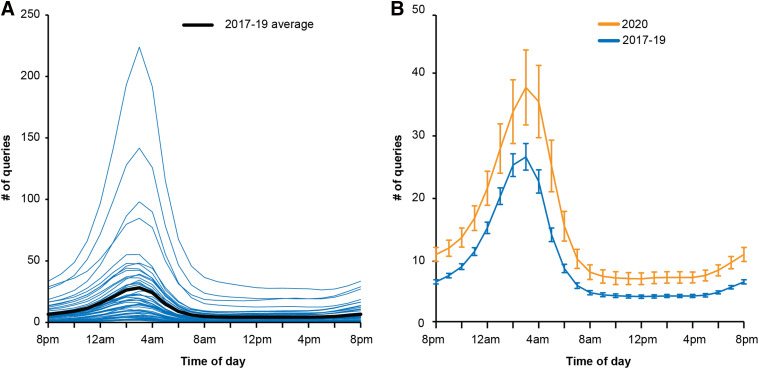
Figure 4. Diurnal pattern in Google search queries per hour.
Diurnal pattern in Google search queries per hour for the search term “insomnia” in the United States (black line) and in each of the 50 states (blue lines) (A). There was a significant diurnal pattern in the number of insomnia search queries per hour in 2017–2019 (P < 0.0001), with the greatest interest observed around 3 am. While the number of search queries per hour was significantly higher in 2020 compared with 2017–2019 (P < .0001 for all comparisons, log-transformed data), the overall pattern did not change except for a small delay in peak time in 2020 compared with 2017–2019 (3:06 am in 2017–2019 vs 3:19 am in 2020; P < .0001) (B).
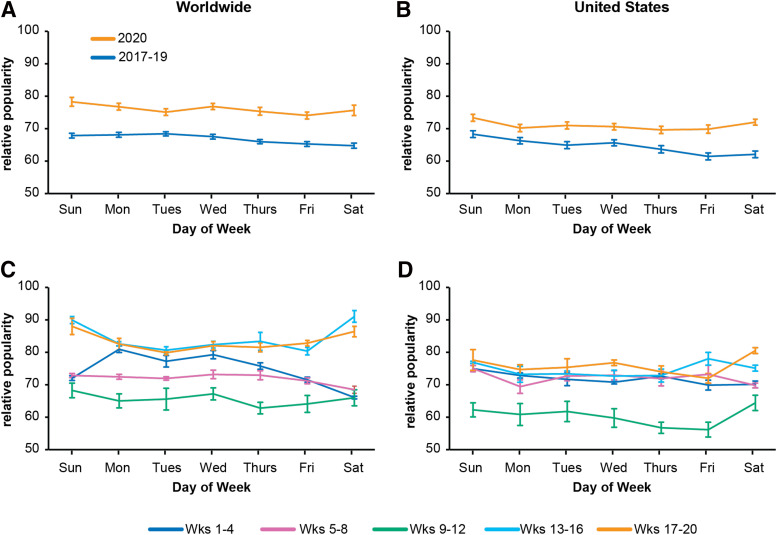
Figure 3. Daily and weekly pattern in Google search queries for the search term “insomnia” worldwide and in the United States.
There was a significant daily pattern in search interest for “insomnia” both worldwide (A) (P = .0045) and in the United States (B) (P < .0001), with the greatest interest in insomnia observed during the weekend–weekday transition on Sundays and Mondays and the least toward the weekday–weekend transition on Fridays and Saturdays. There was a significant interaction between weeks and day of the week in 2020 worldwide (C) (P = .0437), but not in the United States (D), with a greater number of “insomnia” search queries on weekdays compared with weekends in January and February (weeks 1–8) and fewer search queries on weekdays compared with weekends in April and May (weeks 13–20). Wks = weeks.
Study approval
This study used publicly available information that can be obtained without any special agreements, and it therefore does not meet the criteria for human subjects research as defined under federal regulations [45 CFR 46.102(f) of the Health and Human Services Policy for Protection of Human Research Subjects], and as confirmed via e-mail communication with the director of the Mass General Brigham (formerly Partners HealthCare) Institutional Review Board.
