Abstract
It is important that population-based cancer registries provide accurate and reliable data for public health purposes. These data are essential data for planning of cancer control and prevention. In this study, we examined cancer incidence rates (year 2005–2010) in four MECC registries (Cyprus, Jordan, Israel, Izmir (Turkey)) and compared with the rates in the US. The overall age-standardized incidence rates for males were highest in the US followed by Israeli Jews, Izmir (Turkey), Cyprus, Israeli Arabs, and lowest in Jordan. In women the rates of cancer of all sites were also highest in US women followed by Israeli Jews, Cyprus, Israeli Arabs, Izmir (Turkey), and lowest in Jordan. It is of interest that although site-specific cancer rates differ between the countries studied, prostate, lung and colorectal cancers are within the five most common cancers males in all countries studied. In females, breast colorectal and endometrium cancers are three of the five most common cancers in females in all countries studied. The results presented in this paper can have implications for opportunities in cancer control and prevention in these countries. Future studies on individual cancer sites with highest rates in these Countries are currently underway.
Keywords: Population-based cancer registries, Middle East, SEER, Cancer burden, Cancer risk
1. Introduction
Cancer is one of the leading chronic diseases in the world with an estimated 14.1 million new cases and 8.2 million cancer deaths in 2012 [1]. Almost 60% of these new cases and 65% of the deaths occurred in developing and low to middle income countries [1,2]. Because of this growing burden, identifying sources of accurate population-based cancer incidence data in developing Countries is an immediate public health priority to inform local policy around cancer control and prevention, to provide a way to monitor success, and to provide data for international comparison.
The Middle East Cancer Consortium (MECC) was established in 1996 through an agreement of the Ministries of Health of Cyprus, Egypt, Israel, Jordan, and the Palestinian Authority. Turkey joined the consortium in 2004. MECC was supported by the US government through the National Cancer Institute (NCI) and collaborations with the University of California Irvine, Emory University and International Agency for Research on Cancer (IARC). The establishment of population-based cancer registries and reliable data collection in MECC registries was guided by the Manual of Standards for Cancer Registration which was created for the purpose [3]. The primary goal of MECC was to enhance local infrastructure to support cancer control activities in the region and raise cancer awareness in the Middle East through regional cooperation. Its first main project was the establishment of new, or enhancement of existing population-based cancer registries in the consortium member countries [4].
Cancer incidence data from four MECC countries (Cyprus, Jordan, Israel and Izmir (Turkey)) from 2005 to 2010 are included in this paper. The main objectives include: a) examining the consistency of the incidence rates over a six year period for each of the 4 MECC Countries to assess validity; b) comparing cancer rates between populations in the Middle East using unified methods for data collection, quality control and statistical analysis; and c) comparing these rates to US Surveillance, Epidemiology and End Results (SEER) Program cancer rates and identifying the most common cancers in this geographic area compared to the U.S.
2. Materials and methods
2.1. Participating population-based cancer registries
Central to MECC’s early foundation was the development of standardized operating procedures for the registries as well as a standard set of data elements and coding definitions that would be used by all MECC registries. Standardization of both processes and data elements was deemed critical so that consistent quality measures could be applied to the data and reliable comparisons across countries could be made. In addition training program to educate cancer data collectors within the coverage areas of the respective registries, audits and other program evaluation tools were used to assess the level of completeness and accuracy of the data. The data presented here include cancer incidence over the period 2005–2010, drawn from data collected by four MECC registries with comparisons to data from SEER program for the corresponding period. The following are brief descriptions of the four registries included in this analysis.
Cyprus Cancer Registry (CyCR): CyCR is a national population-based registry, started functioning under the MECC structure in May 1998. CyCR covers the population resident in the government controlled Republic of Cyprus. The Registry also includes non-residents who are treated for cancer at facilities operating in the government controlled areas. The population reside in the area is about 800,000. CyCR covers approximately 92–95% of all cancer cases.
Jordan Cancer Registry (JCR): JCR is a national, population–based registry founded as an operational reporting system in the Ministry of Health in collaboration with MECC in 1996. JCR covers the entire kingdom, including all resident population groups and nationalities, for a total population estimated at nearly 9 million. Cancer cases are identified through a combination of passive methods (wherein providers complete notification forms and forward them to the JCR), and active case finding and data collection on the part of the registry.
Izmir (Turkey) Cancer Registry (ICR): Izmir is a province in the western region of Anatolia, at the western part of Turkey. Its area is 11,973 km2 and it is one of Turkey’s most densely populated areas with 4.1 million inhabitants, of which 91.4% live in urban areas. The ICR was established in 1992 and joined MECC in 2004. ICR became the IARC Regional Hub for North Africa, West and Central Asia in October 2013. ICR collects information for all cancer cases arising in the Izmir Province, following the international standards for cancer registration during all processes. The estimated completeness of case registration is higher than 97%.