RESULTS
Google search queries for insomnia from 2004 until 2019
The worldwide Google Trends data showed that over the past 16 years, the number of Google search queries for “insomnia” is significantly higher relative to queries for 3 other major sleep disorders: “sleep apnea,” “restless legs syndrome,” and “narcolepsy” (Figure 1A; P < .0001 for all comparisons). Closer inspection of the “insomnia” search query data revealed that the number of queries increased significantly in 2009 compared with 2004 and remained consistently higher throughout 2010–2019 (P < .0001 for all comparisons). Data from the United States also showed that the number of “insomnia” search queries was greatest of the 4 sleep disorders over the past 16 years (Figure 1B; P < .0001 for all comparisons), with the rate of “insomnia” queries increasing significantly in 2011 compared with 2004 and staying consistently higher throughout 2012–2019 (P = .0015 for 2004 vs 2011; P < .0001 for all other comparisons). Although less dramatic, similar trends worldwide and in the United States were observed for sleep apnea.
Impact of COVID-19 pandemic on Google search queries for insomnia
The relative popularity of “insomnia” search queries over the first 5 months (January through May) of 2020 was significantly greater compared with the number of queries over the same months from 2017, 2018, and 2019 both worldwide (Figure 2A; P < .0001 for all comparisons) and the United States (Figure 2B; P < .0001 for all comparisons) where the absolute number of search queries for “insomnia” increased by 58% in January through May 2020 compared with the same months from 2017 to 2019 (2019: 1.76 vs 2.77 million; Table S1 (366.9KB, pdf) in the supplemental material).
Closer inspection revealed that, while the number of “insomnia” queries decreased worldwide from January through May in 2017, 2018, and 2019 (P < .0001 for all January vs May comparisons) and in the first quarter of 2020 (P < .0001 for January vs March 2020), there was a significant increase in the number of queries in April and May compared with January in 2020 (P < .0001 for both comparisons). Similar to the worldwide data, there was a significant decrease in “insomnia” search queries in the United States from January through May in 2017, 2018, and 2019 (P < .0001 for all January vs May comparisons), and in the first quarter of 2020 (P < .0001 January vs March 2020), but no significant difference in April or May 2020 compared with January 2020.
Month-by-month comparison of “insomnia” search queries in 2020 worldwide and in the United States revealed no change from January to February, a significant decrease from February to March (P = .0075 worldwide; P < .0001 in the United States), a significant increase from March to April (P < .0001 worldwide and in the United States), and no change from April to May. In contrast, there was a decrease in the number of Google queries for the search term “cancer” in March 2020 (Figure S1 (366.9KB, pdf) in the supplemental material), suggesting that the significant increase in searches for “insomnia” in March was not simply due to an increase in searches for medical information during the acute phase of the pandemic.
Relationship between Google search queries for insomnia and the number of COVID-19–related deaths
As shown in Figure 2C and 2D, while there was no association between search queries for “insomnia” and the cumulative number of COVID-19 deaths in January or February 2020, there was a significant positive relationship between the number of “insomnia” search queries and the cumulative number of COVID-19–related deaths (logarithmic scale) in March, April, and May both worldwide (17 March–22 April; P < .0001) and in the United States (17 March–7 May; P < .0001).
Impact of COVID-19 pandemic on daily and weekly patterns of Google search queries for insomnia
In addition to varying from year to year, the number of “insomnia” search queries worldwide varies significantly among days of the week when comparing across the first 5 months of each year, although the variation is relatively small (Figure 3A; P = .0045). Closer inspection of the pattern revealed that the greatest number of search queries for “insomnia” occurred on Sundays and Mondays during the weekend-to-work-week transition, and the fewest on Fridays and Saturdays during the work-week-to-weekend transition. A similar pattern in “insomnia” search queries among days of the week was observed in the United States (Figure 3B; P < .0001), with the greatest number of search queries occurring on Sundays and Mondays and the fewest on Fridays and Saturdays.
Although there was no significant interaction between year and day of the week either worldwide or in the United States, the data from 2020 revealed a significant interaction between weeks and day of the week worldwide (Figure 3C; P = .0437), with weekends having fewer numbers of insomnia search queries compared with weekdays during the earlier weeks of the year (weeks 1–4 and 5–8, in January and February) and a greater number of insomnia search queries than weekdays during the later weeks (weeks 13–16 and 17–20, in April–May). There was no significant interaction between weeks and day of the week in the United States (Figure 3D).