Israel National Cancer Registry (INCR): INCR is a population-based registry established in 1960. The registry covers the entire Israeli population, which numbers approximately 8 million (75% Jewish, 21% Arab, 4% other). Since 1982, hospitals, pathology and cytology laboratories, and other health care providers have been required by law to submit reports of covered diseases to the registry. The registry currently includes information on about 700,000 cases, with about 30,000 new cases being added to the registry every year. Completeness of the registry for solid tumors has been estimated at 93%. Israeli cancer incidence was calculated separately for the Jewish and Arab populations to allow for comparison of cancer rates in the two groups, as well as to allow for comparison of cancer rates between Israeli Arabs and Arab populations in the other three participating countries.
US SEER (SEER18): The National Cancer Institute SEER Program of the United States contains approximately 97% of all incident cancer cases from 18 registries that cover approximately 28% of the US population [6]. This represents over 86 million individuals. The SEER Program started in 1973 following the National Cancer Act of 1971 and has expanded over time as the US population has expanded. The population covered by SEER is generally representative of the overall US population.
Data quality in MECC registries has been maintained over the years through regular assessment and quality control measures implemented by the steering committee of MECC. The MECC steering committee is comprised of representatives from the NCI, the participating cancer registries, the Department of Epidemiology of the University of California at Irvine, and IARC. The steering committee conducts external audits and site visits of each registry to assure consistency and quality. The four registries participating in this paper have all been routinely audited and have shown rates of coverage ranging from 92% to 97%.
2.2. Data collection
The collection of data by MECC registries is guided by the MECC Manual of Coding and Staging [5]. We used a novel method to generate and combine data from the four registries for this paper. Specifically, a common data dictionary was developed and the data were assessed for quality using standard statistical approaches that included checking for appropriate coding values, reviewing ranges for each variable, and testing for outliers. In order to ensure confidentiality of the individual patient data, raw data remained at each of the MECC registries and statistical analysis code was developed at UC Irvine to be run across the four registry datasets to produce analytic tables ensuring consistent statistical methods and software. This approach could serve as a model for research projects involving multiple countries and registries looking to combine their data for analysis without merging individual data files.
2.3. Data variables
For the purpose of this study, only invasive cancer diagnosed between 2005 and 2010 was included (ICD-O-3 behavior code = 3) with the exception of in situ urinary bladder cancer, which was considered for the calculation of bladder cancer estimates. Basal and squamous cell carcinoma of the skin are not reportable diseases for MECC registries and were excluded from analysis. Aggregate figures for incident cancer cases, grouped by cancer site, age group, gender, and year were reported by the registries. Age group, gender, also provided population data and year to allow for the calculation of age standardized incidence rates (ASIR). All MECC countries follow the rules suggested by the International Association of Cancer Registries (IACR) for multiple primary tumors [7]. The SEER Program follows slightly different rules that generally result in counting more primaries. For example, SEER rules consider each segment of the colon and rectum a separate primary site, each breast a separate organ/primary site and each skin site a separate primary site. In order to assure comparable analyses between MECC and SEER data, we applied the IACR rules to the SEER data.
2.4. Statistical analysis
Age-standardized incidence rates (ASR) and their 95% confidence intervals were calculated using direct standardization with the WHO 2000–2025 World standard population for all cancer sites combined and commonly occurring cancer sites [8]. Age-specific cancer incidence rates were also calculated for each country along with cancer site specific distributions and ASR ratios by gender. All rate calculations and statistical analyses were conducted using SAS and SAS/STAT Version 9.2 (SAS Institute, Cary, NC, USA).