Impact of COVID-19 pandemic on diurnal patterns of Google search queries for insomnia
There was a significant diurnal (hourly) variation in the number of Google search queries for “insomnia” in the United States in the years 2017–2019 (Figure 4A; P < .0001, averaged across all states). The number of “insomnia” queries increased in the evening, reaching its peak around 3 am in each of the 50 states (Table S1 (366.9KB, pdf) ) and then decreased toward the morning, reaching the lowest level in the late the afternoon/early evening. The fitted mean amplitude and peak phase across all states were 22.5 queries/hour and 306.4° (which corresponds to 2:25 am where 0° corresponds to 6:00 am), respectively. The number of insomnia search queries varied by state, with larger states having a higher number of queries per hour, although the differences largely disappeared after adjusting for population size (Table S1 (366.9KB, pdf) ), and there was a significant random variability in the peak phase (P < .0001), suggesting that the states peak at slightly different times (Figure 4A and Table S1 (366.9KB, pdf) ).
While there were more search queries for “insomnia” in January through May in 2020 compared with the same months in 2017–2019 (P < .0001 for all comparisons), the diurnal pattern did not change except for a small delay in peak time which shifted by approximately 10 minutes from 3:06 am in 2017–2019 to 3:19 am in 2020 (Figure 4B; P < 0.0001), suggesting that the increase in “insomnia” search queries during 2020 was due to an increase in interest in insomnia during the COVID-19 pandemic, possibly reflecting increased levels of insomnia in the population.
DISCUSSION
Overall, the COVID-19 outbreak corresponded with an increase in the number of “insomnia” search queries via Google, and those searches were associated with the number of COVID-19–related deaths both worldwide and in the United States. The number of Google search queries for “insomnia” has increased over the last decade and is higher compared with other sleep disorders, with “insomnia” search queries showing a distinct diurnal and weekly pattern.
Similar to a previous report,33 we found an increase in the number of Google search queries for “insomnia” over the past decade both worldwide and in the United States. While it is unlikely that everyone who searches for information about “insomnia” has insomnia symptoms, the increased interest in insomnia (>4.3 million search queries per year in the United States in 2017–2019) parallels findings of its growing prevalence in the general population.36 A similar pattern was observed for sleep apnea, which also likely reflects its increasing prevalence fueled by the obesity epidemic. However, both conditions are linked in that insomnia symptoms are frequently observed in those with sleep apnea,37 and therefore the increase in insomnia search queries may be partially explained by concomitant searches for sleep apnea.
The COVID-19 outbreak led to a significant increase in the number of “insomnia” search queries between April and May 2020 both worldwide and in the United States, suggesting it may have been a consequence of the pandemic’s negative impact on mental health and well-being on a global scale. This increase in the number of “insomnia” search queries is in accordance with recent findings of increased insomnia symptoms among health care workers and others during the pandemic,1-4,24 with 71% of surveyed health care workers at a New York Hospital reporting insomnia symptoms following the COVID-19 surge.38 The global scale of the increase in “insomnia” search queries in the early months of the pandemic suggests that an increase in insomnia symptoms is not limited to those directly exposed to the health or economic impacts of the pandemic, but that the pandemic has also impacted many people indirectly via exposure to mass media. In fact, there was a significant association both worldwide and in the United States between the increase in the number of Google search queries for “insomnia” and the increase in the number of COVID-19–related deaths, suggesting that the constant media coverage of the pandemic may have heightened anxiety and stress among the general population, contributing to an increase in insomnia symptoms 11.
Interestingly, before the large increase in insomnia search queries in April and May 2020 there was a temporary decrease in the number of search queries for “insomnia” in March both worldwide and in the United States. This coincided with an increase in the number of COVID-19–related search queries and a decrease in the number of many common health-related search queries such as “cancer.” The decrease in the number of “insomnia” search queries in March 2020 may reflect a temporary change in people’s information-seeking behavior during the early phase of the pandemic when the scope and seriousness of COVID-19 first became apparent outside of China, and during which the number of infections and deaths started increasing worldwide.
The weekly pattern in “insomnia” search queries was relatively stable from 2017 to 2019, with an increase in the number of search queries for “insomnia” early in the week and a decrease toward the weekend. This may reflect that individuals are more concerned about their (lack of) sleep during weekdays when they are more likely to have to awaken at a specific time for work or school, as opposed to the weekend when many individuals have days off from work or school.39 However, our results suggest that, during the early phase of the pandemic (April–May 2020) when the COVID-19–related stay-at-home restrictions were first implemented in many countries and parts of the United States, this daily search pattern was altered such that the greatest number of “insomnia” search queries occurred toward the end of the week and over the weekend. This may reflect worsening problems with sleep as the work week progressed.