3. Results
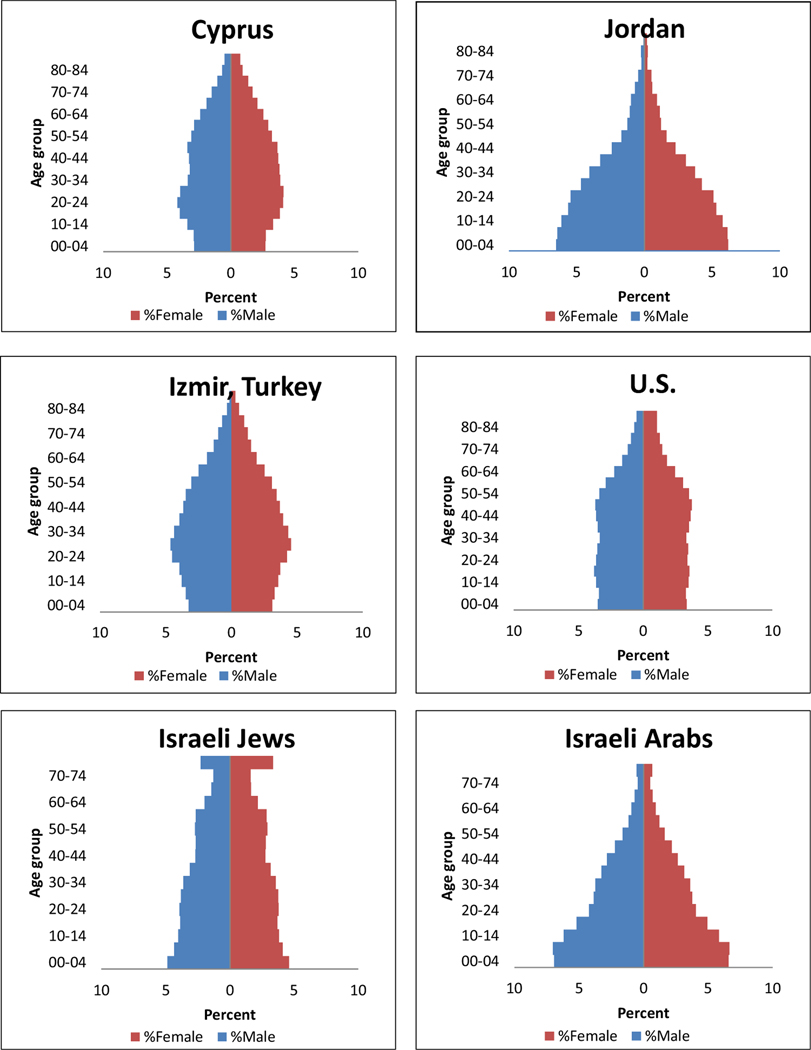
Fig. 1 shows population pyramids by age and gender for each registry. The populations were older among US SEER, Israeli Jews, Cyprus and Izmir to lesser extent and younger among Israeli Arabs and Jordanians. Because of the differences in the population distributions by age comparisons in the cancer experience between the Countries under study use age-standardized and age-specific rates. Table 1A presents the age-standardized incidence rates for all cancer sites combined in males for each country over the study period. As can be seen, the rates are fairly stable over the six year period for each country. Cyprus, Izmir and Israel have higher overall rates, ranging from 276 to 340 per 100,000 in males and 196–307 per 100,000 in females, while Jordan shows consistently lower rates (131/100,000 in males and 137/100,000 in females). Among males, the ASR of all cancers was highest in the US followed by Israeli Jews and Izmir. Similar results were also observed among females (Table 1B) with US women having the highest incidence rate, followed by Israeli Jews and Cyprus.
Fig.1.
Population pyramids, 2005–2010 (Israel population data have combined age 75+).
Table 1.
Age-standardized incidence ratesa (per 100,000) for all cancers for each country by gender, 2005–2010 (For interpretation of the references to colour in this Table, the reader is referred to the web version of this article.).
| Table 1A: Age-standardized Incidence rates (2005–2010, 95%CI) of all cancers in Males (per 100,000) by each country/registry. | ||
|---|---|---|
| Cyprus | 283 (277, 289) | 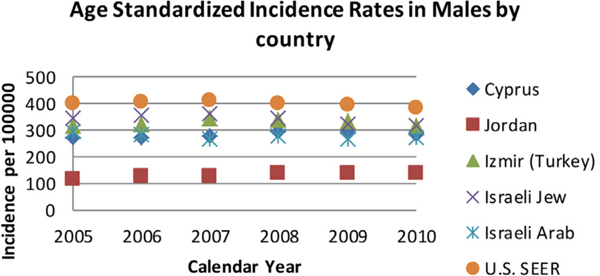 |
| Jordan | 131(129, 134) | |
| Izmir (Turkey) | 329 (326, 333) | |
| Israeli Jew | 340 (338, 343) | |
| Israeli Arab | 276(269, 283) | |
| U.S. SEER | 402 (401, 403) | |
| Table 1B: Age-standardized Incidence rates (2005–2010, 95%CI) of all cancers in Females (per 100,000) by each country/registry. | ||
|---|---|---|
| Cyprus | 244(239, 249) | 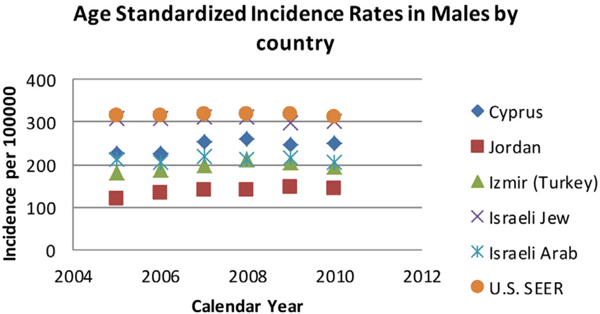 |
| Jordan | 137(135, 140) | |
| Izmir (Turkey) | 196(194, 199) | |
| Israeli Jew | 307 (305, 309) | |
| Israeli Arab | 211(205, 217) | |
| U.S. SEER | 318(317,318) | |
Direct standardization using the WHO 2000–2025 World standard population [8].