In contrast, while COVID-19 increased the absolute number of search queries for “insomnia,” it did not change the diurnal pattern in “insomnia” search queries in the United States other than delaying the peak time by approximately 10 minutes. Each of the 50 states showed a similar increase in search interest for “insomnia” during the early hours of the night, with the number peaking around 3 am, a time of the night that many patients with insomnia would likely be awake. This diurnal pattern in “insomnia” search queries and the nocturnal peak in search interest support an interpretation that these “insomnia” search queries are predominantly from people who are experiencing insomnia symptoms and who are therefore seeking information about insomnia. Moreover, the differences in the peak timing in “insomnia” search queries between the 50 states were relatively small, suggesting that this diurnal pattern is very robust.
Limitations
There may be a number of reasons why a given internet search term such as “insomnia” is popular, so our results must be interpreted with caution. However, the robust diurnal and weekly patterns in “insomnia” search queries, together with the increase in insomnia symptoms during the COVID-19 pandemic reported in other studies, suggest that the increase in “insomnia” search queries in the spring of 2020 likely reflects an increase in insomnia levels/symptoms in the general population. The search queries may be biased toward younger people, who are more digitally connected than older individuals, although data from the Pew Research Center on internet use by age in the United States suggest that the gap between young and older people has decreased, with 73% of those older than 65 using the internet as compared with 100% of those between ages 18 and 29 in 2019 (https://www.pewresearch.org/internet/chart/internet-use-by-age/). Finally, exclusion of non-English search terms may limit the generalizability of the results in countries where English is not a major language and the Google Trends data were only available from countries where Google is the dominant search engine, which excludes some countries such as China.
In summary, our study showed that online search query data can provide informative data on the sleep-related health-seeking behaviors of the population worldwide and, together with results from other studies, also suggested an increase in sleep disturbances with COVID-19, highlighting the scope and magnitude of the impact the COVID-19 pandemic has had on sleep health. Follow-up studies will be needed to determine whether the increase in insomnia searches is associated with increases in diagnoses of insomnia, prescription or over-the-counter medication sales, and/or use of behavioral treatments for insomnia (including sleep apps). These data also highlight the need for easily accessible, quality information about healthy sleep and sleep disorders.
DISCLOSURE STATEMENT
All authors have seen and approved the manuscript. K.-M.Z. was supported in part by P01 AG009975 and awards from the American Academy of Sleep Medicine Foundation, the President and Fellows of Harvard College, and the William F. Milton Fund of Harvard University. H.M.L.-v.d.H. was supported by National Institutes of Health (NIH) grant R01 AG044416. R.K.Y. was supported by National Institutes of Health (NIH) grant F32 HL143893. J.F.D. and W.W. were supported in part by National Institutes of Health (NIH) grants P01 AG09975 and R01 AG044416. K.M.Z.’s spouse works at Google but did not participate in the writing of this paper. S.F.Q. is a consultant for Jazz Pharmaceuticals, Whispersom, and Best Doctors. He is also the Chair of the Scoring Manual Committee and a member of the Hypopnea Taskforce for the American Academy of Sleep Medicine and receives grant funding from the NIH. The other authors report no conflicts of interest.
SUPPLEMENTARY MATERIAL
ACKNOWLEDGMENTS
The authors thank Mr. John Wise for assistance with the references. Author contributions: K.-M.Z. developed the research question and downloaded the data. K.-M.Z., H.M.L.-v.d.H., R.K.Y., and J.F.D. designed the study and analyzed the data. R.K.Y. prepared the figures and table. K.-M.Z. and W.W. conducted the statistical analyses. All authors wrote and reviewed the final version of the paper.