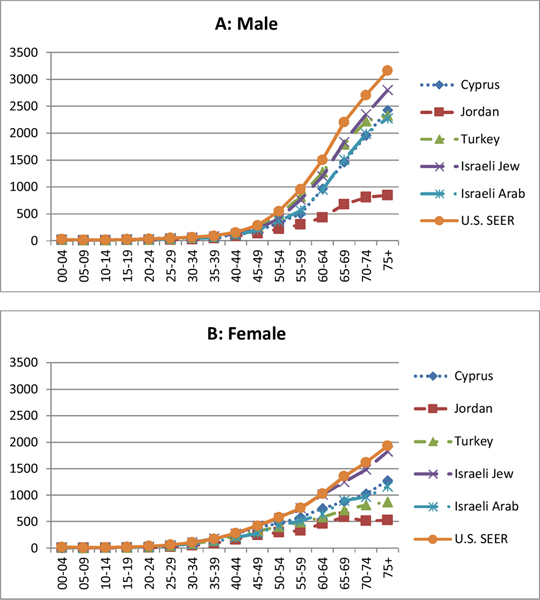
Figs. 2A and B present the age-specific rates per 100,000 for cancer of all sites in males and females respectively. In males, age-specific rates in different populations differ after age 40, with Jordan continues to have the lowest rates in all age groups. The rate of increase by age is variable between Countries. Cyprus, Izmir and Israel males have similar age-specific rates and the rates, while the SEER rates are highest. The comparison of female rates among registries appears to have similar patterns as in males. In both gender, the age-specific rates for SEER and Israeli Jews share the most similarity and are almost identical in females. Jordan, Israeli Arabs and Izmir show delay in rising of the rates by age, with Jordan showing the slowest rise.
Fig. 2.
Age-specific incidence rate (per 100,000) of all cancer sites by gender.
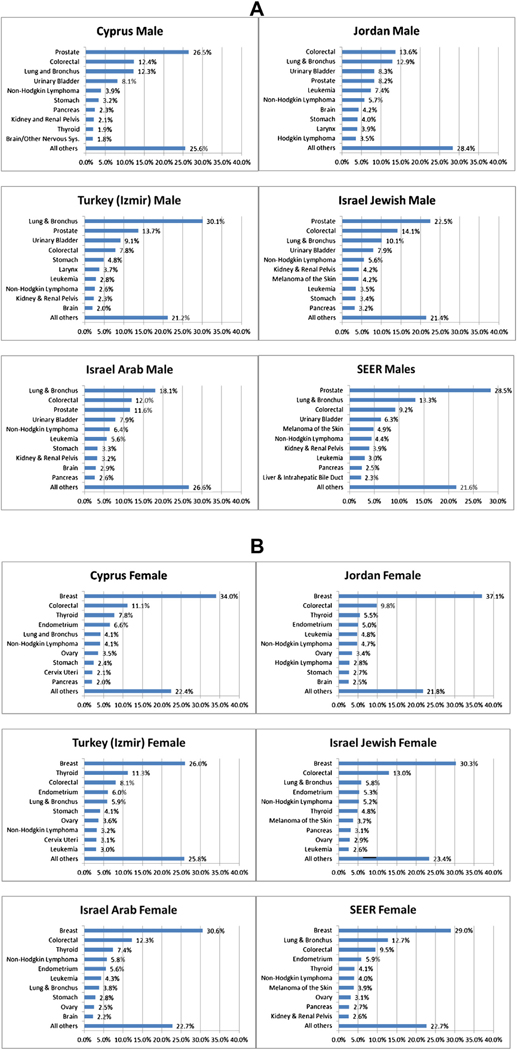
Figs. 3A and B present bar charts for the ten most common cancer types in each registry. There is variability in the distribution of cancer types observed within each country. In men, lung cancer constituted 30.1% of all cancers in Izmir while only 10.1% in the Israeli Jewish male population. The proportion of prostate cancer is similar in Cyprus (26.5%) and Israel Jews (22.5%) and SEER (28.5%), compared to only 8.2% in Jordan, 11.6% in Israeli Arabs and 13.7% in Izmir. Jordan and Israeli Arabs show the highest leukemia rates (7.4% and 5.6% respectively) compared to only 3.0% in US SEER. Breast cancer is the most common cancer in females in all participating registries, ranging from 26.0% of cases in Izmir to 37.1% of cases in Jordan. Female lung cancer accounted for less than 6% in all four Countries studied compared to, 12.7% in SEER.
Fig. 3.
A: Cancer case distribution by country in males. B: Cancer case distribution by country in females.