ABBREVIATION
- COVID-19
2019 coronavirus disease
REFERENCES
- 1.Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–907. 10.1016/j.bbi.2020.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang C, Yang L, Liu S, et al. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front Psychiatry. 2020;11:306. 10.3389/fpsyt.2020.00306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Simpson N, Manber R. Treating insomnia during the COVID-19 pandemic: observations and perspectives from a behavioral sleep medicine clinic. Behav Sleep Med. 2020;18(4):573–575. 10.1080/15402002.2020.1765781 [DOI] [PubMed] [Google Scholar]
- 4.Voitsidis P, Gliatas I, Bairachtari V, et al. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Res. 2020;289:113076. 10.1016/j.psychres.2020.113076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Casagrande M, Favieri F, Tambelli R, Forte G. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020;75:12–20. 10.1016/j.sleep.2020.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morin CM, Rodrigue S, Ivers H. Role of stress, arousal, and coping skills in primary insomnia. Psychosom Med. 2003;65(2):259–267. 10.1097/01.PSY.0000030391.09558.A3 [DOI] [PubMed] [Google Scholar]
- 7.Åkerstedt T. Psychosocial stress and impaired sleep. Scand J Work Environ Health. 2006;32(6):493–501. 10.5271/sjweh.1054 [DOI] [PubMed] [Google Scholar]
- 8.Varela E, Koustouki V, Davos CH, Eleni K. Psychological consequences among adults following the 1999 earthquake in Athens, Greece. Disasters. 2008;32(2):280–291. 10.1111/j.1467-7717.2008.01039.x [DOI] [PubMed] [Google Scholar]
- 9.Bayleyegn T, Wolkin A, Oberst K, et al. Rapid assessment of the needs and health status in Santa Rosa and Escambia counties, Florida, after Hurricane Ivan, September 2004. Disaster Manag Response. 2006;4(1):12–18. 10.1016/j.dmr.2005.10.001 [DOI] [PubMed] [Google Scholar]
- 10.Li X, Buxton OM, Hikichi H, et al. Predictors of persistent sleep problems among older disaster survivors: a natural experiment from the 2011 Great East Japan earthquake and tsunami. Sleep. 2018;41(7):zsy084. 10.1093/sleep/zsy084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goodwin R, Lemola S, Ben-Ezra M. Media use and insomnia after terror attacks in France. J Psychiatr Res. 2018;98:47–50. 10.1016/j.jpsychires.2017.12.006 [DOI] [PubMed] [Google Scholar]
- 12.Galea S, Ahern J, Resnick H, et al. Psychological sequelae of the September 11 terrorist attacks in New York City. N Engl J Med. 2002;346(13):982–987. 10.1056/NEJMsa013404 [DOI] [PubMed] [Google Scholar]
- 13.Schlenger WE, Caddell JM, Ebert L, et al. Psychological reactions to terrorist attacks: findings from the National Study of Americans’ Reactions to September 11. JAMA. 2002;288(5):581–588. 10.1001/jama.288.5.581 [DOI] [PubMed] [Google Scholar]
- 14.Pandya A. A review and retrospective analysis of mental health services provided after the September 11 attacks. Can J Psychiatry. 2013;58(3):128–134. 10.1177/070674371305800302 [DOI] [PubMed] [Google Scholar]
- 15.DiGrande L, Neria Y, Brackbill RM, Pulliam P, Galea S. Long-term posttraumatic stress symptoms among 3,271 civilian survivors of the September 11, 2001, terrorist attacks on the World Trade Center. Am J Epidemiol. 2011;173(3):271–281. 10.1093/aje/kwq372 [DOI] [PubMed] [Google Scholar]
- 16.Tsang HW, Scudds RJ, Chan EY. Psychosocial impact of SARS. Emerg Infect Dis. 2004;10(7):1326–1327. 10.3201/eid1007.040090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sinha SS. Trauma-induced insomnia: a novel model for trauma and sleep research. Sleep Med Rev. 2016;25:74–83. 10.1016/j.smrv.2015.01.008 [DOI] [PubMed] [Google Scholar]
- 18.American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014. [Google Scholar]
- 19.Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Rössler W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep. 2008;31(4):473–480. 10.1093/sleep/31.4.473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Taylor DJ, Mallory LJ, Lichstein KL, Durrence HH, Riedel BW, Bush AJ. Comorbidity of chronic insomnia with medical problems. Sleep. 2007;30(2):213–218. 10.1093/sleep/30.2.213 [DOI] [PubMed] [Google Scholar]
- 21.Roth T. Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med. 2007;3(5, Suppl):S7–S10. 10.5664/jcsm.26929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perlis ML, Vargas I, Ellis JG, et al. The natural history of insomnia: the incidence of acute insomnia and subsequent progression to chronic insomnia or recovery in good sleeper subjects. Sleep. 2020;43(6):zsz299. 10.1093/sleep/zsz299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.LeBlanc M, Mérette C, Savard J, Ivers H, Baillargeon L, Morin CM. Incidence and risk factors of insomnia in a population-based sample. Sleep. 2009;32(8):1027–1037. 10.1093/sleep/32.8.1027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Batool-Anwar S, Omobomi OS, Quan SF. Impact of the novel coronavirus disease on treatment adherence and sleep duration in patients with obstructive sleep apnea treated with positive airway pressure. J Clin Sleep Med. 2020;16(11):1917–1920. 10.5664/jcsm.8746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sullivan D. Google now handles at least 2 trillion searches per year. 2016. https://searchengineland.com/google-now-handles-2-999-trillion-searches-per-year-250247. Accessed July 1, 2020.