Table 2A and B present the age-standardized incidence rates (per 100,000) of the eight most common cancers in males (prostate, colorectal, lung and bronchus, non-Hodgkin lymphoma, urinary bladder, kidney and renal and kidney pelvis, stomach and pancreas) and in females (breast, colorectal, lung and bronchus, non-Hodgkin lymphoma, thyroid, ovarian, stomach and endometrium) for each of the four MECC countries and US SEER. Among the four MECC registries, the largest variability of rates between countries in males is for lung cancer followed by prostate cancer. Izmir has the highest lung cancer rate of 98.0 per 100,000, five times as high as the rate in Jordan (19.1 per 100,000). Israeli Jews show the highest prostate cancer rate (75.7 per 100,000), twice as high as Arabs living in the same country (38.5 per 100,000) and five times as high as in Jordan (13.7 per 100,000). Among females, the magnitude of variation across registries is not as large as in males. The largest variation is in breast cancer rates with the highest rate in Israeli Jews (100.4 per 100,000) and lowest rate in Izmir (50.7 per 100,000) and Jordan (51.9 per 100,000).
Table 2.
Age-standardized incidence rate (per 100,000) of common cancer in each country.
| A: Age-standardized incidence rate of cancers in male, 2005–2010 | ||||||||
|---|---|---|---|---|---|---|---|---|
| Prostate | Colorectal | Lung & Bronchus | Non-Hodgkin Lymphoma | Urinary Bladder | Kidney and Renal Pelvis | Stomach | Pancreas | |
| Cyprus | 71.3 | 34.1 | 33.8 | 11.8 | 22.3 | 6.0 | 9.1 | 6.4 |
| Jordan | 13.7 | 19.6 | 19.1 | 6.5 | 12.3 | 3.5 | 5.6 | 2.8 |
| Izmir | 47.4 | 25.8 | 98.0 | 8.4 | 30.7 | 7.3 | 15.8 | 6.4 |
| I.J. | 75.7 | 46.7 | 33.9 | 19.7 | 26.0 | 14.8 | 11.1 | 10.3 |
| I.A. | 38.5 | 34.9 | 54.3 | 14.9 | 24.0 | 8.4 | 9.2 | 7.8 |
| SEER | 114.9 | 36.5 | 52.5 | 17.8 | 24.5 | 15.9 | 7.4 | 9.7 |
| B: Age-standardized incidence rate of cancers in female, 2005–2010 | ||||||||
|---|---|---|---|---|---|---|---|---|
| Breast | Colorectal | Lung & Bronchus | Non-Hodgkin Lymphoma | Thyroid | Ovarian | Stomach | Endometrium | |
| Cyprus | 85.8 | 24.4 | 9.5 | 9.7 | 22.6 | 8.7 | 5.2 | 15.4 |
| Jordan | 51.9 | 14.9 | 3.9 | 6.5 | 6.0 | 4.7 | 4.1 | 8.1 |
| Izmir | 50.7 | 15.7 | 11.4 | 6.3 | 22.1 | 7.1 | 7.8 | 11.9 |
| I.J. | 100.4 | 35.5 | 16.4 | 15.7 | 18.2 | 9.1 | 6.1 | 16.2 |
| I.A. | 62.9 | 29.0 | 9.4 | 12.3 | 12.4 | 5.4 | 6.4 | 13.1 |
| SEER | 95.1 | 27.3 | 37.5 | 12.2 | 15.8 | 9.9 | 3.8 | 19.4 |
Izmir:Izmir (Turkey); I.J.:Israeli Jew; I.A.:Israeli Arab.
Table 3 presents age-adjusted male to female rate ratios by country for major cancer types (breast (multiplied by 100), colorectal, lung, bladder, non-Hodgkin lymphoma, kidney and renal pelvis, thyroid, pancreas and all cancers) during the time period 2005–2010 and male to female ratios of age standardized prevalence of smoking from 1980 to 2012 [9]. There are major differences in the rate of smoking related cancers such as lung where Izmir has a ratio of 8.6 compared to US SEER of 1.4, and bladder cancer where Izmir and Israeli Arabs have a ratio of 7.3 compared to a ratio of 4.0 in US SEER. It is worth noting here that male to female rate ratios for lung and bladder cancers are approximately twice as high as in four Middle East countries compared to US SEER. The rate ratios are similar across countries for other cancer sites listed in Table 3. For all cancers combined, the rate ratio in Izmir is 1.7 compared to other registries where the rate ratios range from 1.0 to 1.3. Smoking prevalence rate ratios during the period of 1980–2012 were highest in Jordan (5.1) followed by Izmir (3.0), Cyprus (2.3), Israel (1.6) and US (1.2).
Table 3.
Age adjusted male to female incidence rate ratios of specified cancers and male to female ratio of age-standardized prevalence of smoking 1980–2012 by country.
| Male to female ratio |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Breast (Multiplied by 100) | Colorectal | Lung | Bladder | NHLa | Kidney | Thyroid | Pancreas | All cancers | Prevalence of smoking [9] | |
| Cyprus | 1.2 | 1.4 | 3.6 | 6.2 | 1.2 | 2.2 | 0.3 | 1.6 | 1.2 | 2.3 |
| Jordan | 1.5 | 1.3 | 4.9 | 6.8 | 1.0 | 2.1 | 0.3 | 1.6 | 1.0 | 5.1 |
| Izmir (Turkey) | 2.0 | 1.6 | 8.6 | 7.3 | 1.3 | 1.9 | 0.2 | 1.6 | 1.7 | 3.0 |
| Israeli Jew | 1.3 | 1.3 | 2.1 | 5.0 | 1.3 | 2.1 | 0.3 | 1.3 | 1.1 | 1.6b |
| Israeli Arab | 1.7 | 1.2 | 5.8 | 7.3 | 1.2 | 2.5 | 0.3 | 1.5 | 1.3 | |
| 0.9 | 1.3 | 1.4 | 4.0 | 1.5 | 2.0 | 0.3 | 1.3 | 1.3 | 1.2 | |
Non-Hodgkin lymphoma.
Data for both Israeli Arabs and Jews.
4. Discussion
The increase in life expectancy in low to middle income countries, the reduction in mortality rates due to decrease in infectious diseases, and the increase in environmental exposures to carcinogens, including tobacco smoke and industrial chemicals are expected to result in a worldwide rise in cancer incidence in the coming years. Consequently, there is an urgent need for accurate data on population-based cancer rates in low and middle-income countries to monitor increases and implement cancer prevention and control where needed. The purpose of this study was to examine the consistency of cancer rates over a six year period and identify the most common cancers in four Middle East countries using unified standardized methods for data collection, quality control and data analysis. Our results show consistency in overall incidence rates within the countries over the six-year study period (Table 1). This indicates a high quality and completeness of case ascertainment at the population level, which supports the validity of the rates reported.
Among the four Middle East registries, Israeli Jews have the highest overall cancer rates in both males and females. Genetic predisposition in different race/ethnic groups may account for the different incidence rates within the same country. Jordan has consistently lower cancer rates compared to other populations studied. Since we used uniform methods for data collection, quality control and analysis, it is possible that the lower rates in Jordan are due to lower life expectancy compared to the other three countries studied. Cancer cases among the elderly population, especially elderly women over the age of 70 in Jordan may be related to under diagnosis. Also, due to the small size of the elderly population in Jordan, the rates may be unstable which accounts for the drop in age specific incidence rates for older than 70 age groups (Fig. 2A and B).
Despite similar overall ASR in the four Middle East countries studied, the distributions of proportions of cancer sites in the countries are different. The highest proportion of male cancer in Cyprus, Israeli Jews and US is prostate cancer which may be related to much more common PSA prostate cancer screening in these Countries. Lung cancer is the top male cancer in Izmir and Israeli Arabs which may be related to the prevalent smoking and other environmental exposures in these populations. More Jordanian males were diagnosed with colorectal cancer than other cancer sites in Jordan. However the rates do not exceed the rates from SEER. Among females, breast cancer has the highest proportion in all countries including US, which supports the importance of international efforts in breast cancer prevention and control efforts.
Smoking is the leading cause of cancer especially lung cancer [10–12]. Due to high smoking prevalence in Middle East countries, it was important to examine the relationship of lung cancer incidence rate and smoking patterns. The rates of male lung cancer showed large differences among countries and between genders. Turkish men have the highest rate of lung cancer (98.0 per 100,000), which is almost twice as high as in Israeli Arabs (54.3 per 100,000) and in U.S males (52.5 per 100,000). However, among the four Middle East registries, Turkish women have the second highest lung cancer rate of 11.4 per 100,000. However this rate is lower than that among Israeli Jewish women (16.4 per 100,000). Moreover, the rate in U.S females (37.5 per 100,000) is much higher compared to females in the four Middle East countries. These differences suggest possible differences in history of smoking prevalence in women in the past and the latency period for lung cancer. The trend is likely to change in the future with less women smoking in the US and more women smoking in the Middle East countries. In general, countries with high smoking prevalence (Turkey and Israeli Arabs) have high lung cancer rate. Jordan’s low lung cancer rates provides a paradox of a high smoking prevalence country but low lung cancer incidence and merits further investigation. It is possible that the high smoking prevalence in Jordan is causing lung cancer that is diagnosed at late stage leading to high mortality, short survival time before their cancer registration leading to low incidence in Jordan. Table 2A and B indicate that smoking-related cancers (lung and bladder) are more prevalent in males in countries with high population smoking rates, in particular in Izmir. Of interest is that this correlation was not observed in females which pose doubt that smoking is the only exposure factor in males. Other epidemiological risk factors, e.g. asbestos-like exposure and high arsenic level in drinking water in Turkey may also play a role in the observed high male lung cancer rate in Turkey [13,14]. However, the high lung cancer rate in men and low rate in women can be explained by the male to female ratios of lung cancer and smoking prevalence presented in Table 3. There is generally a good correlation of male to female smoking ratios with ratios of lung cancer in males and females in all four Middle East countries, except for Izmir where it has the highest male to female ratio for lung cancer (8.6) while the male to female smoking rate ratio is only 3.0. This observation may be associated with the latency period of at least 20 years that is generally required for smoking to cause lung cancer [15,16]. Hence not only women in the Middle East countries have taken up smoking overall at a lower rate than men, it is also likely that they have taken up smoking at a later stage chronologically (more recently), and it is likely that lung cancer rates in women especially in Izmir will increase in the future. This is supported by a descriptive model of gender related smoking prevalence and rate of deaths in developed countries proposed by Lopez et al. [17], which potentially can explain the figures seen in the Middle East countries.