- 26.Teng Y, Bi D, Xie G, et al. Dynamic forecasting of Zika epidemics using Google Trends. PLoS One. 2017;12(1):e0165085. 10.1371/journal.pone.0165085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kapitány-Fövény M, Ferenci T, Sulyok Z, et al. Can Google Trends data improve forecasting of Lyme disease incidence? Zoonoses Public Health. 2019;66(1):101–107. 10.1111/zph.12539 [DOI] [PubMed] [Google Scholar]
- 28.Jun S-P, Yoo HS, Choi S. Ten years of research change using Google Trends: from the perspective of big data utilizations and applications. Technol Forecast Soc Change. 2018;130:69–87. 10.1016/j.techfore.2017.11.009 [DOI] [Google Scholar]
- 29.Mavragani A, Ochoa G, Tsagarakis KP. Assessing the methods, tools, and statistical approaches in Google Trends research: systematic review. J Med Internet Res. 2018;20(11):e270. 10.2196/jmir.9366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ayers JW, Althouse BM, Allem JP, Rosenquist JN, Ford DE. Seasonality in seeking mental health information on Google. Am J Prev Med. 2013;44(5):520–525. 10.1016/j.amepre.2013.01.012 [DOI] [PubMed] [Google Scholar]
- 31.Ingram DG, Plante DT. Seasonal trends in restless legs symptomatology: evidence from Internet search query data. Sleep Med. 2013;14(12):1364–1368. 10.1016/j.sleep.2013.06.016 [DOI] [PubMed] [Google Scholar]
- 32.Ingram DG, Matthews CK, Plante DT. Seasonal trends in sleep-disordered breathing: evidence from Internet search engine query data. Sleep Breath. 2015;19(1):79–84. 10.1007/s11325-014-0965-1 [DOI] [PubMed] [Google Scholar]
- 33.Ji K-H, Kang M-R. Trends of public interest in sleep disorders: looking by internet searching volume. Sleep Med Res. 2017;8(2):62–67. 10.17241/smr.2017.00101 [DOI] [Google Scholar]
- 34.Ginsberg J, Mohebbi MH, Patel RS, Brammer L, Smolinski MS, Brilliant L. Detecting influenza epidemics using search engine query data. Nature. 2009;457(7232):1012–1014. 10.1038/nature07634 [DOI] [PubMed] [Google Scholar]
- 35.Zitting KM, Vujovic N, Yuan RK, et al. Human resting energy expenditure varies with circadian phase. Curr Biol. 2018;28(22):3685–3690, e3. 10.1016/j.cub.2018.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hisler GC, Muranovic D, Krizan Z. Changes in sleep difficulties among the U.S. population from 2013 to 2017: results from the National Health Interview Survey. Sleep Health. 2019;5(6):615–620. 10.1016/j.sleh.2019.08.008 [DOI] [PubMed] [Google Scholar]
- 37.Zhang Y, Ren R, Lei F, et al. Worldwide and regional prevalence rates of co-occurrence of insomnia and insomnia symptoms with obstructive sleep apnea: a systematic review and meta-analysis. Sleep Med Rev. 2019;45:1–17. 10.1016/j.smrv.2019.01.004 [DOI] [PubMed] [Google Scholar]
- 38.Shechter A, Diaz F, Moise N, et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen Hosp Psychiatry. 2020;66:1–8. 10.1016/j.genhosppsych.2020.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schlotz W, Hellhammer J, Schulz P, Stone AA. Perceived work overload and chronic worrying predict weekend-weekday differences in the cortisol awakening response. Psychosom Med. 2004;66(2):207–214. 10.1097/01.psy.0000116715.78238.56 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.