The highest incidence rate of prostate cancer in Middle East registries studied was observed in Israeli Jews and in Cyprus, considerably higher than Izmir, Israeli Arabs and in Jordan but lower than SEER. Beyond differences in diet and lifestyle this large difference is likely to be due to large differences in the rate of implementation of the Prostate-Specific Antigen (PSA) screening test with more PSA screening in more organized/affluent health care systems (US, Israeli Jews, Cyprus) compared to low to middle income countries.
There is less but clear variation in incidence rates of female breast cancer between the four countries studied. The rates in Cyprus, Jordan, Izmir and Israeli Arabs range from 50.7 to 85.8 per 100,000, and a higher rate of 100.4 per 100,000 in Israeli Jews, which is similar to 95.1 per 100,000 to US SEER. The differences in rates are consistent with the expected level of screening practices in the countries studied. The differences observed are also likely to relate to diet, lifestyle and genetic differences [18].
As another smoking related malignancy, bladder cancer appears to have similar trends as in lung cancer in Middle East countries studied. Of note is that there is a discrepancy in the male to female ratio of bladder cancer in SEER (4.0 compared to a smoking prevalence ratio in the US of 1.2). This male preponderance has been reported before and found to persist unrelated to smoking rates or exposure to occupational hazards. This indicates that unidentified environmental, dietary exposures or hormonal factors may play a role in the etiology of bladder cancer. On the other hand, this discrepancy may also be due to a protective effect of estrogens in premenopausal women [19]. This may also explain why the male to female ratios for bladder cancer are higher in Middle East countries with the exception of Izmir compared to the same ratios for lung cancer despite the same etiological factor of smoking.
Colorectal cancer is common in both genders in the four Middle East countries. The incidence rate in the Israeli Jewish population (46.7 per 100,000 in males and 35.5 per 100,000 in females) are the highest among the four Middle East countries and are similar to the rates in the US. The lowest incidence rates observed are in the Jordanian population (19.6 per 100,000 in males and 14.9 per 100,000 in females).
Of interest in this paper is the statistical approach and data analysis used for this research project. The four registries used unified standardized and quality controlled methods for case findings, ascertainment, abstraction of cancer patient data coding, data entry and consolidation of records for more than 10 years. For data analysis and combining the data without the lengthy process of creating a combined database with concerns about confidentiality, we implemented a novel method to generate and combine the data from all registries. This approach includes communications and agreement about the direction of the analysis, the objectives of the analysis for each joint publication and generating statistical code to be used by all participating registries. This resulted in unified data collection, data analysis and seamless way of combining the results to generate the tables and figures in this paper as well as other papers. The results of this study demonstrate that the approach, standardization and collaboration between investigators from different countries, languages and policies are feasible, effective and reliable. It provides an opportunity for other countries in Middle East and Northern and Central Africa where it is expected that cancer registries will be established to participate in future studies led by International Agency for Research on Cancer where the regional hub is located in Izmir.
In conclusion, our study provides reliable information about cancer incidence in four Middle East countries compared to the US SEER. The results provide baseline information for future cancer control and prevention programs in these countries. The study also shed light on the relationship of cancer incidence with possible lifestyle and health care system factors in different countries. Moreover, cancer incidence rates in Israeli Jewish and Arab populations were examined separately, which gives us a unique way to study incidence rates of two race/ethnicities in one country. This study also has identified major differences in age-standardized incidence rates for various common cancers. We also examined the relationship between smoking prevalence and smoking-related cancers such as lung and bladder cancers. Future studies examining individual cancer sites are in progress and are likely to help design cancer prevention and control research programs specific for these countries.
Acknowledgments
Novelty and Impact: We used a novel unified statistical analysis method to generate combined cancer registry data from four Middle East countries (Cyprus, Jordan, Israel (Jews and Arabs) and Izmir (Turkey)) while maintaining the security and confidentiality of data in individual registries. This paper also focusses on the consistency of cancer incidence rates of common cancer types in each of the four countries to examine the validity and quality of registry data in the four countries to encourage the use of the data for future cancer control and prevention programs.
Abbreviations:
- MECC
Middle East Cancer Consortium
- SEER
Surveillance, Epidemiology and End Results
References
- [1].GLOBOCAN 2012: Estimated cancer incidence, mortality and prevalence worldwide in 2012 http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx (last accessed January 2016). [Google Scholar]
- [2].Preparing developing countries to face increase in cancer. International Agency for Research on Cancer http://gicr.iarc.fr/en/The-Problem (last accessed January 2016) [Google Scholar]
- [3].Silbermann M, Manual of Standards for Cancer Registration, Fourth edition, March 2005. http://www.moh.gov.cy/MOH/MOH.nsf/All/D6C382E728E5320FC22579C600265CDE/$file/MECC%20Manual%20of%20Standards%204th%20Edition%20March%202005.pdf (last accessed January 2016). [Google Scholar]
- [4].Middle East Cancer Consortium, http://www.cancer.gov/about-nci/organization/cgh/research/mecc (last accessed January 2016). [Google Scholar]
- [5].Silbermann M, MECC Manual of Coding and Staging Version 5.1, July 2009. http://www.moh.gov.cy/Moh/moh.nsf/All/D6C382E728E5320FC22579C600265CDE/$file/MECC%20Manual%20of%20Coding%20and%20Staging%205.1%20July%202009.pdf (last accessed January 2016). [Google Scholar]
- [6].Overview of the SEER program, http://seer.cancer.gov/about/overview.html (last accessed January 2016). [Google Scholar]
- [7].International rules for multiple primary cancers (ICD-O; Third edition), http://www.iacr.com.fr/images/doc/MPrules_july2004.pdf. [DOI] [PubMed] [Google Scholar]
- [8].http://seer.cancer.gov/stdpopulations/world.who.html (last accessed January 2016).
- [9].Ng M, Freeman MK, Fleming TD, Robinson M, Dwyer-Lindgren L, Thomson B, Wollum A, Sanman E, Wulf S, Lopez AD, Murray CJ, Gakidou E, Smoking prevalence and cigarette consumption in 187 countries, 1980–2012, JAMA 311 (January (2)) (2014) 183–192. [DOI] [PubMed] [Google Scholar]
- [10].Gandini S, Botteri E, Iodice S, Boniol M, Lowenfels AB, Maisonneuve P, Boyle P, Tobacco smoking and cancer: a meta-analysis, Int. J. Cancer 122 (2008) 155–164. [DOI] [PubMed] [Google Scholar]
- [11].Bray F, Tyczynski JE, Parkin DM, Going up or coming down? The changing phases of the lung cancer epidemic from 1967 to 1999 in the 15 European Union countries, Eur. J. Cancer 40 (1) (2004. January) 96–125. [DOI] [PubMed] [Google Scholar]
- [12].Sasco AJ, Secretan MB, Straif K, Tobacco smoking and cancer: a brief review of recent epidemiological evidence, Lung Cancer 45 (Suppl. 2) (2004) S3–S9. [DOI] [PubMed] [Google Scholar]
- [13].Berk S, Yalcin H, Dogan OT, Epozturk K, Akkurt I, Seyfikli Z, The assessment of the malignant mesothelioma cases and environmental asbestos exposure in Sivas province, Turkey, Environ. Geochem. Health 36 (February (1)) (2014) 55–64. [DOI] [PubMed] [Google Scholar]
- [14].Gunduz O, Bakar C, Simsek C, Baba A, Elci A, Gurleyuk H, Mutlu M, Cakir A, Statistical analysis of causes of death (2005–2010) in villages of Simav Plain, Turkey, with high arsenic levels in drinking water supplies, Arch. Environ. Occup. Health 70 (1) (2015) 35–46. [DOI] [PubMed] [Google Scholar]
- [15].Archer Victor E., Coons Teresa, Saccomanno Geno, Hong Dae-Yong, Latency and the lung cancer epidemic among United States uranium miners, Health Phys. 87 (5) (2004) 480–489. [DOI] [PubMed] [Google Scholar]
- [16].Weiss W, Cigarette smoking and lung cancer trends. A light at the end of the tunnel? Chest 111 (1997) 1414–1416. [DOI] [PubMed] [Google Scholar]
- [17].Lopez AD, Collishaw NE, Piha T, A descriptive model of the cigarette epidemic in developed countries, Tob. Control 3 (1994) 242–247. [Google Scholar]
- [18].Chlebowski RT, Nutrition and physical activity influence on breast cancer incidence and outcome, Breast 22 (2013) S30–S37. [DOI] [PubMed] [Google Scholar]
- [19].Zhang Y, Understanding the gender disparity in bladder cancer risk: the impact of sex hormones and liver on bladder susceptibility to carcinogens, J. Environ. Sci. Health C Environ. Carcinog. Ecotoxicol. Rev 31 (4) (2013) 287–304. [DOI] [PMC free article] [PubMed] [Google Scholar]